Platelets Generated In Vitro From Proplatelet-Displaying
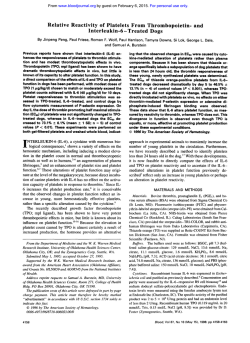
From www.bloodjournal.org by guest on February 6, 2015. For personal use only. Platelets Generated In Vitro From Proplatelet-Displaying Human Megakaryocytes Are Functional By Esther S.Choi, Janet L. Nichol, Martha M. Hokom, Alex C. Hornkohl, and Pamela Hunt An in vitro culturesystemdemonstrating the transitions from megakaryocyte progenitors to functional platelets is described. CD3Cselected cells from normal human peripheral blood are cultured under conditions that promote megakaryocyte formation. After 8 to 11 days, enriched populations of mature megakaryocytes are replated under conditions that favor the development of proplatelets. Proplatelets express the platelet-specificproteins,glycoproteins Ib and Ilb (GPlb and GPllb), and fibrinogen and also contain microtubule coils equal in size to those found in plasma-derived platelets. In addition, proplatelets have ultrastructuralfeatures in common with plasma-derivedplatelets. Platelet-sized particlesfrom the proplatelet culture su- pernatants are examined. Ultrastructurally, these particles are identicalto plasma-derivedplatelets. Functionally, these culture-derived platelets aggregate in response to both thrombin and adenosine diphosphate (ADP) plus fibrinogen. This aggregation is specifically inhibited by the addition of a function-blocking anti-GPllbllla antibody. Culture-derived platelets stimulated with agonists also express the activation-dependent antigens P-selectin and functional fibrinogen receptor. This is the first description of an in vitro culture system that sequentially demonstrates megakaryocyte growth, development, and platelet production. 0 1995 by The American Societyof Hematology. P LATELETS ORIGINATE from megakaryocytes during tems that rely on rodent10~14~15~18~23,24"29 or bovine" megathe terminal differentiationphase of karyocytes may be of limited value to the study of human thrombopoiesis. However, the precise mechanism by which platelets are shed This report describes a model system in which functional from megakaryocytes is not fully understood. Studies of this platelets are generated in vitro from human megakaryocytes. process are hampered by the low frequency of megakaryoPlatelet formation appears to occur via proplatelet intermedicytes in bone marrow as well as by a lack of in vitro systems ate structures. The system exploits earlier observations that in which platelet shedding reproducibly occurs. Theoretic human megakaryocytes can be generated from peripheral models of platelet shedding have been developed from obserblood leukocytes stimulated with plasma from thrombocytovations of fixed cells. Megakaryocytes displaying membrapenic ani mal^.^' In the present study, the frequency of culnous structures outlining platelet-fields form the basis of ture-generated megakaryocytes was improved by preenrichthe demarcation membrane model of platelet shedding.'.' ing the leukocyte population for CD34+ megakaryocyte Observations of long cytoplasmic processes emanating from progenitors. Mature megakaryocytes that appear within 8 to megakaryocyte cell bodies have led to the proplatelet con1l days of culture are then available for studies of proplatelet cept?"' Proplatelets, dependent on microtubules for stabildevelopment and, subsequently, for platelet fragmentation. ity,l2-I5display constrictions along their lengths that define This in vitro system is relevant to clinical conditions that platelet-sized area^.",^^"^ The areas between the attenuation affect the last phase of thrombopoiesis, platelet formation points contain platelet-specific organelles and proand release. t e i n ~ . ' " ' ' ~Micrographs ~ ~ ~ , ~ ~ . of ~ ~bone marrowfixed in situ show proplatelets projecting through the endothelial cell MATERIALS AND METHODS layer of marrow venous sinusoids into the c i r ~ u l a t i o n . ~ ~ " ~ ' ~ ~ ' ~ It has been postulated that the circulatory shear force within Isolation of CD34+ Progenitor Cells From Peripheral the m a r r ~ w ' . ~or~possibly .~~ the aids in the fragBlood mentation of proplatelets into platelets. Written informed consent was obtained from donors of leukapherThe study of proplatelet development has been advanced esis units, normal AB plasma, and plasma-derived platelets. Leuthrough the use of tissue culture systems that permit this kapheresis units from a pool of normal healthy donors committed to differentiation process to occur in vitro.L4~15'1',1y,23-30 Although the program were purchased from HemaCare (LeukaPAK; Sherman these culture systems have been useful for the study of proOaks, CA). Peripheral mononuclear cells were isolated by FicollPaque (Pharmacia, Piscataway, NJ), rinsed, and adherence-depleted platelet development, they have been of limited value for overnight. Nonadherent cells were collected and fractionated with the study of platelet fragmentation as observations of platecounterflow centrifugal elutriation in a Beckman (Fullerton, CA) J2let-like particles in these cultures are reported as rare M1 centrifuge with a JE-6B elutriation rotor to enrich for megakaryevents14.15.18,25,26.31 and in no case has the identity and function ocyte progenitor^.'^" Rotor speed was 2,020 rpm, and the flow rate of the particles been established. Furthermore, culture syswas increased by 0.5 W m i n from 8.5 W m i n to 13 W m i n over From AMGEN, Inc Thousand Oaks, CA. Submitted March 17, 1994; accepted September 13, 1994. Address reprint requests to Pamela Hunt, PhD, AMGEN,Inc, Amgen Center, mail stop T-1A-206, Thousand O a b , CA 91320. The publication costs of this article were defrayed in part by page charge payment. This article must therefore be hereby marked "advertisement" in accordance with 18 U.S.C. section 1734 solely to indicate this fact. 0 1995 by The American Society of Hematology. 0006-4971/95/8502-0002$3.00/0 402 63 minutes. Cells of interest were collected in 50-mL fractions at flow rates from 11 to 13 mUmin and frozen in 90%fetal bovine serum (FBS) and 10% dimethylsulfoxide (DMSO) in the cell freezer (Gordinier 9000) using Cryopack Software Version 3.2 (Gordinier Electronics Inc. Roseville, MI) until use. In some experiments, leukapheresis units were processed without elutriation. Mononuclear cells were isolated by Ficoll-Paque in Hank's buffered saline solution (HBSS) containing phenol red (GIBCO, Grand Island, NY). After rinsing in HBSS, cells were either processed immediately or after overnight incubation in Iscove's Modified Dulbecco's medium (IMDM) and 10% FBS at 4°C. Blood, Vol 85, No 2 (January 15). 1995: pp 402-413 From www.bloodjournal.org by guest on February 6, 2015. For personal use only. 403 FUNCTIONALCULTURE-DERIVED HUMAN PLATELETS CD34" progenitor cells were isolated using a magnetic cell sorting system, Mini-MACS (Miltenyi Biotec, Auburn, CA) by one of two methods. One method used anti-CD34-biotinylated antibody from AMAC (Westbrook, ME) followed by stxptavidin microbeads (Miltenyi Biotec). The other method used the CD34 isolation kit (Miltenyi Biotec) in accordance with the manufacturer's recommendations. When elutriated, frozen/thawed cells were processed; an average of 1.4 X 106 CD34' cells were obtained per leukapheresis unit, with a range of 2.0 X 10" to 4.0 X 106 (n = 9). When nonelutriated, fresh cells were processed, an average of 4.8 X lo6 CD34+ cells were obtained per leukapheresis unit, with a range of 2.9 X lo6to 6.2 X lo6 (n = 4). Elutriated cell populations contained fewer CD34" cells than nonelutriated cell populations as they had been preenriched for megakaryocyte progenitors. The wide range in the number of CD34+ cells obtained was attributed to donor variation3& The purity of CD3Cselected cells was determined for each isolation by using a combination of anti-CD34 antibodies [HPCA-l and HPCA-2, each at 1:lO in phosphate-buffered saline (PBS); Becton Dickinson, Lincoln Park, NJ] and the HistoMark Streptavidin-P-Gal system (Kirkegaard and Perry Labs, Gaithersburg, MD). Immunopositive blue cells were counted microscopically. On the average, cells selected with anti-CD34 biotinylated antibody followed by streptavidin microbeads were about 40% CD34' (range, 15% to 93%; r = 19). Similarly, cells selected with the CD34 isolation kit averaged about 50% CD34+ (range, 22% to 90%; n = 8). When CD34-selected cells were reapplied to Mini-MACS columns, the percentage of CD34+ cells increased to an average of 90% (range, 83% to 93.5%; n = 4). The percentage of CD34+ cells obtained by this staining method and by flow cytometric analyses were virtually identical in every case studied. Culture of Human Megakaryocytes CD34+ enriched cells were stimulated to form megakaryocytes in the culture system described by Mazur et a l . 3 2 All of the reagents were purchased from GIBCO unless indicated otherwise. Briefly, the cells were plated at 5 X 10' cells per milliliter in growth medium (Meg GM) that consisted of IMDM with 1 X penicillin/streptomycin/ glutamine (P/S/G), 1 X sodium pyruvate, 1 X minimum essential medium vitamins, 1 X nonessential amino acids, 0.1 mmoVL 3mercapto l-propanediol, 2 mg/mL L-asparagine, and 0.2% deionized bovine serum albumin (BSA; Calbiochem, San Diego, CA). Fresh Meg GM was prepared every 2 weeks. Meg GM was supplemented with 10% normal human platelet-poor heparinized (33 U/mL) AB plasma, and 10% aplastic canine Cells were incubated in 96-well or 24-well tissue culture plates (Falcon, Lincoln Park, NJ) in volumes of 100 pL or 5 0 0 pL, respectively, at 37°C with 5% CO2 for 8 to 11 days. Enrichment of Human Megakaryocytes Megakaryocytes were enriched from the cultured cell population according to the procedure of Levine and F e d ~ r k o ?with ~ some , OO modifications. Cultured cells were collected, centrifuged at 1O rpm for 15 minutes, resuspended in CATCH buffer at 5 X lO%nL, and subjected to velocity ~edimentation~'.~~ that consisted of a twostep BSA-gradient, 2.41% (450 pL) and 4.83% (900 pL), at lg for 1.5 hours. No more than 2.5 X 10' cells were applied to onevelocity sedimentation tube (Falcon no. 2063). Cells that entered the bottom layer were collected. Megakaryocytes were identified by immunostaining with an anti-glycoprotein Ib/Ib/IIb antibody cocktail (antiGPIb/Ib/IIb; anti-Ib purchased from DAKO Corp, Carpenteria, CA; anti-Ib and anti-IIb purchased from Biodesign, Kennebunkprt, ME) and the HistoMark Streptavidin-b-Gal System. Immunopositive blue cells were microscopically counted. For morphologic analyses, the cells were cytocentrifuged onto slides (Shandon Inc, Pittsburgh, PA) at 400 rpm for 5 minutes and stained with a modification of WrightGiemsa stain using Wescor's automatic cell stainer (Wescor Inc, Logan, UT; model no. 7120). Megakaryocytes were staged according to the criteria of vin ne." Induction of Proplatelets From Mature Megakaryocytes The megakaryocyte-enriched population was replated in Meg GM at 5 X 1cv' cells per milliliter in 96-well plates (Falcon no. 3072) supplemented with 10% heparinized human AB plasma but without aplastic canine serum. Some experiments were conducted in the absence of 10% AB plasma to determine the necessity of plasma for proplatelet induction. The cultures were examined daily for emergence of proplatelets. A megakaryocyte bearing one or more cytoplasmic processes was considered a proplatelet-displaying megakaryocyte. The processes were at least twice the length of the cell body diameter. The percentage of megakaryocytes displaying one or more cytoplasmic processes was determined by visual examination of video prints taken of the culture wells. Detection of Platelet-Specijc GPIbIIbIIIb on Proplatelet Membranes Megakaryocytes displaying proplatelets were fixed in situ by adding glutaraldehyde (1.6% final concentration) to the culture wells. The culture plates were then centrifuged at 800 rpm for 15 minutes. The cells were rinsed and blocked with 10% normal goat serum (NGS) for 20 minutes at room temperature. Anti-GPIb/Ib/IIb cocktail and the HistoMark Streptavidin-P-Gal system was used as described above. Detection of Fibrinogen Within Proplatelets by Indirect Imrnunojluorescence Megakaryocytes displaying proplatelets were stabilized with 0.38% formaldehyde and 100 mmoVL EDTA and sedimented onto silanized slides (Oncor, Gaithersburg, MD) by cytocentrifugation. These cells were fixed for 20 minutes in 4% paraformaldehyde and 1% Triton-X 100, rinsed three times in PBS, and then blocked for 20 minutes in 10% FBS-PBS at room temperature. Mouse antifibrinogen monoclonal antibody (MoAb; American Diagnostics, Greenwich, CT) was used at 1:50 in 10% FBS-PBS for 1 hour at room temperature. Goat anti-mouse-fluorescein isothiocyanate (FITC; Cappel, Durham, NC) was used at 1:1,OOO in 10% FBSPBS for 30 minutes at room temperature. Slides were mounted in Immumount (Shandon) and visualized with an Olympus BH2 microscope (Olympus, Chatsworth, CA). Detection of Microtubules Within Proplatelets by Indirect Imrnunojluorescence For microtubule staining, megakaryocytes displaying proplatelets were treated as above except that 4% paraformaldehyde, 1% TritonX 100, and 10%methanol was used as a fixative. Cells were blocked with 5% NGS in PBS for 20 minutes at room temperature. The antitubulin antibody cocktail (anti-a-tubulin MoAb, Amersham, Buckinghamshire, England; anti-P-tubulin MoAb, Amersham; and rabbit anti-tubulin antibody, Biomedical Technologies, Stoughton, MA, at manufacturers' recommended dilutions) was incubated with cells at 37°C for 1 hour. Goat anti-mouse IgG-FITC and goat anti-rabbit IgGFITC (Cappel; at 1:1,OOO each) were used as secondary antibodies at 37°C for 30 minutes. Cells were rinsed and mounted in Immumount and visualized with a Nikon MICROPHOT-FXA microscope (Nikon, Irvine, CA). Electron Microscopy of Proplatelets and Platelets Megakaryocytes displaying proplatelets were stabilized with 0.38% formaldehyde and 100 mmoVL EDTA, centrifuged at 800 From www.bloodjournal.org by guest on February 6, 2015. For personal use only. CH01 ET AL 404 . Y . "- Fig l. Mature megakaryocyte selection, proplatelet development, and presence of platelet-specific proteins detected on the surface and within proplatelets. (AI A representative Wright-Giemsa staining of megakaryocytes after 8 days of culture time enriched by velocity sedimentation 153% megakaryocytes; bar, 40 pm). (B) Phase micrograph of proplatelet development 3 days after replating (bar, 40 pm). (C1 Anti-GPlbl Ib/llb antibody staining on proplatelets detected by HistoMark, bright-field micrograph (bar, 15 pm). (D) Control panel for HistoMark, in which the primary antibody cocktail was omitted (bar, 13 pm). (E) Anti-fibrinogen antibody within proplatelets detected by indirect immunofluorescence (bar, 40 pm). rpm for 1 S minutes, resuspended in 1% glutaraldehyde, and allowed to settle on poly-L-lysine coated aclar film for 4.5 minutes. The cells were rinsed with PBS, treated with I % OsOI for I hour, rinsed with PBS,and sequentially dehydrated with ethanol (30%. SO%, 70%. and 90%). Uranyl acetate (2%) was included during the 70% ethanol dehydration step. The cells were infiltrated with 50% L.R. White plastic (EM Sciences, Fort Washington, PA: medium grade) in ethanol for IS minutes, then treated to two changes of 1 0 0 % L.R. White over 24 hours. Fresh L.R. White was polymerized onto aclar film in aluminum dishes at 52°Cfor 24 hours. Proplatelets were identified under the light microscope on polymerized plastic, sectioned, and viewed under the electron microscope (Phillips 300, Mahwah, NJ). Plasma-derived platelets were obtained as reported previo~sly.'~ Platelet-sized fragments (putative culture-derived platelets) were isolated from culture supernatantsin which significant numbersof megakaryocytes displaying proplatelets had been visible 24 hours earlier (proplatelet cultures). These culture supernatants were centrifuged at 1,OOO rpm (Sorvall RT6000, DuPont, Newtown, C T ) for IS minutes at roomtemperature. Half ofthe culture volumes (approximately S0 pL per well) was taken from the top of each well and pooled to one tube. The pooled material was centrifuged at 1,200 rpm (Sorvall RT6000) for IS minutes to pellet cells carried over from culture. The supernatant containing platelet-sized fragments was placed in fresh 1.5-mL microfuge tubes and centrifuged at 7,000 rpm (Beckman Microfuge 12) for S minutes at room temperature. The supernatant from each tube was aspirated, leaving about 20 pL of medium in each tube. The pellets containing platelet-sized fragments were resuspended in the residual 20 pL ofmedium of each tubeand pooled in one microfuge tube. Plasma-derived and culture-derived platelets were fixed, dehydrated, and infiltrated as above in microfuge tubes that were centrifuged for each change of solution. Polymerization was also performed in the microfuge tubes, which were cut away before sectioning. Platelet Aggregation Studies Thrombin aggregation. Plasma-derived (citrated blood) or culture-derived platelets were rinsed three times withPBSandincubated with or without 0.8 UlmL thrombin (Sigma, St. Louis, MO) at 37°C for 10 minutes. Platelet preparations were then cytocentrifuged onto glass slides at 1,200 rpm for 5 minutes. The slides were air-dried and stained in a slide stainer. Adenosine diphosphate (ADP)/fibrinogenaggregation. Plasmaderived or culture-derived platelets were prepared bygel filtration according to Shattil et al'" on Sepharose-2B (Pharmacia) in gel filtration buffer (l37 mmol/L NaCI, 2.7 mmol/L KCI, 1 mmol/L MgCI2, 5.6 mmol/L glucose, I mglmL BSA, and 20 mmol/LHEPES: pH 7.4). For aggregation studies, I X 10' platelets were incubated for S minutes in 600 pglmL of human fibrinogen (American Diagnostica, Greenwich, CT) and 2 mmol/L ADP (Calbiochem) in a final volume of IS0 pL. Ten microliters of each platelet suspension were pipetted into wells of Terasaki-style microtiter plates (Vanguard International, Neptune, NJ) and fixed with glutaraldehyde (1.6% final concentration) for 15 minutes with low speed centrifugation (800 rpm: Sorvall6OOO).Preliminary experiments were performed todetermine the optimal concentrations of ADP and fibrinogen necessary to cause From www.bloodjournal.org by guest on February 6, 2015. For personal use only. 405 FUNCTIONAL CULTURE-DERIVED HUMAN PLATELETS Fig 2. Microtubule coils within proplatelets detected by anti-tubulin antibody cocktail indirect immunofluorescence. (AI Platelet-sizedcoils (3 to 5 p m ) are shown at thetips of fully developed proplatelets. Arrow indicates a proplatelet tip that ends in a tapered fashion. (B1 Plateletsized coils are also present along the lengths of proplatelets. (C) Negative control in which the primary antibody cocktail was omitted to demonstrate the specificity of fluorescence. All panels contain images of the same magnification (bar, 10 p m ] . aggregation of platelets at this concentration. Photographs ofthe platelet aggregates were taken through an inverted microscope. Inhibition of Platelet Aggregation by Anti-GPIIhIIIa Antibody Culture- and plasma-derived platelets were washed by gel filtration.'" Platelets were diluted to 2,000 platelets per microliter in the gel filtration buffer. To 10' platelets, 50 pglmL (final concentration) of either isotype control antibody (anti-CD34; AMAC) or anti-GPIIbIlIa antibody (AMAC; no. 0145) was added and allowed to incubate for 5 minutes at room temperature. 200 pglml of Human fibrinogen (200 pglmL; American Diagnostica) and 900 pmol/L of ADP (Calbiochem) were then added with gentle pipetting and allowed to incubate for an additional S minutes. Platelet suspensions were pipetted into microtiter wells to observe for aggregation. Platelets were tixed and photographed as described above. Video prints were taken of each field containing aggregates, and the longest diameter of each aggregate was measured. Detection of Activation-Dependent Antigens on Platelets P-selectin. Culture- and plasma-derived platelets were washed by gel filtration." A set of platelets from each population was fixed immediately (resting platelets) withan equal volume of cold 1% paraformaldehyde, pH 7.4. for at least 2 hours. Another set of platelets was stimulated with I UlmL thrombin for 1 minute and then fixed as above (activated platelets). Preliminary experiments determined the minimal concentration of thrombin necessary for activationof platelets at this concentration. Fixed platelets were rinsed and incubated for I hour with MoAb against CD62 (Serotec, Oxford, UK) or the isotype control mouse IgG, (Becton Dickinson) at final incubated concentrations of 10 pglmL. Platelets wererinsedand with goat anti-mouse-FITC (Cappel; 1:500) for 30 minutes, rinsed, and analyzed for fluorescence intensity by flow cytometry (FACScan Flow Cytometer, Becton Dickinson). The FACScan was calibrated using 2-pm beads (Becton Dickinson). Events were collected, without gating, on a log scale for forward side scatter (FSC) and side scatter (SSC; FSC, EOO; SSC, 326 V; fluorescence I [FLI 1. 686 V; FSC threshold, 1 0 0 V). An analytical gate was drawn on the FSC/ SSC dot plot ofresting platelets, which excluded a few large contam- inating cells and small debris. The same gate was transposedonto the FSClSSC plot of the activated platelet populations. The histograms shown represent gated events. For plasma-derived platelets, 50.000 events were collected from resting and activated populations, of which 48.821 and 48.010 respective events were analyzed. For culture-derived platelets, 7.000 events were collected from resting and activated populations, of which 4,068 and 3.503 respective events were analyzed. Specific fluorescence-positive platelets werethose with higher fluorescence intensity than seen with the isotype control. Percent specific fluorescence intensity was obtained by comparing specific fluorescence intensity to total fluorescence intensity. F~tnctir~nd Jihrinogenreceptor (nctir~ntdGPlIhllIn). Culturederived and plasma-derived platelets wereprepared bygel filtration." ADP stimulation and identification of activated GPllbllla by thePAC1 antibody was performed according to Shattil et al.'".'* Platelets were incubated with SO pglmL PACI-FITC with or without 40 pmol/L ADP andwithout stirring at room temperature for 15 minutes. Preliminary experiments determined the concentration of ADP necessary for significant activation. The platelets were diluted with equal volume of the gel elution buffer and analyzed byflow cytometry without fixation. Platelets were collected through a live FCSlSSC gate preset on the platelet population within whole blood.2x This gate excluded white blood cells. red blood cells, and debris. For each histogram. 25,000 gated events were collected. RESULTS Proplatelet Induction From Mature Megc~kan~ocytes CD34-enriched human peripheral blood cells were stimulated to form megakaryocytes by the addition 10% of aplastic canine plasma to Meg GM. After 8 days in culture, 82%. 8%. 7%. and 3% of the megakaryocytes were classified as stage I, 11, 111, or IV, respectively. After 12 days in culture, the relative proportions of megakaryocytes within each stage had shifted to 48%, 19%, 138, and 20%. respectively. Megakaryocyteswereenrichedfromthepopulationof cultured cells by velocity sedimentation (Fig IA). Cells selected by this procedure averaged S4% megakaryocytes (n = 13). with a range of 31 % to 82%. An average of 2 X IO6 From www.bloodjournal.org by guest on February 6, 2015. For personal use only. CH01 ET AL 406 Fig 3. Ultrastructural similarities between proplatelets and normal platelets. (A, B) Electron micrographs of megakaryocytes displaying proplatelets showing platelet-sized structures that are linked by thin cytoplasmic bridges (arrows in B). (C) Electron micrograph of plasmaderived (normal) platelets shown for size andultrastructuralcomparison with (A) and (B).All panels contain images of the same magnification (bar, 3 pm). mature megakaryocytes was obtained per leukapheresis unit, with a range of 4 X IOJ to 3 X IO". The megakaryocyte percentage values obtained from immunostaining closely correlated with those obtained by morphologic analysis. Other cell types frequently present in the megakaryocytecnriched population includedmyelomonocytic cells and blast cells of unknown origin. Veryfew lymphoid andno erythroid cells were detected (F. Naeim. UCLA Medical Center, University of California, Los Angeles, CA: July 1993). Enriched megakaryocytes were replated in Meg GM supplementedwith 10% heparinized human AB plasma but without aplastic canine serum. Within 2 to 3 days. megakaryocytes displaying proplatelets were observed (Fig 1 B). Constrictions delineating platelet-sized areas were seen along the length of the proplatelets. The frequency of cells displaying proplatelets increased with time after replating. At the peak of proplatelet development. generally occurring after 3 to 4 days postreplating, an average of 40% 5 16% of the megakaryocytes exhibited proplatelets. In some experiments, enriched megakaryocytes were replated on Matrigel (Collaborative Biomedical Research, Bedford, MA) to determine if the presence of extracellular matrix proteins and proteoglycansenhanced proplatelet development. Megakaryocytes replated on plastic or on Matrigel-coated surfaces both developed proplatelets with a similar time course. The percentage of megakaryocytes undergoing differentiation was approximately60% 5 S% in each case by day 3 postreplating (data not shown).To determine if plasmaproteinsaffectedproplateletdevelopment, megakaryocyte-enriched populations were replatcdin Mcg GM in theabsenceofheparinizedhumanABplasma. In these plasma-freeexperiments.proplateletdevelopmentstill occurred. although ata decreased frequency, which was generally 30% to 50% ofthatobservedwhenheparinizedhumanAB plasma was included in the medium. To determine if serum proteins affected proplatelet development, megakaryocyte-enriched populations were replated in Meg GM in the presence of 10% serum. The presence of serum significantly inhibited proplatelet development (data not shown). Detection of Platelet-Specjfic Proteins o n the S ~ r j a c eqf and Within Proplatelets GPIb and IIb are platelet-specific plasma membrane proteins found on the surface of megakaryocytes.""" Figure 1C shows that GPlb and IIb arepresent on thecellbody of megakaryocytes and throughout proplatelets. all the way to the tip. Figure I D shows the control experiment in which the primary antibody cocktail was omitted. The use of antiGPllla was avoided due to its tendency for non-specific binding in the presence of serum or plasma. Fibrinogen is a protein found in alpha-granules of mature megakaryocytes and resting Fibrinogen is localized within proplatelets as seen by indirect immunofluorescence of detergent-permeabilized megakaryocytes displaying proplatelets (Fig IE). There was no detectable staining when detergent was omitted during the fixation step (data not shown), indicating thatthefibrinogenmolecules are not cell surface-associated. Microtubule Coil Detection Within Proplatelets The presence of microtubule coils circumferentially located within platelets has beenwell documented andis a From www.bloodjournal.org by guest on February 6, 2015. For personal use only. _" Fig 4. Observation ofplatelet-sizedfragments from culture supernatants of megakaryocytes displaying proplatelets by phase microscopy. (A) The arrow indicates a row of platelet-sized fragments (putative culture-derived plateletsl, as if it had just been released from a proplatelet.(B)The arrow indicates platelet-sized doublets. Both panels contain images of the same magnification (bar, 40 pm). - _."I. *,* (4 a 1 Fig 5. Electron micrographs of culture-derived platelets(A,B) and plasma-derived platelets (C). (A) A culture-derived platelet with a smooth contour, resembling an inactivated platelet. (B)A culture-derived plateletwith ruffledcontour, resembling an activated platelet. (Cl A plasmaderived (normal) plateletwith activated morphology. Allpanels contain images of the same magnification (bar, l pm). From www.bloodjournal.org by guest on February 6, 2015. For personal use only. 408 CH01 ET AL Fig 6. Cukure-derived platelets aggregate in response t o thrombin or ADP/fibrinogen. Phase micrographs of cukurederived platelets before agonist addition (A), after thrombin addition(C), and after ADPlfibrinogen addition (E). Plasma-derivedplatelets before agonist addition (B), after thrombin addition (D), and after ADP addition (F). All panels contain images of the same magnification (reference bars in B and F, 20 pm). structural characteristic by which platelets are defined..'".'' Figure 2 demonstrates the presence of microtubule coils within proplatelets. The diameter of these microtubule coils iswithin the same range as those within plasma-derived platelets (approximately 3 to 5 pm). Some proplatelets displayed microtubule coils along the processes, whereas some displayed microtubule coils only at the tips (Fig 2A and B). Some proplatelet tips were rounded with a microtubule coil enclosed and some were not, in which case the microtubule strands ended in a fashion Fig Ultrastructure Similarities Between Proplatelets and Platelets Electron micrographs demonstrate ultrastructural similarities between proplatelets and plasma-derived platelets. Pro- From www.bloodjournal.org by guest on February 6, 2015. For personal use only. 409 FUNCTIONAL CULTURE-DERIVED HUMAN PLATELETS ments in the culture supernatant was approximately 3.2 X 106/mL(range, 1.4 X 106/mLto 5.3 X 106/mL;n = 10). Table 1. Platelet Aggregation is Blocked With Anti-GPllbllla Antibody Aaareaate Diameter (urn) Culture-derived platelets lsotype control GPllbllla antibody Plasma-derived platelets lsotype control GPllbllla antibody 0-10 11-20 21-30 31-40 41-50 250 0 0 8 22 0 19 0 8 0 14 0 19 0 27 0 15 0 4 0 0 0 6 0 0 Specific inhibition of platelet aggregation by anti-GPllbllla antibody. Gel-filtered culture- and plasma-derived plateletswere incubated with 50 pg/mL of either isotype control antibody (anti-CD34) or anti-GPllbllla antibody in the presence ofhuman fibrinogen and ADP asdetailed in Materials and Methods. From each population, 20,000 platelets were aliquoted into microtiter wells, where they formed a monolayer suspension. Platelet aggregate diameters were measured from video prints. platelets contain electron-dense alpha granules (Fig 3A and B) similar to those found in normal platelets (Fig 3C). In the proplatelet sample shown in Fig 3B, platelet-sized areas defined by constrictions (arrows) can be seen that are similar in size (approximately 3 to 5 pm) and morphologic appearance to plasma-derived platelets. Observation of Platelet-Size Fragments Examination of proplatelet cultures showed the presence of platelet-sized fragments (putative culture-derived platelets; Fig 4). These fragments were observed in every proplatelet culture examined. Generally, these particles were first observed within 24 hours after proplatelet development. If the culture vessel was handled gently to minimize agitation, the putative culture-derived platelets could be seen lined-up, as if they had just undergone the transition from proplatelets to platelets (arrow, Fig 4A). Sometimes, two or three putative culture-derived platelets were seen linked together by thin cytoplasmic bridges (arrow, Fig 4B). The mean platelet volume (MPV) of the putative culture-derived platelets was similar to that ofnormal platelets (6 to 10 H L ) , according ~~ to analyses with an electronic cell counter (data not shown). The concentration of platelet-sized frag- Fig 7. P-selectin expression on thrombin-stimulated platelets. Culturederived(AI or plasma-derived (B1 platelets were fixed before (unshadedl or after (shaded) 60 secondsof activation with 1 U/ mL thrombin. Platelets were incubated with anti-Pselectin (anti-CDWI antibody followed by goat antimouseFlTC. Ultrastructural Similarities Between Culture-Derived and Plasma-Derived Platelets Putative culture-derived platelets were examined by transmission electron microscopy. The size and ultrastructural composition of the culture-derived fragments (Fig 5A and B) were virtually identical to those of normal platelets derived from plasma (Fig 5C). The diameter of the culturederived platelets was approximately 3 pm. A culture-derived platelet shown inFig5A displays a smooth contour and spherical shape. Another culture-derived platelet shown in Fig 5B displays a ruffled and irregular contour, similar in shape to the plasma-derived platelet shown in Fig 5C. The activated appearance of the platelets in Fig 5B and C is most likely due to centrifugation before fixation. In addition to the similarities in size and granular components of culturederived and plasma-derived platelets, careful examinations of culture-derived platelet micrographs showed circumferential microtubule strands, although they were not as prominent as those found in plasma-derived platelets. Sometimes microfibrils were also observed in culture-derived platelets. Culture-Derived Platelets Aggregate in Response to Thrombin and ADP/Fibrinogen The function of culture-derived platelets was investigated. Culture-derived or plasma-derived platelets incubated in the absence of agonists do not aggregate, as shown in Fig 6A and B, respectively. After addition of the strong platelet agonist thrombin, both populations of platelets aggregated (Fig 6C and D). Because of the concern that the cytocentrifugation involved in the assay may have caused the aggregation, all these slides were examined with extreme caution, and the aggregates were found to be unique to platelet preparations treated with thrombin. Addition of the weak platelet agonist ADP together with fibrinogen also induced aggregation of gel-filtered, culture-derived and plasma-derived platelets (Fig 6E and F). ADP/fibrinogen-induced aggregation was dependent on an interaction between fibrinogen and the fibrinogen receptor as aggregation could be blocked with a neutralizing anti-GPIIbIIIa antibody. Culture- and plasmaderived platelets incubated with either anti-GPIIbIIIa or an isotype-control antibody (anti-CD34) were stimulated with m From www.bloodjournal.org by guest on February 6, 2015. For personal use only. CH01 ET AL Fig 8. Activation-dependent GPlbllla expression on ADP-dmulated pletelets. Culturederived (AI or plaame-derived (B1 platelets were incubated with PAC1-FKCantibody ss eitherrestingpopulations (unshadd) or as activatedpopulations (shadedd). Platelets were activated with 40 pmol/L ADP for 15 minutes. ADP and fibrinogen. Whereas both culture-derived and plasma-derived platelets aggregated in the presence of the control antibody, neither population aggregated in the presence of anti-GPIIbIIIa (Table I). Expression of Activation-Dependent Antigens on CultureDerived Platelets Normal functional platelets, when activated, express certain cell surface antigens not associated with resting platelets. Two antigens of this type are P-selectin (CD62, GMP-140, or PADGEM)37*49 and the functional fibrinogen receptor (activated GPIIbIIIa).36~50 P-selectin, present on the alpha granules of resting platelets, becomes mobilized to the plasma membrane after activation. As shown in Fig 7A, P-selectin (CD62) expression on culture-derived platelets increased significantly after activation with thrombin. The percentage of specific CD62' platelets increased from 15.2% to 61.5% with activation. Figure 7B shows an identical experiment performed with plasma-derived platelets where the percentage of specific CD62' platelets increased from 20.6% to 58.6% with activation. The presence of a CD62+ subpopulation of resting platelets is attributed to accidental activation occurring during the platelet isolation procedures. The platelet surface protein complex GPIIbIIIa changes conformation after platelet activation in its conversion to a functional fibrinogen receptor. PAC 1, a MoAb against the activated form of GPIIbIIIa, has been previously described to be specific for activated platelet^.^^'^^ As shown in Fig SA, PAC-1labeling of culture-derived platelets increased significantly after activation with ADP. The percentage of specific PAC1 platelets increased from 7.04% to 95.1 % with activation. When this experiment was performed with plasma-derived platelets (Fig 8B), the percentage of specific PAC-1+ platelets increased from 2.13% to 97.9% with activation. + DISCUSSION This report describes an in vitro culture system in which to study human megakaryocyte development and platelet formation. CD34+ megakaryocyte progenitors are selected from leukapheresis units that are now commonly prepared by manyblood banks. The number of CD34' cells recovered per leukapheresis unit is sufficient to generate as many as 3 X IO6 megakaryocytes in culture. This fact, along with the observations that megakaryocytes generated in culture from peripheral blood progenitor cells are morphologically, antigenically, and endomitotically normal,51make this an ideal system for the study of in vitro human platelet formation. Human megakaryocytes will spontaneously form proplatelet structures in culture. While normal human plasma enhances the phenomenon, it is not required. Matrigel has no apparent effect on the frequency or the rate of in vitro proplatelet development. These data suggest that direct interactions between megakaryocytes and the extracellular matrix are perhaps not necessary for proplatelet development, in agreement with somez3but not al119*25*26 reports. The developmental point at which megakaryocytes become capable of spontaneously producing proplatelets is not known but obviously occurs within the time frame of the culture system. Although at any given time 40% to45% of the megakaryocytes display proplatelets, the possibility remains that all the megakaryocytes could eventually do so upon reaching the critical maturation point. One explanation for less than 100% of the megakaryocytes developing proplatelets at any given time may be due to the wide range in cytoplasmic and nuclear maturity displayed by the culturegenerated megakaryocytes. Megakaryocyte differentiation is not synchronous in culture, despite the fact that the starting cell population is enriched for CD34+ cells. Another explanation maybe related to the use of CATCH buffer. The metabolic inhibitors adenosine and theophylline inthe buffer, necessary to maintain maximum megakaryocyte integrity:3 may differentially inhibit proplatelet development depending on cell cycle or maturation stages of the megakaryocytes. Microtubules are essential structural elements of proplatelets and of platelets. In proplatelets, longitudinal microtubules may guide or direct the membrane and organelle flow of the developing processes.12~1s~38~5*~53 In platelets, microtubule coils provide structural support and may also harbor microtubule-associated proteins important for platelet function, analogous to the situation found in neurites." In this report both longitudinal microtubules and circumferential From www.bloodjournal.org by guest on February 6, 2015. For personal use only. 41 1 FUNCTIONALCULTURE-DERIVED HUMAN PLATELETS microtubule coils are observed in human proplatelets. Other investigators using rodent systems have not observed microtubule coils in proplatelets and have proposed that the structures may not form until after platelet fragmentation." The differences in these results may be due to species variation or to the possibility that the described culture system allows for additional maturation of proplatelets during the culture period. Human proplatelets also display the platelet antigens GpIb and 11t,41.55-57 and electron-dense alpha granules containing fibrin~gen!~"*~~*~~ Taken together, these antigenic and structural data emphasize the platelet-like nature of proplatelets and support the notion that proplatelets may be the structural precursors to platelets. There have been scattered reports suggesting that plateletlike fragments can be found in megakaryocyte cultures. Radley and Hatshom" observed fragments consisting of 2 to 10 linked, putative platelets migrating out of mouse marrow explants. The presence of platelet strings suggests that platelet release may not occur sequentially from the distal proplatelet tip. More recently, the same group has identified proplatelet-fragments within murine long-term bone marrow cultures. The presence of fragments was reported as occumng rarely.B Leven and Yed4also reported fragmentation of guinea pig proplatelets, but only in response to thrombocytopenic rabbit plasma and cytochalasin D in combination. Although elaborate proplatelet-like networks have been seen on cultured human megakaryocytes, evidence of detached platelet-sized particles in culture has not been presented.= This report presents the first formal identification and functional analysis of platelets most likely arising from proplatelet cultures of any species. These are de novo synthesized platelets and not residual platelets from leukapheresis units, as the average culture time before platelets are observed is 14 days. Furthermore, cultured cells are subjected to extensive processing, including Ficoll, counter-current flow elutriation, freeze-thaw, CD34+ selection, and velocity sedimentation. The ultrastructural similarities between culture-derived and normal platelets strongly suggest that the populations are identical. The functional similarities between culture-derived and plasma-derived platelets with respect to thrombin- and ADP-induced aggregations and activationdependent expression of P-selectin and activated GPIIbIIIa also fully support this notion. There are approximately 240 platelets recovered from these cultures for every proplateletbearing megakaryocyte. This ratio is certainly within the theoretical range proposed by othersm"* and is possibly an underestimate of the fragmentation capacity of megakaryocytes. Uncharacterized platelet-shedding factors or rheostatic shear forces may be necessary to increase the rate and/or number of platelets observed. It will be of interest to combine this megakaryocyte culture system with one of the emerging artificial capillary culture systems to test this idea. ACKNOWLEDGMENT We thank Dr F. Naeim, UCLA Medical Center, for expert morphologic differentiations of megakaryocyte cultures; Dr Sanford Shattil (University of Pennsylvania, Philadelphia, PA) for PAC1FITC antibody; S. Richardson for excellent technical assistance in transmission electron microscopy, and UCSB Biological Sciences and UCSB Neuroscience Research Institute (University of California, Santa Barbara, CA) for the use of the electron microscope facilities. We additionally thank Drs Joan Egrie and Eric Mazur for critical reading of the manuscript. REFERENCES 1. Wright J H The origin and nature of blood plates. Boston Med Surg J 154643,1906 2. Wright JH: Histogenesis of the bloodplatelets.JMorpho1 21:263, 1910 3. Thiery JB, Bessis M: La genese des plaquettes a partir des megacaryocytes observes sur la cellule vivante. Acad Sci 242:290, 1956 4. Thiery JB, Bessis M: Mecanisme de la plaqettogenese. Etude in vitro par la microcinematographie. Rev Hemat 2162, 1956 5. Yamada F: The fine structure of the megakaryocyte in the mouse spleen. Acta Anat 29:267, 1957 6. Behnke 0 An electron microscope study of megakaryocytes of rat bone marrow. I. The development of the demarcation membrane system and the platelet surface coat. J Ultrastruct Res 24:412, 1968 7. Behnke 0: An electron microscope study of the rat megakaryocyte. 11. Some aspects of platelet release and microtubules. J U1trastruct Res 26:111, 1969 8. Zucker-Franklin D, Petursson S : Thrombocytopoiesis: Analysis by membrane tracer and freeze fracture studies on fresh human and cultured mouse megakaryocytes. J Cell Biol 99:390, 1984 9. Becker RP, De Bruyn PPH: The transmural passage of blood cells into myeloid sinusoids and the entry of platelets into the sinusoidal circulation: A scanning microscopic investigation. Am J Anat 145:183, 1976 10. Radley JM, Scurfield G: The mechanism of platelet release. Blood 56:996, 1980 11. Scurfield G, Radley JM: Aspects of platelet formation and release. Am J Hematol 10285, 1981 12. Radley JM: Ultrastructural aspects of platelet production. Prog Clin Biol Res 215:387, 1986 13. Handagama PJ, Feldman BF, Jain NC, Farver TB, Kono CS: In vitro platelet release by rat megakaryocytes: Effect of metabolic inhibitors and cytoskeletal disrupting agents. Am J Vet Res 48:1142, 1987 14. Leven RM, Yee MK: Megakaryocyte morphogenesis stimulated in vitro by whole and partially fractionated thrombocytopenic plasma: A model system for the study of platelet formation. Blood 69:1046, 1987 15. Tablin F, Castro M, Leven RM: Blood platelet formation in vitro. The role of the cytoskeleton in megakaryocyte fragmentation. J Cell Sci 97:59, 1990 16. Lichtman MA, Chamberlain JK, Simon W, Santillo PA: Parasinusoidal location of megakaryocytes in marrow: A determinant of platelet release. Am J Hematol 4303, 1978 17. Tavassoli M, Aoki M Migration of entire megakaryocytes through the marrow-blood barrier. Br J Haematol48:25, 1981 18. Handagama PJ, Jain NC, Feldman BF, Farver TB, Kono CS: In vitro platelet release by rat megakaryocytes: Effect of heterologous antiplatelet serum. Am J Vet Res 48:1147, 1987 19. Topp K, Tablin F, Levin J: Culture of isolated bovine megakaryocytes on reconstituted basement membrane matrix leads to proplatelet process formation. Blood 76:912, 1990 20. Smith CM 11, Burris SM, White JG: High frequency of elongated platelet forms in guinea pig blood: Ultrastructure and resistance to micropipette aspiration. J Lab Clin Med 115:729, 1990 21. Bessis M: The thrombocytic series, in Masson, Cie (eds): Living Blood Cells and Their Ultrastructure. New York, NY, Springer-Verlag, 1973, p 367 22. Trowbridge EA, Martin JF, Slater DN: Evidence for a theory From www.bloodjournal.org by guest on February 6, 2015. For personal use only. 412 of physical fragmentation of megakaryocytes implying that all platelets are produced in the pulmonary circulation. Thromb Res 28:461, 1982 23. Hunt P, Hokom MM, Wiemann B, Leven RM, Arakawa T: Megakaryocyte proplatelet-like process formation in vitro is inhibited by serum prothrombin, a process which is blocked by matrixbound glycosaminoglycans. Exp Hematol 21:372, 1993 24. Hunt P, Hokom MM, Hornkohl A, Wiemann B, Rohde M: The effect of the platelet-derived glycosaminoglycan serglycin on in vitro proplatelet-like process formation, Exp Hematol 21:1295, 1993 25. Caine YG, Vlodavsky I, Hersh M, Polliack A, Gurfel D, Or R, Levine RF, Eldor A: Adhesion, spreading and fragmentation of human megakaryocytes exposed to subendothelial extracellular matrix: A scanning electron microscopy study. Scanning Electron Microsc 3:1087, 1986 26. Leven RM, Tablin F: Extracellular matrix stimulation of guinea pig megakaryocyte proplatelet formation in vitro is mediated through the vitronectin receptor. Exp Hematol 20: 1316, 1992 27. Radley JM, Hatshorn MA: Megakaryocyte fragments and the microtubule coil. Blood Cells 12:603, 1987 28. Radley JM, Hartshorn MA, Green SL: The response of megakaryocytes with processes to thrombin. Thromb Haemost58:372, 1987 29. Radley JM, Rogerson J, Ellis SL, Hasthorpe S: Megakaryocyte maturation in long-term marrow culture. Exp Hematol 19:1075, 1991 30. An E, Ogata K, Kuriya S , Nomura T: Interleulun-6 and erythropoietin act as direct potentiators and inducers of in vitro cytoplasmic process formation on purified mouse megakaryocytes. Exp Hematol 22149, 1994 31. Leven RM: Megakaryocyte motility and platelet formation. Scanning Microsc 1:1701, 1987 32. Mazur EM, Basilic0 D, Newton JL, Cohen JL, Charland C, Soh1 PA, Narendran A: Isolation of large numbers of enriched human megakaryocytes from liquid cultures of normal peripheral blood progenitor cells. Blood 76: 1171, 1990 32a. Nichol JL, Homkohl AC, Choi ES, Hokom MM, Ponting I, Schuening F W , Hunt P Enrichment and characterization of peripheral blood-derived megakaryocyte progenitors that mature in shortterm liquid culture. Stem Cells 12:494, 1994 33. Levine RF, Fedorko ME: Isolation of intact megakaryocytes from guinea pig femoral bone marrow. Successful harvest made possible with inhibitors of platelet aggregation: Enrichment achieved with a two-step technique. J Cell Biol 69:159, 1976 34. Leven RM, Nachmias VT: Cultured megakaryocytes: Changes inthe cytoskeleton after ADP-induced spreading. J Cell Biol 92:313, 1982 35. Levine RF: The origin, development and regulation of megakaryocytes. Br J Haematol 52: 173, 1982 36. Shattil SJ, Hoxie JA, Cunningham M, Brass LF: Changes in the platelet membrane glycoprotein IIb-IIIa complex during platelet activation. J Biol Chem. 260: 1 1 107, 1985 37. Tschoepe D, Spangenberg P, Esser J, Schwippert B, Kehrel B, Roesen P, Gries FA: Flow-cytometric detection of surface membrane alterations and concomitant changes in the cytoskeletal actin status of activated platelets. Cytometry 11:652, 1990 38. Shattil SJ, Cunningham M, Hoxie JA: Detection of activated platelet in whole blood using activation-dependent monoclonal antibodies and flow cytometry. Blood 70:307, 1987 39. RuanCG, Xi XD, Du XP, Wan HY, Wu X, Li PX, Gu JM: Studies on monoclonal antibodies against human platelets-A monoclonal antibody to human platelet glycoprotein I-SZ-2. Sci Sin 30:404, 1987 40. van Pampus EC, Denkers IA, van Gee1 BJ, Huijgens PC, CH01 ET AL Zevenbergen A, Ossenkoppele GJ, Langenhuijsen MM: Expression of adhesion antigens of human bone marrow megakaryocytes, circulating megakaryocytes and blood platelets. Eur J Haematol 49:122, I992 41. Debili N, Kieffer N, Nakazawa M, Ghichard J, Titeux M, Cramer E, Breton-Gonus J, Vainchenker W: Expression of platelet glycoprotein Ib by cultured human megakaryocytes: Ultrastructural localization and biosynthesis. Blood 76:368, 1990 42. Duperray A, Troesch A, Berthier R, Chgnon E, Frachet P, Uzan G, Marguerie G: Biosynthesis and assembly of platelet GPIIbIIIa in human megakaryocytes: Evidence that assembly between proGPIIb and GPIIIa is a prerequisite for expression of the complex on the cell surface. Blood 74:1603, 1989 43. Bray PF, Leung CS, Shuman MA: Human platelets and megakaryocytes contain alternately spliced glycoprotein IIb mRNAs. J Biol Chem 265:9587, 1990 44. Binnie CG, Lord ST: The fibrinogen sequences that interact with thrombin. Blood 81:3186, 1993 45. Wencel-Drake JD, Painter RG, Zimmerman TS, Ginsberg MH: Ultrastructural localization of human platelet thrombospondin, fibrinogen, fibronectin and von Willebrand factor in frozen thin section. Blood 65:929, 1985 46. Steiner M: Fluorescence studies of platelet tubulin. Biochemistry 19:4492, 1980 47. Behnke 0: Microtubules in disc shaped blood cells. Int Rev Exp Pathol 9:1, 1970 48. Bessis M: Living Blood Cells and Their Ultrastructure. Heidelberg, Germany, Springer-Verlag Berlin, 1973 49. Peng J, Friese P, Heilmann E, George J, Burstein SA, Dale GL: Aged platelets have an impaired response to thrombin as quantitated by P-selectin expression. Blood 83:161, 1994 50. Abrams CS, Ellison N, Budzynski AZ, Shattil SJ: Direct detection of activated platelets and platelet-derived microparticles in humans. Blood 75:128, 1990 5 1. Mazur EM, South K. Human megakaryocyte colony-stimulating factor in sera from aplastic dogs: Partial purification, characterization, and determination of hematopoietic cell lineage specificity. Exp Hematol 13: 1 164, I985 52. Shattil SJ, Budzynski A, Scrutton MC: Epinephrine induces platelet fibrinogen receptor expression, fibrinogen binding, and aggregation in whole blood in the absence of other excitatory agonists. Blood 73: 150, 1989 53. Shroer TA, Kelley RB:In vitro translocation of organelles along microtubules. Cell 40:729, 1985 54. Allen RD, Weiss DG, Hayden JH, Brown DI, Fujiwake H, Simpson M: Gliding movement of and bidirectional transport along single native microtubules from squid axoplasm: Evidence for an active role of microtubules in cytoplasmic transport. J Cell Biol 100:1736, 1985 55. NurdenAT, Caen JP: Membrane glycoproteins andhuman platelet function. Br J Haematol 38:155, 1978 56. Phillips DR, Jennings LK, Edwards HH: Identification of membrane proteins mediating the interaction of human platelets. J Cell Biol 86:77, 1980 57. Nurden AT, Dupuis D, Kunicki TJ, Caen JP: Analysis of the glycoprotein and protein composition of Bernard-Soulier platelets by single and two-dimensional sodium dodecyl sulfate-polyacrylamide gel electrophoresis. J Clin Invest 67:1431, 1981 58. Stenberg PE, Shuman MA, Levine SP, Bainton DF: Redistribution of alpha-granules and their contents in thrombin-stimulated platelets. J Cell Biol 98:748, 1984 59. Fukami MH, Salganikoff L: Human platelet storage organelles: A review. Thromb Haemost 38:963, 1977 60. Kaufman RM, Airo R, Pollack S, Crosby WH: Circulating megakaryocytes and platelet release in the lung. Blood 26:720, 1965 From www.bloodjournal.org by guest on February 6, 2015. For personal use only. FUNCTIONALCULTURE-DERIVED HUMAN PLATELETS 61. Harker LA, Finch CA: Thrombokinetics in man. J Clin Invest 48:963, 1969 62. Tavassoli M: Megakaryocyte-platelet axis and the process of platelet formation and release. Blood 55:537, 1980 63. Trowbridge EA, Martin JF, Slater DN, Kishk YT, Warren CW, Harley PJ, Woodcock B: The origin of platelet count and volume. Clin Phys Physiol Meas 5:145, 1984 64. Trowbridge EA, Harley PJ: A computer model of the random binary sequential division of megakaryocyte cytoplasm to produce platelets. Phys Med Biol 29:1477, 1984 413 65. Trowbridge EA, Slater DN, Kishk YT, Woodcock BW, Martin JF: Platelet production in myocardial infarction and sudden cardiac death. Thromb Haemost 52:167, 1984 66. Crosby WH: Normal platelet numbers. Pulmonary-platelet interactions. Ser Haematol 8:89, 1976 67. Slichter SJ, Harker LA: Thrombocytopenia: Mechanisms and management of defects in platelet production. Clin Haematol 7:523, 1978 68. Stenberg PE, Levin J: Mechanisms of platelet production. Blood Cells 15:23, 1989 From www.bloodjournal.org by guest on February 6, 2015. For personal use only. 1995 85: 402-413 Platelets generated in vitro from proplatelet-displaying human megakaryocytes are functional ES Choi, JL Nichol, MM Hokom, AC Hornkohl and P Hunt Updated information and services can be found at: http://www.bloodjournal.org/content/85/2/402.full.html Articles on similar topics can be found in the following Blood collections Information about reproducing this article in parts or in its entirety may be found online at: http://www.bloodjournal.org/site/misc/rights.xhtml#repub_requests Information about ordering reprints may be found online at: http://www.bloodjournal.org/site/misc/rights.xhtml#reprints Information about subscriptions and ASH membership may be found online at: http://www.bloodjournal.org/site/subscriptions/index.xhtml Blood (print ISSN 0006-4971, online ISSN 1528-0020), is published weekly by the American Society of Hematology, 2021 L St, NW, Suite 900, Washington DC 20036. Copyright 2011 by The American Society of Hematology; all rights reserved.
© Copyright 2026