Scott Syndrome, Characterized by Impaired Transmembrane
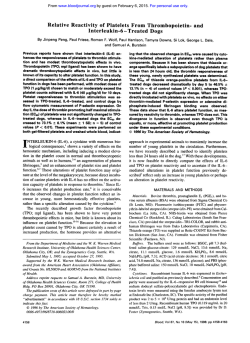
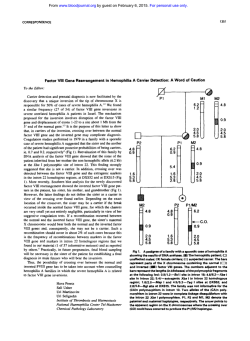
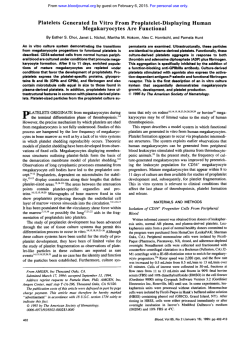
From www.bloodjournal.org by guest on February 6, 2015. For personal use only. Scott Syndrome, Characterized by Impaired Transmembrane Migration of Procoagulant Phosphatidylserine and Hemorrhagic Complications, Is an Inherited Disorder By Florence Toti, Nathalie Satta, Edith Fressinaud, Dominique Meyer, and Jean-Marie Freyssinet An as yet single family with a bleeding historyis shown to Epstein-Barrvirus-infectedBlymphocytes.Thedataare present the characteristic lack of membrane expression of compatible with homozygous status ofthe propositus and procoagulantphospholipidsobserved in Scott syndrome. heterozygousstatusofherchildren. Scott syndrome apLow prothrombin consumption in the serum of the propospears to be transmitted as an autosomal recessive trait reitus, a 71-year-oldwoman, and two of her children was the flecting the deletion or mutation of a putative outward phossole abnormal hemostasis parameter. The degree of expophatidylserine translocase. The detailed knowledge of this sure of procoagulant phospholipids, chiefly phosphatidylser-transporter could have an impact in membrane physiology. 0 1996 by The American Society of Hematology. he. was reduced in stimulated platelets, erythrocytes and T HE COMPLETION OF THE blood coagulation process requires the surface assembly of the characteristic enzyme complexes involving several of the clotting factors.' The exposure of negatively charged phospholipids, chiefly phospatidylserine, sequestered in the inner leaflet of the plasma membrane of resting cells, is a prerequisite for the local concentration of actors playing a fundamental role in the generation of thrombin. Stimulated platelets are thought to be the major source of phosphatidylserine, previously referred to as platelet factor 3. When available at the surface of activated cells or derived fragments, phosphatidylserine acquires a procoagulant character due to its ability to complex vitamin K-dependent factors VII, IX, X, and 11, as well as activated cofactors VI11 and V. The surface amplification potential of such a system is linked to the feedback control exerted by thrombin through retroactivation of cofactors VI11 and V and platelet ~timulation.'~~ Vitamin K antagonists enable efficient prevention of thromboembolic disorders by interfering in the maturation process of vitamin K-dependent clotting factors, resulting in an impaired capacity of the latter to associate with procoagulant phospholipids.' The symmetrical approach consisting in the pharmacologic modulation of the degree of exposure of phosphatidylserine by stimulated platelets has been hampered by the lack of knowledge of the mechanism governing its transmembrane migration. The production of a procoagulant response is certainly not the sole consequence of the loss of the asymmetric distribution of phospholipid species between the two leaflets of the plasma membrane, but physiologic implications in cell types other than blood cells remain poorly understood. Ubiquitous cytodynamic events such as endocytosis or exocytosis are accompanied by the loss of membrane a~ymmetry.~ Membrane fusion of enveloped viruses with target cells is facilitated in the presence of phosphatidyl~erine.~.~ Programmed cell death, apoptosis, essential in many aspects of normal development and occurring in major diseases such as cancer, acquired immunodeficiency syndrome (AIDS), autoimmune disorders, et^,^ results in the release of apoptotic fragments bearing exposed pho~phatidylserine.~.~ Several protective mechanisms could neutralize the pathogenic potential of circulating cell fragments. Phosphatidylserine is a determinant of reticuloendothelial and antiphospholipid antibodies could counteract its procoagulant character." Such antibodies are precisely associated with an increased risk of thrombosis." The availability of procoagulant phospholipids is essential Blood, Vol 87, No 4 (February 15). 1996: pp 1409-1415 for a normal hemostatic response, as clearly shown by the severe to moderate bleeding episodes due to a deficiency of platelet procoagulant activity.l3-I6Several isolated cases were reported, but a unique one has been well documented as Scott syndrome.17 The defect also results in decreased membrane emission of procoagulant vesicles or microparticles.'s It is not restricted to platelets but also affects red blood cells and lymphocytes, suggesting that it reflects a mutation occurring in multiple hematologic lineages.'' The possibility of an inherited disorder transmitted as an autosomal recessive trait was discussed but not confirmed.I4 In a more recent report, Epstein-Barr virus (EBV)-infected B cells from the first case of Scott syndrome were fused with the myeloma cell line UC-LUC, resulting in hybridomas in which the Scott abnormality was corrected. The investigators concluded to possible complementation of aberrant gene(s)." We report here the first characterization of a familial Scott syndrome and confirm that it is a genetic disorder affecting the outward transmembrane migration of phosphatidylserine. PATIENTS AND METHODS Subject selection. The propositus [E51 (Fig l), a 71-year-old woman born from first cousins, suffered from severe to moderate hemorrhagic episodes for a long time, including epistaxis, traumarelated hematoma, bleeding after tooth extractions, and at childbirths. She has been successfully treated using whole blood transfusions. Her older sisters [11-1 and 11-31 died from hemorrhage in childbirth. Her children [III-6 to 111-101, nephews [III-1 and 111-3 to 111-51, and grandchildren [IV-I to IV-201 denied any bleeding tendency. No From theInstitut d'He'matolgoie et Immunologie, Faculte' de Me'decine, Universite'Louis Pasteur,Strasbourg; the Laboratoire d'He'matologie, Institut de Biologie, CHU Hbtel-Dieu, Nantes; and the Unite' I43 INSERM, Hbpital de Bicgtre, Le Kremlin-Bicgtre, France. Submitted August 2, 1995; accepted September 28, 1995. Supported by Grants from the Institut National de la Santd et de la Recherche Me'dicale (CRE93-04-06), the Universite' Louis Pasteur de Strasbourg (Equipe d'acceuil DREDno. 1313), the Fondation pour la Recherche Me'dicale, and the Fondation de France. Address reprint requests to Jean-Marie Freyssinet, DSc, lnstitut d'He'wtologieet Imrnunologie, Faculte' de Mddecine, 4, rue Kirschleger, F-67085 Strasbourg Cedex, France. The publicationcosts of this article were defrayed in part by page charge payment.This article must therefore be hereby marked "advertisement" in accordance with I% U.S.C. section I734 solely to indicate this fact. 0 1996 by The American Society of Hematology. 0006-4971/96/8704-0002$3.00/0 1409 From www.bloodjournal.org by guest on February 6, 2015. For personal use only. TOTI ET AL 1410 I II J 111 IV 2F 1M 3M ZF M ZF other recurrent symptom was reported by any ofthe members of this family. The nature of the study was explained to the patient, one of her sons [ I I M ] , two of her daughters 1111-9 and 111-IO], two ofher grandnieces [IV-l and !V-21 (nephew [Ill-11's daughters), and I O control subjects who gave fully informed consent. Hemosmsis pnrmneters. cell prepomtions. and culture. The hemostasis parameters were determined according to standard routine procedures." For studies performed with cells, blood samples from the propositus, her son [III-S], and hcr daughter [ I l l - I O ] were collected in National Institute of Health (NIH) formula A acid-citratedextrose ( I part anticoagulant:6 parts blood) and immediately processed for platelet"andredblood cell isolation."' Lymphocytcs were isolated under sterile conditions and stored in liquid nitrogen. Infection of B lymphocytes by EBV (EBV B9S8, Marmouset) was performed in RPM1 culture medium containing 20% fetal calf serum (FCS; Life Technologies Inc, Paisley, U K ) in the presence of SO ngl mL cyclosporine and was achieved within 3 weeks. EBV-infected B cells were expanded in standard RPM1 culture medium supplemented with S mmollL HEPES. S% FCS. S 8 Hyclone serum (Hyclone Laboratories Inc. Logan, UT), and 50 nglmL gentamicin. In some experiments, cells were cultured in the presence of recombinant human interleukin-4 (!L-4; 1 nglmL; Promega Corp. Madison, W!) to reduce mortality. Cell mortalitywas estimated by Trypan blue staining (0.1% final concentration). F~tnctioncrldetection of procorrgdnnt phospholipid.7. Procoagulant phospholipid exposure in stimulated cells and derived microparticles was detected using a human prothrombinase assay in which phosphatidylserine promotes the activation of prothombin by factor Xa in the presence of factor Va." Thrombin generated by assembled prothombinase complex was measured using a chromogenic assay as described el~ewhere.'~ Red blood cells, platelets, and EBV-infected lymphocytes were studied at IO7 cellslmL, 7 X IO" cellslmL, and 2 X IO' cellslmL, respectively. The ability of each cell type to expose procoagulant phosphatidylserine was examined after stimulation by 0 . 1 NIH UlmL human cy-thrombin'" + 12 pglmL equine tendon collagen (Hormon-Chemie, Munich, Germany) or S pmollL calcium ionophore A23187 for I O minutes at37°C for platelets, S pmol/L A23 I X7 for 90 minutes at 37°C for red blood cells, S pmol/L A231 87 for I O minutes at 37°C for EBV-infected B cells. in the presence of 2 mmol/L external CaCI2 for each cell type. Red blood cells and EBV-infected B lymphocytes were separated from derived microparticles by centrifugation at I2.000g for 30 seconds before the measurements. In each case. results were compared with the prothrombinase activities developed in samples from healthy volunteers. To assess whether the phosphatidylserine content of any cell type was normal, cells were disrupted by three successive freezinglthawingl sonication steps, and the resulting cell fragment suspensions were used in the prothrombinase assay as described above. Flow c ~ t o m e t ~Analysis ~. of the platelet membrane status was ,M M 1F 1F ?F ,M Fig 1. Pedigreeof the family with Scott syndrome. (Solid symbols1individualswith bleedingdisorders and elevated residualserum prothrombin (measuredonly in the propositus111-51): (dotted symbok) individuals with elevated residualserumprothrombin (measured only insubjects 1111-81, 1111-91. and 1111-101). Arrowsindicateindividualsexamined in the whole study. performed using annexin V as a protein probe of phosphatidylserine Annexin V was purified from human placenta and exp"ure,Z".'l.''.~h conjugated to fluorcscein isothiocyanatc (FITC), as alrcady described." Ionophore-stimulated (see above) and nonstimulated cell suspensions were incubated with S pglmL annexin V"'"' for IO minutes at room temperature in the presence of 0.5 mmollL calcium before data acquisition using a BectonDickinsonflow cytometer (Becton Dickinson. San Jose, CA). Parameters weresetto assess phosphatidylserine exposure evidenced by annexin V""' binding andrecordedon FLI Huorescencc scale, simultaneously for cells and derived microparticles that were distinguished according to size (forward light scatter). For each samplc. 10.000 events were recorded and further analyzed in the appropriate gate delineated on dot plots. as previously described." Analysis of the ability of red blood cells to undergo shape change and membrane vesiculation after stimulation by ionophore (see above) was performed using forward-angle versus right-angle light scatter dot plot representation" of I O . 0 0 0 events per sample. Cytoske/eto/ protein onc11y.vis. Cytoskeletal proteins of ionophore-stimulated and unstimulated platelets were analyzed by polyacrylamide gel electrophoresis in thepresenceofsodiumdodecyl sulphate, as described elsewhere.'' RESULTS Table 1 is a representative example of the various assessments of the hemostasis parameters concerning the propositus [H-S], her daughter [Ill-IO], andherson [111-8], who were investigated in this study (Fig l ) . The only abnormal values are those of serum prothrombintimeand consequently residual serum prothrombin. The patient had 68% of residual prothrombin. whereas the levels of her children was lower, but consistently higher than normal at 7.5% for the daughter and 5.5% for the son. The propositus' other daughter [W91could be examined only once and had 5.5% residual serum prothrombin and no other anomaly. The two grandnieces, nephew [Ill- 11's daughters, had normal hemostasis parameters. In the absence of stimulation, platelets or erythrocytes from the propositus exhibited a low prothrombinase activity. This was also true for control samples, reflecting minimal availability of negatively charged phospholipids for prothrombinase complex assembly in each case. Exposure of procoagulant phospholipids remainedweak after various stimulations of propositus' cells when compared with samples from healthy subjects (Figs 2 and 3). Prothrombinase activities in stimulated propositus' red blood cells and corre- From www.bloodjournal.org by guest on February 6, 2015. For personal use only. INHERITED S C O T SYNDROME U) c 15 141 1 c] UnStd T Thr/Coll Son Controls Propositus Daughter Fig 2. Procoagulant phospholipidexternalization in stimulated platelets from the propositus 111-51 measured by prothrombinase or assay. Platelet suspensions wereeitherunstimulated(UnStd) stimulated by the association of thrombin andcollagen (Thr/Coll; 0.1 NIH UlmL and 0.12 pg/mL final respective concentrations1 for 10 minutes at 37°C or by the calcium ionophore A23187(A23187; 5 pmol/L final concentration) for10 minutes at37°C. Stimulations and prothrombinase activitymeasurements were performed in the presence of 2 and 1 mmol/L external CaCI,, respectively. Data are expropospressed as the mean? SEM; n = 3 for the platelets from the subjects. itus andher offspring, and n = 10 for platelets from control sponding supernatants were 7 to 10 times lower than those measured with control cells. Platelets from the patient’s son and daughter displayed a 35% to 45% reduction, respectively, of prothrombinase activity when compared with control cells after stimulation by calcium ionophore (Fig 2). Such a reduction could have been somewhat underestimated because measurements were performed under drastic activation conditions. Table 1. Assessment of theHemostasis Parameters in the propositus [11-5], Her Son [111-81, and Her Daughter [111-101 Propositus 11-5 Son Daughter 111-8 Ill-l0 Bleeding (min) time 3.30ND ND Platelet count (giga/L) 150-500 237 223 395 Prothrombin time (S) 12-14 11.9 11.9 12.7 33-38 aPlT (S)35 34 38 Serum prothrombin 15.7 15.2 11.8 time ( S ) Residual serum 68 7.5 5.5 prothrombin (%) Coagulation factors 105 72 102 FVlll (%) >l20 ND FV (%) 94 ND FIX (%) ND >l20ND FXll (%) vWF (ristocetin cofactor) (%) 118 50-20090 Fibrinogen 2-4 (g/L) 2.96 3 3.5 Abbreviation: ND, not determined. The defect of phosphatidylserine exposure was more easily evidenced in red blood cells that elicit a delayed response to calcium ionophore.’’ Erythrocytes from the propositus were almost insensitive to ionophore treatment. Stimulated red blood cells from the daughter exhibited about twice as much prothrombinase activity as those of her mother, whereas the son’s cells produced a response of about 60% of normal (Fig 3). Diminished prothrombinase activity was also observed in supernatants of corresponding stimulated red blood cells from the three members of the family, testifying to a reduced ability to shed procoagulant microparticles. Again, the propositus’ cells showed the most pronounced defect. Procoagulant phospholipid exposure occurred at comparable basal levels in nonstimulated control and patient’s EBVinfected B lymphocytes (Fig 4), probably as a result of cell mortality, which was estimated between 10% and 15% in both populations, depending on the culture stage. Mortality could be reduced by about 30%, with concomitant reduction of the same order of basal prothrombinase activity, when cells were cultured in the presence of IL-4 (data not shown). Surprisingly, the mortality of offspring’s nonstimulated EBV-B cells was consistently lower, ranging between 3% and 8%, resulting in lower basal prothrombinase activity. Ionophore treatment of control EBV-B cells was responsible for the development of a substantial phospholipid-dependent procoagulant activity almost equally distributed between cells and microparticles. The overall prothrombinase activity (cell and microparticle-associated) of the stimulated pa- l 0 UnStd RBC SN from UnStd RBC 1 Std RBC SN from Std RBC 0.5 Normal Values 2.30-9.30 0 >25 <5 ND ND 75 50-200 80-120 70-120 80-120 Controls Propositus Daughter Son Fig 3. Procoagulant phospholipid externalizationin calcium iono[11-51, her phore-stimulatedredblood cells fromthepropositus daughter [111-101, and her son [Ill-81 measured b y prothrombinase assay. Thrombin generated in the presence of unstimulated red blood cells (Unstd RBC) and corresponding supernatant (SN from UnStd RBC). Thrombin generated in the presence of stimulated cells (Std RBC) and corresponding supernatant (SN from Std RBC). Cells were stimulated by 5 pmollL calcium ionophore A23187 in the presence of 2 mmol/L externalCaCI, for 90 minutes at37°C. The CaCI2concentration was 1 mrno1lL in the prothrombinase assay. Data are expressed as the mean 2 SEM; n = 4 for cells from the propositus and her offspring, and n = 10 for cells from controlsubjects. From www.bloodjournal.org by guest on February 6, 2015. For personal use only. TOTI ET AL 1412 4- 0 0 UnStd H A23187 h v) 7- her offspring’s cells elicited an intermediate response (Fig 6). The dot plot representation of forward-angle versus rightangle light scatter enabled us to clearly distinguish two populations. Cells showed the highest forward and side scatter signals, whereas derived microparticles had lower ones.’’ Less than 1.5% of total events (cells + debris and/or machine noise) was detected in the microparticle gate in any of unstimulated cell types. With stimulated red blood cells, the proportion of microparticles was, respectively, 19.S%, 5%, IO%, and 8% for the normal subject’s, propositus’, daughter’s, and son’s cells. No difference was noticed in the electrophoretic patterns of cytoskeletal proteins of patient’s and control platelets (data not shown). DISCUSSION Cells MP Cells MP Cells MP Cells MP Controls Propositus Daughter Son Fig 4. Procoagulant phospholipidexternalization in calcium ionophore-stimulated EBV-infected B cellsfrom the propositus [ll-51, her daughter [111-101, and herson[Ill-81measured by prothrombinase assay. Thrombin generated in the presence of unstimulated (UnStd) or ionophore-stimulatedcells (A231871 and corresponding shed microparticles (MP). Stimulation was achieved in the presenceof5 pmol/L ionophore and 2 mmollL external CaCIz for 10 minutes at 37°C. The CaCI, concentrationwas 1 mmollL in the prothrombinase assay. Data ere expressed as the mean 2 SEM; n = 4 for cells from the propositus and her offspring, and n = 10 for control cells. tient’s, daughter’s, and son’s EBV-B cells was, respectively, 2S%, 44%, and 53% that of control cells. These values would be, respectively, 15%,’47%, and 56% if the basal corresponding activities were deduced. Microparticle-associated procoagulant activity was almost unaffected by ionophore treatment of propositus’ cells, whereas in her offspring’s cells it remained lower than half of that of the cells. When any of these EBV-B cells including control cells were disrupted, the overall prothrombinase activity was about twice that induced by ionophore in control cells, showing that the absolute values were similar. Disrupted platelets, red blood cells, and EBV-infected B cells from the propositus and her children yielded the same prothrombinase activity as thatof corresponding control cells treated likewise, showing a normal content of procoagulant phospholipids. Flow cytometry analysis using annexin VFITCallowed us to gather evidence regarding the defective exposure of phosphatidylserine and microparticle shedding bythe patient’s platelets compared with control platelets exceedingly stimulated by calcium ionophore (Fig S). The latter underwent massive phosphatidylserine exposure and membrane vesiculation. The patterns corresponding to the binding of annexin Vmc to stimulated cells and derived microparticles were in accordance with prothrombinase activity measurements (Fig 2). Red blood cells from the patient appeared refractory to shape change and showed reduced vesiculation after treatment with S pmol/L calcium ionophore for 90 minutes at 37°C in the presence of 2 mmoYL external Ca2’, whereas The above results clearly establish close links between the almost total absence of phosphatidylserine exposure byin vitro stimulated platelets from the propositus and her hemorrhagic diathesis. The defect was observed not only with the physiologically relevant agonist combination of thrombin and collagen, but also under more drastic conditions using calcium ionophore. The latter was not able to induce significant phosphatidylserine externalization in patient’s red blood cells when compared with corresponding control cells. The reduction of procoagulant phospholipid exposure was also highly significant in her EBV-infected B cells despite interference of cell mortality. Two of her children could be explored for the same anomaly. The overall phospholipid-dependent procoagulant response did not exceed SO% to SS% of normal with the daughter’s cells, whereas the son’s cells showed a behavior closer to normal but consistently lower. These observations are in agreement with measurements of residual prothrombin in serum and have been confirmed by flow cytometry. It has to be emphasized that residual serum prothrombin is a complex function of the degree of availability of procoagulant lipids in whole blood. This could explain the differences of serum prothrombin time and residual serum prothrombin between the propositus and her children. The absence of bleeding in the offspring might precisely be related to residual serum prothrombin close to normal. In our routine practice, under no circumstance of unexplained hemorrhagic disorder, these parameters were found to be abnormal except in this family. The defect of phosphatidylserine exposure and consecutive reduced membrane vesiculation was further evidenced by the reduced binding of a fluorescent derivative of annexin V used to detect available phosphatidylserine. It has to be pointed out that none of the above defects could be due to abnormal composition of membrane phospholipids because patient’s cell fragments bearing fully scrambled phospholipids produced a phosphatidylserine-dependent procoagulant response identical to that of control cells when lysed likewise. In a first instance, these observations appear compatible with homozygous status of the propositus while her children could be heterozygous with respect to Scott syndrome, which wouldbe transmitted as an autosomal recessive trait. The patient’s sisters can reasonably be considered as homozygous because they died from documented hemorrhage. The From www.bloodjournal.org by guest on February 6, 2015. For personal use only. 1413 INHERITED SCOTT SYNDROME 3Normal + A23187 ; I Propositus + A23187 Fig 5. Flow cytometry analysisofphosphatidylserine externalization and membrane microparticle shedding in calcium ionophore-stimulated platelets from the propositus[L51 and normal subject shown by annexin VFmclabeling. Dot plot representations of platelet suspensions showing size parameters on forward light scatter scale and green fluorescence associated to annexin VFmcbound to phosphatidylserine in cells and microparticles. MP, microparticle gates with the proportion ofshedmicroparticles; A23187,calcium ionophore-stimulated cells.Platelets were stimulated by 5 pmol/L ionophore in the presence of 2 mmollL external CaCI, for 10 minutes at 37°C. Thesepatterns correspond to a single analysis representative of results obtained in four independent experiments performed likewise. b Green fluorescence of bound annexin-VFITC possibility of compound heterozygous status appears improbable because it should have been transmitted to the three sisters. However, it has to be emphasized that such conclusions should be viewed as only partly qualified because the genetic analysis could not be performed due to the absence of candidate gene(s). In subjects born from first cousins, ' / , h of the genome has a homozygous character that implies that at least six or seven subjects of this type have to be examined for localization of mutated gene or regulatory element(s) by mapping homozygous loci. Unfortunately, such a study could not be performed here for obvious reasons. The first experimental evidence that a gene defect can give rise to Scott syndrome was reported recently." Our familial study confirms that it is indeed a genetic disorder. The identification of candidate gene(s) is now the next goal but remains dependent on the feasibility of functional rescue methodology in Scott EBV-B cell lines. The maintenance of the asymmetric distribution of phospholipid species between the two leaflets of the plasma membrane of a variety of cells involves a specific inward transporter of aminophospholipids, chiefly phosphatidylethanolamine andphosphatidylserine:Although the gene coding for this transporter remains to be identified," it is tempting to speculate that aminophospholipid translocase activity is increased in Scott syndrome. This would explain the sustained sequestration of phosphatidylserine in the inner membrane leaflet. However, experiments performed by other investigators who had access to the red blood cells from the above Scott subjects excluded this possibility as the inward phosphatidylserine transport was found normal. In addition, (arbitrary units) once incorporated byred blood cells from the propositus, labeled phosphatidylserine could not be re-externalized (A. Zachowski and J.-C. Sulpice, personal communication, February 28, 1995). Identical preliminary observations were also reported by another group who had access to the cells of the first case of Scott syndrome." The flip-flop or transmembrane migration of phospholipids remains mostly mysterious.'.'' Nevertheless, a phosphatidylcholine translocase has been recently characterized using a gene disruption approach. It is the product of the mdr2 gene belonging to the family of P-glycoprotein multidrug transporters. Its absence leads to liver disease due to the lack of phosphatidylcholine in bile.'" Because aminophospholipid translocase activity appears normal in Scott red blood cells, it seems reasonable to hypothesize that the Scott defect could be due to a mutation affecting a putative outward phosphatidylserine or aminophospholipid translocase. Another possibility would be that aminophospholipid translocase operates as both an inward and outward transporter, because several pumps do, depending on particular regulation. In this case, only the outward function would be impaired. This hypothesis could be explored using cell mutants defective in inward phosphatidylserine transport recently described.3n A more general perspective of the identification of the gene(s) and corresponding product(s) involved in phosphatidylserine or minephospholipid externalization is to assess whether it is a moreubiquitous feature involved in theprocessesregulating communication between cells and their environment under various physiologic or pathologiccircumstances. In this respect, Scott syndrome would be an additional example of the prime From www.bloodjournal.org by guest on February 6, 2015. For personal use only. TOTI ET AL 1414 Control A23187 Normal Propositus . . .*h;. . ' I . ' SSC (Side light Scatter) usefulness of genetic variants for the characterization of as yet unknown physiologic mechanisms. ACKNOWLEDGMENT The authors dedicate this publication to Prof M.-J. Lameu and are grateful to Family M... and Dr P. Roger for their kind cooperation. The expert technical assistance of M.-L. Temen is gratefully acknowledged. We are indebted to Prof D. Hurez (Laboratoire d'lmmunologie, CHU d'Angers) for facilitated access to laboratory equipment for experiments thathadto be performed on site. We express our gratitude to Drs A. Zachowski and J.-C. Sulpice for measurements of aminophospholipid translocase activity. We thank Prof J.-L. Pasquali for helpful advice for EBV infection of B cells, and Dr G.Lombard-Platet and Prof J.-L. Mandel for critical comments. REFERENCES 1. Furie B, Furie BC: Molecular and cellular biology ofblood coagulation. N Engl J Med 326:800, 1992 Fig 6. Flow cytometry analysis of phosphatidylserine externalization and membrane microparticle shedding in calcium ionophore-stimulated erythroIll-51, her daughter [Ill-101, cytes from the propositus her son [111-81, and a normal subject. Dot plot representations of cell suspensions showing size parameters on forward light scatter scale (arbitrary units) versus right-angle scatter. Cells show the highest forward and side scatter signals, whereas derived microparticles have lower ones (see Results for proportions). Stimulation was achieved in thepresence of 5 pmol/L ionophore and2 mmol/L external CaCll for 90 minutes at37°C. These patterns correspond t o a single analysis representative of results obtainedin six independent experiments performed likewise. 2. Zwaal RFA, Comfurius P, Bevers EM: Mechanisms and function of changes in membrane-phospholipid asymmetry in platelets and erythrocytes. Biochem SOCTrans 2 I :248, 1993 3. Mann KG. Nesheim ME, Church WR, Haley P, Krishnaswamy S : Surface-dependent reactions of the vitamin K-dependent enzyme complexes. Blood 7 6 I , 1990 4. Devaux P F Static and dynamic lipid asymmetry in cell membranes. Biochemistry 30:1163, 1991 5. Hoekstra D, Kok JW: Entry mechanisms of enveloped viruses. Implications for fusion of intracellular membranes. BiosciRep 9:273, I989 6. Yamada S , Ohnishi S : Vesicular stomatitis virus bindsand fuses with phospholipid domain on target cell membrane. Biochemistry 25:3703, 1986 7. Thompson CB: Apoptosis in the pathogenesis andtreatment of disease. Science 267:1456, 1995 8. Savill J, Fadok V, Henson P, Haslett C: Phagocyte recognition of cells undergoing apoptosis. Immunol Today 14:131, 1993 9. Koopman G,Reutelingsperger CPM, Kuijten GAM, Keehnen RMJ, Pals ST, van Oers MHJ: Annexin V for flow cytometric detec- From www.bloodjournal.org by guest on February 6, 2015. For personal use only. INHERITED S C O T SYNDROME tion of phosphatidylserine expression on B cells undergoing apoptosis. Blood 84:1415, 1994 10. Allen TM, Williamson P, Schlegel R: Phosphatidylserine as a determinant of reticuloendothelial recognition of liposome models of the erythrocyte surface. Proc Natl Acad Sci USA 85:8067, 1988 11. Galli M, Bevers EM, Comfurius P, Barbui T, Zwaal RFA: Effect of antiphospholipid antibodies on procoagulant activity of activated platelets and platelet-derived microvesicles. Br J Haematol 83:466, 1993 12. Santoro SA: Antiphospholipid antibodies and thrombotic predisposition: Underlying pathogenic mechanisms. Blood 83:2389, 1994 13. Weiss HJ, Vicic W, Lages B, Rogers J: Isolated deficiency of platelet procoagulant activity. Am J Med 67:206, 1979 14. Miletich JP, Kane WH, Hofmann SL, Stanford N, Majerus PW: Deficiency of factor Xa-factor Va binding sites on the platelets of a patient with a bleeding disorder. Blood 54:1015, 1979 15. Rosing J, Bevers EM, Comfurius P, Hemker HC, van Dieijen G, Weiss W,Zwaal RFA: Impaired factor X and prothrombin activation associated with decreased phospholipid exposure in platelets from a patient with a bleeding disorder. Blood 65:1557, 1985 16. Ahmad S S , Rawala-Sheikh R, Ashby B, Walsh PN: Platelet receptor-mediated factor X activation by factor IXa. High-affinity factor IXa receptors induced by factor VI11 are deficient on Platelets in Scott syndrome. J Clin Invest 84:824, 1989 17. Weiss HJ: Scott syndrome: A disorder of platelet procoagulant activity. Semin Hematol 31:312, 1994 18. Sims PJ, Wiedmer T, Esmon CT, Weiss HJ, Shattil SJ: Assembly of the prothrombinase complex is linked to the vesiculation of the platelet plasma membrane. Studies in Scott sydrome: An isolated defect in platelet procoagulant activity. J Biol Chem 264:17049, 1989 19. Bevers EM, Wiedmer T, Comfurius P, Shattil SJ, Weiss HJ, Zwaal RFA, Sims PJ: Defective Caz+-inducedmicrovesiculation and deficient expression of procoagulant activity in erythrocytes ofa patient with a bleeding disorder: A study of the red blood cells of Scott syndrome. Blood 79:380, 1992 20. Kojima H, Newton-Nash D, Weiss HJ, Zhao J, Sims PJ, Wiedmer T Production and characterization of transformed B-lymphocytes expressing the membrane defect of Scott syndrome. J Clin Invest 94:2237, 1994 1415 21. Dachary-Prigent J, Freyssinet JM, Pasquet JM, Canon JC, Nurden A T Annexin V as a probe of aminophospholipid exposure and platelet membrane vesiculation: A flow cytometric study showing a role for free sulfhydryl groups. Blood 81:2554, 1993 22. Connor J, Bucana C, Fidler IJ, Schroit AJ: Differentiationdependent expression of phosphatidylserine in mammalian plasma membranes: Quantitative assessment of outer-leaflet lipid inprothrombinase complex formation. ptoc Natl Acad Sci USA 86:3184, 1989 23. Satta N, Toti F, Feugeas 0, Bohbot A, Dachary-Prigent J, Eschwbge V, Hedman H, Freyssinet JM: Monocyte vesiculation: A mechanism for dissemination of membrane-associated procoagulant activities and adhesion molecules following stimulation by lipopolysaccharide. J Immunol 153:3245, 1994 24. Freyssinet J M , Gauchy J, Cazenave J P : The effect of phospholipids on the activation of protein C by the human thrombinthrombomodulin complex. Biochem J 238:151, 1986 25. Thiagarajan P, Tait JF: Binding of annexin V/placental anticoagulant protein I to platelets. Evidence for phosphatidylserine exposure in the procoagulant response of activated platelets. J Biol Chem 265:17420, 1990 26. Ravanat C, Archipoff G, Beretz A, Freund G, Cazenave JP, Freyssinet JM: Use of annexin V todemonstrate the role of phosphatidylserine exposure in the maintenance of haemostatic balance by endothelial cells. Biochem J 282:7, 1992 27. Auland ME, Roufogalis BD, Devaux PF, Zachowski A: Reconstitution of ATP-dependent aminophospholipid translocation in proteoliposomes. Proc Natl Acad Sci USA 91:10938, 1994 28. Higgins CF: Flip-Flop: The transmembrane translocation of lipids. Cell 79:393, 1994 29. Smit JJM, Schinkel AH, Oude Elferink RPJ, Groen AK, Wagenaar E, van Deemter L, Mol CAAM, Ottenhoff R, van der Lugt NMT,van Roon, MA, van der ValkMA, Offerhaus GJA, Bems MM, Borst P Homozygous disruption of the murine mdr2 P-glycoprotein gene leads to a complete absence of phospholipid from bile and to liver disease. Cell 75:451, 1993 30. Hanada K, Pagano RE: A Chinese hamster ovary cell mutant defective in the non-endocytic uptake of fluorescent analogues of phosphatidylserine: Isolation using a cytosol acidification procedure. J Cell Biol 199793, 1994 From www.bloodjournal.org by guest on February 6, 2015. For personal use only. 1996 87: 1409-1415 Scott syndrome, characterized by impaired transmembrane migration of procoagulant phosphatidylserine and hemorrhagic complications, is an inherited disorder F Toti, N Satta, E Fressinaud, D Meyer and JM Freyssinet Updated information and services can be found at: http://www.bloodjournal.org/content/87/4/1409.full.html Articles on similar topics can be found in the following Blood collections Information about reproducing this article in parts or in its entirety may be found online at: http://www.bloodjournal.org/site/misc/rights.xhtml#repub_requests Information about ordering reprints may be found online at: http://www.bloodjournal.org/site/misc/rights.xhtml#reprints Information about subscriptions and ASH membership may be found online at: http://www.bloodjournal.org/site/subscriptions/index.xhtml Blood (print ISSN 0006-4971, online ISSN 1528-0020), is published weekly by the American Society of Hematology, 2021 L St, NW, Suite 900, Washington DC 20036. Copyright 2011 by The American Society of Hematology; all rights reserved.
© Copyright 2026