Effect of Albumin on the Inhibition of Platelet Aggregation by
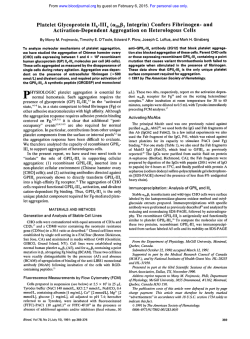
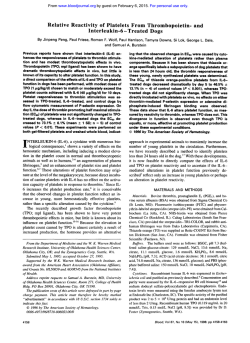
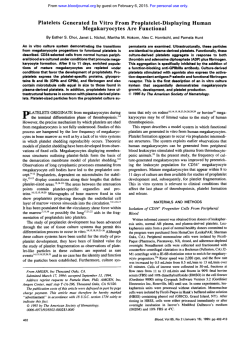
From www.bloodjournal.org by guest on February 6, 2015. For personal use only. Effect of Albumin on the Inhibition of Platelet Aggregation by &Lactam Antibiotics By E.M. Sloand, H.G. Klein, K.B. Pastakia, P. Pierce, and K.N. Prodouz Platelet aggregation and bleeding time abnormalities are reported in patients receiving p-lactam antibiotics (pLAs), although clinical bleeding most frequently occurs in chronically ill, malnourished patients. Although most pLAs bind to serum albumin, the relative influence of bound versus unbound pLAs on platelet function is unknown. We examined the effect of pLAs on the aggregation of gel-filtered platelets from normal subjects and on platelet-rich plasma (PRP) from hypoalbuminemic patients. Therapeutic concentrations of five BIASwere added to normal platelets at different albumin concentrations (1.5 to 4.5 g/dL). Inhibitionof aggregation by the pLAs was inversely proportional to the albumin concentration, and most antibiotic-treated samples showed more than 50% inhibition at albumin levels below 2.0 g/dL. When P -LACTAM ANTIBIOTICS (PLAs)may contribute to bleeding episodes in patients by depleting vitamin K-dependent coagulation factors,’,*interfering with fibrin polymeri~ation,~ or causing defects in platelet f~nction.~.’ Despite well-documented platelet abnormalities in both normal and patient groups receiving PLAs,*.~clinical bleeding primarily occurs in chronically ill and/or malnourished patients. Although platelet defects have been described at therapeutic concentrations for many some antibiotics produce defective platelet function in vitro only at concentrations greatly in excess of those used therapeutically.3,7&12 PLAs reportedly inhibit platelet function by binding to the platelet surface, thereby preventing interaction of platelet agonists with their receptor^.".'^ Bleeding complications in hypoalbuminemic patients receiving PJAs are often associated with abnormal aggregation activity in vitro, suggesting that PLAs may exert an effect on platelet glycoprotein receptors.’’ Although most PLAs bind to albumin as well as to other plasma proteins,’6 the effect of albumin concentration on the PLA inhibition of platelet function has received little attention. We investigated the PLA effect on platelet aggregation in the presence of varying albumin concentrations in an effort to explain the reports of bleeding in hypoalbuminemic patients receiving PLAs. We selected cephalothin, moxalactam, ceftriaxone, cefamandole, and penicillin to investigate PLA-mediated inhibition of platelet aggregation in platelets collected from From the National Heart, Lung, and Blood Institute, and the Department of Transfusion Medicine, National Institutes of Health; the Warren G. Magnuson Clinical Center; the Center for Biologics Evaluation and Research, Food and Drug Administration, Bethesda, MD; and the Georgetown UniversityMedical Center, Washington, DC. Submitted May 22,1991; accepted December IO, 1991. Address reprint requests to E.M. Sloand, MD, NIH Building 31, Room 5A21,9000 Roclcville Pike, Bethesda, MD 20892. The publication costs of this article were defrayed in part by page charge payment. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C. section 1734 solely to indicate this fact. This is a USgovemment work There are no restrictions on its use. 0006-49711921 7908-0019$0.00/0 2022 PRPs from hypoalbuminemic patients were incubated with cephalothin, aggregation was completely inhibited, in contrast to samples from patients with normal albumin levels, and this decreased platelet aggregation was partially restored (25% to 75%) by increasing the albumin concentration above 4.0 g/ dL. Specific binding of [%]-benzylpenicillin to normal platelets decreased proportionately as the albumin concentration increased in the range of 1.0 to 5.0 g/dL. The inhibitory effects of pLAs on platelets in vitro appear to be influencedby albumin concentration.Plasma albumin concentration may influence bleeding in patients receiving BUS. This is a US government work. There are no restrictions on its use. patients with normal albumin levels and from hypoalbuminemic patients. In addition, we used [35S]-benzylpenicillinto study PLA binding to platelets and the effect of albumin on this binding. METHODS AND MATERIALS Platelet sources. Platelets were obtained from three groups of individuals. Group 1 consisted of platelet concentrates from normal blood donors obtained by automated plateletpheresis (Fenwal CS-3OOO; Baxter Health Care, Deerfield, IL). Group 2 consisted of platelet-rich plasma (PRP) samples from selected oncology patients, six with normal serum albumin (range, 3.0 to 4.6 g/dL) and four with low serum albumin levels (range, 2.5 to 2.8 g/dL; mean, 2.6 g/dL), studied to determine the effect of overnight incubation of platelets with cephalothin (200 kg/mL; Eli Lilly, Indianapolis, IN). In group 3, PRPs from patients with low levels of albumin (range, 2.6 to 3.0 g/dL; mean, 2.8 g/dL) receiving PLA were studied to determine the effects of adding human serum albumin in vitro, Two patients with uremia and one with cirrhosis who were receiving cephalothin (1 g six times daily) and one uremic patient receiving 250 mg of cephalothin orally four times daily were compared with one cirrhotic and six uremic patients not receiving PLAs. All patients and normal donors denied ingestion of aspirin, other nonsteroidal anti-inflammatory agents, or other plateletactive drugs for at least 2 weeks before this study. The hematocrits and platelet counts were similar in patients used for comparison (mean hematocrit of 22.5 in hypoalbuminemic patients and a mean of 20.0 in patients with normal albumin). Venous blood was drawn with minimal negative pressure from the antecubital vein of the arm not containing an arteriovenous fistula. Blood was drawn using the double plastic syringe technique and was immediately transferred into siliconized glass tubes at room temperature, containing sodium citrate at 3.8% (vollvol) final concentration. PRP was prepared by centrifuging the citrated blood at 16Og for 15 minutes at room temperature. Measurement of the aggregation response of normalplatelets treated with $ U s . Platelet concentrates obtained from normal individuals were gel-filtered on Sepharose 2B (Pharmacia Fine Chemicals, Piscataway, NJ), as previously described,” and eluted with 3.8 mmol/L HEPES buffer pH 7.35 (Sigma Chemical Co, St Louis, MO), containing NaCl 0.14 mol/L, KCI 2.7 mmol/L, dextrose 1.0 g/L, NaH,PO, 3.8 mmol/L. Samples were adjusted to a platelet count of 2 x 105/pL(Coulter Counter, Model S; Coulter Electronics, Hialeah, FL) and fibrinogen was added (final concentration, 1.5 mg/mL). The albumin level in the gel-filtered platelets, measured as previously described,18was less than 0.4 g/dL. SamBlood, Vol79, No 8 (April 15), 1992: pp 2022-2027 From www.bloodjournal.org by guest on February 6, 2015. For personal use only. 2023 ANTIBIOTIC-MEDIATED PLATELET INHIBITION ples were divided into paired aliquots and albumin levels were adjusted to different levels (1.5 to 4.5 g/dL) by the addition of fatty acid-free human albumin (25 g/dL; Sigma) or albumin for human use (Armour Pharmaceutical, Bluebell, PA). PLAS were added to one of the paired aliquots (at each albumin level) at concentrations equivalent to plasma levels achieved therapeutically: cephalothin, 100 pg/mL; moxalactam, 400 pg/mL; cefamandole, 13 pg/mL (Eli Lilly); ceftriaxone, 250 pg/mL (Roche Pharmaceutical, Nutley, NJ); and penicillin G 10 pg/mL (Squibb and Sons, Inc, Princeton, NJ). The interval between gel filtration and addition of PLA never exceeded 15 minutes. Platelet function was measured by platelet aggregation 15 minutes after BLA addition. Each sample (0.45 mL) was incubated at 37°C for 10 minutes and aggregation was induced by adding 50 ILL of 80 pmol/L adenosine diphosphate (ADP; Sigma) and stirring. The maximum slope of aggregation was determined for duplicate samples and the results were averaged.” Inhibition for each albumin level was calculated as the percent of maximum slope of aggregation of the control sample at the same albumin level, but without PLAs. Aggregation response of platelets from hypoalbumrnemic patients. Thirty milliliters of PRP from nine oncology patients (six with normal albumin and three hypoalbuminemic) was prepared from venous blood collected into a solution of acid-citrate dextrose (15% [vol/vol]) and centrifuged at 160g for 15 minutes at room temperature. Platelet counts ranged from 1.4 to 2.0 x 1@/mL.Cephalothin (in phosphate-buffered saline [PBS], pH 7.4) was added to a sample of PRP at a concentration of 200 kg/mL and an equal volume of PBS was added to a control sample. The PLA-treated and untreated samples were stored overnight in modified PL 732 platelet storage bags (Fenwal; Baxter Health Care) at 22°C with constant agitation. Platelet aggregation was measured as described above. The maximum slope of aggregation in response to 8 Fmol/L ADP was calculated for samples tested in duplicate. In separate experiments, PRP from 10 hypoalbuminemic patients (four of whom were receiving cephalothin) was divided into two aliquots. Fatty acid-free human albumin (25 g/dL in 0.9% NaCI; Sigma) was added to one aliquot to adjust the albumin concentration to approximately 4.0 g/dL. An equal volume of 0.9% NaCl was added to the control aliquots. Platelet aggregation in response to 0.5 p,mol/L ADP was measured as described above. Penicillin brnding experiments. A 15-pL suspension of Apiezon oil A (Biddle Co, Bluebell, PA) and n-butyl phthalate (1:9 vol/vol) together with 4 p L of [35S]-benzylpenicillin(0.28 to 4.0 nmol/L, 27 to 162 pmol/lO’pplatelets; Du Pont Co,Wilmington, DE) in ethanol (final concentration, < O S % ) was added to 200 pL samples of gel-filtered albumin-free platelets obtained from normal individuals?’ Samples were inverted several times, incubated at 37°C for 15 minutes, and then centrifuged at 1,200g for 15 minutes. The supernatant was removed and the tip of the tube containing the pellet was excised. The pellet was solubilized in 500 pL of 1% sodium dodecyl sulfate. Radioactivity was measured after addition of Aquasol (Du Pont Co). Binding specificity was assessed by measuring the displacement of [’5S]-benzylpenicillinby 1,000-fold excess nonradioactive penicillin. Binding experiments were also performed on three gel-filtered plateletpheresis concentrates at different albumin levels. All samples were tested in quadruplicate. RESULTS Aggregation response of normal platelets treated with PLA. Aggregation was decreased significantly in gel-filtered platelets treated with any of the five PLAs tested at albumin concentrations less than 2.5 g/dL in the medium. An example of the relationship of platelet inhibition to albumin l O O r “---f+q 90 80 0 .-C \ ‘t 70. al 6 60 2 5 50 Albumin Levels (g/dL) 4.0 Fig 1. The albumin concentrations of gel-filtered platelets obtained from a normaldonor were adjusted to levels in the range of 1.5 to 4.5 g/dL by the addition of 25 g/dL human albumin; PES was added, where appropriate, to maintain a constant volume. The aggregation responses to 8 pmol/L ADP were determined on duplicate samples for each different albumin level before and 15 minutes after the addition of five different BLAs: (0-0) cephalothin, 100 pg/mL; (A-A)moxalactam, 400 pg/mL; (0-0) ceftriaxone, 250 pg/mL; (e-+) cefamandole, 13 pg/mL; (0-0) penicillin 0, 10 pg/mL for each albumin level. These responses were compared with those of platelets at similar albumin levels but without @LA.Inhibition was calculated as the percent of the maximum slope of aggregation of the control sample at the same albumin level but without PIA. Similar results were obtained when the maximum aggregation at 3 minutes was used as an index of aggregation instead of slope of aggregation. level is seen in Fig 1 when 8 wmol ADP was used as an agonist. The mean inhibition of aggregation for cephalothin in the five different platelet samples was 64% ? 35% for an albumin of 2 g/dL and 0% for an albumin of 4.0 g/dL. For most PLAs tested, platelet aggregation was either slightly affected or similar to the control sample (at the same albumin concentration but without PLA) when albumin levels exceeded 3.0 to 3.5 g/dL. Below this level, the inhibitory effect of PLAs was inversely related to albumin level in all samples. Similar effects were observed in washed platelets when 8 Kmol/L ADP or thrombin (0.1 to 1.0 U/mL) were used as agonists and in gel filtered platelets when collagen and epinephrine were used (Table 1).When Table 1. Effect of Antibiotics on Platelet Aggregation Response Agonistldose Albumin (%) Antibiotic Aggregation Rate I%control) Extent (% control) ~~ Thrombin 0.08 U/mL 0.08 U/mL 0.20U/mL 0.20 U/mL Co IIagen 5 pmol/L 5 kmol/L Epinephrine 50 *mol/L 50 p n o l / L 1.8 2.7 1.8 2.7 2.0 3.0 2.0 4.0 Penicillin 4 mg/mL 4 mg/mL 4 mg/mL 4 mg/mL Cephalothin 100 pg/mL 100 kg/mL Cephalothin 100 kg/mL 100 bg/mL 0 14 94 0 50 70 82 103 88 100 16 100 35 42 100 100 From www.bloodjournal.org by guest on February 6, 2015. For personal use only. 2024 SLOAND ET AL doses of cephalothin, 10-fold in excess of those used therapeutically, were added to gel filtered platelets, all samples showed inhibition of function regardless of albumin level (when ADP [8 pmol/L], collagen [200 pg/mL], or epinephrine were used as agonists). Aggregation response of platelets from hypoalbuminemic patients. Complete inhibition of platelet aggregation in response to 8 pmol/L ADP was achieved when platelets from four hypoalbuminemic individuals were incubated overnight with 200 pg/mL cephalothin (Fig 2B). Little or no inhibition of ADP aggregation (8 pmol/L) occurred in platelets from six patients with albumin levels greater than 3.0 g/dL (Fig 2A). The inhibition exhibited by the platelets in hypoalbuminemic plasma was partially reversible (25% to 75%) when the albumin levels were increased to 4.0 to 4.8 g/dL by the addition of 25 g/dL human albumin. Representative aggregation curves from a single subject are shown in Fig 3. When the albumin concentration of PRP from hypoalbuminemic patients (albumin range, 2.6 to 3.0 g/dL; mean, 2.8 g/dL) receiving cephalothin (1 g every 4 hours) was increased to 4.0 to 4.5 g/dL by the addition of human albumin, the platelet aggregation response to 0.5 pmol/L ADP increased (Fig 4A). The maximum slope of platelet aggregation increased from a mean of 0.72 to 1.6 in patients receiving cephalothin when the albumin level was raised from an average of 2.8 g/dL to 4.2 g/dL. In contrast, the slope of aggregation decreased in PRP samples from patients with hypoalbuminemia who were not receiving PLA (Fig 4B). The maximum slope of aggregation de- B A Hypoalbuminemic Patients Patients with Normal Albumin 25 A c a i a 10 0 1 0 0 " Cephalothin Concentration (pglmll 0 1 0 0 2 0 0 3 0 0 Cephalothin Concentration (pg/ml) Fig 2. Samples of PRP from six patients with normal albumin levels (A) and from four with low levels (B) were split Into two samples and stored overnight after the addition of either cephalothin (200 pg/mL) or an equal volume of PBS in PL 732 platelet storage bags with constant agitation at 22°C. Samples were removed and platelet aggregation in response to 8 pmol/L ADP was determined in duplicate samples. 0 1 2 Minutes 3 Fig 3. A sample of PRP from a hypoalbuminemicpatient (albumin, 2.6) was storedovernight with cephalothin (200 pg/mL). The aggregation response to 8 pnol/L ADP was determined before pLA addition (A), after storage of platelet sample with @LA (B), and after the albumin was raised to 4.2 g/dL in this stored sample by the addition of 25 g/dL fatty acid-free albumin (C). creased from a mean of 1.7 to 1.2 in samples from those individuals not receiving cephalothin. This latter observation is consistent with previous reports of the effect of albumin concentration on platelet a g g r e g a t i ~ n . Similar ~'~~~ effects were obtained by using albumin prepared for human use. Penicillin binding. The binding of [35S]-labeled benzylpenicillin to albumin-free ( < 0.04 g/dL) gel-filtered platelets is shown on the Scatchard plot in Fig 5. Binding was specific and reversible, as indicated by displacement of radiolabeled penicillin by unlabeled penicillin. Saturation was achieved in albumin-free platelets at 130 pmol/108 platelets. Scatchard plot analysis of these data indicates, under these conditions, approximately 4,800 binding sites per platelet with an apparent dissociation constant of 200 nmol/L and an affinity constant of 5 x lo6 L/mol. At a concentration of 54 pmol of benzylpenicillin/108 platelets, binding of penicillin to platelets was increased in samples with lower albumin concentrations, and platelets showed a decrease in binding with increasing albumin concentrations (Fig 6). Similar results were obtained when stabilized albumin prepared for transfusion was substituted for fatty acid-free albumin. Platelets exposed overnight to radiolabeled penicillin continued to show decreased binding of penicillin at higher albumin levels. However, platelets incubated overnight bound less penicillin than those incubated for 15 minutes. This is most likely due to a loss of platelet integrity that occurs after gel filtration and storage in a non-gas-permeable container. DISCUSSION Bleeding episodes observed in patients who receive PLAs have been attributed to platelet dysfunction, hypoprothrombinemia, and the inhibition of fibrin polymerization. Factors that have been implicated in the increased risk of bleeding include thrombocytopenia, uremia, chemother- From www.bloodjournal.org by guest on February 6, 2015. For personal use only. 2025 ANTIBIOTIC-MEDIATED PLATELET INHIBITION A Cephalothin Treated Hypoalbuminemic Patients 3.0 B Untreated Hypoalbuminemic Patients i .014 .012 t \ .OlO[ 3.0 .008 -JX+ . \ U 2.5 2.5 $ 2.0 m 2.0 C 7 m ?! \ ,002 m 8 1.5 1.5 c 0 0 100 200 0 300 400 500 600 700 800 900 Bound (fmolesll08 platelets) 0" 1.o 5 1.0 0.5 0.5 u 1 2 3 4 5 Albumin Level (g/dL) u 1 2 3 4 5 Albumin Level (g/dL) Fig 4. Platelet aggregation responses to 0.5 pmol/L ADP were tested using PRP obtained from four hypoalbuminemic patients (meanalbumin, 2.8 g/dL) receiving cephalothin (1 g every 4 hours) (A) and six hypoalbuminemic patients receiving no antibiotics (B). Samples were split and the albumin levels of one of the pair were adjusted to approximately 4 g/dL; a similar volume of PBS was added to the control sample. Samples of PRP from patients not receiving antibiotics showed decreased aggregation after addition of albumin, a well-described phenomenon.'9 while the aggregation responseof PRP from patients receiving PIASincreased. apy, chronic illness, and malnutrition." The latter two conditions are often accompanied by hypoalbuminemia. Although serum albumin concentration influences the action of many drugs in vivo," no relationship between albumin concentration and @LA-inducedplatelet dysfunction has been reported. In this study, the degree of inhibition of aggregation of gel-filtered platelets by @LAswas shown to be inversely related to albumin levels at concentrations below approximately 3.5 g/dL. This inhibition of function parallels the increased binding of radiolabeled penicillin to platelets at declining albumin levels. Platelet aggregation in patients with low albumin levels was inhibited after an overnight incubation with cephalothin (200 pg/mL), while platelets from patients with normal albumin levels exhibited no such inhibition. This inhibition of @LA-treated platelets was partially reversible after albumin levels were returned to normal by the addition of exogenous albumin. In this study, platelets bound to the antibiotic in a specific manner and the amount of binding was inversely related to the albumin concentration. The protective effect of albumin is most likely a function of the avid binding of antibiotics to and the consequent depletion of free PLA available to the platelets. The binding of albumin Fig 5. The binding of [a6S]-benzylpenicillinto samples of gelfiltered, albumin-free platelets from two donors was determined as previously described for concentrations of benzylpenicillin of 27 pmol through 162 pmol/ lo" platelets. Saturation was previously determined to have been achieved a t 130 pmol/lo" platelets. A Scatchard analysis is presented. Nonspecific binding was determined by the addition of 1,000-fold excess unlabeled benzylpenicillin. A total of 4,800 sites per platelet were seen with an apparent dissociation constant of 200 nmol/L and an affinity constant of 5 x lO'L/mol. to the antibiotic is reversible and drug molecules are in constant equilibrium between the bound and unbound ~ t a t e . ~For ' penicillin, one molecule of drug binds to one molecule of albumin.%When concentrations of drug exceed the amounts that can be bound to albumin, or when concentrations of albumin decline, the levels of free unbound drug increase. Although it is clear that antibiotic bound to albumin has no antimicrobial a~tivity?~*~' the relationship of protein binding to other drug-related actions has not been explored. All PLAs used in this study v) 8E 0.4 0.2 0 0 1 2 3 4 5 6 Albumin (g/dL) Fig 6. The effect of albumin concentration on the binding of ["SI-benzylpenicillin was measured for three different gel-filtered plateletpheresis concentrates. Binding of benzylpenicillin at each albumin level was measured in quadruplicate for each sample using a concentration of 54 pmol of benzylpenicillin/lV platelets. Results were averaged and plotted using linear regression analysis. The error bars representthe standard error of the mean. From www.bloodjournal.org by guest on February 6, 2015. For personal use only. 2026 SLOAND ET AL exhibit significant binding to p r ~ t e i n ,and ~ ~ the . ~ ~inhibition of platelet function by each PLA was blocked by albumin in a similar manner. It is likely that PLAs exert their inhibitory effect by interfering with agonist interaction with platelet surface receptor^.'^^'^ This mechanism is supported by evidence that binding of an a-adrenergic antagonist, (3H)dihydroergocryptine, to platelet adrenergic receptors is reduced twofold, and (I4C)serotonin release is completely blocked after incubation of platelets with PLAs.I3 Evidence supporting reversible PLA binding to the platelet surface can be found in reports that platelet function returns to normal after exposed platelets are resuspended in PLA-free In our storage studies, in which platelets were stored under standard blood banking conditions, but in the presence of a therapeutic concentration of cephalothin, antibiotic-mediated platelet dysfunction was at least partially reversed by the addition of albumin. However, irreversible binding of radiolabeled penicillin to platelets and irreversible inhibition of platelet function after prolonged exposure to very high doses of penicillin (10 to 20 mmol/L) have been reported.” Using similar conditions, we found that 24 hours of exposure to a high dose of penicillin G (5.4 mmol/L) in the presence of lowered albumin levels (1.27 to 1.45 g/dL; average, 1.36 g/L) impaired the aggregation response of platelets to thrombin even after removal of the antibiotic by washing, but no structural changes were observed in glycoprotein Ib or IIb by polyacrylamide gel electrophoresis and immunoblotting (data not shown). This finding is consistent with the report that in rat platelets treated with a variety of P U S , the loss of platelet function does not correlate with structural changes in surface glycoprotein^.^' This irreversible inhibition of platelet function seen at higher doses of penicillin probably is caused by a different mechanism of platelet membrane damage from the one responsible for the reversible inhibition seen at lower doses. Our observation that inhibition of platelet aggregation by PLAs is inversely related to the albumin level suggests that albumin-bound antibiotic is unable to bind to platelets, or does so with less affinity than does unbound antibiotic. While our experiments do not directly address PLAinduced bleeding, we suspect that the increased frequency of bleeding reported in individuals with chronic illness who are treated with PLAs may be related to low albumin concentration. Our observations may further explain why PLA administration to normal subjects is rarely associated with platelet dysfunction or bleeding. REFERENCES 1. Sattler FR, Weitekamp MR, Ballard JO: Potential for bleeding with the new beta-lactam antibiotics. Ann Intern Med 105:924, 1986 2. Pineo GF, Gallus AS, Hirsh J: Unexpected vitamin K deficiency in hospitalized patients. Can Med Assoc J 109:880,1973 3. Johnson H, Niklasson PM: Effects of some antibiotics on platelet function in vitro and in vivo. Thromb Res 11:237, 1977 4. George JN, Shattil SJ: The clinical importance of acquired abnormalities of platelet function. N Engl J Med 324:27, 1991 5. Agnelli G, Guerciolini R, Grasselli S, Menichetti F, Pauluzzi S, Nenci GG, Del Favero A Effects of the moxalactam antibiotic aztreonam on platelet function and blood coagulation. Chemotherapy 33:9,1987 6. Uchida K, Kakushi H, Shike T Effect of latamoxef (moxalactam) and its related compounds on platelet aggregation in vitroStructure activity relationships. Thromb Res 47:215, 1987 7. Fletcher C, Pearson C, Choi SC, Duma RJ, Evans HJ, Qureshi GD: In vitro comparison of antiplatelet effects of p-lactam penicillins. J Lab Clin Med 108:217,1986 8. Bang NU, Tessler SS, Heidenreich RO, Marks CA, Mattler LE: Effects of moxalactam on blood coagulation and platelet function. Rev Infect Dis 4:S546, 1982 9. Gentry LO, Jemsek JG, Natelson E A Effects of sodium piperacillin on platelet function in normal volunteers. Antimicrob Agents Chemother 19532, 1981 10. Ballard JO, Barnes SG, Sattler FR: Comparison of the effects of mezlocillin, carbenicillin, and placebo on normal hemostasis. Antimicrobial Agents Chemother 25:2,1984 11. Brown CH, Natelson EA, Bradshaw W, Temple WW, Alfrey CP: The hemostatic defect produced by carbenicillin. N Engl J Med 291:6,1974 12. Burroughs SF, Johnson GJ: P-Lactam antibiotic-induced platelet dysfunction: Evidence for irreversible inhibition of platelet activation in vitro after prolonged exposure to penicillin. Blood 75:1473, 1990 13. Cazenave JP, Guccione MA, Packham MA, Mustard JF: Effects of cephalothin and penicillin G on platelet function in vitro. Br J Hematol35:135,1977 14. Mihara S, Fujimoto T, Okabayashi T: Suppression by betalactam antibiotics of thromboxane A2 generation and arachidonic acid release in rabbit platelets in vitro. Thromb Res 44:265,1986 15. Shattil SJ, Bennett JS, McDonough M, Turnbull J: Carbenicillin and penicillin G inhibit platelet function in vitro by impairing the interaction of agonists with the platelet surface. J Clin Invest 65:329,1980 16. Barre J, Tillement JP: Protein binding of antimicrobials: Questions to be answered in focus on coagulase-negative staphylococci, in Phillips I (ed): Focus on Coagulase Negative Staphylococci. New York, NY,Royal Society of Medicine Services, 1989, p 81 17. Timmons S, Hawiger J: Separation of human platelets from plasma proteins including factor VIIIwp by a combined albumin gradient-gel filtration method using hepes buffer. Thromb Res 12:297,1978 18. Savoy J, Hammond JE: Measurement of proteins in biological fluids, in Sonnenwirth AC,’Jarett S (eds): Gradwohl’s Clinical Laboratoly Methods and Diagnosis. St Louis, MO, Mosby, 1980, p 262 19. Weiss H: Abnormalities of factor VI11 and platelet aggregation: Use of ristocetin in diagnosing von-Willebrand syndrome. Blood 45:403,1975 20. Nesheim ME, Pittman DD, Wang JH, Slonosky D, Giles AR, Kaufman RJ: The binding of 35S-labeledrecombinant factor VI11 to activated and unactivated platelets. J Biol Chem 263:16467, 1988 21. Sloand EM, Bern MM, Kaldany A Effect on platelet function of hypoalbuminemia in peritoneal dialysis. Thromb Res 44:419,1986 22. Purdon AD, Rao AK: Interaction of albumin, arachidonic acid and prostanoids in platelets. Prostaglandins leukotrienes and essential fatty acids. 35:213,1989 From www.bloodjournal.org by guest on February 6, 2015. For personal use only. ANTIBIOTIC-MEDIATEDPLATELET INHIBITION 23. Fine KM, Ashbrood PC, Brigden LP, Maldonado JE, Didisheim P Gel-filtered human platelets: Ultrastructure, function, and role of proteins in inhibition of aggregation by aspirin. Am J Pathol841,1976 24. Fass RJ, Copelan EA, Brandt JT, Moeschberger ML, Ashton JJ: Platelet-mediated bleeding caused by broad-spectrum penicillins. J Infect Dis 1512242,1987 25. Benet LZ, Mitchell JR, Sheiner LB: Pharmacokinetics: The dynamics of drug absorption, distribution and elimination, in Gilman AC, Rall TW,Nies AS, Taylor P, Gelman L, Rall T (eds): The Pharmacological Basis of Therapeutics. New York, NY, Pergamon, 1990, p 11 26. Wise R: Protein binding of p-lactams: The effects on activity and pharmacology particularly tissue penetration. I. J Antimicrob Chemother 121,1983 2027 27. Wise R Protein binding of p-lactams: The effects on activity and pharmacology particularly tissue penetration. 11. J Antimicrob Chemother 12105,1983 28. Barza M, Vine H, Weinstein L: Reversibility of protein binding of penicillins: An in vitro study employing a rapid defiltration process. Antimicrobial Agents Chemother 1:427,1972 29. Robinson G, Sutherland R: The binding of antibiotics to serum proteins. Br J Pharmacol25:638,1965 30. Rolinson G N The significance of protein binding of antibiotics in antibacterial chemotherapy.J Antimicrob Chemother 6:311, 1980 31. Anta H, Nakano T, Terawaki A Influence of p-lactam antibiotics on platelets. 1. In vivo effects of latamoxef and related p-lactam antibiotics on membrane proteins and glycoproteins of rat platelets. J Pharmacobiodyn 9896,1986 From www.bloodjournal.org by guest on February 6, 2015. For personal use only. 1992 79: 2022-2027 Effect of albumin on the inhibition of platelet aggregation by betalactam antibiotics EM Sloand, HG Klein, KB Pastakia, P Pierce and KN Prodouz Updated information and services can be found at: http://www.bloodjournal.org/content/79/8/2022.full.html Articles on similar topics can be found in the following Blood collections Information about reproducing this article in parts or in its entirety may be found online at: http://www.bloodjournal.org/site/misc/rights.xhtml#repub_requests Information about ordering reprints may be found online at: http://www.bloodjournal.org/site/misc/rights.xhtml#reprints Information about subscriptions and ASH membership may be found online at: http://www.bloodjournal.org/site/subscriptions/index.xhtml Blood (print ISSN 0006-4971, online ISSN 1528-0020), is published weekly by the American Society of Hematology, 2021 L St, NW, Suite 900, Washington DC 20036. Copyright 2011 by The American Society of Hematology; all rights reserved.
© Copyright 2026