Prostaglandin E2 potentiates platelet aggregation
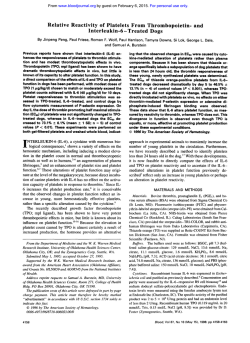
From www.bloodjournal.org by guest on February 6, 2015. For personal use only. Prostaglandin E, Potentiates Platelet Aggregation by Priming Protein Kinase C By Roberta Vezza, Rita Roberti, Giuseppe Giorgio Nenci, and Paolo Gresele Prostaglandin E, (PGE,) is produced by activated platelets and by several other cells, including capillary endothelial cells. PGE, exerts a dual effect on platelet aggregation: inhibitory, at high, supraphysiologic concentrations, and potentiating, at low concentrations. No information exists on the biochemical mechanisms through which PGE, exerts its proaggregatory effect on human platelets. We have evaluated the activity of PGE, on human platelets and have analyzed the second messenger pathways involved. PGE, (5 t o 500 nmol/L) significantly enhanced aggregation induced by subthreshold concentrations of U46619, thrombin, adenosine diphosphate (ADP), and phorbol 12-myristate 13-acetate (PMA) without simultaneously increasing calcium transients. At a high concentration (50 pmol/L), PGE, inhibited both aggregation and calcium movements. PGE, (5 to 500 nmol/L) significantly enhanced secretion of &thromboglobulin (j3TG) and adenosine triphosphate from U46619- and ADP-stimulated platelets, but it did not affect platelet shape change. PGE, also increased the binding of radiolabeled fibrinogen to the platelet surface and increased the phosphorylation of the 47-kD protein in 32Plabeled platelets stimulated with subthreshold doses of U46619. Finally, the amplification of U46619-induced aggregation by PGE, (500 nmol/L) was abolished by four different protein kinase C (PKC) inhibitors (calphostin C, staurosporine, H7, and TMB8). Our results suggest that PGE, exerts its facilitating activity on agonist-induced platelet activation by priming PKC t o activation by other agonists. PGE, potentiates platelet activation at concentrations produced by activated platelets and may thus be of pathophysiologic relevance. 0 1993by The American Society of Hematology. A function by itself, but it can affect aggregation when platelets have been previously challenged by an agonist. Indeed, low concentrations of PGE, have a proaggregatory effect, whereas high doses of this prostanoid inhibit platelet aggregation.'-'' It is quite conceivable that the amounts of PGE, normally produced by activated platelets contribute to physiologic platelet activation because they are in the range of those found to potentiate aggregation when exogenously added (1 to 15 n m ~ l / L ) " "and ~ because platelets appear to possess specific receptors for PGE,.I4 In addition, when the enzyme Tx-synthase is pharmacologically blocked, the concentrations of PGE, generated by stimulated platelets increase up to 20 time^,^^^,'^,'^,'^ attaining levels that cause a more pronounced potentiation of platelet aggregation. Indeed, the failure of Tx-synthase inhibition to suppress arachidonate-induced aggregation in a subset of normal subjects (nonresponders) depends largely on PGE, formation.4,9.15 Studies with citrated and heparinized platelet-rich plasma (PRP) have led to the conclusion that the proaggregatory effect of PGE, is mediated by an increased influx of extracellular calcium into platelets,' whereas the inhibitory effect is due to a nonspecific binding to the PGI, receptor with stimulation of adenylate cyclase.I6No recent investigations have been performed to ascertain the biochemical mechanisms through which PGE, potentiates aggregation in human platelets. The aim of our study was thus to assess the effect of PGE, on different excitatory second messenger systems in human platelets. Our results suggest that PGE, is capable of amplifying the platelet response to stimuli by facilitating the activation of protein kinase C (PKC). RACHIDONIC ACID metabolism plays an important role in the regulation of the functional response of platelets to stimuli.' Once liberated from membrane phospholipids by the activity of a phospholipase A, or phospholipase arachidonate undergoes further metabolism either through the 12-lipoxygenaseor through the cyclooxygenase (prostaglandin G, [PGG,]/PGH,-synthase) pathway. The main products of cyclooxygenase are the PG endoperoxides (PGG, and PGH,) and thromboxane A, (TxA,) that is produced by their metabolism through the Tx-synthase enzyme. Minor amounts of the PG endoperoxides are also transformed, by specific isomerases, into PGD,, PGF,,, and PGEz.',4Whereas the role of PGH, and TxA, in the regulation of platelet function in health and disease has been deeply e~plored,'.~ the physiologic functions of PGD,, PGF,,, and PGE, have been much less investigated. PGD, acts on a specific receptor located on the platelet membrane to stimulate adenylate cyclase and thus suppresses platelet function, whereas PGF, appears to be inactive on platelets, if not at high, supraphysiologic, concentration~.'.~ PGE, does not have any effect on platelet From the Institute of Internal and Vascular Medicine and Institute of Medical Biochemistry, University of Perugia, Perugia, Italy. Submitted March 3, 1993; accepted June 30, 1993. Supported in part by a grant to P.G. of the Italian National Research Council (Grant No. 920104104/115). Presented in part at the 7th International Congress on Prostaglandins and Related Compounds (Florence, May 28-June I , 1990) (abstr p 26). at the 1lth Congress ofthe Italian Society on Thrombosis and Haemostasis (Bari. September 24-28, 1990) (abstr 85), and at the 13th Congress ofthe InternationalSocietyon Thrombosis and Haemostasis (Amsterdam, June 30-July 6 , 1991) (abstr 1447). Address reprint requests to Paolo Gresele. MD, PhD, Institute of Internal and Vascular Medicine, University of Perugia, via E. dal Pozzo, I-06126 Perugia, Italy. The publication costs ofthis article were defrayed in part by page charge payment. This article must therefore be herebjJ marked "advertisement" in accordance with 18 U.S.C.section 1734 solely to indicate this fact. 0 1993 by The American Society of Hematology. 0006-4971/93/8209-0014$3.00/0 2704 MATERIALS AND METHODS Preparation of platelets. Blood was collected into 1/ 10 vol/vol trisodium citrate 3.8% from drug-free, healthy donors who had been fasting for I 2 hours; PRP and platelet-poor plasma (PPP) were obtained as previously described"; platelet count in PRP was adjusted to 2.5 X 108/mL with autologous PPP. In some selected experiments, PRP was incubated with aspirin at 1 mmol/L for 15 minutes at 37°C before use. In other experiments, creatine phosphate (CP; 2 mmol/L) and creatine phosphokinase (CPK; 20 U/ mL) were added to PRP to exclude the contribution of endogenous Hood, Vol82, No 9 (November 1). 1993: pp 2704-2713 From www.bloodjournal.org by guest on February 6, 2015. For personal use only. PROSTAGLANDIN E2 AND PLATELET AGGREGATION adenosine diphosphate (ADP) to the results obtained. In other experiments, EGTA at 2 mmol/L was added to citrated PRP 30 seconds before adding PGE2 to analyze the effects of PGE, in a medium without calcium (external calcium <lo-’ mol/L). Before starting each experiment, PRP was tested to see whether the blood donor was a “responder” or a “nonresponder” to in vitro Tx-synthase inhibition? Briefly, PRP was incubated with two different Tx-synthase inhibitors (either dazoxiben at 10 pmol/L or OKY-046 at 10 pmol/L) for 15 minutes at 37°C and then platelets were stimulated with arachidonic acid at the threshold aggregating concentration (TAC) defined as the minimal amount of the stimulus giving full, irreversibleplatelet aggregation (more than 60%light transmission) starting within 2 minutes from the addition of the inducer. Subjects were defined as “responders” when no aggregation was In the observed within 4 minutes after arachidonicacid experiments on PRP, only the platelets from nonresponder donors were used to assess the proaggregatoryactivity of PGE,. Indeed, in PRP from responder people, PGEz does not exert any clear proaggregatory effect even at low concentration^.^ In the experiments on washed platelets (WP), instead, no selection was made between responder and nonresponder donors because PGE, potentiates systematically the aggregation of platelets resuspended in a buffer. For experiments in which WP were used, blood was collected either in 1/6 vol/vol of acid citrate dextrose, pH 5 (ACD formula A; Baxter, Lessines, Belgium), or in EDTA and processed according to the methods described below. Platelet aggregation. Platelet aggregation was studied either in PRP or in WP with the photometric method by using a Chrono-Log 540 dual channel aggregometer (Chrono-Log Corp, Havertown, PA). The calibrationwas performed with autologousPPP in studies on PRP and with HEPES-Tyrode buffer in studies using WP. The samples (0.25 mL) were incubated under continuous stirring for 2 minutes with PGE, or its vehicle and were then challenged with various inducers. Stimuli used were the stable PG endoperoxides analogue U466 19 (9,l I-dideoxy-1l a , 9a-epoxymethano-PG Fh), ADP, thrombin, and phorbol 12-myristate 13-acetate(PMA). To assess the proaggregatory activity of PGE,, a dose-response curve to the aggregatory agent under study was built in every experiment and the subthreshold concentration was defined as the dose giving an aggregation tracing with an amplitude between 20% and 40% of maximal; for thrombin, the amplitude was between 40% and 60% of maximal because, due to the extreme steepness of the dose-responsecurve, it was impossibleto obtain reproducibly a 20% to 40% maximal amplitude. Percentage increases produced by different concentrations of PGE, were calculated from the increase of either the maximal amplitude or the slope of the aggregation tracings in relation to the values obtained in the paired solvent experiments. For the aggregation studies, and for all the other experiments, control samples always contained the identical amount of organic solvents as the treated samples, the final concentration of which never exceeded 0.04%, even in complex experiments in which platelets were treated with three reagents. Aggregations were observed for 3 minutes after the inducer was added; in the experiments with PMA, the aggregations were recorded for 5 minutes. Platelet secretion. Adenosine triphosphate (ATP) release was measured using the luciferin-luciferase method. ATP release and aggregation were monitored simultaneously in PRP samples (0.45 mL) using a Chrono-Log Platelet Ionized Calcium Aggregometer (PICA; Chrono-Log). ATP secretion was quantitated by the luminescenceemitted on the addition of a mixture of luciferin-luciferase (50 pL; Chrono-Lume 395; Chrono-Log) to the sample and expressed as micromoles of ATP per liter. The calibration ofthe signal 2705 of ATP release was performed by adding ATP (2 pmol/L) at the end of the stimulation period to each sample. The release of 0-thromboglobulin (@E) was also assessed, essentially as previously de~cribed.~ Briefly, 3 minutes after the inducer was added, the samples were rapidly transferred into Eppendorf tubes and immediately centrifuged at 12,OOOg for 2 minutes; the supernatant was frozen at -20°C for subsequent assay. Total PTG and ATP content were assessed in the supernatant of samples submitted to three cycles of freezing in liquid nitrogen and thawing at 37°C; for @TG, a blank value was obtained by centrifuging unstimulated samples at 12,OOOgfor 2 minutes and was subtracted from the values obtained in the supernatant of stimulated samples for the measurement of the actual PTG release. PTG was measured by a commercially available enzyme-linked immunosorbent assay (ELISA) kit (Boehringer Mannheim, Mannheim, Germany), as described.’ Platelet shape change. Shape change can be evaluated only when aggregation can not take place, ie, when there is no calcium in the external medium. Thus, blood was collected into EDTA (0.1% final concentration) and PRP was obtained as described above. Platelet shape change was studied with a turbidimetric method” by using an Elvi 840 aggregometer(Elvi Logos, Milan, Italy). The Calibration of the instrument was performed with PRP (10% light transmission)and PPP (90% light transmission). The shape change recording signal was then amplified fivefold to obtain curves of a larger amplitude. The amplitude of shape change was then measured on the recorded tracings and expressed as a percentage of control. In experiments using U46619 as a stimulus, aspirin at 1 mmol/L was added to exclude any contribution from endogenous arachidonic acid metabolites. Calcium measurements. Blood was collected into ACD and WP were prepared as described.” If not differently specified, calcium measurements were performed in platelet suspensionsloaded with aequorin by using small amounts of dimethyl sulfoxide (DMSO).” Aequorin-loaded platelets were finally diluted at a concentration of 108/mLin HEPES-Tyrode buffer (129 mmol/L NaCl, 9.9 mmol/L NaHCO,, 2.9 mmol/L KCI, 0.8 mmol/L KHzP04,0.8 mmol/L MgCI, X 6H,O, 5.6 mmol/L glucose, 10 mmol/L HEPES, pH 7.4) containing Ca2* I mmol/L. Some experimentswere also performed by loadingaequorin with the hypo-osmotic shock treatment (HOST) technique, as previously d e s ~ r i b e d . ’ Aequorin ~.~~ signals were measured by using a calibration curve obtained in a cell-free system. A fixed amount of aequorin (in the order of nanomolar concentrations) was added to a solution containing 5 mmol/L HEPES, 150 mmol/L KCl, 1 mmol/ L Mg2+and Ca2+between and IO-, mol/L. The ratio between the luminescenceobtained for each Ca2+concentration (L) and the luminescence obtained when aequorin was exposed to a saturating CaZ+concentration (1 mmol/L) (Lmax) were measured and the calibration curve was obtained by plotting Log L/Lmax against Log [Ca’’]. Aggregation and calcium release were monitored simultaneously by the use of a Chrono-Log PICA (Chrono-Log). One-milliliteraliquots of aequorin-loaded platelets were incubated with microliter amounts of PGE, or its vehiclefor 2 minutes at 37°C under continuous stirring and then challenged with the inducer. Finally, a separate series of experiments was performed using the fura-2 technique.” Briefly, human blood was collected into disodium EDTA (15 mg/lO mL of blood) and centrifuged at 7008 for 5 minutes, and PRP was then removed. PRP was incubated for 30 minutes at 37°C with I pmol/L fura-2-AM (CalbiochemCorporation, La Jolla, CA) and then centrifuged at 3508 for 20 minutes to obtain a platelet pellet. After careful removal of the supernatant plasma, fura-2loaded platelets were resuspended in HEPES buffer containing 145 mmol/L NaC1, 10 mmol/L glucose, 10 mmol/L HEPES, and 1 From www.bloodjournal.org by guest on February 6, 2015. For personal use only. VEZZA ET AL 2706 mmol/L MgCl,, pH 7.4, at a count of 4 X 107/mL. Each test was performed by adding to I part of this platelet suspension 1 part of the same buffer as above, but containing 2 mmol/L CaC1,. A doseresponse curve to U466 19 was built and the experiment was performed with the dose of the inducer giving the half-maximal calcium peak. PGE, or its vehicle (saline) was incubated for 2 minutes at 37°C before adding the inducer. Fluorescence was measured, under gentle stimng, at 37°C using an Aminco-Bowman spectrofluorimeter (Silver Spring, MD), adjusting the excitation wavelength at 335 nm and the emission wavelength at 505 nm. The calibration of the signal was performed in each sample by adding 0.2% Triton X-100 to obtain the maximal fluorescence (Fmax) and then 1 mmol/L MnC1, to remove all the calcium bound to fura-2 to get the minimal fluorescence (Fmin). Cytosolic free calcium concentration was calculated by the following equation: [CaZ+]= kd[F - Fmin]/[Fmax - F], where kd is the apparent dissociation constant (224 nmol/L) of fura-2 and F is the fluorescence of nonstimulated platelets (basal level of calcium) or the peak of fluorescence obtained in each sample after the stimulation.z2 Fibrinogen binding. Human fibrinogen (specificradioactivity, 122 pCi/mg) was dissolved in distilled water at a concentration of 0.8 mg/mL. The preparation of iodinated fibrinogen was found to be 9790 k 4% (n = 4) clottable. WP were prepared according to Mustard” with slight modifications as previously described3 and diluted to 3 X 108/mL in Tyrode’s buffer (140 mmol/L NaCI, 2.7 mmol/L KCI, 12 mmol/L NaHCO,, 0.4 mmol/L NaH,PO,, 2 mmol/L CaCl,, 1 mmol/L MgCl,) containing 0.35% bovine serum albumin and 0. I % glucose, pH 7.4. The binding of fibrinogen to WP was measured as rep0rted.2~Briefly, 200-pL aliquots of WP were placed into Eppendorf tubes at 37°C without stirring and 5 FL oflabeled fibrinogen was added. A time- and dose-response curve to U466 19 were built by adding the stimulus 30 seconds after labeled fibrinogen. The reactions were stopped by removing three 50+L aliquots from each sample. These aliquots were immediately layered onto 300 pL of a sucrose solution (Tyrode’s buffer containing 2% bovine serum albumin and 20% sucrose, pH 7.4). Free and platelet-bound ligand were separated by centrifugation for 2 minutes at 12,OOOgin an Eppendorf centrifuge. Platelet pellets were counted for the radioactivity in a gammacounter (Packard Instrument CO, Meriden, CT). Nonspecific binding was measured in the presence of a large excess of unlabeled fibrinogen and was always less than 10% of the total binding. Results are expressed as molecules of fibrinogen bound per latel let.'^ In the experiments in which the effects of PGE, were assessed, the PG or its vehicle were added to the samples 30 seconds after labeled fibrinogen; after 2 minutes, the samples were stimulated with increasing concentrations of U466 19 and the reactions were stopped 10 minutes later. Protein phosphorylation. Blood was collected into ACD plus aspirin (1 mmol/L) and platelets were washed twice in a phosphateand calcium-free Tyrode’s buffer (136 mmol/L NaCl, 2.7 mmol/L KCl, 12 mmol/L NaHCO,, 2 mmol/L MgCI2, 5 mmol/L glucose, pH 6.8), resuspended at 2 X lo9in a volume of I mL, and incubated with 500 pCi of carrier-free ”P, neutralized with 1 mol/L Tris-HCI (pH 7.4), for 1 hour at room temperature. After this period, platelets were centrifuged (1,0008 for 10 minutes) and resuspended in Tyrode’s buffer containing phosphate and calcium (1 36 mmol/L NaCl, 2.7 mmol/L KCI, 12 mmol/L NaHCO,, 0.4 mmol/L Na2HP0,, 1 mmol/L MgCl,, 2 mmol/L CaCl,, 5 mmol/L glucose, pH 7.4) at a count of 2 x 108/mL;each test was performed with 250 pL of the ”P-labeled platelet suspension. An aliquot of platelets, prepared as above, was studied by awegometry to establish the TAC to U46619. Platelets were then incubated with PGE2 for 2 minutes and challenged with U466 19 for 90 seconds. The reactions were stopped by the addition of 15% trichloroacetic acid (TCA) and energetic vortexing for 2 minutes. Protein pellets were washed twice with water and then solubilized in 2% sodium dodecyl sulfate (SDS). Samples were subjected to 10%SDS-polyacrylamide gel electrophoresis according to Laemmli.2’ Gels stained with Coomassie blue were dried and autoradiographed through a 17-hour exposure to Kodak X-Omat-AR film (Eastman Kodak, Rochester, NY) at -80°C. The extent ofphosphorylation ofthe 47-kD protein (molecular mass was determined by comparison with concomitantly run molecular mass standards) was assessed by scanning densitometry (Scanning Densitometer SG300; Hoefer Scientific Instruments, San Francisco, CA). In addition, bands containing the 47-kD protein were cut out from the dried gels and radioactivity was determined by liquid scintillation counting. Reagents. PGE, (Sigma Chemical CO, St Louis, MO) was dissolved in ethanol. EGTA (Sigma) was dissolved in NaOH at the concentration of 0.25 mol/L. Acetylsalicylic acid, lysine salt (Lyrca Synthelabo, Milan, Italy); dazoxiben (4-[2-( 1H-imidazol- I -yl)ethoxylbenzoic acid hydrochloride; Pfizer, Sandwich, UK), kindly given by Dr H. Tyler (Pfizer); OKY-046 sodium salt (sodium (E)-3ONO Pharmaceuti[4-( 1-imidazolylmethyl)phenyl]-2-propanoate; cal CO,Osaka, Japan), kindly given by Dr M. Tsuboshima (ONO); creatine phosphate, creatine phosphokinase, and apyrase (all Sigma) were dissolved in distilled water. PGE, (Sigma) was dissolved in ethanol at a concentration of 50 mmol/L and further diluted in 0. I mol/L phosphate buffer. For the experiments in which calcium was measured with the fura-2 technique, PGE, was diluted in saline. U466 19 (9,l I-dideoxy-1 1q 9 a epoxymethano-PGF,,; Sigma) was dissolved in ethanol and further diluted with saline. Thrombin (bovine thrombin; Behring, Marburg, Germany) was dissolved in distilled water. PMA (Sigma) was dissolved in DMSO at a stock concentration of I O mmol/L and further diluted in distilled water. Arachidonic acid, sodium salt (>99% pure; Sigma) were dissolved in 0.05 mol/L phosphate buffer, pH 7.4. ADP (Sigma) was dissolved in ice-cold saline. Adrenaline bitartrate, a 5 mmol/L solution in Tris buffer, was from Mascia Brunelli (Milan, Italy). PGI, (Sigma) was dissolved in glycine buffer at a concentration of 20 pmol/L. Human ’2SI-fibrinogenwas purchased from Amersham (Amersham, UK) and human cold fibrinogen from Kabi (Stockholm, Sweden). Phosphorus-32, as orthophosphoric acid in 1 mL of HC1-free water, was from New England Nuclear (Boston, MA). Reagents for electrophoresis and molecular mass standards were from Bio-Rad (Richmond, CA). Staurosporine (Streptomyces species),Z6calphostin C (Cladosporium cladosporioides),” and 4a-phorbol 12, 13 didecanoate (4aPDD)” (Calbiochem, San Diego, CA) were dissolved in DMSO and further diluted in water (staurosporine and 4aPDD) or saline. H-7 (1-[5isoquinoline sulfonyl]-2 methylpiperazine dihydrochloride; RBI, Natick, USA)29and TMBI ([S-(N,N-diethylamino)octil-3,4,5-trimethoxybenzoate]; Sigma)” were dissolved in water. Sulprostone, kindly given by Dr K.H. Thierauch (Schering AG, Berlin, Germany), was dissolved in saline. Statistical analysis. Data are expressed as mean k SEM. Oneway analysis of variance followed by Tukey’s multiple comparison test between all pairs was applied. A probability level less than .05 was considered to be significant. When data are presented as a percentage of control, statistical analysis was performed on absolute values. RESULTS Efects of PGE, on platelet aggregation, calcium movements, and secretion. PGE, ( 5 to 500 nmol/L) caused an increase of the maximal amplitude of aggregation of aequorin-loaded WP stimulated with subthreshold concentrations of U466 19 (0.1 to 0.4 Kmol/L). The increase was sta- From www.bloodjournal.org by guest on February 6, 2015. For personal use only. 2707 PROSTAGLANDIN E, AND PLATELET AGGREGATION crease of aggregation (+33%) observed only with PGE, at 5 pmol/L; PGE, at 50 pmol/L decreased thrombin-induced aggregation significantly (-43.5%) (Fig 2). Low doses of thrombin induced a calcium increase of I .44 2 0.2 pmol/L; PGE, ( 5 nmol/L to 5 pmol/L) did not increase calcium transients induced by thrombin, whereas high concentrations of the prostaglandin (50 pmol/L) decreased calcium increase by 41% (Fig 2). We also studied the effects of PGE, on aggregation in WP challenged with low doses (10 to 50 nmol/L) of PMA, a phorbol ester that can directly stimulate PKC. The maximal amplitude of PMA-induced aggregation was increased by PGE, at 50 nmol/L (+15.7% k lo%, n = 5) and at 500 nmol/L (+71.7% k 4.4%, n = 5, P < .05), whereas it was depressed by PGE, at 50 pmol/L (-52.6% 18.6%,n = 4). On the other hand, PGE, was not able to increase calcium movements in platelets stimulated by low doses of PMA (from 0.95 k 0.14 pmol/L without PGE, to 0.87 k 0.19 pmol/L with PGE, at 500 nmol/L, n = 5 ) despite its proaggregatory effect (data not shown). When 4aPDD (40 nmol/ L to 1 pmol/L), a phorbol ester lacking the ability to stimulate PKC?' was used as a stimulus, no platelet aggregation was seen either in the absence or in the presence of PGE, (500 nmol/L; data not shown). In washed platelets stimulated with fully aggregatory doses of U466 19 (0.2 to 0.5 pmol/L), thrombin (0.05 to 0.1 U/mL), or PMA (40 to 500 nmol/L), PGE, ( 5 to 500 nmol/ L) caused only minor, not significant increases of platelet aggregation (maximum +20%), with no effects on the calcium transients. In platelets loaded with aequorin by either the DMSO or the HOST technique, PGE, alone, in the range of concentrations used (5 nmol/L to 50 pmol/L), never caused an increase ofcalcium levelsabove the basal in any ofthe preparations tested. When using the fura-2 technique, low doses (0.1 to 0.2 pmol/L) of U466 19 gave an increase of calcium above the basal level of 58% k 7%; with PGE, (5 to 500 nmol/L), no further increases of calcium were observed. On the other tistically significant with PGE, at 50 nmol/L (+61%), 250 nmol/L (+ 1 13%), and 500 nmol/L (+ 150%);the highest dose of PGE, tested (50 pmol/L) caused a strong inhibition of platelet aggregation (-88%) (Fig 1). The slope of aggregation was also increased significantlyby PGE, at 250 nmol/L and 500 nmol/L (+61% and +79%, respectively), whereas PGE, at 50 pmol/L had a significant depressing effectalso on this parameter (-83.5%) (Fig 1). Subthreshold doses of U46619 induced a calcium rise of 1.37 k 0.17 pmol/L; PGE, (50 to 500 nmol/L), despite its clear potentiating effect on aggregation, did not enhance calcium increases significantly as compared with the control. The maximum, not significant, increase was obtained with PGE, at 500 nmol/L (+38%), a concentration that enhanced aggregation by 150%.On the other hand, PGE, at 50 pmol/L caused a significant decrease of calcium transients (-78%) (Fig I). When the same experiments were repeated in platelets loaded with aequorin by the HOST te~hnique,'',~~ identical results were obtained (namely, subthreshold U466 19 = calcium increase of l. 17 k 0.23 pmol/L [n = 41; +PGE, at 500 nmol/L = 1.29 k 0.22 pmol/L [+IO%, n = 4, P = NS]). Similar data (potentiation of aggregation by PGE, with no increase of calcium movements) were obtained with aspirin-treated ( 1 mmol/L) platelets stimulated with subthreshold U466 19 (data not shown). Experiments were also performed to assess the effects of sulprostone (a PGE, analogue)I0on platelets challenged with subthreshold doses of U466 19. Sulprostone (5 nmol/L to 100 pmol/L) caused a significant increase of the maximal amplitude of aggregation at all the doses tested (maximum increase, 106%with sulprostone at 50 pmol/L; n = 5, P < .0001) without a parallel increase of calcium increases as detected with the aequorin method (maximum increase, +36% with sulprostone at 500 nmol/L; n = 5, P = NS). At none of the doses tested did sulprostone induce any inhibition of platelet aggregation or calcium movements. When WP were stimulated with low doses of thrombin (0.02 to 0.03 U/mL), the proaggregatory effects of PGE, were less evident than with U46619, with a significant in- * + 75 * h. K v Fig 1. Maximal amplitude of aggregation (0). and slope of aggregation (m) and calcium movements (E) in aequorinloaded WP stimulated by subthreshold doses of U46619 (0.1 to 0.4 pmol/L) and preincubated with increasing concentrations of PGE, or with its vehicle (C).*A significant difference as compared with the control (P < .05, at least). With threshold doses of U46619 (0.2 to 0.5 pmol/L), calcium increase was 2.56 f 0.23pmol/L(n = 7). F 50 * * T h. 1 T dw 3 4 25 0 0 50nM C 5nM 500nM 25pM 250nM 5pM 50pM + PGE2 From www.bloodjournal.org by guest on February 6, 2015. For personal use only. VEZZA ET AL 270% 100 h x v T ++ a 7 l *I 1 -V 1 0 C 50nM 250nM 500nM 5pM 50pM + PGE2 hand, PGE, at 5 and 50 pmol/L significantly inhibited calcium increases by 65% and loo%, respectively (Fig 3). The effects of PGE, were studied also in PRP stimulated with subthreshold doses of U46619 (0.4 to 0.7 pmol/L) or ADP (0.6 to 1 pmol/L). Aggregation induced by U46619 was increased by PGE, up to a maximum of +465% (PGE, at 500 nmol/L); PGE2 at 50 pmol/L totally suppressed aggregation. ADP-induced aggregation was also potentiated with a maximal increase of + 179%with PGE, at 500 nmol/ L. PGE, at 50 pmol/L exerted an inhibitory effect (-55%) (Fig 4). Another set of experiments was performed in PRP supplemented by EGTA, ie, in a low extracellular calcium environment. Without external calcium, the dose-response curve to U46619 was shifted to the right, but PGE, at 500 nmol/L was still able to give an increase of aggregation (Fig 5). The Fig 2. Maximal amplitude of aggregation (U) and calcium increases (E!) in aequorin-loaded WP stimulated by subthreshold doses (0.02 to 0.03 U/ mL) of thrombin and preincubated with PGE, or its vehicle (C). *A significant difference as compared with the control (P< .05, at least). With threshold doses of thrombin (0.05 to 0.1 U/mL), calcium transients attained 3.6 -C 0.8 pmol/L (n = 7). stimulatory effect of PGE, on U466 19-induced aggregation was not diminished by the preincubation of PRP with aspirin and CP/CPK (data not shown). In the range of concentrations tested (5 nmol/L to 50 pmol/L), PGE, alone did not induce platelet aggregation in either WP or in PRP in any of the volunteers tested. From these data, it appears that PGEz potentiates aggregation both in WP and in PRP. We then studied the effects of PGE, on secretion of a- and dense-bodies in PRP. With subthreshold concentrations of U466 19 (0.4 to 0.7 pmol/L), the release of ATP was negligible. PGE, dose-dependently increased ATP release up to a maximum of 1.2 f 0.13 pmol/L at 500 nmol/L (Fig 6). In aspirin-treated platelets, the release of ATP induced by U46619, although blunted, was still significantly enhanced by PGE, at 500 nmol/L (from 0 to 0.74 k 0.27 pmol/L, n = 5, P < .05, data not shown). ATP release induced by subthreshold doses of 70 1 * C 5nM 50nM 500nM 5pM 50pM + PGEz Fig 3. Effects of PGE, on calcium movements as measured by the fura-2 technique in platelets stimulated with low doses of U46619 (0.1 to 0.2 pmol/L) (n = 5). Results are expressed as the percentageof increase above the basal level (111.5 -C 6.2 nmol/L, n = 25); maximal doses of the inducer (0.2 to 1 pmol/L) increased calcium by 137% 18%above basal (n = 7). *A significant difference as compared with the control (P < .05, at least). C 50nM 250nM 500nbi 50pM f PGEz Fig 4. Effects of PGE2on aggregation induced by subthreshold doses of ADP (E!) or of U46619 (0)in PRP from nonresponder donors. Data represent mean -C SEM of four experiments for U46619 and of five for ADP. *A significant difference as compared with the control (P < .05, at least). The inset shows representative aggregation tracings in response to a subthreshold dose of U46619 (0.4 pmol/L) or of ADP (1 pmol/L) in the absence (C) or in the presence of PGE, at 500 nmol/L ( +PGE,). From www.bloodjournal.org by guest on February 6, 2015. For personal use only. PROSTAGLANDIN E2 AND PLATELET AGGREGATION 2709 n 60 - 3 h be v 3 W 40- 2W F: 4 0 4 W k 200 4 0- 0.4 i 2 B [U466191 (pM) -T Fig 5. Effects of PGE, (500 nmol/L) on the platelet aggregation dose-response curve to U46619 in PRPfrom nonresponder donors. Thirty seconds after the addition of EGTA at 2 mmol/L (0, 0) or water (A,A), PGE, or itsvehicle was added and PRP was incubated for additional 2 minutes. Platelets were then stimulated with increasing concentrations of U46619 and the maximal amplitude of aggregation was recorded. One experiment representative of three others is shown. Open symbols represent controls (vehicle-pretreated); solid symbols represent PGEz (500 nmol/L)-pretreated samples. C ADP (0.12 & 0.04, n = 5) was also strikingly enhanced by PGE, at 500 nmol/L (1.85 & 0.72 pmol/L, n = 5 , P < .05), whereas PGE, at 50 pmol/L totally suppressed it (Fig 6). PGE, was also able to increase U466 19-induced /3TG secretion from 145.5 k 145.5 ng/108 platelets to 967 k 145 ng/ 10' platelets with PGE, at 500 nmol/L; with PGE, at 50 pmol/L, PTG release was 142 k 50 ng/108 platelets (Fig 6). Eflects of PGE, on shape change. In our experimental conditions, all the platelet agonists tested induced shape change (U466 19, thrombin, ADP, and collagen) except adrenaline (10 to 100 pmol/L) and PMA (40 to 200 nmol/ L). From a dose-response curve to U466 I9 or thrombin an average concentration of the inducer giving half-maximal amplitude of shape change was identified (U46619, 400 nmol/L; thrombin, 0.1 U/mL) and used throughout the experiments. At proaggregatory concentrations (50 to 500 nmol/L), PGE, did not affect the shape change induced either by U466 19 or by thrombin. High concentrations of PGE, (50 pmol/L) significantly reduced shape change. Effects ofPGE, onfibrinogen binding. U466 19 caused a time- and dose-dependent binding of labeled fibrinogen to human platelets. In time-course experiments of fibrinogen binding induced with U466 19 at 2.5 pmol/L, a plateau was reached in 5 minutes and the values remained stable up to 20 minutes (data not shown). For this reason, a 10-minute stimulation period was chosen for the experiments with PGEl. A dose-response curve for fibrinogen binding induced by U466 19 was performed in the absence and in the presence of PGE,; PGE, at 500 nmol/L shifted the dose-response curve to the left. Indeed, whereas the maximal number of fibrinogen molecules bound in the absence or in the presence of PGE, did not differ, the concentration of U466 I9 giving half-maximal binding was lowered by PGE, from 0.88 to 0.26 pmol/L (Fig 7). PGE, at 50 pmol/L inhibited fibrinogen binding induced 50nM 250nM500nM 50pM + PGE2 Fig 6. Effects of PGE, on platelet secretion induced by subthreshold doses of U46619 or ADP. (A) ATP release; (B) j3TG release. (A) ATP levels inthe supernatant of lysed platelets (totalATP content) were 7.1 1 2 0.3 pmol/L (n = 3). ATP release in platelets or ADP stimulated with maximal aggregatory doses of U46619 (0) (H) was 1.9 2 0.1 25 pmol/L (n = 4) and 2.9 2 1 pmol/L (n = 4). respectively. (B) j3TG levels in the supernatant of resting platelets (blank value) were 754 2 142 ng/108 platelets (n = 4); total platelet j3TG content was 2,850 f 137 ng/108 platelets (n = 4). *A significant difference as compared with the control (P C .05, at least). by U466 19 (1 pmol/L) by 76% f 7% (P< .05, n = 5 ) (data not shown). Eflect ofPGE, on protein phosphorylation. Platelet stimulation with U466 19 at subthreshold concentrations in- 1 12 I T ' 8 . 4 0 - 10-6 10-7 10-6 [U466191 (M) Fig 7. Dose-response curve of fibrinogen binding induced by U46619 in the presence of PGE, (500 nmol/L) (A)or its vehicle (control, 8) (n = 4). The EC,, for U46619 was shifted from 0.88 pmol/L (control) to 0.26 pmol/L ( + PGE, at 500 nmol/L). From www.bloodjournal.org by guest on February 6, 2015. For personal use only. 2710 P47 VEZZA ET AL 4 100 189 259 294 298 107 256 249 409 % U46 SdaM UdDM SOODM PGE.2 U46 +%Ea PMA STIM mb -----SbOllM TAC %hf NOT TAC +PG& Fig 8. Protein phosphorylation was assessed as described in Materials and Methods by stimulating platelets with U46619 (U46)at 6 pmol/L (subTAC), in the presence of increasing concentrations of PGE, or its vehicle, with U46619 at 12 pmol/L (TAC) in the presence of PGE, at 50 pmol/L or its vehicle, or with PMA (2.5 pmol/L). The radioactivity of the 47-kD protein, expressed as a percentage of the nonstimulated sample (not stim), is reported below each lane. duced only a slight incorporation of radioactivity into the 47-kD protein, whereas with fully aggregatory concentrations of the inducer the radioactivity of the 47-kD band was higher (Fig 8). When PGE, (50 to 500 nmol/L)-preincubated platelets were stimulated with subthreshold U466 19, a higher degree of phosphorylation of the 47-kD protein was found. In basal conditions. the radioactivity in the 47-kD band was 108 cpm/108 platelets: in the presence of low doses of U466 I9 alone. the count was 204 cpm/ IO8 platelets, whereas with PGE, the radioactivity increased up to 321 cpm/lO* platelets (+l98% as compared with the nonstimulated sample). In staurosporine (200 nmol/L)preincubated platelets, the increase of radioactivity of the 47-kD protein given by PGE, at 500 nmol/L was suppressed (+26% over the basal) (data not shown). PGE, alone (500 nmol/L) did not induce any phosphorylation of the 47-kD protein. PMA (2.5 pmol/L) induced a marked increase of the radioactivity of the 47-kD band (+309% over the basal) (Fig 8). The analysis of the autoradiography of the gels with scanning densitometry gave results similar to those obtained with scintillation counting concerning the 47-kD band and showed that the stimulation of platelets with PMA, as well as with U46619 plus PGE,, enhances the phosphorylation of other proteins, including a band of a p proximate 20 kD that may represent myosin light chain (data not shown). The latter result is compatible with PKC activation because a 20-kD protein is also a substrate of this enzyme.” E / ~ Y qf . YPKC inliihitors. In view of the ability of PGE, to enhance the phosphorylation of the 47-kD protein, we undertook a series of experiments to assess the effects of different PKC inhibitors on the proaggregatory activity of this prostaglandin. Experiments were performed with staurosporine.a powerful PKC inhibito?6 that also interferes with some tyrosine kinase activities’,: H7, an inhibitor of PKC’’ also active on cyclic-nucleotide-dependent protein kinase and on calmodulindependent protein kinase 11”; TMBR, an intracellular calcium antagonist’’ also able to interfere with the PKC path~ay’~; and, finally, calphostin C, a recently described, highly selective PKC inhibit~r.~’ Aspirin-treated ( I mmol/L) PRP was preincubated with staurosporine (100 and 200 nmol/L), H7 (100 and 500 pmol/L), TMB8 (50 and 100 pmol/L), calphostin C (200 nmol/L). or their vehicle, for 2 minutes before adding PGE,. Subthreshold aggregatory concentrations of U466 19 (0.2 to 0.6 pmol/L) were then added and maximal amplitude of aggregation at 3 minutes was measured. PGE, at 500 nmol/L increased significantly the maximal amplitude of aggregation from 1 1 % f 7% to 36.5% f 9.5% (+228%, n = 5. P < .Ol): with staurosporine at 100 and 200 nmol/L, the increase induced by PGE, was reduced to 63% and 4% respectively, and with calphostin C at 200 nmol/L to +44%: H7 and TMB8 also blunted the amplifying effect of PGE, on U466 19-induced aggregation (Fig 9). The increase of aggregation induced by PGE, in the presence of the four PKC inhibitors was no longer significant as compared with control. The inhibitory effect of the PKC inhibitors on PGE,-induced potentiation of aggregation was present also in nonaspirinated platelets (data not shown). At the concentra- /46+g; U46 Fig 9. Effect of calphostin C (calph C; 200 nmol/L), staurosporine (stauro; 200 nmol/L), H7 (100 pmol/L), or T M B I (100 pmol/L) on the ampliwing activity of PGE, (500 nmol/L) on aggregation induced by subthreshold U46619 (U46). In the last tracing, the effects of calphostin C, staurosporine, and T M B I on aggregation induced by fully aggregatory doses of U46619 (0.4 to 1 pmol/L) are shown. Aggregation tracings of one representative experiment from a total of five are reported. From www.bloodjournal.org by guest on February 6, 2015. For personal use only. 271 1 PROSTAGLANDIN E, AND PLATELET AGGREGATION calcium in the activity of PGE, .37 In addition, PGE, potentiates platelet aggregation even in the presence of EGTA added to chelate external Ca", which is also against a preeminent role of calcium influx in the proaggregatory activity of this prostaglandin, in contrast to what was previously ~uggested.~ PGE, did not potentiate agonist-induced platelet shape change, whereas it strongly amplified both dense- and agranule secretion; shape change is strongly dependent on calcium and is not significantly affected by PKC,38,39 whereas PKC activation is essential for platelet secretion, a phenomenon in which calcium increases are less important.36340341 The activation of PKC is also involved in the expression of fibrinogen receptors on platelet^^^^^^ and we found that FGE, strongly increases fibrinogen binding to platelets stimulated with the endoperoxide analogue U466 19. Potentiation by PGE, of platelet aggregation and secretion induced by U466 19 was accompanied by an enhanced phosphorylation of the 47-kD protein that is the main substrate of PKC in platelets,& although PGE, itself did not induce any phosphorylation. In addition, three substances (staurosporine, H7, and TMB8) able to suppress nonselectively PKC but with a pattern of accessory activities different from one another:6.29,32-34and a highly selective PKC DISCUSSION inhibitor (calphostin C),27all abolished the amplifying effect Our results confirm that PGE, exerts a proaggregatory of PGE, on U466 19-induced platelet aggregation. Interesteffect at concentrations generated by activated platelets. A ingly, staurosporine only marginally affected, instead, the potentiation of agonist-induced platelet aggregation is obamplifying effect of adrenaline on U466 19-induced aggreserved both in PRP and in WP. PGE, amplifies the platelet gation. Similar to PGE,, adrenaline is able to potentiate the response to a range of agonists acting on different receptors, platelet aggregatory response to other stimuli35but with a such as U466 19 (TxA,/PGH, receptor agonist), thrombin, mechanism largely independent from PKC a ~ t i v a t i o n . ~ ~ or ADP, as well as the response to PMA, a PKC activator, Thus, our results indicate that low concentrations of implying that the proaggregatoryeffect is exerted at the level PGE, amplify the platelet response to various agonists by of a second messenger system common to different agonists. potentiating PKC activity. Considering that direct activaThe amplifying effect of PGE, on platelet aggregation is not tion of PKC by PGE, seems unlikely, because this PG does paralleled by a similar activity on calcium transients. Innot phosphorylate the 47-kD protein, a priming effect on deed, in conditions in which aggregation is almost triplithe enzyme appears to be the most likely explanation. PGE, cated, the intraplatelet calcium increase is enhanced only by might prime PKC to other stimuli by favoring the translocaone-third. Although no linear relation exists between the tion of the enzyme to the membrane,36by lowering the calmagnitude of calcium increase and the amplitude of the or by cium threshold necessary for enzyme a~tivation,~' platelet aggregation response in conditions of synergistic other, as yet undefined mechanisms. Alternatively, PGE, platelet activation by pairs of agonist^,^' an initial priming might favor the generation of diacylglycerol, a known acticalcium increase must be provoked by the first agonist to vator of PKC,& as a consequence of either phospholipase C enhance the aggregation response to the ~ e c o n d .In ~ ~our . ~ ~ or phospholipase D a ~ t i v a t i o n .Indeed, ~ ~ , ~ ~a stimulatory efexperiments, PGE, alone never induced any calcium tranfect of PGE, on PKC activation has already been described sients in human platelets; thus, a priming effect exerted in other cell types, such as the bovine adrenal chromaffin through calcium movements appears to be unlikely. The cells,"8 and both phospholipase and phospholipase DS0 lack of effect of PGE, on calcium transients in platelets was activation have been reported. Further studies are detected with fura-2 and with aequorin, the latter loaded warranted to clarify the exact mechanism of PKC priming into platelets by two different techniques, the DMSO" and by PGE, in platelets. the HOST method^.'^,^" Different aequorin-loading techThe effects of PGE, on platelet activation are likely to be niques were used because some agonists that induce a calreceptor-mediated because sulprostone, a PGE, analogue cium increase when platelets are loaded by the HOST techthat binds to the platelet surface, could reproduce the proagnique do not cause such an increase when the cells are gregatory activity of PGE,. It has been suggested that plateloaded by the DMSO technique, presumably because of an lets possess at least two different PGE, receptor subtypes, inhibitory effect of DMSO.I9 The observation that similar one with high and the other with low affinity.I4One ofthese results were obtained with various Ca" measurement techmight mediate the priming effect of low concentrations of niques excludes the possible insensitivity of the method PGE, on platelet PKC, and the other might be responsible used as the cause of the apparent lack of involvement of for the stimulation of adenylate cyclase and platelet inhibitions suppressing the proaggregatory effect of PGE,, the four PKC inhibitors did not affect aggregation induced by fully stimulatory doses (0.4 to 1 pmol/L) of U466 19 (Fig 9) except for the highest concentration of H7 (500 pmol/L), whichreduceditby81.4%(n = 5,P<.Ol)(datanotshown). Additional experiments were performed to assess the synergistic effect of adrenaline on U466 19-induced platelet agg r e g a t i ~ n .Adrenaline, ~~.~~ at a dose not provoking aggregation (0.2 to 2 pmol/L), potentiates platelet aggregation induced by subthreshold doses of U46619 (from 12.9% f 1.8% to 45.4% f 6.8%; +252%, n = 4, P < .05) in 4 of 6 blood donors tested. Staurosporine (200 to 400 nmol/L) did not suppressthe proaggregatoryeffect ofadrenaline on platelets stimulated with subthreshold doses of U466 19 (adrenaline + U466 19 = 45.4% f 6.8%;staurosporine + adrenaline U46619 = 38.8% f 12.6%,n = 4, P = NS). In aspirintreated platelets, adrenaline potentiated platelet aggregation in5 of6blooddonorstested(from 14.6%+ 1.6%to41.3% k 6.6%; + 18370, n = 5, P < .01). Even in these conditions, staurosporine (200 to 400 nmol/L) did not significantly inhibit the proaggregatory effect of adrenaline (adrenaline U46619 = 41.3% 6.6%; staurosporine adrenaline U46619 = 26.4% f 5.7%, n = 5, P = NS). + * + + + c9 From www.bloodjournal.org by guest on February 6, 2015. For personal use only. 2712 VEZZA ET AL tion provoked by high concentrations of this prostaglandinI6 and could actually be the PGI, receptor. Sulprostone is likely t o interact selectively with only one PGE, receptor subtype as it only potentiates platelet aggregation. The previously described ability of low concentrations of PGE, to antagonize the intraplatelet CAMP increase induced by PGE, , PGI,, and PGD; could also be partly explained by its effect on PKC activation. Indeed, platelet adenylate cyclase is negatively regulated by PKC.” The platelet aggregation facilitating activity of PGE, is probably of pathophysiologic relevance because PGE, exerts its priming effects already at concentrations normally produced by activated platelets (1 to 15 nmol/L). A stronger potentiation is observed with higher concentrations of this prostanoid (50 t o 500 nmol/L) such as those that may be produced by platelets under pathologic conditions, eg, in the nephrotic syndrome, or when the enzyme Tx-synthase is pharmacologically blo~ked.4,’,’~,’~ Interestingly, nephrotic syndrome is characterizated by a high incidence of thrombotic events,52 whereas the neutralization of PGE, by specific antibodies enhances the in vitro effectiveness of Txsynthase inhibitors.’ Finally, PGE, is the main product of endothelial cells in the microcirculations3 where this prostanoid, due to the high endothelial cell/plasma ratio, may well reach elevated concentration^.^^ The development of specific platelet-type (EP,) PGE, receptor antagonists and purification of the PGE, receptor will help to clarify the role of PGE, in pathophysiology. ACKNOWLEDGMENT We thank Prof E. Boschetti for the assistance given with the statistical analysis of data; and Prof L. Binaglia, Prof C. Riccardi, Prof R. Donato, and Dr G. Sorci (Department of Experimental Medicine and Biochemical Sciences, University of Perugia) for the help they gave us for the phosphorylation experiments. We are grateful to Prof G. Goracci (Institute of Medical Biochemistry) for critical reading of the manuscript and to Dr A. Sturk, M. Schaap, and Prof J.W. ten Cate (Department of Haematology, University of Amsterdam) for the suggestionsgiven in the setting up of the fura-2 technique for intraplateletcalcium levels. The technical assistanceof G. Cipiciani is gratefully acknowledged. REFERENCES I . Moncada S, Higgs EA: Arachidonate metabolism in blood cells and the vessel wall. Clin Haematol 15:273, 1986 2. Lapetina EG: Regulation of arachidonic acid production: Role of phospholipaseC and A,. Trends Pharmacol Sci 3: 1 15,1982 3. Stasi M, Gresele P, Porcellati S, Quero E, Nenci GG,Goracci G Activation of phospholipase A, and P-thromboglobulin release in human platelets: Comparativeeffects of thrombin and fluoroaluminate. Biochim Biophys Acta 1124:279, 1992 4. Gresele P, Deckmyn H, Nenci GG, Vermylen J: Thromboxane synthase inhibitors, thromboxane receptor antagonists and dual blockers in thrombotic disorders. Trends Pharmacol Sci 12:158, 1991 5 . Shio H, Ramwell PW, Jessup SJ: Prostaglandin E,: Effects on aggregation, shape change and cyclic AMP of rat platelets. Prostaglandins 1:29, 1972 6. Salzman EW: Cyclic AMP and platelet function. N Engl J Med 286:358, 1972 7. MacIntyre DE, Gordon JL: Calcium-dependent stimulation of platelet aggregation by PGE,. Nature 258:337, 1975 8. Weiss HJ, Willis AL, Kuhn D, Brand H: Prostaglandin E, potentiation of platelet aggregation induced by LASS endoperoxide: Absent in storage pool disease, normal after aspirin ingestion. Br J Haematol32:257, 1976 9. Gresele P, Blockmans D, Deckmyn H, Vermylen J: Adenylate cyclase activation determines the effect of thromboxane synthase inhibitors on platelet aggregation in vitro. Comparison of platelets from responders and nonresponders. J Pharmacol Exp Ther 246:301, 1988 IO. Thierauch KH, Prior G Modulation ofplatelet activation by prostaglandin E, mimics. Adv Prostaglandin Thromboxane Leukot Res 21:383, 1990 1 1. Gray SJ, Heptinstall S: Interactions between prostaglandin E, and inhibitors of platelet aggregation which act through cyclic AMP. Eur J Pharmacol 194:63, 1991 12. Orchard MA, Waddell KA, Lewis PJ, Blair IA: Thromboxane synthase inhibition causes re-direction of prostaglandin endoperoxides to prostaglandin D, during collagen stimulated aggregation of human platelet rich plasma. Thromb Res 39:701, 1985 13. Gresele P, Deckmyn H, Arnout J, Nenci GG, Vermylen J: Characterization of N,N’-bis(3-picolyl)-4-methoxy-isophtalamide (picotamide)as a dual thromboxane synthase inhibitor/thromboxane A, receptor antagonist in human platelets. Thromb Haemost 61:479, 1989 14. Eggerman TL, Andersen NH, Robertson RP: Separate receptors for prostacyclin and prostaglandin E, on human gel-filtered platelets. J Pharmacol Exp Ther 236568, 1986 15. Gresele P, Deckmyn H, Huybrechts E, Vermylen J: Serum albumin enhances the impairment of platelet aggregation with thromboxane synthase inhibition by increasing the formation of prostaglandin D,. Biochem Pharmacol33:2083, 1984 16. Gray SJ, Heptinstall S: The effects of PGE, and CL 115,347, an antihypertensivePGE, analogue, on human blood platelets behaviour and vascular contractility. Eur J Pharmacol l14:129, 1985 17. Dorn GW, De Jesus A: Human platelet aggregation and shape change are coupled to separate thromboxane A,-prostaglandin H, receptors. Am J Physiol 260:H327, I99 1 18. Yamaguchi A, Suzuki H, Tanoue K, Yamazaki H: Simple method of aequorin loading into platelets using dimethyl sulfoxide. Thromb Res 44:165, 1986 19. Malmgren R, Grunfelt S, Joseph R: On the significance of different aequorin loading techniques on intracellular aequorin discharge, baseline calcium, platelet aggregation and aequorin-indicated Ca’+-transients.Thromb Haemost 68:352, 1992 20. Saitoh M, Slayter HS, Watkins SC, Ware JA: Cytoplasmic localization of aequorin loaded into human platelets by a new method. Thromb Haemost 67: 182, 1992 21. Rao GHR, Peller JD, White JG: Measurement of ionized calcium in blood platelets with a new generation calcium indicator. Biochem Biophys Res Commun 132:652, 1985 22. Daniel JL, Selok MA, Purdon AD, Salganicoff L: Methods for the study of the role of calcium in platelet function, in Colman RW, Smith JB (eds): Methods for Studying Plateletsand Megakaryocytes. New York, NY, Liss, 1987, p 185 23. Mustard JF, Perry DW, Ardlie NG, Packman MA: Preparation of suspensions of washed platelets from humans. Br J Haemato1 22:193, 1972 24. Di Minno G, Thiagarajan P, Perussia B, Martinez J, Shapiro S, Trinchieri G, Murphy S: Exposure of platelet fibrinogen-binding sites by collagen,arachidonic acid, and ADP Inhibition by a monoclonal antibody to the glycoprotein IIb/lIIa complex. Blood 6 1: 140, 1983 From www.bloodjournal.org by guest on February 6, 2015. For personal use only. PROSTAGLANDIN E2 AND PLATELET AGGREGATION 25. Laemmli U K Cleavage of structural proteins during the assembly of the head of bacteriophage T4. Nature 227:680, 1970 26. Tamaoki T, Nomoto H, Takahashi I, Kat0 Y, Morimoto M, Tomita F Staurosporine, a potent inhibitor of phospholipid/Ca++ dependent protein kinase. Biochem Biophys Res Commun 135:397, 1986 27. Kobayashi E, Nakano H, Morimoto M, Tamaoki T: Calphostin C (UCN-l028C), a novel microbial compound, is a highly potent and specific inhibitor of protein kinase C. Biochem Biophys Res Commun 152548, 1989 28. Siess W, Lapetina E G Phorbol esters sensitize platelets to activation by physiological agonists. Blood 70: i 373, 1987 29. Kawamoto S, Hidaka Y: 1(5-isoquinolinesulfonyl)-2-methylpiperazine (H7) is a selective inhibitor of protein kinase C in rabbit platelets. Biochem Biophys Res Commun 125:258, 1984 30. Murer EH: The role of platelet calcium. Semin Hematol 22:313, 1985 31. Naka M, Nishikawa M, Adelstein RS, Hidaka H: Phorbol ester-induced activation of human platelets is associated with protein kinase C phosphorylation of myosin light chains. Nature 306:490, 1983 32. Nakano H, Kabayashi E, Takahashi AL, Tamaoki T, Kuznu Y, Iba H: Staurosporine inhibits tyrosine-specific protein kinase activity of Rous-sarcoma virus transforming protein P60. J Antibiot (Tokyo) 5:706, 1987 33. Huang C K Protein kinases in neutrophils: A review. Membr Biochem 8:61, 1989 34. Simpson AWM, Hallam TJ, Rink TJ: TMB-8 inhibits secretion evoked by phorbol ester at basal cytoplasmic free calcium in quin 2 loaded platelets much more effectively than it inhibits thrombin-induced calcium mobilization. FEBS Lett 176: 139, 1984 35. Ware JA, Smith M, Salzman EW: Synergism of platelet-aggregating agents. Role of elevation of cytoplasmic calcium. J Clin Invest 80267, 1987 36. Siess W, Lapetina EG: Ca++-mobilizationprimes protein kinase C in human platelets. Calcium and phorbol esters stimulate platelet aggregation and secretion synergistically through protein kinase C. Biochem J 255:309, 1988 37. Ware JA, Johnson PC, Smith M, Salzman E W Aequorin detects increased cytoplasmic calcium in platelets stimulated with phorbol ester or diacylglycerol. Biochem Biophys Res Commun 133:98, 1985 38. Le Breton GC, Dinerstein RJ, Roth LJ, Feinberg H: Direct evidence for intracellular divalent cation redistribution associated with platelet shape change. Biochem Biophys Res Commun 71:362, 1976 39. Nakano T, Hanasaki K, Arita H: Role of protein kinase C in U466 19-induced platelet shape change, aggregation and secretion. Thromb Res 56:299, 1989 2713 40. Rink TJ, Sanchez A, Hallam TJ: Diacylglycerol and phorbol ester stimulate secretion without rising cytoplasmic free calcium in human platelets. Nature 305:317, 1983 41. Knight DE, Niggli V, Scrutton MC: Thrombin and activators of protein kinase C modulate secretory responses of permeabilized human platelets induced by Ca". Eur J Biochem 143:437, 1984 42. Shattil SJ, Brass L F Induction of the fibrinogen receptor on human platelets by intracellular mediators. J Biol Chem 262:992, 1987 43. Saitoh M, Salzman EW, Smith M, Ware JA: Activation of protein kinase C in platelets by epinephrine and A23 187: Correlation with fibrinogen binding. Blood 74:2001, 1989 44. Imaoka T, Lynham JA, Haslam RJ: Purification and characterization of the 47,000-dalton protein phosphorylated during degranulation of human platelets. J Biol Chem 258:11404, 1983 45. Schatz-Munding M, Ullrich V: Priming of human polymorphonuclear leukocytes with granulocyte-macrophage colony-stimulating factor involves protein kinase C rather than enhanced calcium mobilization. Eur J Biochem 204:705, 1992 46. Haslam RJ: Signal transduction in platelet activation, in Verstraete M, Vermylen J, Lijnen R, Amout J (eds): Thrombosis and Haemostasis. Leuven, Belgium, Leuven University, 1987, p 147 47. Nishizuka Y: Intracellular signaling by hydrolysis of phospholipids and activation ofprotein kinase C. Science 258:607, 1992 48. Negishi M, Ito S, Hayaishi 0: Involvement ofprotein kinase C in prostaglandin E,-induced catecolamine release from cultured bovine adrenal chromaffin cells. J Biol Chem 265:6182, 1990 49. Negishi M, Ito S, Hayaishi 0: Prostaglandin E receptors in bovine adrenal medulla are coupled to adenylate cyclase via G, and to phosphoinositide metabolism in a pertussis toxin-insensitive manner. J Biol Chem 264:3916, 1989 50. Wu H, Tumer JT, Halenda SP: Activation of phospholipase D by E-series prostaglandins in human erythroleukemia cells. J Pharmacol Exp Ther 258:607, 1991 5 1. Williams KA, Murphy W, Haslam RJ: Effects of activation of protein kinase C on the agonist-induced stimulation and inhibition of cyclic AMP formation in intact human platelets. Biochem J 243:667, 1987 52. Bennett WM: Renal vein thrombosis in nephrotic syndrome. Ann Intern Med 83577, 1975 53. Charo IF, Shak S, Kerasek MA, Davison PM, Goldstein IM: Prostaglandin I, is not a major metabolite of arachidonic acid in cultured endothelial cells from human foreskin microvessels. J Clin Invest 74:914, 1984 54. Nowak J, FitzGerald CA: Redirection of prostaglandin endoperoxide metabolism at the platelet-vascular interface in man. J Clin Invest 83:380, 1989 From www.bloodjournal.org by guest on February 6, 2015. For personal use only. 1993 82: 2704-2713 Prostaglandin E2 potentiates platelet aggregation by priming protein kinase C R Vezza, R Roberti, GG Nenci and P Gresele Updated information and services can be found at: http://www.bloodjournal.org/content/82/9/2704.full.html Articles on similar topics can be found in the following Blood collections Information about reproducing this article in parts or in its entirety may be found online at: http://www.bloodjournal.org/site/misc/rights.xhtml#repub_requests Information about ordering reprints may be found online at: http://www.bloodjournal.org/site/misc/rights.xhtml#reprints Information about subscriptions and ASH membership may be found online at: http://www.bloodjournal.org/site/subscriptions/index.xhtml Blood (print ISSN 0006-4971, online ISSN 1528-0020), is published weekly by the American Society of Hematology, 2021 L St, NW, Suite 900, Washington DC 20036. Copyright 2011 by The American Society of Hematology; all rights reserved.
© Copyright 2026