of Erythropoiesis in P-ThalassemialHemoglobin E Disease
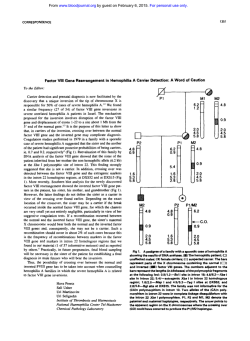
From www.bloodjournal.org by guest on February 6, 2015. For personal use only. Hydroxyurea Increases Hemoglobin F Levels and Improves the Effectiveness of Erythropoiesis in P-ThalassemialHemoglobin E Disease By Suthat Fucharoen, Noppadol Siritanaratkul, Pranee Winichagoon, Jew Chowthaworn, Wipapun Siriboon, Wanna Muangsup, Suchet Chaicharoen, Nalinee Poolsup, Busaba Chindavijak, Pensri Pootrakul, Anong Piankijagum, Alan N. Schechter, and Griffin P. Rodgers * 8% ( P Hydroxyurea (HU) is one of several agents that have been shown t o enhance hemoglobin (Hb) F levels in patients with sickle cell disease and may be useful as a therapy for /3globinopathies. However, limited information exists on the effects of HU in patients with thalassemia. Accordingly, we examined the hematologic effects of orally administered HU in 13 patients with /3-thalassemialHb E, including four patients who had been splenectomized.These patients were treated with escalating doses (final range, 10 t o 20 mg/kg/ d) for 5 months and were observed in the outpatient hematology clinic every 2 t o 4 weeks. Complete blood counts including reticulocyte counts, amounts of Hb E and Hb F, 'y:*y and a:non-a globin biosynthetic ratios were evaluated before and during treatment. Almost all patients responded with an average increase of 33% in Hb F levels, from a mean (*SDI of 4 2% 11% t o 56% 2 8% ( P < .0001), and areciprocal decline in thepercentage of Hb E from 59% k 9% t o &% .001). Reticulocytosiswas decreasedfrom a mean (+SDI of 18.0% 15.6% t o 11.7% k 9.1% ( P < .05); there was also a slight (10%) but statistically significant increase in hemoglobin levels and an improved balance in a:non-a globin chains ratios. The side effectswere minimal in most patients, although these patients tended t o tolerate a lower dose of HU before significant myelosuppression than has been ourprevious experience in sickle cell disease. Onesplenectomized patient died of sepsis during the trial. We conclude that increased HbF production in fi-thalassemia/Hb E patients, with an improvement in thea:non-a globin ratios and, probably, the effectiveness of erythropoiesis, can be achieved using HU. Longer trials of HU in this population, including at other dosesand in combination with other agents, appear warranted. This is a US government work. Thereare no restrictions on its use. T in patients with @-thalassemiaand sickle cell anemia, which could be a therapeutic approach for these patients.1°12 Among these agents, hydroxyurea (HU), acell cycle-specific agent that blocks DNA synthesis, has been shown to enhance Hb F levels in both nonhuman primates and in patients with myeloproliferative and sickle cell Although early results in thalassemia have been variable," recently it has been reported that virtually all of 14 patients with sickle cell/ @-thalassemiatreated with HU have had an increase in Hb F levels and an apparent decrease in crisis freq~encies.'~ In this study, we examined the hematologic effects of orally administered HU in 13 patients with P-thalassemialHb E. * HALASSEMIA is a heterogeneous group of genetic defects that results in defective globin synthesis. It is the most common genetic disorder among the people living in Southeast Asia; a-thalassemia, @-thalassemia, hemoglobin (Hb) E, and Hb Constant Springs (CS) are prevalent. The gene frequencies of a-thalassemia reach 20% to 30% in Northern Thailand and Laos. Frequencies of @-thalassemia gene vary between 1% and 9%. Hb E is the hallmark of Southeast Asia, attaining a gene frequency of 50% to 60% at the junction of Thailand, Laos, and Cambodia. Hb CS frequencies vary between 1% and 8%.'z2 These abnormal genes in different combinations lead to over 60 thalassemia syndromes. Interaction between @-thalassemia and Hb E genes leads to homozygous @-thalassemia and P-thalassemia/Hb E diseases that are major @-thalassemiasyndromes in this region. P-thalassemialHbE can be as severe as homozygous @-thalassemia. Indeed, hemoglobin levels in 802 cases of @-thalassemia/HbE disease at steady state varied from 2.6 to 13.3 g/dL, with an average of 7.7 g/dL.3-5 Many factors may contribute to this heterogeneity, such as concomitant inheritance of a-thalassemia, which can ameliorate the severity of @-thalassemia.6Recently, we found that the inheritance of a @-thalassemiachromosome with the Xmn I cleavage site at position - 158 of the 'y-globin gene that was linked to the haplotype -+ - ++ was associated witha milder anemia, as in the case of homozygous pthalassemia.' Increased expression of the 'y-globin gene and higher production of hemoglobin F, which could reduce the overall globin chain imbalance, were also associated with homozygosity for the Xmn I cleavage site and, thus, with less severe anemia. The finding that higher production of Hb F paralleled higher hemoglobin levels in P-thalassemia/Hb E patients was similar to findings in other @-thalassemiadisease and sickle cell During the last 10 years, there have been several studies attempting to enhance Hb F production Blood, Vol 87, No 3 (February l), 1996: pp 887-892 * PATIENTSELECTION AND METHODS Patients were considered eligible for the study if they exhibited signs of moderate to severe thalassemia, including evidence of osteoFrom the Thalassemia Center, Division of Hematology, Department of Medicine, Faculty of Medicine, Siriraj Hospital, Bangkok, Thailand; the Institute of Sciences and Technology for Research and Development, Bangkok, Thailand; the Department of Pharmacy, Faculty of Pharmacy, Mahidol University9Bangkok, Thailand; and the Laboratory of Chemical Biology, National Institute of Diabetes, Digestive and Kidney Diseases, Bethesda, MD. Submitted September 26, 1994; accepted August 30, 1995. Supported in part by the Commission of the European Communities, Science and Technology for the Development Program, Contract No. TS3*-CT92-0081; and the Prajadhipok-Rambhai Bami Foundation. Address reprint requests to Gri@n P. Rodgers, MD, Chief; Molecular Hematology Section, Laboratory of Chemical Biology, Bldg 10, Room 9N-318,IO Center Dr MSC-1822, Bethesda, MD 20895-1822. The publication costs of this article were defrayed in part by page charge payment. This article must therefore be hereby marked "advertisement" in accordance with 18 U.S.C. section 1734 solely to indicate this fact. This is a US govemment work. There are m restrictions on its use. 00oS-4971/96/8703-0$0.00/0 887 From www.bloodjournal.org by guest on February 6, 2015. For personal use only. FUCHAROEN ET AL 888 porotic bone disease, intermittent transfusion-dependency, and hemochromatosis. Thirteen patients with p-thalassemialHb E-nine nonsplenectomized and four splenectomized cases-were recruited in this study. The patients, six menand seven women,rangedin age from 18 to 55 years (average age, 34 years). All of them were treated at the outpatient hematology clinic of Siriraj Hospital (Bangkok, Thailand) with regular followup every 2 to 4 weeks. An exemption for treatment with an investigational new drug was obtained from the Food and Drug Administration. The treatment protocol was approved separately by clinical research subpanels at Siriraj Hospital, Mahidol University (Bangkok, Thailand) and the National Heart, Lung and Blood Institute (Bethesda, MD). After informed consent was obtained, baseline and serial hematologic tests and measurements were performed. Hematologic data, Hb analysis, and reticulocyte count were determined by conventional methods. Percentages of Hb E and Hb F were obtained by elution after cellulose acetate electrophoresis. Determination ofthe ratio was obtained from the globin chains separated by Triton X-100 acid urea polyacrylamide gel electrophoresis.16In vitro globin chain synthesis was determined from the reticulocytes of heparinized bloodas previously described," and theglobin chains were separated using a Fast Protein Liquid Chromatography (FPLC) system (Pharmacia Biotech, Piscataway, NJ). Complete blood counts including reticulocyte count, the amounts of Hb E and Hb F, serum tests indicating the level of renal and hepatic function, and ' y : * y and ct:non-ct ratios were evaluated before and serially during treatment. Restriction endonuclease analysis of genomic leukocyte DNA was performed to assess the alphaglobin genotype'"'' and the haplotype of the beta-globin gene cluster.' The patients were initially treated with a dose of HU of approximately 10 mgikg (to nearest 250-mg capsule). This dose was maintained for approximately 10 weeks, at which point, in the absence of hematologic toxicity, the dose was increased to 20 mgikg and continued for an additional 10 weeks. Therapy was discontinued at the end of the 20-week trial. Evidence of hematologic suppression was defined as an absolute reticulocyte count less than 50,00O/pL, a white blood cell count less than 3,OOO/pL (or neutrophil count less than l,OOO/pL), or a platelet count less than 100,00O/pL. Statistical methods to detect the significance of the differences in the individual pairs of data included the paired Student's f test for data with a Gaussian distribution and Mann-Whitney U test for data with a non-Gaussian distribution. Repeated measures-analysis of variance (ANOVA) with Bonferroni's correction-was also used to analyze multiple measurements on the same individual. Univariate and multivariate analyses were used to describe the strength of relationships between variables.'') RESULTS Fetal hemoglobin responses. Overall, patients responded with a 32.5% increase in fetal hemoglobin from a mean (?SD) of 42% ? 11% to 56% -c 8% (P < .0001). As indicated in Table 1, while there was a spectrum in the Hb F responses, only 1 of the 13 patients (patient 8) did not show an increase in Hb F expressed in grams per deciliter and, thus, would be considered a nonresponder. Hb E levels declined from 59% t 9% to 49% t 8% (P < .001). A sample of the reciprocal changes in the levels of Hb E and Hb F in one patient is shown in Fig 1, whilethemean changes for the entire group of 13 patients are depicted in Fig 2. The increase in Hb F due to increased y-globin chain synthesis led to improvement in the a:non-cu ratios, and there were no significant changes in the G y : A y ratio with this enhanced production of fetal hemoglobin (Table 2). We were unable to detect an absolute relationship between the initial percent Hb F, Gy:Ay ratio, @-globinhaplotype, a-globin genotype, or basal level of renal or hepatic function with the magnitude of the Hb F response. Fetal hemoglobin was detectedin all of the red cells (F cells) before and during therapy by the modified Kleihauer acid-elution technique." Thus, we estimate that with treatment the proportion of Hb F per red cell increased by about one third. Hematologicresponses. There was a small but statistically significant increase in the level of hemoglobin, from 6.6 ? 0.6 g/dL to7.3 t- 0.7 g/dL (Student's t-test, P < .02). When a more conservative method of analysis (repeated measures-ANOVA with Bonferonni's correction) was applied, taking into account the multiple measurements of hemoglobin before andat entry, this change inhemoglobin remained statistically significant (F = 6.95, P = .15; with Bonferroni correction, P < .05). There was also a moderate decrease in bilirubin (4.9 ? 1.6 mg/dL to 3.5 ? 1.9 mg/dL, P < ,001) and the reticulocyte count (18.0% ? 15.6%to 1 1.7% ? 9.1 %, P < .05). As noted in previous clinical trials, HU therapy was associated with a marked increase in the meanred cell volume (MCV) andhemoglobin content (MCH), while there was no net change in the meancorpuscular hemoglobin concentration, which iscalculated from these two indices. Changes in these parameters correlated with the increments in fetal hemoglobin augmentation ( r = .61, P = .03; Table 1). A summary of all patients' hematologic profiles is shown in Table 2. Subset analysis indicated that there were no statistically significant differences before or after HU treatment in any of these listed parameters between the splenectomized and nonsplenectomized patients. During this 20-week trial, therewas indication ofmild hematopoietic toxicity in the majority of our patients. The maximal average tolerable dose in these patients was 15 mg/ kg/d (range, 11.1 to 17.9 mg/kg/d). There was a significant decline in the white blood cell (WBC) count (average decrease, approximately 50%) in 6 of 13 patients, in the platelet count (average decrease, approximately 30%) in 3 of 13 patients, and in the reticulocyte count in 1 of 13 patients. It should be notedthat the nadir of these counts in most patients was at a level above what wasconsidered significant hematologic suppression (see Patient Selection and Methods), and only three patients required a dose adjustment due to WBC count less than 3,00O/pL. These declines in blood cell counts occurred precipitously within the 2 weeksbetween clinic visits and are to be distinguished from the moregradual decline in the WBC and reticulocyte counts occurring over the 5-month treatment period (Table 2). Thus, it may be concluded that requisite doses of HU tostimulate fetal hemoglobin levels in patients with P-thalassemiab E are at or near the threshold for myelosuppression. Clinical effects. In addition to the modest increase in the hemoglobin, most patients described an increase in exercise tolerance and sense of well-being in comparison with their symptoms before treatment. Because this wasnot a controlled trial, we cannot formally exclude a placebo effect. Side effects were minimal in most patients, except for the From www.bloodjournal.org by guest on February 6, 2015. For personal use only. HU IN P-THALASSEMINHbE DISEASE 889 Table 1. Changes in the Level of Hemoglobin and Absolute Amount of Hb F in 13 Patients With pThalassemialHbE During 5 Months of HU Treatment HbF (g/dL) Hemoglobin (g/dL) Patient 6.6 30/F 7.6 6.0 1. P.N.' 6.9 2. P.P.* 6.1 3. CS.' 6.9 4. T.S. 7.2 7.6 5.B.T. 6. V.N. 6.2 7. S.I.' 6.1 8. RN.' 4.8 9. I.J. 7.5 10.6.6M.I.' 11. B.C. 12. 7.1L.S. 13. 6.0 S S . Mean 2 SD Age (yr)/Sex 18/M 26/M 29/M 36/M 42/M 48/M 23/F 26/F 27/F 28/F 0-Day Pre 7.2 6.6 6.8 6.0 7.4 5.9 6.4 6.0 7.1 8.0 7.1 7.4 6.7 8.0 6.2 7.2 6.0 7.3 7.7 7.8 4.2 8.1 7.4 8.1 7.7 5 mo 0-Day 2 mo Pre 2.2 1.9 2.8 3.0 2.5 NAt 2.7 2.2 2.0 5.9* 4.0 2.2 1.9 2.6 2.5 2.4 2.6 1.8 2.7 3.4 3.2 3.4 2.0 4.0 3.0 3.2 3.5 3.6 3.4 2.4$ 4.1 2 mo 5 mo 3.2 2.6 3.4 3.3 3.6 4.4 3.2 1.9 4.4 NAt 2.5 34/F 42/F 6.51 2 0.59 6.56 2 0.83 6.91 2 1.07 7.25 2 0.63 2.60 2 0.57 2.85 2 0.75 3.51 2 0.73 3.67 2 0.65 The pretreatment value of hemoglobin is the average of three consecutive baseline values, while the 0-day value is the average of two determinations obtained within 2 weeks of initiation of HU. Abbreviations: Pre, pretreatment value; NA, not applicable. Splenectomized patient. t HU was stopped because the patient could not come for regular follow-up. Patient had upper respiratory tract infection, and 1 U of blood was given at the end of the third month of HU. § The last hematologic data were obtained 2 weeks before patient died. * anticipated changes in hematologic parameters, as described above. One splenectomized patient died in the last month of the trial because of septicemia after diarrhea. She had been on a stable dose of HU (14 mg/kg/d) for the preceding 3.5 months, which she tolerated well. Her W C count was 12,OOO/pL with 85% neutrophils when she was brought to the hospital in a semicomatose condition, and she died within a few hours after her arrival at the hospital. Hemoculture revealed Streptococcal pneumococci in all three blood samples. This specific complication should beviewed in the context of an underlying significantly increased incidence of fatal pneumococal bacteremia among splenectomized pthalassemia patients in Southeast Asia, which we have previously reported." DISCUSSION Numerous studies have demonstrated that HU can enhance Hb F production in patients with sickle cell anemia. However, there has been limited and mainly negative information on the effect of HU in thalassemia." Two recent reports of HU therapy of P-thalassemia intermedia suggest modest beneficial effect^:^.'^ while we have observed several patients with P-thalassemia with the IVS-654 mutation who have responded to HU with increased &globin ~ynthesis.'~ Recently, HU has been shown to be of potential benefit in sicklelp-thalassemia double heterozygotes, although no effect on hemoglobin levels was achieved.I5The two major hemoglobin components in patients with p-thalassemia/Hb E disease are Hb E and Hb F, and the levels of Hb F can vary from 30% to 70%.' Recent studies have demonstrated that there is a good correlation of hemoglobin levels with the amount of Hb F production in certain groups of patients with @'-thalassemia/Hb E.5.7 Our results demonstrated that increased Hb F production in patients with P-thalassemiakIb E associated with an improvement in the adnon-a globin production can be achieved using HU. Red cell MCV and MCH were also increased in all subjects (Table 2). Although there were no dramatic changes in the hemoglobin levels, the percentage and the absolute amount of reticulocytes were decreased, which reflects the improvement in bone marrow stress due to tissue anoxia. Alternatively, this decrease in reticulocyte count may reflect marrow toxicity. However, the fact that the reticulocytes decreased after the hemoglobin increased and that the patients exhibited a decrease in serum bilirubin and lactic dehydrogenase (LDH; data not shown) would support the improved erythropoiesis hypothesis. The temporal relationship between the increase in the percent HbF (and the reciprocal decrease in percent HbE) and the increase in total hemoglobin (Fig 2) is also consistent with this view. Bone marrow failure due to aplastic crisis (and presumably secondary to myelotoxicity) in the severe &globin disorders may be accompanied by a transient decrease in the reticulocyte count and bilirubin and LDH levels, and a transient increase in Hb F levels.26However, such effects are most often accompanied by more profound declines in the reticulocyte count (often to zero) and a concomitant decrease in hemoglobin levels, while the mean (red) cell volume remains unchangedZ6-findings in marked contrast with our observations. Finally, we observed that the hemoglobin levels and red cell indices in these patients returned to baseline levels within 8 weeks of cessation of HU (data not shown), again From www.bloodjournal.org by guest on February 6, 2015. For personal use only. 890 FUCHAROEN ET AL IA was not possible to study F-reticulocyte levels because of technical limitations in our method. The enumeration of F cells by acid-elution shows that all red cells in patients with ,@"thalassemia/Hb E give a positive reaction with heterochromatic staining for Hb F. Ideally, it would be necessary to use immunofluorescence staining and flow cytometry to distinguish increases in the F-cell production and/or in the quantity of Hb F per F cell. --I--Hemoglobin (@dl) 6 . 5 ' m ' ' z . 1 5 -100 0 100 2 Treatment Day W 16 'O U. . n I z 7 z 50 - A I I 1 1 1 1 1 1 1 , 1 , 6 8 10 12 14 16 18 20 22 24 " ' . . ~ . . . . ~ 8 6.5 5 -100 5 J I 0 2 4 . 5 " 40 W 40 . I I 0 100 30 200 0 m 1 5.5 Treatment Day Fig 1. Effect of HU onhematologicvalues in a patient with pthalassemia/Hb E. (A) Sequential change in hemoglobin values. (B) Reciprocal changes in the proportion of Hb F. reflecting that the changes in hematologic parameters were coincident with HU therapy. It is noteworthy that in these patients, the fetal hemoglobin and total hemoglobin levels continued to increase during treatment, and thus, the absolute improvement in the level of ineffective erythropoiesis and the effects on the characteristic peripheral hemolysis of these patients achievable with HU cannot be stated definitively. Indeed, long-term HU treatment of patients with sickle cell anemia indicates that a continued improvement in Hb F levels and in the hemoglobin values can bedemonstrated for up to a year while ona stable dose ofHU (G.P.R., unpublished observations, December 1 994). Fetal hemoglobin levels in patients with beta-globin disorders are determined by three factors: F-cell production, the amount of Hb F per F cell, and the preferential survival of F cells.27We had previously shown that during short-term trials of HU in patients with sickle cell anemia, F-cell production, as estimated by the F-reticulocyte levels, accounted for 70% of the increase in Hb F 1e~els.I~ Unfortunately, it ~ 1 50 2 n I ~ "-a"% HbE WW ~ 4.5 Week on Hydroxyurea Fig 2. Effect of HU onhematologicvaluesin 13 patients with p-thalassemialHb E.Theaveragesandstandarddeviationsinthe percentages of (A) Hb F, (B) Hb E, and (C1 total hemoglobin in this group of patients duringHU treatment is shown. ~ From www.bloodjournal.org by guest on February 6, 2015. For personal use only. HU THERAPY IN P-THALASSEMINHbEDISEASE 891 Table 2. HematologicEffects of HU in 13 Patients With B-ThalassemialHbE Test Hb (g/dL) MCV (fL) MCH (pg) WBC (//L) Reticulocytes (%) nRBC (X103/pL) = y A y ratio a:Non-a globin Baseline Value (mean 2 SE) After 5 Months HU (mean 2 SE) P Value 7.3 2 0.6 6.6 2 0.6 <.05 64.8 t 7.1 74.2 2 6.2 < .05 19.4 t 1.4 23.3 t 2.0 <.05 13,900t 9,500 9,500t 6,300<.05 18.0 f 15.6 <.05 11.7 t 9.1 2.26 t 3.24 3.04 2 4.52 .l5 1.8 t- 0.7 .53 0.6 1.4 2.6 t- 0.5 <.02 0.5 2.1 Baseline values were obtained within 1 month before the initiation of H U treatment; P value determined by two-tailed Student's t-test. Abbreviation: nRBC, nucleated red blood cell count. Because of the short period of this clinical trial, it is very difficult to draw conclusions on the clinical response to HU treatment. Most of the patients reported feeling better; side effects generally have been minimal. In this group of patients who exhibit a @-thalassemiaintermedia phenotype, even a modest increase in red cell production with coincident suppression of bone marrow turn-over might be highly beneficial; the need for transfusion support might be delayed or eliminated, Further studies will be required to evaluate the long-term toxicity and benefit to the patients. It is notable that these patients with P-thalassemialHbE seem to tolerate a lower dose of HU than has been reported in patients with sickle cell anemia'3314before hematopoietic toxicity is evident. Nonetheless, we have treated two Chinese patients with @-thalassemiaintermedia for periods of 1 and 2 years both on a dose of HU of 8 mgkgld, which has led to a 50% and 100% increase, respectively, in their baseline hemoglobin values.25Based on these results expanded studies of HU in patients with P-thalassemia seem warranted, especially for longer periods of time and at other doses. Moreover, clinical trials of other agents such as butyric acidz8and its derivatives29.30 alone and in combination with HU3' or erythropoietin3' should be considered to identify optimal regimens in this patient population. ACKNOWLEDGMENT We acknowledge Bristol-Myers Squibb (Princeton, NJ) for the contribution of HU. We also thank Drs Marvin Podgor and Craig Stotts for advice with statistical methods. REFERENCES 1. Wasi P, Na-Nakron S, Pootrakul S , Sookanck M, Distha- songehan P, Pornpatkul M, Panich V: Alpha-and beta-thalassemia in Thailand. Ann N Y Acad Sci 165:60, 1969 2. Fucharoen S , Winichagoon P Hemoglobinopathies in Southeast Asia. Hemoglobin 11:65, 1989 3. Fucharoen S, Winichagoon P, Pootrakul P, Wasi P: Determination for different severity of anemia in thalassemia: Concordance and discordance among sib pairs. Am J Med Genet 19:39, 1984 4. Wasi P, Pootrakul P, Fucharoen S, Winichagoon P, Wilairat P, Promboon A: Thalassemia in Southeast Asia: Determinants of different degrees of severity of anemia in Thalassemia. Ann N Y Acad Sci 445119, 1985 5. Fucharoen S , Winichagoon P, Pootrakul P, Piankijagum A, Wasi P Variable severity of Southeast Asian 8-thalassemialHb E disease. Birth Defects 23A:41, 1988 6. Winichagoon P, Fucharoen S , Weatherall DJ,WasiP: Concomitant inheritance of a-thalassemia in P-thalassemia/Hb E. Am J Hematol 20:217, 1985 7. Winichagoon P, Thonglairoam V, Fucharoen S , Wilairat P, Fukumaki Y, Wasi P: Severity differences in P-thalassemiahaemoglobin E syndromes: Implication of genetic factors. Br J Haematol 83:633, 1993 8. Thein SL, Wainscoat JS, Sampietro M, Old JM, Capellini D, Fiorelli G, Modell B, Weatherall DJ: Association of thalassemia intermedia with beta-globin gene haplotype. Br J Haematol 65:367, 1987 9. Perrine R P , Pembrey ME, John P, Perrine S , Shoup F: Natural history of sickle cell anemia in Saudi Arabs. A study of 270 subjects. Ann Intern Med 88:1, 1978 10. Ley TJ: The pharmacology of hemoglobin switching of mice and men. Blood 77:1146, 1991 11. Stamatoyannopoulos JA, Neinhuis AW: Therapeutic approaches to hemoglobin switching in treatment of hemoglobinopathies. Annu Rev Med 43:497, 1992 12. Rodgers GP: Pharmacological modulation of fetal hemoglobin, in Embury SH, Hebbel RP, Mohandas N, Steinberg MH (eds): Sickle Cell Disease: Basic Principles and Clinical Practice. New York, NY, Raven, 1994, p 829 13. Rodgers GP, Dover GJ, Noguchi CT, Schechter AN, Nienhuis AW: Hematologic responses of patients with sickle cell disease to treatment with hydroxyurea. N Engl J Med 332:1037, 1990 14. Charache S , Dover GJ, Moore RD, Eckert S, Ballas SK, Koshy M, Milner PF, Orringer EP, Phillips G Jr, Platt OS: Hydroxyurea: Effects on hemoglobin F production in patients with sickle cell anemia. Blood 79:2555, 1992 15. VoskandouE, Kalotychou V, Loukopoulos D: Clinical and laboratory effects of long-term administration of hydroxyurea to patients with sickle celllP-thalassemia. Br J Haematol 89:479, 1995 16. Marengo-Row AJ: Rapid electrophoresis and quantitation of hemoglobins on cellulose acetate. J Clin Pathol 18:790, 1965 17. Alter BP, Goff SC, Efremov GD, Gravely ME, Huisman THJ: Globin chain electrophoresis: A new approach to the determination of the ' y l A y ratio in fetal hemoglobin andto studies of globin synthesis. Br J Haematol 44527, 1980 18. Weatherall DJ, Clegg JB: Structure, function, genetics and biosynthesis of hemoglobin,in Weatherall DJ, CleggJB (eds): The Thalassemia Syndromes. Oxford, UK,Blackwell Scientific, 1981, p 19 19. Winichagoon P, Higgs DR, Goodboum SEY, Clegg JB, Weatherall DJ: The molecular basis of a-thalassemia in Thailand. EMBO J 3:181, 1984 20. Remington RD, Schork MD: Statistics With Applications to the Biological and Health Sciences. Englewood Cliffs, NJ, PrenticeHall, 1970 21. Sanguantsermsri T: Resistance of hemoglobin Bart's to acid elution. J Med Assoc Thai 61:62, 1978 22. Fucharoen S, Piankijagum A, Wasi P: Deaths in P-thalassemia/Hb E patients secondary to infections. Birth Defects 23:495, 1988 23. Hajjar F M , Pearson HA: Pharmacologic treatment of thalassemia intermedia with hydroxyurea. J Pediatr 125:490, 1994 24. Bachir D, Galacteros F: Potential alternatives to erythrocyte transfusion in hemoglobinopathies: Hydroxyurea, erythropoietin, butyrate derivatives, blood substitutes. Transfus Clin Biol 1:35, 1994 25. Huang SZ, Zeng YT, Lu ZH, Ren ZR, Schechter AN, Rodgers From www.bloodjournal.org by guest on February 6, 2015. For personal use only. 892 GP: Hydroxyurea therapy in beta-thalassemia intermedia: Improvement in hematological parameters due to enhanced beta-globin synthesis. Br J Haematol 90557, 1995 26. Dover GJ, Boyer SH,Charache S , Heintzelman K: Individual variation in the production and survival of F-cells in sickle cell disease. N Engl J Med 299:1428, 1978 27. Goldstein AR, Anderson MJ, Serjeant GR: Parvovirus associated aplastic crisis in homozygous sickle cell disease. Arch Dis Child 62585, 1987 28. Penine SP, Ginder GD, Faller DV, et al: A short-term trial of butyrate to stimulate fetal-globin-gene expression inthebetaglobin disorders. N Engl J Med 328:81, 1993 FUCHAROEN ET AL 29. Collins AF, Pearson HA, Giardina P, McDonagh KT, Brusilow SW, Dover GJ: Oral sodium phenylbutyrate therapy in homozygous beta thalassemia: A clinical trial. Blood 85:43, 1995 30. Fibach E, Prasanna P, Rodgers GP, Samid D: Enhanced fetal hemoglobin production by phenylacetate and 4-phenylbutyrate in erythroid precursors derived from normal donors and patients with sickle cell anemiaandbeta-thalassemia. Blood 82:2203,1993 31. Rodgers GP, Dover GJ, Uyesaka N. Noguchi CT, Schechter AN, Nienhuis AW: Erythropoietin augments the fetal in sickle cell patients. N hemoglobin response to hydroxyurea Engl J Med 328:75, 1993 From www.bloodjournal.org by guest on February 6, 2015. For personal use only. 1996 87: 887-892 Hydroxyurea increases hemoglobin F levels and improves the effectiveness of erythropoiesis in beta-thalassemia/hemoglobin E disease S Fucharoen, N Siritanaratkul, P Winichagoon, J Chowthaworn, W Siriboon, W Muangsup, S Chaicharoen, N Poolsup, B Chindavijak, P Pootrakul, A Piankijagum, AN Schechter and GP Rodgers Updated information and services can be found at: http://www.bloodjournal.org/content/87/3/887.full.html Articles on similar topics can be found in the following Blood collections Information about reproducing this article in parts or in its entirety may be found online at: http://www.bloodjournal.org/site/misc/rights.xhtml#repub_requests Information about ordering reprints may be found online at: http://www.bloodjournal.org/site/misc/rights.xhtml#reprints Information about subscriptions and ASH membership may be found online at: http://www.bloodjournal.org/site/subscriptions/index.xhtml Blood (print ISSN 0006-4971, online ISSN 1528-0020), is published weekly by the American Society of Hematology, 2021 L St, NW, Suite 900, Washington DC 20036. Copyright 2011 by The American Society of Hematology; all rights reserved.
© Copyright 2026