Selective impairment of T lymphocyte activation
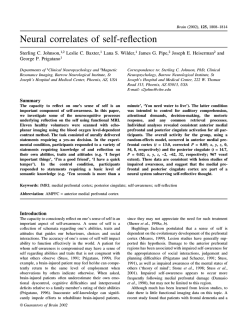
Clin Exp Immunol 1993; 94:38-42 Selective impairment of T lymphocyte activation through the T cell receptor/CD3 complex after cytomegalovirus infection M. TIMON, A. ARNAIZ-VILLENA, J. RUIZ-CONTRERAS*, J. T. RAMOS-AMADOR*, A. PACHECOt & J. R. REGUEIROt Departments of Immunology and *Paediatrics, Hospital 12 de Octubre Madrid, and tDepartment of Immunology, Universidad Complutense, Madrid, Spain (Acceptedfor publication 15 April 1993) SUMMARY Cytomegalovirus (CMV) infection is reported to cause transient immunosuppression in man. In this study we have analysed the effect of CMV on T lymphocyte function in 29 children diagnosed for acute CMV infection. Peripheral blood mononuclear cells (PBMC) obtained from the patients showed a significant specific impairment in their proliferative response to enterotoxins A and Cl, to concanavalin A and to the anti-CD3 MoAb OKT3. The impaired responses were corrected with exogenous IL-2. In contrast, stimulation using phytohaemagglutinin, as well as activation signals delivered through the surface molecules CD26 or CD28, elicited normal proliferative responses in CMV PBMC. The results indicate that the T cell anergy associated with CMV infection is restricted to the T cell receptor/CD3 activation pathway. Keywords T lymphocyte cytomegalovirus anergy T cell receptor activation disease CD28, CD69), lectins (phytohaemagglutinin (PHA), concanavalin A (Con A), pokeweed mitogen (PWM)) or reagents that bypass membrane signals, like phorbol esters and calcium ionophores [7]. The results indicate that the T cell anergy associated with CMV infection is restricted to the T cell receptor/CD3 activation pathway. INTRODUCTION Human cytomegalovirus (CMV) is an ubiquitous, potentially pathogenic herpesvirus, usually associated with a carrier state, with minor or no symptomatology in non-immunosuppressed hosts [1]. CMV causes damage only if the host immune response is immature or compromised, as in neonates, transplant recipients, or patients with AIDS [2]. Some characteristic features of the virus are its ability to establish latency for the life of the individual, its ability to bind the host protein f2-microglobulin, and to have in its genome a gene which, if expressed, would have considerable homology with HLA class I-like molecules [3]. Acute infection by CMV frequently results in depressed cellular immune function, as evidenced by a decreased lymphoproliferative response to mitogens and viral antigens [4,5], and diminished reactivity to skin tests [4]. Reports have shown that CMV mononucleosis patients have elevated levels of suppressor-cytotoxic T cells (CD8 +), as well as inverted ratios of helper to suppressor T cells compared with normal individuals [6]. However, the precise mechanism underlying this CMV-induced T cell anergy is mostly unknown. In the present study a further analysis of this CMVassociated T lymphocyte function impairment was carried out PATIENTS AND METHODS Patients and control donors Twenty-nine patients (10 female and 19 male, aged between 3 months and 7 years) were included in the study, and analysed during: (i) the acute symptomatic phase (n = 7, studied from 7 to 30 days after onset of symptoms); (ii) the latent asymptomatic period (n = 22, studied beyond 50 days after the onset of symptoms; in seven of them the exact date of infection was unknown, and the carrier status was diagnosed by urine CMV isolation and CMV-specific antibodies (negative IgM, positive IgG)). CMV infection was diagnosed by clinical, serological and virological criteria [8]. Patients in the acute phase had a heterophile-negative mononucleosis characterized by protracted fever, peripheral blood lymphocytosis, hepatosplenomegaly, small anterior cervical lymphadenopathy, and CMVspecific IgM antibodies [8,9]. IgM- and IgG-class antibodies to the late antigen of CMV were detected using an ELISA [10]. Antibody titres of 40 (IgM)/23 (IgG) or greater were considered positive. Sixteen of the 29 patients tested had CMV isolated from urine, three of them also in the pharynx. Control donors were 29 healthy individuals of comparable age and sex distribution, with no history of CMV mononucleosis. in a sample of 29 children after an acute CMV infection. Peripheral T lymphocytes were activated in a polyclonal fashion by using antigens (bacterial enterotoxins), antibodies directed against different monomorphic surface molecules (CD3, CD26, M.T. and A.A.-V. are joint first authors. Correspondence: A. Arnaiz-Villena, Inmunologia, Hospital 12 de Octubre, Universidad Complutense. 28041 Madrid. Spain. 38 T lymphocyte anergy in CMV infection 39 Table 1. Peripheral blood mononuclear cell phenotype of cytomegalovirus-infected patients Patients (n = 29) Monoclonal antibody (subset) Lymphocytes Total lymphocytes/pl OKTl1 (total Tcells+NK cells) OKT3 (mature T cells) Leu-4 (mature T cells) OKT4 (helper T cells) OKT8 (cytotoxic/suppressor T cells) DR (mature B cells + activated T cells) OKB7 (B cells) Leu-7 (NK cells) Monocytes Total monocytes/ilOKM14 OKT4 DR Controls (n = 29) CD equivalent Per cent of total cells Absolute no. per il Per cent of total cells Absolute no. per /l CD2 CD3 CD3 CD4 CD8 CD21 CD57 81 +2 64+ 1** 69+2 34+2*** 26+ 1 20+ 1 15+ 1** 10+ 1** 5606+435*** 4552+382*** 3575+ 298** 3874+318*** 2001 + 182 1400 + 117** 1153 + 136** 834+92*** 570+92 84+2 72 + 2 73+2 44+2 28 + 2 18 +0 10+ 1 15+ 1 3394+ 150 3002+ 143 2421 + 115 2447+ 105 1518+98 916 + 70 639 +43 360+35 526+58 CD14 CD4 - 86 + I*** 24+4*** 82+3*** 683 + 71 577 + 65** 202+39*** 596+83 97+0 53+5 94+ 1 848 + 56 823 + 54 471 +56 779+57 Results are expressed as mean + s.e.m. *P<0-05 compared with normal controls. **P<0-01 compared with normal controls. ***P < 0-001 compared with normal controls. NK, Natural killer. Immunofluorescence staining andflow cytometry Whole blood samples were stained by direct immunofluorescence with different MoAbs, their erythrocytes lysed and the remaining cells fixed for flow cytofluorometry analysis by standard techniques (Q-Prep; Coulter, Hialeah, FL) [11]. The results were recorded as the percentage of positive cells for each MoAb within the lymphocyte population (electronically gated by size/complexity criteria). A logarithmic scale of fluorescence intensity was used, and cells whose intensity exceeded the upper limit of values for the negative control were considered positive. The cells were stained with the following MoAbs: OK series from Ortho Pharmaceuticals (Raritan, NJ), and Leu-7 from Becton Dickinson (Sunnyvale, CA). Anti-CD25 (IL-2-Ra) MoAb was purchased from Coulter, and anti-CD28 (IOT28) from Immunotech. The expression level of the different molecules was simultaneously recorded in arbitrary units for comparative purposes only. Isolation of lymphocytes andfunctional tests Peripheral blood mononuclear cells (PBMC) were isolated from heparinized peripheral blood by density gradient centrifugation and Ficoll-Hypaque (Lymphoprep, Nycomed AS, Oslo, Norway) [12] and resuspended in RPMI 1640 (Flow, Flow Labs, UK) supplemented with 10% fetal calf serum (FCS; Flow), 1% L-glutamine (200 mM) (Flow). PBMC (1 x 105 cells/well) were cultured in triplicate in complete medium in 96-well roundbottomed microwell plates (Nunc, Roskilde, Denmark). The following reagents or their combinations were used: anti-CD3 (OKT3) 12-5 ng/ml, anti-CD28 (Kolt-2) 50 ng/ml, Con A (Calbiochem, La Jolla, CA) 10 pg/ml, PHA (Difco, Detroit, MI) 10 jug/ml, phorbol myristate acetate (PMA; Sigma, St Louis, MO) 1-10 ng/ml, ionomycin (Calbiochem, La Jolla, CA) 1 yzM, rIL-2 (Genzyme, Boston, MA) 100 U/ml, PWM (Difco) 1% v/v, anti-CD26 (TAI, Coulter) 0-2 yg/ml, anti-CD69 (Leu-23, Becton Dickinson) 0-25 pg/ml. The plates were incubated at 37 C for 90 h in a humidified atmosphere containing 5% CO2 in air. Cell proliferation was measured by 3H-thymidine (3H-TdR) incorporation (1 pCi/well; sp. act. 25 Ci/mmol; Amersham, UK) during the last 15-18 h of culture. The samples were washed and harvested on glass fibre filters, resuspended in a liquid scintillation mixture, and the incorporated radioactivity determined in a liquid scintillation counter (LKB Betaplate). Results are expressed as ct/min x 10-3 3H-TdR. For cytokine determination, supernatants of 1 x 105 PBMC/well from patients and controls were collected at day 5 after stimulation and assayed for IL-2 activity. Cytokine concentrations were measured in each supernatant using ELISA kits, according to the manufacturer's technical guidelines (R & D Systems, Minneapolis, MN). Statistical analysis Mann-Whitney U-test (Sigma Horus Hardware, New York, NY) was used for all comparisons between patients and normal controls. Only P values below 0 05 were considered significant. Data are presented as mean + s.e.m. The s.e.m. of the mean was calculated as s.d./I/n. RESULTS Peripheral blood mononuclear cell phenotype (Table 1) The main significant differences between CMV patients and controls were as expected and already described, increased numbers of total and mature T cells (CD2, CD3), mostly due to the CD8 subset, as well as of total B cells (CD2 1), and decreased monocytes (CD14). The percentage of CD4 T cells was, as a consequence, significantly reduced. In addition, a higher expression of CD8 molecules on the surface of CMV patients' T M. Timon et al. 40 Table 2. Stimulation of cytomegalovirus (CMV) peripheral blood lymphocytes with antigens and lectins Table 3. Stimulation of cytomegalovirus (CMV) peripheral blood lymphocytes with antibodies against surface molecules 3H-TdR incorporation (ct/min x 10 - 3) 3H-TdR incorporation (ct/min x 10 - 3) Stimulus Medium rI L-2 PMA Enterotoxin A Enterotoxin C I PHA PHA + rIL-2 PHA + PMA Con A Con A+ rl L-2 Con A+PMA PWM PWM + rlL-2 PWM+PMA lonomycin + PMA Patients (n = 29) Controls (n = 29) significance 1+0 13+2 5+1 36 +4 11+3 113+15 174 + 18 177+ 19 56 +9 159 + 18 116+ 17 15 + 2 14+2 40 + 5 148 + 30 2+0 11+1 7+0 70 + 7 30 +4 141 + 19 228 + 15 189 + 18 110+ 13 166 + 16 161 +27 29 + 3 32 +4 71+6 193 + 27 NS NS P<0.05 P<0 001 P<0 001 NS P<0.05 NS P<0.001 NS NS P<0-001 P<000I P<0.001 NS Statistical Stimulus Medium rlL-2 PMA aCD3 iCD3 +rlL-2 YCD3+PMA XCD3 +iCD28 zCD28 + rIL-2 iCD28 + PMA xCD26 + PMA oCD69+PMA lonomycin + PMA PBMC were cultured in the presence of the indicated stimuli and pulsed for 18 h with I pCi/well 3H-TdR. The mean ct/min of triplicate samples was determined by liquid scintillation on day 3. Results Patients (n = 29) 1 +0 13+2 5+ 1 6+0 52 + 6 74+ 13 16 +4 6+3 96 + 25 119+28 55+ 13 148 + 30 Controls (n = 29) Statistical significance 2+0 NS NS P<0 05 P<0 001 NS P<0 001 P<0 001 NS NS NS* 11+1 7+0 30+5 67 + 5 151 + 15 73 + 10 11 + I 147 +28 152 + 35 174+49 193 + 27 P<0.05* NS *n = 8 for these stimuli. Peripheral blood mononuclear cells (PBMC) were cultured in the presence of the indicated stimuli and pulsed for 18 h with I pCi/well 3HTdR. The mean ct/min of triplicate samples was determined by liquid scintillation on day 3. Results represent mean+ s.e.m. PMA, Phorbol myristate acetate; NS, not significant. represent mean + s.e.m. PHA, Phytohaemagglutinin; PMA, phorbol myristate acetate; PWM, pokeweed mitogen; Con A, concanavalin A; NS, not significant. £ IL-2 3r IL-2 E600 I (b) ~~~~~~~IL-? )T 00 2500F rLE[~~~~~U 2500i 0Medium A PMA Fig. 1. PMAl after synthesis IL-2 + stimulation of cytomegalovirus (CMV) peripheral blood lymphocytes with lectins (a) or anti-CD3 antibodies (b). A small sample of six patients and nine controls was analysed. Controls; bol *U, CMV patients. PHA, Phytohaemagglutinin ; PM myristate acetate; Con A. concanavalin PWM, A; A, fl, phor- pokeweed mitogen. cells was recorded normals, (148±+ P<005). Our 1 1 arbitrary units groups of acute versus 1 16 +10 in and latent CMV patients did not show significant differences for these phenotypical (or functional, see below) parameters, except for a higher P<0001). This was not due to a general proliferation impairment of CMV PBMC, because stimulation of the same cells with PHA induced normal proliferation. In contrast, CMV PBMC showed a decreased (around two-fold) proliferative response to two other lectins, PWM and Con A. Interestingly, the impaired proliferation of CMV PBMC in response to Con A, but not PWM, was recovered by addition of exogenous rIL-2 or PMA (a protein kinase C activator). These results indicate that T cells from individuals infected with CMV show a defined pattern of unresponsiveness to mitogens, probably due to insufficient signalling to protein kinase C (PKC) moieties and, as a consequence, lower induction of IL-2. Direct assessment of cytokine induction in a small sample of patients (n =6) and controls (n=9) confirmed the existence of an IL-2 synthesis defect after stimulation of CMV PBMC with PHA (around twofold reduction), Con A (three-fold) and PWM (three-fold) (Fig. la). Thus, PWM and Con A stimulation, which caused a significantly decreased proliferation in CMV PBMC (Table 2), induced an average two-fold lower IL-2 production than PHA in the patients; these PHA-induced IL-2 levels may have been sufficient to allow a normal proliferation in response to PHA, as shown in Table 2. Lastly, addition of PMA completely normalized the lectin-induced synthesis of IL-2. number of CD8 cells in acute patients. For practical reasons, they were pooled for the analysis, but the conclusions hold if the two separate Stimulation sets of patients are maintained (data not shown). with antigens and lectins (Table 2) Upon stimulation recognize the V/I of CMV region PBMC of the T with enterotoxins which cell receptor (TCR), a significant decrease in T cell proliferation was observed (compared with control cells) both with enterotoxin A (around twofold, P<0001) and with enterotoxin Cl (almost four-fold, Stimulation with antibodies against CD3, CD28, CD26 and CD69 (Table 3) Further analysis of T cell function was performed using specific MoAbs. The proliferative response to anti-CD3 was markedly lower in CMV than in control PBMC samples (around five-fold, P<0 001). Co-stimulation of CMV PBMC with anti-CD3 and antibodies directed against any other signal-transducing molecules, like CD28, also resulted in impaired proliferative responses (around five-fold, P<0001) compared with control T lymphocyte anergy in CMV infection cells. This could not be due to a CD28 signalling defect in CMV PBMC, because a specific antibody was capable of inducing significant responses in the presence of PMA. The impaired response to anti-CD3 is corrected with exogenous rIL-2, but only in part with PMA, which directly activates PKC. Direct assessment of IL-2 induction as above confirmed the existence of an IL-2 synthesis defect after stimulation of CMV PBMC with anti-CD3 (five-fold reduction) or anti-CD3 plus PMA (10fold reduction) (Fig. lb). Two other T cell surface molecules, CD26 and CD69, which, like CD28, are capable of inducing T cell proliferation in the presence of PMA, were triggered in a small number of patients (n = 8). The results showed that CD26, but not CD69, induced normal proliferation in CMV PBMC. Lastly, the distal cytoplasmic signal-transducing biochemistry of CMV PBMC seemed to be adequate, since their proliferative response to the transmembrane activators PMA (which directly activates PKC) plus ionomycin (which increases cytosolic Ca2+) was comparable to that of normal controls. This suggests that the proliferation defects observed in CMV PBMC using surface stimuli are probably due to TCR/CD3 membrane-proximal defects. DISCUSSION Secondary immunodeficiencies are a heterogeneous group of disorders of the immune system that occur together with other pathological conditions [13]. Due to the transient nature of the alterations, the molecular basis of secondary immunodeficiencies is mostly unknown, precluding the development of rational therapies. In this study, an attempt has been made to characterize a common herpesvirus-induced secondary immunodeficiency due to CMV infection. Our results show that CMV infection, both acute and latent, causes a selective anergy of the TCR/CD3 activation pathway. This is supported by the observed low proliferative response of PBMC obtained from CMV patients to enterotoxins, certain lectins (Con A) and anti-CD3 MoAbs, whereas stimulation using other lectins (PHA) or anti-CD28 or -CD26 antibodies elicited normal proliferations. The impaired responses to antiCD3 antibodies and Con A were corrected with exogenous IL-2, suggesting the existence of a TCR/CD3-associated signalling defect to certain response genes like that of IL-2. Direct assessment of IL-2 synthesis confirmed that it was more severely reduced in response to Con A and anti-CD3. The defect was probably proximal to the TCR/CD3 complex, because direct activation of PKC using phorbol ester PMA corrected the impaired proliferative responses to anti-CD3 only partially. Although tested in only a small number of patients, the low responses elicited through CD69 compared with CD26 (or CD28) may suggest that CD69 activation is more CD3dependent than CD26 or CD28 [14], at least in this model. A range of secondary immunodeficiencies is associated with defects in T cell activation [15]. Secondary defects in CD3mediated, but not CD2-mediated (or CD28-mediated [15]) T cell activation have been reported in certain pathological situations like uraemia [16], HIV infection [17], Epstein-Barr virus (EBV) infection [18]. Conversely, defects in the CD2 but not in the CD3 activation pathway are believed to be secondary to several disease states, like Sjogren's syndrome [19], lupus [20], atopy [21], alcoholic liver disease [22] and Hodgkin's disease [23]. In certain patients both the CD2 and CD3 activation 41 pathways show quantitative impairments, but a normal transmembrane activation biochemistry is preserved, as in Down's syndrome [24], healthy aged individuals [25] and bone marrow recipients [26]. More recently, biochemical defects in certain TCR-associated proteins have been observed in tumour-bearing mice and humans [27]. The molecular basis in each case is undoubtedly heterogeneous. However, the association of at least three viral infections (HIV, EBV and CMV) with selective CD3-associated activation defects may suggest the existence of a common evolutive immunosuppression mechanism. The ability of these viruses to encode for cell surface protein homologues of immunological significance (CD4 ligands, CD21 ligands and HLA molecules, respectively) may underlie the defect. Other interpretations are possible, however. First, intracellular interferences like the induction of apoptosis rather than proliferation, as shown for HIV [28], may be involved in the observed CMV-associated T cell anergy. Second, the observed increased levels of peripheral blood CD8+ T cells in CMV patients may cause the selective defect of T cell activation, as CD8 + cells are thought to contain suppressor as well as cytotoxic lymphocytes [29]. Third, as we have not assessed which subsets of T cells actually proliferate in controls versus patients, a strong expansion of a set of anergic T cells (in terms of proliferation to certain stimuli ex vivo) after CMV infection could explain our data. In the last two cases, immune response to CMV, rather than the virus itself, would mediate the T cell anergy. Further immunological and virological work is required to elucidate the molecular basis of the interaction of CMV with the human immune system. This, in turn, will allow rational therapies to be developed for this (and other) common secondary immunodeficiencies. ACKNOWLEDGMENTS We thank Ana Garcia for her help. This work was supported in part by grants from FIS (91/324) and DGICYT (92/270). REFERENCES I Weller TH. The cytomegalovirus, ubiquitous agents with protean clinical manifestations. N Engl J Med 1971; 285:203-67. 2 Rinaldo CRJ, De Bianco RL. Alteration of immunoregulatory mechanism during cytomegalovirus mononucleosis: effect of in vitro culture of lymphocyte blastogenesis to viral antigens. Clin Immunol Immunopathol 1983; 28:46. 3 Browne H, Smith G, Beck S. Menson T. A complex between the MHC class I homologue encoded by human cytomegalovirus and ,B2 microglobulin. Nature 1990; 347:770. 4 Hirsh MS, Felsenstein D. Cytomegalovirus induced immunosuppression. Ann NY Acad Sci 1984; 437:8. 5 Schrier RD, Rice GPA, Oldstone MBA. Suppression of natural killer cell activity and T cell proliferation by fresh isolates of human cytomegalovirus. J Infect Dis 1986; 153: 1084. 6 Carney WP, Rubin RH, Hoffman RA, Hansen WP, Healey K, Hirsch MS. Analysis of T lymphocyte subsets in cytomegalovirus mononucleosis. J Immunol 1981; 126:2114. 7 Moretta A, Ciccone E, Pantaleo G et al. Surface molecules involved in the activation and regulation of T or natural killer lymphocytes in humans. Immunol Rev 1989; 111:145-75. 8 Britt WJ, Pass RF, Stagno S, Alford CA. Pediatric cytomegalovirus infection. Transplant Proc 1991; 23:115-7. 9 Carney WP, Tacoviello V, Hirsch MS. Functional properties of T lymphocytes and their subsets in cytomegalovirus mononucleosis. J Immunol 1983; 130:390-5. 42 M. Timon et al. 10 Middeldorp JM, Jongsma J, Terhoor A, Schirm J, The TH. Conditions for the detection of IgM and IgG antibodies against CMV early (CMV-EA) and late (CMV-LA) antigens by ELISA. J Clin Microbiol 1984; 20:763. 11 Caldwell CW, Taylor HM. A rapid, no-wash method for immunophenotypic analysis by flow cytometry. Am J Clin Path 1986; 86:600-7. 12 Regueiro JR, Lopez-Botet M, Landazuri MO et al. An in vivo functional immune system lacking polyclonal T cell surface expression of the CD3/Ti (WT3 1) complex. Scand J Immunol 1987; 26:699-707. 13 Amman AJ. Immunodeficiency diseases. In: Stites DP, Stobo JD, Wells JV, eds. Basic and clinical immunology. East Norwalk: Appleton and Lange, 1987:347-53. 14 Rinc6n M, Cebridn M, Sanchez-Madrid F, Lopez-Botet M. Induction of T cell function via the gp 33/27 activation inducer molecule (AIM) requires co-expression of the CD3/TCR complex. Eur J Immunol 1989; 19:959-62. 15 Arnaiz-Villena A, Tim6n M, Rodriguez-Gallego C, Perez-Blas M, Corell A, Martin-Villa M, Regueiro JR. Human T-cell activation deficiencies. Immunol Today 1992; 13:259-65. 16 Meuer SC, Hauer M, Kurz P, Meyer zum Buschenfelde KH, Kohler H. Selective blockade of the antigen-receptor-mediated pathway of T cell activation in patients with impaired primary immune responses. J Clin Invest 1987; 80:743-9. 17 Linette GP, Hatzman RJ, Ledbetter JA, June CH. HIV- I -infected T cells show a selective signaling defect after perturbation of CD3/ antigen receptor. Science 1988; 241:573-6. 18 Perez-Blas M, Regueiro JR, Ruiz-Contreras J, Arnaiz-Villena A. T lymphocyte anergy during acute infectious mononucleosis is restricted to the clonotypic receptor activation pathway. Clin Exp Immunol 1992; 89:83-88. 19 Dauphinee MJ, Tovar Z, Ballester A, Talal N. The expression and function of CD3 and CD5 in patients with primary Sjogren's syndrome. Arthritis Rheum 1989; 32:420-9. 20 Fox DA, Millard JA, Treisman J et al. Defective CD2 pathway T cell activation in systemic lupus erythematosus. Arthritis Rheum 1991; 34:561-71. 21 Romano MF, Valerio G, Turco MC et al. Defect of CD2- and CD3mediated activation pathways in T cells of atopic patients: role of interleukin 2. Cell Immunol 1992; 139:91-97. 22 Spinozzi F, Bertotto A, Rondoni F et al. T-lymphocyte activation pathways in alcoholic liver disease. Immunology 1991; 73:140-6. 23 Meuer SC, Roux MM, Schraven B. The alternative pathway of T cell activation: biology, pathophysiology, and perspectives for immunopharmacology. Clin Immunol Immunopathol 1989; 50:133-9. 24 Bertotto A, Crupi S. Arcangeli C et al. T-cell response to phorbol ester PMA and calcium ionophore A23187 in Down's syndrome. Scand J Immunol 1989; 30:583-6. 25 Beckman I, Dimopoulos K, Xu X, Ahern M, Bradley J. Age-related changes in the activation requirements of human CD4+ T-cell subsets. Cell Immunol 1991; 132:17-25. 26 Yamagami M, McFadden PW, Koethe SM, Ratanatharathorn V, Lum LG. Failure of T cell receptor-anti-CD3 monoclonal antibody interaction in T cells from marrow recipients to induce increases in intracellular ionized calcium. J Clin Invest 1990; 86:1347-51. 27 Mizoguchi H, O'Shea JJ, Longo DL, Loeffler CM, McVicar DW, Ochoa AC. Alterations in signal transduction molecules in T lymphocytes from tumor-bearing mice. Science 1992; 258:1795-98. 28 Groux H, Tarpier G, Maute D, Montan Y, Capron A, Ameisen JC. Activation-induced death by apoptosis in CD4 + T cells from human immunodeficiency virus-infected asymtomatic individuals. J Exp Med 1992; 175:331-40. 29 Takata M, Maiti PK, Kubo RT, Chen YH, Holford-Stevens V, Rector ES, Sehon AH. Cloned suppressor T cells derived from mice tolerized with conjugates of antigen and monomethoxypolyethylene glycol. Relationship between monoclonal T suppressor factor and the T cell receptor. J Immunol 1990; 145:2846-53.
© Copyright 2026