A Defect in the Early Phase of T-cell Receptor
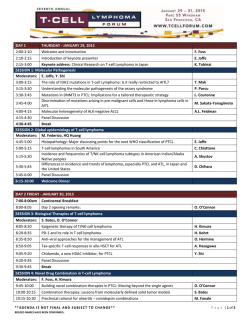
From www.bloodjournal.org by guest on February 6, 2015. For personal use only. A Defect in the Early Phase of T-cell Receptor-Mediated T-cell Activation in Patients With Common Variable Immunodeficiency By Michael B. Fischer, Ilona Hauber, Heinz Eggenbauer, Vojtech Thon, Erich Vogel, Elfriede Schaffer, Jindrich Lokaj, Jiri Litzman, Hermann M. Wolf, Josef W. Mannhalter, and Martha M. Eibl Common variable immunodeficiency (CVID) is characterizedCD3 monoclonalantibody, phytohemagglutinin) was norby an impairment of specific antibody production and a de- mal. The defect in interleukin-2 and interferon-y release on crease in all or selected Ig isotypes. Abnormalities at the tetanus toxoid stimulation could alsobe documented in purified CD4 T cells of the patients and was present in patients level of the B cells, T cells, and antigen-presentingcells have been described. In the present study, we have focused our with highand normal CD8counts alike. Furthermore, paattention on T-cell activation in CVID. T cells from 15 of 24 tients' T cells failed to mount a significant elevationin free patientsfailed to respond to recall antigens (eg, tetanus toxintracellular calciumE a + +flux) in response to superantigen, oid, Escherichia coir).Of these 15 patients, 11 were studied in whereas the response to phorbol myristate acetateand detail and showed significantly decreased T-cell Proliferativeionomycin, bypassing receptor-mediated signaling, was unresponses and/or decreased interleukin-2 and interferon-y impaired. These results indicate a defectin the early phase production on T-cellreceptor-mediatedstimulation with reof T-cell activation after triggering of the T-cell receptor in call antigens and superantigens (staphylococcal enterotoxa significant subgroup of CVID patients. response to mitogens (antiins [SEI); however, T-cell 0 1994 by The American Society of Hematology. C OMMON VARIABLE immunodeficiency (CVID) is characterized by heterogeneity in the clinical manifestations of the disease as well as in the underlying mechanisms leading to immunodeficiency. An impairment in specific antibody production and a decrease in all or some Ig isotypes are the characteristic features, and defects in B-cell differentiation andor antibody secretion are common."3 Abnormal distribution of T-cell subsets hasbeen shown in some CVID patients with an increase in the number of CD8+ cells>5 and multiple immunological abnormalities including functional T-cell defects such as abnormal helper function and increased T-cell suppressor activity have been described in these patients.' Reduced production of lymphokines in response to stimulation with mitogens such as antiCD3 monoclonal antibodies (MoAbs) and phytohemagglutinin (PHA) have also been rep~rted.'~'~ In prior studies, we had investigated T-cell activation in response to recall antigens (Escherichia coli, tetanus toxoid) in three CVID patients andshowed that proliferative responses as well as interleukin-2 (IL-2) and interferon-y (IFN-7) mRNA levels were significantly reduced after antigen stimulation, whereas T cells responded normally to antiCD3 (OKT3) and mitogen." These results pointed to a defect in T-cell activation after triggering of the T-cell receptor (TCR). In the present study, we investigated whether the defect described is limited to rare cases or is expressed in a large subgroup of CVID patients. To further characterize the defect, we addressed the question of whether the impaired From the Institute of Immunology, University of Vienna, Vienna; the Institute of Clinical Immunology, Masaryk University, Brno, the Czech Republic; and Immuno AG, Vienna, Austria. Submitted March 7, 1994; accepted August 9, 1994. Address reprint requests to Martha M. Eibl, MD, Institute of Immunology, University of Vienna, Borschkegasse 8A, A-l090 Vienna, Austria. The publication costsof this article were defrayedin part by page charge payment. This article must therefore be hereby marked "advertisement" in accordance with 18 U.S.C. section 1734 solely to indicate this fact. 0 1994 by The American Society of Hematology. 0006-4971/94/8412-03$3.00/0 4234 response to recall antigen is caused by defective recognition of the antigen by the TCR or by a defect in the transduction of transmembrane signals leading to impaired generation of second messengers after TCR triggering. The results obtained show that the T-cell activation defect is detectable in a relevant subset of CVID patients and that the defect is observed after triggering of the TCR with antigen, superantigen, or anti-TCR MoAb. In addition, TCR-mediated stimulation with superantigens failed to induce a rapid andsustained increase in levels of intracellular free Ca++in patients' lymphocytes, whereas the response to phorbol myristate acetate (PMA) and ionomycin (IM) was normal. These results suggest a defect in the early phase of T-cell activation after triggering of the TCR before the generation of intracellular free Ca++and before protein kinase C activation. MATERIALS AND METHODS Patients. At thetime of thestudy, 24 patients with CVIDas defined by the World Health Organization classification of primary immunodeficiencies" were followed up by our immunology division. The patients had a history of recurrent bacterial infections of the upper and lower respiratory tract and reduced or absent serum IgG, IgA, and IgM levels.In 9 of the 24 patients, the T-cell response to recall antigen ( E coli or tetanus toxoid) was comparable with the response in healthy individuals, and 2 of these 9 patients had low numbers of B cells in their peripheral blood. Fifteen patients had T lymphocytes incapable of responding to recall antigen presented by autologous antigen-presenting cells (APCs). One patient was shown to have a defect in APCs." Three further patients were excluded from the study because of severe concomitant disease (lymphoma, alcoholic cirrhosis of the liver, and eosinophilic gastroenteritis with severe gastrointestinal loss of protein). The remaining I1 patients, S menand 6 womenranging in agefrom 17 to 50 years,were enrolled in thestudyafterinformedconsent had been obtained. These 1 1 patients showed hypogammaglobulinemiaor agammaglobulinemia with a decrease in all Ig isotypes and consistently impaired production of specific antibodies in the presence of normal numbers of B cells, as well as impaired ability of their T cells to respond to recall antigens(eg,tetanustoxoid, E coli).Duringthecourse of this study, all patients were on regular gammaglobulin replacement therapy (7 patients, intravenous administration of 400 mg IgGkg body weight per month; 4 patients, intramuscular administration of 100 mg I g k g body weight per month). All patients had received tetanus toxoid vaccination or boosters within the last6 to 12 months before the study. At the timeof evaluation, none of the patients was Blood, Vol 84, No 12 (December 15). 1994: pp 4234-4241 From www.bloodjournal.org by guest on February 6, 2015. For personal use only. IMPAIRED TCR-MEDIATED T-CELL ACTIVATION IN CVID suffering from severe infections requiring hospital admission. Blood samples were taken 2 to 4 weeks after the last administration of Igs. Phenotypic analysis of CVID patients’ peripheral blood (PB) leukocytes showed that total numbers of T cells (CD3’[Leu 4]), B cells (CD19+[B4]), and natural killer cells (CD56+ [Leu 191) were within the normal range. Five patients had normal CD8’ counts (32% ? 9% of lymphocytes; mean t SD), whereas high CD8 counts could be detected in 6 patients (52% ? 12%of lymphocytes). Healthy age-matched volunteers were investigated in parallel and served as controls. The vaccination history of the controls was comparable with that of the patients. Isolation of mononuclear cells (MNCs) and preparation of a Tenriched lymphocyte population. PBMNCs were isolated from heparinized whole blood (7.5 IU/mL of preservative-free heparin) by buoyant density gradient centrifugation.’6 Monocytes were prepared by adherence to plastic surfaces as described previously.” Adherent cells were washed several times and removed gently with a rubber policeman. Cell purity was 80% to90% monocytes, as defined by flow cytometry with a CD14 MoAb. Nonadherent cells were removed and fractionated into T-enriched cells (>95% CD2+ and >90%CD3+ cells) and non-T cells by rosetting with sheep erythrocytes treated with 2-aminoethylisothiouronium bromide (Sigma Chemicals, St Louis, MO) as described earlier.” Lymphocyte proliferation. Triplicate cultures containing adherence-purified monocytes (1 X 104/well) and T-enriched cells (1 X 105/well)were set up in flat-bottomed microtiter plates (Falcon Microtest 11; Becton Dickinson, Lincoln Park, NJ), and one of the following stimuli was added tetanus toxoid (IO Loeffler flocculation (LF) units/mL; Swiss Serum and Vaccine Institute, Berne, Switzerland); heat-inactivated E coli 089:HlO (5 X IO6 E colilml); staphylococcal enterotoxins (SEs) SEA, SEC3, and SED (1 ng/mL; Toxin Technology, Madison, WI); PHA (1:1250; Wellcome, Dartford, UK); anti-CD3 MoAb (IO ng/mL OKT3; Ortho, Raritan, NJ); or anti-TCRa-P (2 pg BMA-031 were coated on 4 X IO8 sheep antimouse Ig-coated beads in a total volume of 1 mL [Dynabeads M450; Dynal, Oslo, Norway] and used at a final concentration of 1 X IO6 beaddl X IO6 T cells). Recombinant human IL-2 (Genzyme Corp, Cambridge, MA) was used at a final concentration of 20 U/mL. The cells were kept for 7 days (antigen), 5 days (superantigen, anti-TCR MoAb), or 3 days (PHA, OKT3) at 37°C in a COz incubator (5% CO2 in humidified air) in RPMI-1640 medium supplemented with 10% voUvol heat-inactivated human AB serum, 2/mmol/L L-glutamine, I O 0 IU/mL penicillin, and 100 pg/mL streptomycin. ’H-thymidine incorporation was determined as described earlier.’’ Results are shown as disintegrations per minute (mean t SEM of the average values of individual experiments performed in triplicate). Induction and measurement of IL-2 and IFN- y in T-cell supernatants. Cultures of macrophages (l X 105/mL)and T-enriched cells (1 X 106/mL)were set up in 24-well tissue culture plates and activated using the stimuli and culture media as described above. Culture supernatants were removed after 24 or 72 hours of incubation, were sterile-filtered, and were analyzed for their cytokine content. The IL-2 concentration was determined using the murine cytotoxic lymphoid cell line CTLL-2 as described earlier.13Concentrations of IFN--y in culture supernatants were determined using a commercial enzyme-linked immunosorbent assay (ELISA) kit (IFN--yMedgenix, Brussels, Belgium). IFN-y concentrations were calculated using a standard curve derived by linear regression of the log-transformed concentrations of the cytokine standards supplied with the ELISA kits versus the respective log-transformed ELISA-optical density (OD) values. Separation of CD4+ T lymphocytes. CD4+ T cells were isolated by negative magnetic immunoselection. In brief, MNC were adhered to plastic surfaces to remove monocytes; nonadherent cells were E+rosetted and the E’ cells were incubated with saturating concentra- 4235 tions of CD8 MoAb (Leu 2a) and CD56 MoAb (Leu 19; Becton Dickinson, used at a final concentration of 2.5 pg/l X lo7 cells) for 30 minutes at 4°C under continuous rotation. Cells were washed twice, mixed with sheep antimouse IgG-coated beads (Dynabeads M450; at a final concentration of 1 X IO’ beads11 X IO’ cells) and incubated for another 30 minutes at 4°C under continuous rotation. Cells that were reactive with the two MoAbs and thus bound to the magnetic beads were removed with a powerful permanent cobaltsumarium magnet (HPC-I; Dynal). The remaining cells were collected, washed twice, and analyzed by flow cytometry. Cell purity was 90% to 95% CD4’ cells. Assay of intracellular free Ca++Concentration. The increase in intracellular free Cat+ observed after stimulation of T cells was measured byflow cytometry. In brief, T-enriched cells (2 X lo6/ mL) were loaded with two fluorochromes, the Ca++-sensitive dye Fluo-3 (final concentration, 1 pmol; Molecular Probes, Eugene, OR), and the Ca++-insensitive dye Snarf-l (final concentration, 0.2 pmol; Molecular Probes) dissolved in buffer A (Iscove’s modified Dulbecco’s medium [IMDM; Sigma Chemicals] containing 10 mmol/L HEPES [Sigma Chemicals], pH 7.0). Pluronic F-l27 (BASF; final concentration, 37.5 g/L; Wyandotte, OR) was used to increase the uptake of the two fluorochromes by the cells. Cells were incubated for 30 minutes in a COz incubator at 37°C. Next, an equal volume of buffer B (IMDM containing 10 mmol/L HEPES and 10% fetal calf serum [FCS; HyClone Laboratories, Inc, Logan, UT], pH 7.4) was added to the cells suspended in buffer A, and the cells were incubated for an additional 10 minutes at 37°C. Cells were then washed twice and resuspended in buffer C (IMDM containing 10% FCS, 10 mmoVL HEPES and 10 pg/mL DNAse [Sigma Chemicals]) at a final concentration of 2 X 106/mL. Autologous monocytes (2 X 105/mL) that had been preincubated at 37°C for 3 hours with a cocktail of SEs (final SE concentrations: SEA, 5 pg/mL; SEB, I O pg/mL; SECI, I O pg/mL; SEC2,5 pg/mL; SEC3, 5 pg/mL; SED, 5 pg/mL; SEE, 1 pg/mL) were added to Fluo-3- and Snarf-lloaded T cells. The mixture of monocytes and T cells was immediately centrifuged for 20 seconds at 200g in an Eppendorf cup (Eppendorf, Hamburg, Germany), and the cells were gently resuspended before fluorescence-activated cell sorter (FACS) analysis. The flow cytometric analysis of intracellular Ca++ was performed using a FACScan (Becton Dickinson) interfaced to a Hewlett Packard computer system using Lysis and Chronys software (Becton Dickinson). Forward and right angle light scatter were used to gate selectively on the lymphocyte population. For kinetic analysis of Ca++changes, events were continuously monitored with the Chronys software, and themean fluorescence intensity of events measured atIO-second intervals was calculated. Relative intracellular Ca++ increase was calculated in computed parameters with the Chronys software using the increase in Fluo-3-specific fluorescence intensity measured in F11 compared with the stable Snarf-l -specific fluorescence intensity measured in F13by the formula: Fll/Fl3* = F11 t,/[n3 t, x (F11 t,/ F13 tl)]. In every experiment, unpulsed autologous macrophages were included as a control for T-cell activation induced by autologous monocytes. The combination of PMA + IM (1 pg/mL PMA [Sigma Chemicals] and 5 pg/mL ionomycin [Calbiochem, San Diego, CA]) added to the T cells after investigation of the superantigen-induced Ca++flux served as a positive control inducing maximal Ca++ release. Induction and assessment of B-cell Ig secretion in patients’ MNCs. A total of 1 X lo6 MNCs were stimulated with pokeweed mitogen (PWM; GIBCO, Grand Island, NY), anti-IgM MoAb plus recombinant IL-2 (rIL-2; Genzyme), or Staphylococcus aureus Cowan I (SAC; Calbiochem). The anti-IgM MoAb (kindly provided by Dr 0. Majdic, Institute of Immunology, University of Vienna) was coupled to Dynabeads M 450 (2 pg anti-IgM MoAb were coated on 4 X 10’ sheep antimouse IgG-coated beads in a total volume of 1 From www.bloodjournal.org by guest on February 6, 2015. For personal use only. 4236 FISCHER ET AL h The defect in T-cellactivation results in impaired IL-2 and IFM-y release and can be observed after triggering of g 300000 100000 v the TCR by dzfferent stimuli. Further studies were designed to characterize the T-cell activation defect observed in the .-E 100000 patients unresponsive to recall antigens. Superantigens such a 2 0 0 as SEs are an appropriate tool for studying TCR-mediated 10000 EtT-cell activation. Because they do not have to be processed 10000 0 0 by APCs tobe presented in context with the major histocomK .o * patibility complex class I1 molecule, they stimulate the T a, K cells by binding to the TCR-V@chain outside the recognition .1000 E 1000 site for antigen and activate between 1 in 5 and 1 in 20 PB T cells. In contrast, conventional antigens stimulate fewer E, &l 5 300 300 than 1 in 10,000 PB T cells. Although patients' T cells i Tet.tox. expressed comparable levels of Vp2, Vp3, VP5a and c, PHA VP6a, Vp8, VP8a, Vp12a, Vp13, Vp17. and V019 (data Fig 1. Proliferative response of CVlD patients' T cells stimulated not shown), their proliferative response as well as IL-2 and with mitogen (PHA) and the recell antigen tetanus toxoid (Tet. tox.). I F N -y production after stimulation with SEA, SEC3, or SED T-enriched cells (1 x 105/well) and autologous monocytes (1 x 10'1 (1 ng/mL) were significantly impaired (Fig 2). Furthermore, well)were cocultivated and stimulated withthe mitogen PHA patients' T cells released significantly reduced amounts of (1:1250) or the recall antigen tetanus toxoid ( l 0 LflmL). 3H-thymidine incorporationwas determined after 3 days (PHA) or7 days (antigen) IL-2 and IFN-y when stimulated with an MoAb specific for asdescribed in Materials and Methods. Proliferative response obthe constant region of the TCR &chain (BMA-031 ; see Fig sewed in unstimulated cultures of patients and controls never ex2). When the patients' T cells were stimulated via CD3, ceeded 1.000 dpm. Open symbols represent individual subjects (0. proliferation and IL-2 release were comparable with that of patients; A,controls). Closed symbols representthe mean, bars indithe controls (Fig 2), and IFN-y production was slightly (but cate SD ( +,controls; V, CVlD patients unresponsiveto recall antigen; A, CVlD patients reactive to recall antigen). The star indicates the not statistically significantly) decreased ( P = .096 as comstatistically significant difference between patients unresponsive to pared with that of the controls; see Fig 2). Levels of T-cell PHA, P = ,213; tetanus toxoid, P recall antigen (V)and controls ( proliferative responses and IL-2 and IFN-y production after = .0001). Statistical comparison between patients unresponsive to stimulation with PHA were comparable in patients and conrecall antigen (V)and patients reactive to recall antigen (A):PHA, P trols (for statistical comparison between patients and controls = 246; tetanus toxoid, P < .0001. see legend of Fig 2). The defect in TCR-mediated T-cell activation can be detected in purijied CD4' T cells and cannot be corrected by mL), and anti-IgM-coated beads were used at a final dilution of l exogenous rIL-2. Because increased numbers ofCD8' X lo6 beaddl X lob MNCs.PWM and SACwereused at a final cells have been described to be associated with impaired Tdilution of 1500 and 1:5000, respectively, and rIL-2 was used at cell function in CVID?5 we examined whether the impair100 U/mL. Culturesupernatantswereharvested on day 7, were ment of T-cell activation observed in our patients correlated sterile-filtered, and were assayed usingan Ig isotype-specific ELISA with the levels of CD8' cells in the PB. As shown in Table as described earlier.'.' Statistics. For statisticalevaluation of thedifferencebetween 1, antigen-induced T-cell proliferation as well as IL-2 and patients and controls, the nonparametric Mann-WhitneyV test (oneIFN-y release were equally depressed in patients with high tailed) or the Student's t-test for unpaired samples was used.Multinumbers of CD8' T cells (ie, >40% CD8' lymphocytes) as variate analysis of more than two study groups was calculated using well as in those with normal numbers of CD8' T cells. the Kruskal-Wallis one-way ANOVA by ranks to confirm a signifiTo assure thatthe defect observed wasnot caused by cant difference between two study groups. A difference was considsuppression by CD8' cells, purified CD4+ cells (purity beered to be statistically significant at a level of P < .05. tween 90% and 95%) were prepared by depletion of CD8' and CD56+ cells from the T-enriched population. Patients' RESULTS CD4-enriched cells as well as their T cells responded norImpaired T-cell response to recall antigen is expressed in mally to PHA stimulation (Fig 3) or anti-CD3 MoAb stimua relevant subset of CVID patients. At the time of the lation (controls [n = 61: 'H-thymidine incorporation (dpm), study, 24 patients with CVID were followed up byour immu84127 2 54962 and IFN-y release, 157 2 149 U/mL; panology division. As shown in Fig I, all 24 patients responded tients [n = 71: 'H-thymidine incorporation (dpm), 108944 to PHA with substantial proliferation. In contrast, analysis ? 40176 and IFN-y release, 175 2 82 U/mL; mean t SD). of the response to recall antigen (tetanus toxoid or E coli) In contrast, purified CD4+ T cells of the patients were unable showed two distinct populations. Of the 24 patients recently to respond with substantial proliferation and with IL-2 and (within 1 year before the study) vaccinated with tetanus I F N -y production to the recall antigen tetanus toxoid. Additoxoid, 15 showed an impairment of tetanus toxoid-induced tion of exogenous rIL-2 to the patients' CD4' T cells significantly increased antigen-induced T-cell proliferation and T-cell activation in the presence of functionally intact autoloIFN-y release as compared with tetanus toxoid ( P < ,005) gous macrophages (Fig 1). T cells of these 15 patients were or IL-2 ( P < .01) alone, but proliferative responses and IFNalso unresponsive to stimulation with E coli (data not y release in the patients were still significantly lower than shown). The remaining 9 patients responded normallyto that in the controls (Fig 3). tetanus toxoid (Fig 1) or E coli (data not shown). E CI +; From www.bloodjournal.org by guest on February 6, 2015. For personal use only. 4237 IMPAIRED TCR-MEDIATEDT-CELL ACTIVATION IN CVlD A. T cellproliferation €3. IL-2 release C. IFN-gamma release Medw in PHA OKT3 TCR Tet.tox. SEA SEC3 SED 0 %-thymidine 60180 120 (Thousands) incorporation (dpm) 0 40120 80 IL-2 (Wml) 0 60180 120 Interferon-gama (U/ml) Fig 2. Proliferativeresponse and IL-2 and IFN-y releaseby CVID patients‘ T cells after activation with diffarent stimuli. T-enriched cellsand autologous monocytes were cocultured in thepresence of PHA (1:1250), anti-CD3 MoAbs ( O m ; 10 nglmL), anti-TCR (BMA-031) coupledon Dynebeads M460 (2 pg/mL BMA-031 MoAb per 4 x l@beedslmL, 1 x l @beedslwell), recall antigen tetanus toxoid (Tat. tox.; 10 LFlmL), or SEs (SEA, SEC3, and SED in a final concentration of 1 nglmL) as described in Materials and Methods. Supernatants from PHA-, anti-CDg-, anti-TCR-, andsuperantigen-stimulatedcultureswere harvested 24 hours after stimulation, whereas supernatants from antigen-driven cultures were collected after 72hours. The supernatants wera assayed for IL-2 and IFN-y as described in Materials and Methods. sH-thymidine incorporation was determined after 3 days ofculture for PHA and anti-CD3 MoAb,after 5 days of culture for superantigen and anti-TCR MoAb, and after 7 days ofculture for antigen, as described in Materials and Methods. Values represent mean f SD; statistically significant differences between patients and controls are marked with an asterisk. Statistical comparison between patients and controls is as follows: for PHA for anti-TCR M o b proliferation, P = .112; IL-2, P = .33; IFN-y, P = .308; for anti-CD3 M o b prolieration, P = ,179; L-2, P = .5; IFN-y, P = .M; proliieration, P = .311;IL-2, P = .0083; IFN-y, P .OO01; for Ter.tox.: proliferation, P < .Mol; IL-2, P ,0001; IFN-y, P .0001; for SEA proliferation, P = .0015; IL-2, P = .00029; IFN-y, P = .01; for SEC3: proliferation, P = .0021; IL-2, P = .0003; IFN-y, P = . O W ; and for SED: proliferation. P = .0022; IL-2, P = .00045, IFN-y, P = .03. (U)Controls (n = IO); (B) patients (n = 10). Impaired intracellular free Cat+ in patients’ T cells after triggering of the TCR by superantigens. A cocktail of seven different superantigens as described in Materials and Methods was used to examine the increase in intracellular free Ca++after triggering of the TCR. T cells from healthy controls responded with a significant Cat+ flux to triggering of the TCR by superantigen presented on the surface of autologous monocytes. In contrast, patients’ T cells were significantly (P< .001) depressed in their capacity to mount an increase in intracellular free Ca++ after triggering with superantigens (Fig 4).Stimulation of the same cells with the combination of PMA + IM, which thus bypassed receptormediated signal mechanisms by direct activation of diacylglycerol (DAG) and mobilization of free Ca’ from intracellular and extracellular stores, resulted in a significant Ca++ flux in the patients’ cells to levels that were comparable with that of the controls (Fig 4). These results indicate a defect in the early phase of T-cell activation after triggering via the TCR, before the generation of the second messengers DAG and inositoltriphosphate (IP3). B cells of CVID patients produce IgM, but not &G, after in vitro stimulation. PB B cells in patients whose T cells were unresponsive to recall antigen were normal in numbers (data not shown), but Ig secretion in vitro was impaired. Although stimulation of PB lymphocytes with P M , SAC, or anti-IgM plus rIL-2 resuited in levels of IgM secretion that were comparable with that of controls, none of the stimulants induced IgG release in the patients’ B cells (Table 2). DISCUSSION The results presented here confirm and extend our previous observation made in three patients with CVID by showing that T cell activation on triggering of the TCR is defective in a significant subset of CVID patients (15 of 24 patients). Furthermore, the results of the present study provide evidence that a major subgroup of CVID patients expresses a defect in the early phase of T-cell activation after triggering of the TCR. Impaired T-cell activation, including defective 1L-2 production on activation with mitogenic lectins or anti-CD3, has been observed previously by several investigator^.^"' Sneller et al’ described four patients with CVID whose T From www.bloodjournal.org by guest on February 6, 2015. For personal use only. FISCHER ET AL 4238 Table 1. Antigen-Induced T-cell Activation Is Depressed in Patients With High as Well as in Those With Normal Numbers of CD8' T Cells T-cell Response to the Recall Antigen Tetanus Toxoid Patients I N = 6) With High CD8* Proliferation (dpm) 2,060 IL-2 (U/mL) 1.3 IFN-y lU/mL) 3.9 t 2,040 t 0.5 2 3.6 Patients ( N = 5) With Normal CD8t Controls I N = 10) 1,233 t 463 1.1 t 0.9 1.5 t 0.7 25,219 t 13,698 46.8 ? 16.7 55.1 t 24.6 T-enriched cells (1 x 105/well) and autologous monocytes (1 x 10'/well) were cocultivated and stimulated with tetanus toxoid (10 Lf/mL). After 3 days, culture supernatants were removed andassayed for IL-2 and IFN-y content. 3H-thymidine incorporation was determined after 7 days of culture as described in Materials and Methods. Values represent mean f SD. Statistical comparison between patients with high levels of CD8' T cells and patients with normal levels of CDB- T cells are as follows: for proliferation, P = .23; for IL-2. P = .32; and for IFN-y. P = .25. Statistically signlficant differences as compared with the controls are as follows: for proliferation, P = .00057; for IL-2, P = ,00045; and for IFN-y, P = .00067. t Statistical differences as compared with controls are as follows: for proliferatlon, P = .0011; for IL-2, P = .00091; and for IFN-y, P = ,0023. cells had a normal phenotype but were unable to express detectable levels of IL-2, IL-4, IL-5, and IFN-y mRNA after lectin (PHA) stimulation. The same patients' PHA-stimulated T cells showed a normal proliferative response and expressed adequate amounts of IL-2 receptor and c-myc mRNA. These investigators discussed the possibility ofan impairment in the interaction of nuclear transcription factors with specific DNA sequences located in the 5' regulatory regions of lymphokine genes. In a subsequent report, these investigators clarified that the lymphokine production defect observed in their four patients with CVID was a primary abnormality of CD4+ T cells that might berelated to an impairment of a membrane receptor-dependent signaling pathway." However, antigen-induced T-cell responses have not been studied. A. V Conflicting data have been reported withregardtothe role of immunoregulatory abnormalities such as an increase in CD8' T cells in the impairedresponse of T cells to antigen in CVID patients. A report by Wright et a14 described 5 of 12 CVID patients with high CD8 counts who wereanergic as determined by skin testing of delayed-type hypersensitivity (DTH) reaction, whereas, in the group of CVID patients with normal numbers of CD8 positive cells, only 1 of 15 patients was anergic to recall antigens. These data suggest that, in CVID patients withhigh levels of CD8' T cells, antigen unresponsiveness ismore frequent thanin CVID patients with normal numbers of CD8' T cells. Jaffe et allx reported thatCD4' T-cell function (the principal T-cell subsetresponding to antigen) of patients with high numbers of CD8' T cells was unimpaired. The defect in T-cell antigen responsiveness observed in the subgroup of CVID patients we studied was expressed normal CD8 counts, both in patients with highandwith and no correlation could be found between CD8 counts and tetanus toxoid-specific T-cell proliferation (linear regression analysis; data not shown). Purified CD4' cells expressed the T-cell activation defect both in the absence or presence of CD8' T cells alike. Therefore, it appears unlikely that the defect described is caused by immunoregulatory abnormalities such as an increase in CD8' cells leading to excessive suppression at the T-cell level. Defective ligand recognition by TCR is not likely to be the only explanation for the impaired response to antigen. The combination of antigen and exogenously added rIL-2 induced significantly higher proliferative response and lymphokine secretion in the patients' T cells than did either antigen orIL-2 alone. Furthermore, antigenic stimulation induced normal production of IL-2 receptor, IL-3, and IL-4 mRNA transcripts in these patients' T lymphocytes in the B. OL-2 cell proliferation C. QFN-gamma release release 1ocl - 150 CD4-enriched 75 -E 3 N I 50l ' 4 25 0 PHA T.T. T.T.+IL-2 IL-2 MedlUn FHA T.T. Medtm PHA T.T. T.T.+IL-2 IL-2 Medfm Fig 3. Impaired antigen-induced T-cell activation can be observed in purified CD4'Tcells obtained from CVID patients and cannot be corrected by addition of rlL-2. CDCenriched T cells (1 x lo5 cellslwell) were cocultivated in the presence of autologous monocytes (1 x lo' cellslwelll and stimulated with PHA (1:1250J or tetanus toxoid (T.T.; 10 LFlmLJwith or without IL-2 (10 IUlmL). 3H-thymidineincorporation was determined after 3 days for PHA or 7 days for antigen,as described in Materials and Methods. Supernatants of patients' and controls' Tcell cultures were collected after 24 hours (PHA) and 72 hours (antigen), and IL-2 and IFN-7 levels were determined as described in Materials and Methods. Values represent mean 2 SD; statistically significant differences between patients and controls are marked with an asterisk. Statistical comparison between patients and controls is as follows: for PHA proliferation, P = .2; IL-2, P = .057; IFN-7, P = .087; for T.T.: proliferation, P = .0013; IL-2, P = .01; IFN-y, P = .0051; for T.T. + IL-2 proliferation, P = ,012; IFN-y, P = ,0071; and for IL-2 prolfferation, P = .074; IFN-y, P = .07. (m) Controls (n = 61; (B) patients (n = 71. From www.bloodjournal.org by guest on February 6, 2015. For personal use only. 4239 IMPAIRED TCR-MEDIATEDT-CELL ACTIVATION IN CVlD addition of PMA + IM 2.80 2.60 2.40 addition of SE-pulsed monocytes 2.20 2.00 1.80 1.60 1.40 1.20 1.oo W . V V -1 3 Fig 4. Decreased CB++ mobilization in T lymphocytes of CVlD patients after stimulation with superantigen. T-enrichedcalls (2 x lO'/mL) were loaded with Fluo-3 (1 pmol) and Snarf-l (0.2 pmol) and were subsequently stimulated with autologous monocytes (2 x 106/mL) that had been pulsed with a cocktail of different superantigens (final SE concentrations: SEA, 5 pg/mL; SEB, 10 pg/mL; SECl, 10 pg/mL; SEC2.5 pg/mL; SE=, 5 pg/ml; SED, 5 pg/mL; SEE, 1 pg/mLI. Changes in the levels of intracellular free Ca+* in patients' and controls' T-enriched lymphocyteswere determined using a cytofluorograph as described in Materials and Methods.Stimulation with a combination of PMA (1pg/ mL) and IM (5 pg/mL) resulted in a maximum increase in intracellularfree CB++ and servedas a positive control in these experiments. Results are depkted as relative intracellular Ca*+ increase (F111F13'; mean ? SD) calculated as described in Materials and Methods. The relative intracellular Ca++ increase observedafter addition of unpulsed autologous monocytes to patients' or controls' T cells did not exceed 1.10. Statistically significant differences between patients and controls (Student's t-test, P < .001) are marked with an asterisk. (W) Controls (n = 10); (0)patients (n = 8). presence of impaired IL-2 and IFN-.)I gene expression (Hauber et al, manuscript submitted), clearly indicating that the antigen had been recognized by the T cell and delivered a signal. In addition, T-cell response to superantigen stimulationwas impaired. Superantigens stimulate the T cell by binding to the TCR-VP chain apart from the antigen binding site. No evidence for narrowing of the TCR-VP repertoire could be found, because T cells of this group of patients with CVID expressed comparable levels of VP2, VP3, VPSa and c, VP6a, VPS, VpSa, VP12a, VP13, VP17, and VP19 (data not shown), as has also been described by others." Even though binding of superantigen to the TCR has not been assessed directly, the normal expression of the TCR-VP repertoire makes impaired binding of superantigens unlikely. Finally, stimulation via the monomorphic region of the TCR with anti-TCR MoAb resulted in impaired T-cell activation as shown by significantly reduced cytokine release, whereas expression of the TCRa-P molecule on the T-cell surface was normal (data not shown). The reduced response to antigen, superantigen, and anti-TCR MoAb binding to distinct sites of the TCR points to defective TCR-mediated signaling and makes impaired ligand recognition unlikely. Increasing experimental evidence points to the possibility that signaling events in T-cell activation on stimulation of the TClUCD3 complex might follow at least two different pathways.20.z'Examples of this dichotomy also come from experiments of nature. T cells of patients with Wiskott-Aldrich syndrome were shown to function normally when triggered with antigen but showed a defect in activation when triggered with a11ti-CD3.~~ T cells from our CVID patients could be activated normally on anti-CD3 triggering but could notbe activated to express IL-2 after stimulation of the TCRa-P molecule. The possibility that T-cell activation by superantigen and by antigen follows different signal transduction pathways has been indicatedz3but needs further clarification. The question of Ca++mobilization in T cells after superantigen stimulation is controversial. Oyaizu et a1,24 when studying human T-cell lines and their response to superantigen, did not observe a significant Ca++flux, whereas two groups using resting human T cells from the PB25*z6 were able to induce Ca++flux on stimulation with superantigens. These discrepancies could be explained by differences in the cell population studied or the nature and concentration of the superantigen applied. It is feasible that superantigens applied at lower concentrations, as in the study by Oyaizu et al," may preferentially stimulate T-cell activation without From www.bloodjournal.org by guest on February 6, 2015. For personal use only. 4240 FISCHER ET AL Table 2. B Cells of CVID Patients Secrete IgM But Not IgG lg Secretion (NgimL) Stimulus Patients (N IgM Medium PWM SAC IgM + IL-2 IgG Medium PWM SAC IgM + IL-2 = 10) 0.17 i- 0.13 10.43 t 9.01 7.95 i- 7.30 2.78 t 2.50 0.18 t 0.03 0.28 t 0.16’ 0.12 f 0.06* 0.25 t 0.16’ Controls (N = 6) 0.21 2 0.12 7.80 f 5.61 6.36 t 5.68 2.19 i- 2.18 0.20 t 0.18 5.99 f 2.13 6.67 ? 3.04 4.73 t- 3.28 Patients’ PBMNC (1 x 106/mL)were stimulated with PWM (1:500), anti-lgM coupled to Dynabeads M450 (5 fig anti-lgM coated on 1 x lo6 sheep antimouse IgG beads/mL) in combination with rlL-2 (100 U/mL) or SAC (1:5000).After 7 days of cultivation the levels ofIgM and IgG were determined byELISA. Values represent mean f SD. * Statistically significant difference as compared with the controls is as follows: for PWM. P = ,00073; for SAC, P = ,00074; and for IgM + IL-2, P = ,00057. inducing measurable Ca++ flux. Our experiments followed the experimental design described by Fleischer et alZSand Chatila et alZ6and confirm that, in resting PB T cells of healthy individuals, bacterial superantigens appliedat microgramconcentrationsinduce a measurable Ca++ flux. The patients’ T cells were clearly deficient in mounting a Ca++ flux after superantigen stimulation in this system. Although itisunlikely, our results cannot rule out adelayed Ca++ response after triggering of the TCR with superantigen in the patients. The combination of PMA and I M , agents that bypass receptor-mediated signal mechanisms, was shown to induce an appropriate and immediate increase in cytosolic freeCa++concentration in the patients’ lymphocytesand also triggered normal proliferation and cytokine release (data not shown). Therefore, it appears likely that the impairment in T-cell activation observed in our patients is caused by a defect in early signaling events after triggering of the TCR. Although our results indicate that TCR-coupled generation of second messengers such as intracellular free Ca++ is defective in the patients, other TCR-coupled signaling pathways independent of Ca++ mobilization could also be impaired. The impairment in T-cell activation found in this subset of CVID patients is notabsolute. Although IL-2 mRNA and protein levels are decreased after TCR stimulation, possibly as a consequence of reduced Ca++mobilization, other events triggered by TCR activation such as gene expression of IL2receptor, IL-3,and IL-4 are unimpaired (Hauberet al, manuscript submitted). This might be because of different signaling requirements, eg,different pathways and/or quantitative differences in the levels of second messengers prodUced.Z0,21,27,28 Furthermore, T cells from these patients are principally capable of producing IL-2 after triggering of surfacereceptorsother than TCR (eg, mitogenicstimulation with PHA known totrigger both the TCWCD3 complex and CD2)29,”’or by stimuli that bypass surfacereceptor-mediated IM).I3 signaling (eg, PMA + A defect in antigen-induced T-cell activation leading to decreased lymphokine release canhave severalimportant implications for the pathogenesis of CVID. T cells act on isotype-uncommitted ornaive B cells by signaling via CD40 and modulate switch mechanismsat the DNA level.In addition, T cells support the expansion of committed B cells that already have undergone Ig isotype switching.”.” IL-2 is a potent inducer of human B-cell proliferation and differentiation,’j and deficient production of IL-2 by T cells on antigenic stimulation may contribute to the B-cell abnormalities observed in these CVID patients. In addition, decreased IFNy production, whether primary or secondary to the decreased IL-2 release, may also haveimplications for B-cell differentiati0n.j’ In agreement with this notion, patients with impaired TCR-mediated T-cellactivation showed aratheruniform pattern with respect to B-cell numbers and function. B-cell numberswerenormal, andthe B cells secretednormal amounts of IgM in response to several stimuli (PWM, SAC, IgM + IL-2) but were unable to produce IgG. A defect in the production of specific antibodies is common to all patients with CVID. The impairment of TCR-mediated signaling leading to reduced IL-2 and IFN-y production is likely to contribute to the pathophysiology of the disease in a significant subset of these patients. REFERENCES 1. Saiki 0, Ralph P, Cunningham-Rundles C, Good RA: Three distinct stages of B-cell defects in common varied immunodeficiency. Proc Natl Acad Sci USA 79:6008, 1982 2. Bryant A, Calver NC, Toubi E, Webster ADB, Farrant J: Classification of patients with common variable immunodeficiency by B-cell secretion of IgM and IgG in response to anti-IgM and interleukin-2. Clin Immunol Immunopathol 56:239, 1990 3. Farrant J, Bryant A, Almandoz F, Spickett G, Evans SW, Webster ADB: B-cell function in acquired “common variable” hypogammaglobulinaemia: Proliferative responses to lymphokines. Clin Immunol Immunopathol 5 1 : 196, 1989 4. Wright JJ, Wagner DK, Blaese RM, Hagengruber C, Waldmann TA, Fleisher TA: Characterization of common variable immunodeficiency: Identification of a subset of patients with distinctive immunophenotypic and clinical features. Blood 76:2046, 1990 5. Baumert E, Wolff-Vorbeck G , Schlesier M, Peter HH: Immunophenotypical alterations in a subset of patients with common variable immunodeficiency. Clin Exp Immunol 90:25, 1992 6. Waldmann TA, Broder S, Blaese RM, Durm M, Blackman M, Strober W: Role of suppressor T-cells in pathogenesis of common variable hypogammaglobulinaemia. Lancet 2:609, 1974 7. Sneller MC, Strober W: Abnormalities of lymphokine gene expression in patients with common variable immunodeficiency. J Immunol 144:3762, 1990 8. North ME, Spickett GP, Allsop J, Webster ADB, Farrant J: Defective DNA synthesis by T cells in acquired “common variable” hypogammaglobulinemia on stimulation with mitogens. Clin Exp Immunol 76: 19, 1989 9. North ME, Webster ADB, Farrant J: Role of interleukin-2 and interleukin-6 in the mitogen responsiveness of T-cells from patients with “common variable” hypogammaglobulinaemia. Clin Exp Immunol 81:412, 1990 10. Pastorelli G, Roncarolo MG, Touraine JL, Peronne G, Tovo PA, DeVries JE: Peripheral blood lymphocytes of patients with common variable immunodeficiency produce reduced levels of interleu- From www.bloodjournal.org by guest on February 6, 2015. For personal use only. IMPAIRED TCR-MEDIATED T-CELL ACTIVATION IN CVID kin-4, interleukin-2 and interferon-gamma, but proliferate normally upon activation by mitogens. Clin Exp Immunol 78:334, 1989 11. Rump JA, Jahreis A, Schlesier M, Drager R, Melchers I, Peter HH: Positive role of IL-2 deficiency for hypogammaglobulinemia in patients with common variable immunodeficiency. Clin Exp Immunol 89:204, 1992 12. Fiedler W, Sykora KW, Welte K, Kolitz JE, CunninghamRundles C, Holloway K, Miller GA, Souza L, Mertelsmann R: T cell activation defect in common variable immunodeficiency: Restoration by phorbol myristate acetate (PMA) or allogeneic macrophages. Clin Immunol Immunopathol44:206, 1987 13. Fischer MB, Hauber I, Vogel E, Wolf HM, Mannhalter JW, Eibl MM: Defective IL-2 and IFN-gamma gene expression in response to antigen in a subgroup of CVID patients. J Allergy Clin Immunol 92:340, 1993 14. Report of a WHO Scientific Group: Primary immunodeficiency diseases. Immunodeficiency Rev 3:195, 1992 15. Eibl MM, Mannhalter JW, Zlabinger G, Mayer WR, Tilz GP, Ahmad R, Zielinski CC: Defective macrophage function in a patient with common variable immunodeficiency. N Engl J Med 307:803 1982 16. Blayum A: Isolation of mononuclear cells and granulocytes from human blood. Scand J Clin Lab Invest 21:77, 1968 (suppl 97) 17. Eisenstein EM, Jaffe JS, Strober W: Reduced IL-2 production in common variable immunodeficiency is due to a primary abnormality of CD4’ T cell differentiation. J Clin Immunol 13:247, 1993 18. Jaffe JS, Eisenstein EM, Sneller MC, Strober W: T cell abnormalities in common variable immunodeficiency. Pediatr Res 33:24, 1993 19. Pandolfi F, Trentin L, San Martin JE, Wong JT, Kurnick JT, Moscicki RA: T cell heterogeneity in patients with common variable immunodeficiency as assessed by abnormalities of T cell subpopulations and T cell receptor gene analysis. Clin Exp Immunol 89:198, 1992 20. Mills GB, Cheung RK, Grinstein S, Gelfant EW: Increase in cytosolic free calcium concentration is an intracellular messenger for the production of interleukin 2 but not for expression ofthe interleukin 2 receptor. J Immunol 134:1640, 1985 21. Tamura T, Yanagida T, Nariuchi H: Difference in signal transduction pathway for IL-2 and IL-4 production in T helper 1 and T helper 2 cell clones in response to anti-CD3. J Immunol 151:6051, 1993 4241 22. Molina IJ, Sancho J, Terhorst C, Rosen FS, Remold-O’Donne11 E: T cells of patients with the Wiskott-Aldrich Syndrome have a restricted defect in proliferative responses. J Immunol 151:4383, 1993 23. Liu H, Lampe MA, Iregui MV, Cantor H: Conventional antigen and superantigen may be coupled to distinct and cooperative T cell activation pathways. Proc Natl Acad Sci USA 88:8705, 1991 24. Oyaizu N, Chirmule N, Yagura H, Pahwa R, Good RA, Pahwa S: Superantigen staphylococcal enterotoxin B-induced T helper cell activation is independent of CD4 molecules and phosphatidylinositol hydrolysis. Proc Natl Acad Sci USA 89:8035, 1992 25. Fleischer B, Schrezenmeier H: T cell stimulation by staphylococcal enterotoxins. J Exp Med 167:1697, 1988 26. Chatila T, Wood N, Parsonnet J, Geha RS: Toxic shock syndrome toxin- 1 induced inositol phospholipid turnover, protein kinase C translocation, and calcium mobilization in human T cells. J Immuno1 140:1250, 1988 27. Guba SC, Stella G, Turka LA, June CH, Thompson CB, Emerson SG: Regulation of interleukin 3 gene induction in normal human T cells. J Clin Invest 84:1701, 1989 28. Gottschalk LR, Giannola DM, Emerson SG: Molecular regulation of the human IL-3 gene: Inducible T cell-restricted expression requires intact AP-l and Elf-l nuclear protein binding sites. J Exp Med 178:1681, 1993 29. Chilson OP, Kelly-Chilson AE: Mitogenic lectins bind to the antigen receptor on human lymphocytes. Eur J Immunol 19:389, 1989 30. O’Flynn K, Krensky AM, Beverley PCL, Burakoff SJ, Linch DC: Phytohaemagglutinin activation of T cells through the sheep red blood cell receptors. Nature 313:686, 1985 31. Forman MS, Pur6 E: T-independent and T-dependent B lymphoblasts: Helper T cells prime for interleukin 2-induced growth and secretion of immunoglobulins that utilize downstream heavy chains. J Exp Med 173:687, 1991 32. van Vlasselaer P, Gascan H, de Wall Malefyt R, de Vries JE: IL-2 and a contact-mediated signal provided by TCR-alpha-beta or TCR-gamma-delta CD4 T cells induce polyclonal Ig production by committed human B cells. J Immunol 148:1674, 1992 33. Nakagawa T, Hirano T, Nagakawa N, Yoahizaki K, Kishimoto T: Effect of recombinant IL-2 and gamma-IFN on proliferation and differentiation of human B cells. J Immunol 134:959. 1985 From www.bloodjournal.org by guest on February 6, 2015. For personal use only. 1994 84: 4234-4241 A defect in the early phase of T-cell receptor-mediated T-cell activation in patients with common variable immunodeficiency MB Fischer, I Hauber, H Eggenbauer, V Thon, E Vogel, E Schaffer, J Lokaj, J Litzman, HM Wolf and JW Mannhalter Updated information and services can be found at: http://www.bloodjournal.org/content/84/12/4234.full.html Articles on similar topics can be found in the following Blood collections Information about reproducing this article in parts or in its entirety may be found online at: http://www.bloodjournal.org/site/misc/rights.xhtml#repub_requests Information about ordering reprints may be found online at: http://www.bloodjournal.org/site/misc/rights.xhtml#reprints Information about subscriptions and ASH membership may be found online at: http://www.bloodjournal.org/site/subscriptions/index.xhtml Blood (print ISSN 0006-4971, online ISSN 1528-0020), is published weekly by the American Society of Hematology, 2021 L St, NW, Suite 900, Washington DC 20036. Copyright 2011 by The American Society of Hematology; all rights reserved.
© Copyright 2026