1-s2.0-S1569905614607478-main
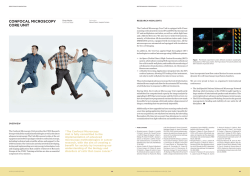
758 Intraoperative confocal laser endomicroscopy during robotic-assisted radical prostatectomy: Initial feasibility study Eur Urol Suppl 2014;13;e758 Print! Print! Lopez A., Mach K.E., Bui D., Liu J.J., Harris T., Leppert J.T., Mach K.E., Liao J.C. Stanford University School of Medicine, Dept. of Urology, Stanford, United States of America INTRODUCTION & OBJECTIVES: Robotic assisted radical prostatectomy (RARP) is a common surgical treatment for localized prostate cancer. Advances in intraoperative optical imaging technologies can potentially improve oncologic and functional outcomes of RARP. Confocal laser endomicroscopy (CLE) enables non-invasive optical biopsy of tissues of interest with dynamic visualization of tissue microarchitecture and cellular features. The objectives of this study are to develop a protocol for in vivo CLE imaging of prostatic and periprostatic structures during RARP and ex vivo CLE imaging of prostatic parenchymal structures with histopathological correlation. MATERIAL & METHODS: With local institutional review board approval, 13 patients scheduled for RARP were recruited. Probe-based CLE was performed with a Cellvizio® system (Mauna Kea Technologies, Paris France) using either a 0.85-mm (Uroflex B) or 2.6-mm probe (GastroFlex UHD) inserted through a standard laparoscopic port. Intravenous fluorescein (10%) was used as the optical contrast agent. Standard robotic instruments were used to grasp and direct the probe for image acquisition. TilePro™ functionality (Intuitive Surgical, Sunnyvale) was used to integrate the 3D-view of the operative field with CLE imaging. In selected patients, additional ex vivo imaging was performed on prostatectomy specimens following removal. Confocal video sequences were recorded for additional image processing after the procedure and compared with standard histopathological analysis. RESULTS: In vivo confocal endomicroscopy was successfully completed in all 13 patients with 52 video sequences obtained. There were no intraoperative or postoperative adverse events related to image acquisition or administration of fluorescein. Prostatic and periprostatic regions including capsule, neurovascular bundle, urethra, and bladder neck were imaged. Confocal imaging of the neurovascular bundle after nerve-sparing procedure revealed dynamic vascular flow and intact axonal fibers. Imaging of the bladder neck identified normal urothelium. Ex vivo CLE imaging of prostatic tissue slices and cores allowed visualization of parenchymal glandular and stromal structures that correlated with standard H&E staining. CONCLUSIONS: We report clinical feasibility and safety of in vivo microscopy using CLE during robotic-assisted surgery. Anatomic landmarks of oncologic and functional significance that may be helpful during surgical dissection were visualized. Pending further investigation, optical biopsy of prostatic and periprostatic tissues using CLE may be used for intraoperative surgical guidance to improve oncological and functional outcomes of RARP.
© Copyright 2026