p53 Mutations Are Associated With Resistance to
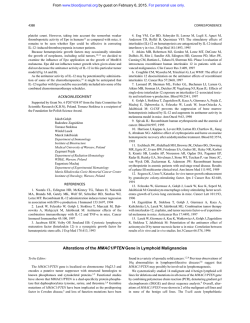
From www.bloodjournal.org by guest on February 6, 2015. For personal use only. p53 Mutations Are Associated With Resistance to Chemotherapy and Short Survival in Hematologic Malignancies By Eric Wattel, Claude Preudhomme, Bernard Hecquet, Michael Vanrumbeke, Bruno Quesnel, Isabelle Dervite, Pierre Morel, and Pierre Fenaux We analyzed the prognostic value of p53 mutations for response t o chemotherapy and survival in acute myeloid leukemia (AML), myelodysplastic syndrome(MDS), and chronic lymphocytic leukemia (CLL). Mutations were detected by single-stranded conformation polymorphism (SSCP) analysis of exons 4 t o 10 of theP53 gene, and confirmed by direct sequencing. A p53 mutation was found in 16 of 107 (15%) AML, 20 of 182 (11%) MDS, and 9 of 81 (11%) CLL tested. In AML, three of nine (33%) mutated cases and 66 of 81 (81%) nonmutated cases treated with intensivechemotherapy achieved complete remission(CR) ( P = .005) and none of five mutated cases and three of six nonmutated cases treated by low-dose Ara C achieved CR or partial remission (PR) ( P = .06). Median actuarial survival was 2.5 months in mutated cases, and 15 months in nonmutated cases ( P < lo-‘). In the MDS patients who received chemotherapy (intensive chemotherapy or low-dose Ara C), 1 of 13 (8%) mutated cases and 23 of 38 (60%) nonmutated cases achieved CR or PR ( P = .004), and medianactuarialsurvivalwas 2.5 and 13.5 months, respectively ( P C lo-’). In all MDS cases (treated and untreated), the survival difference between mutated cases and nonmutated cases was also highly significant. In CLL, 1 of 8 (12.5%) mutated cases treated bychemotherapy (chlorambucil andlor CHOP andlor fludarabine) responded, as compared with 29 of 36 (80%)nonmutated cases ( P = .02). In all CLL cases, survival from p53 analysis was significantly shorter in mutatedcases (median 7 months) thanin nonmutated cases (median not reached) ( P < IO-’). In 35 of the 45 mutated cases of AML, MDS, and CLL, cytogenetic analysis or SSCP and sequence findings showedloss of thenonmutated P53 allele. Our findings show that p53 mutations are a strong prognostic indicator of response t o chemotherapy and survival in AML, MDS, and CLL. The usual association of p53 mutations t o loss of the nonmutated P53 allele, in those disorders, ie, t o absence of normalp53 in tumor cells, suggests that p53 mutations could induce drug resistance, at least in part, by interfering with normal apoptotic pathways in tumor cells. 0 1994 by The American Societyof Hematology. T dominate in advanced stages of the disease and have been correlated withshort survival in carcinoma of the breast, prostate, lung, and s t o m a ~ h . ’ ~In‘ ’most ~ hematologic malignancies, p53 mutations also seem to be a late event in the disease course: in CML, they are almost exclusively seen after progression to acute leukemia4;in MDS, they predominate in patients with an excess of marrow blasts7and in CLL in patients with Binet’s stage C disea~e.”~ In a recent work, El Rouby et all’found a correlation between p53 mutations and resistance to chemotherapy in CLL. However, no other attempt at correlating p53 mutations to response to chemotherapy and survival in hematologic malignancies has been made, to our knowledge. In the past 3 years, we looked for p53 mutations in large series of hematologic malignancies. In this report, we tried to correlate the presence of those mutations to results of treatment and survival. HE p53 GENE IS a tumor suppressor gene often inactivated by deletion andor point mutation in most types of solid tumors.’.’ In hematologic malignancies, P53 gene mutations are found in 25% to 30% of Burkitt’s lymphoma” and chronic myeloid leukemia (CML) in blast crisis: 15% of chronic lymphocytic leukemia (CLL),3,’ and5% to 10%of acute myeloid leukemia (AML): myeloysplastic syndrome (MDS),’ and large cell non-Hodgkin’s lymphoma (NHL),’ but are very rare in acute lymphocytic leukemia (ALL, except in Burkitt’s ALL or in relapse)’ in multiple myeloma’” and in follicular NHL (except after histologic progression).” P53 gene mutations are generally missense mutations, involving almost exclusively exons 4 to 8 of the gene.’.’* They are generally detected by single-stranded conformation polymorphism (SSCP) analysis of DNA or immunocytochemical analysis of p53 in the nucleus of tumor cells because the latter method can only detect p53 with a prolonged half-life, which generally correspond to mutated p53.’ In solid tumors, P53 gene mutations are generally considered to be a late event in carcinogenesis because they preFrom the Service desMaladies duSang, CHU; Laboratoired’Himatologie A, Centre Hospitalier Universitaire; U,,,INSERM, Institut de Recherche sur le Cancer; and the Department of Biostatistics, Centre Oscar Lambret, Lille, France. Submitted April 14, 1994; accepted July IO, 1994. Supported by the Association de Recherche sur le Cancer, the Comite‘ du Nord de la Ligue contre le Cancer, the Gefiuc, and the Centre Hospitalier Universitaire of Lille. Address reprint requests to P. Fenaux, MD, Service des Maladies du Sang , CHU-l, Place de Verdun, 59037 Lille. France. The publication costsof this article were defrayed in part by page chargepayment. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C. section 1734 solely to indicate this fact. 0 1994 by The American Society of Hematology. 0006-4971/94/8409-002$3.00/0 3148 MATERIALS AND METHODS Patients Between January 1991 and December 1993, welooked for p53 mutations by single-stranded conformation polymorphism (SSCP) analysis of exons 4 to 10 of the P53 gene, a sensitive method for the detection of P53 gene mutations,I8 in 503 cases of hematologic malignancies diagnosed at our institution, including 107 cases of AML, 93 cases of ALL, 182 cases of MDS, 81 cases of CLL, and 40 cases of myeloma. In those patients, results of SSCP and sequence analysis of the P53 gene have already been published in part,5-7.9.~n.~9.20 Because p53 mutations were very rare inALLand myeloma (3 of 93 and 1 of 40 cases, respectively) comparisons between mutatedand nonmutated cases for initial characteristics, response to chemotherapy and survival were only made in AML, MDS, and CLL in the present study. AML and MDS were classified according to French-AmericanBritish (FAB) criteria2’,2zand CLL according to Binet’s classificat i ~ n . ’No ~ documented MDS phase was seen in any of the cases of AML. No familial history of Li Fraumeni syndrome or of clustering Blood, Vol 84, No 9 (November l), 1994: pp 3148-3157 From www.bloodjournal.org by guest on February 6, 2015. For personal use only. 31 49 p53 MUTATIONS AND RESISTANCETOCHEMOTHERAPY of malignancy (especially hematologic) was found in the AML, MDS, and CLL studied. Cytogenetic analysis was successfully performed at the time of DNA analysis in 103 of the 107 AML, 144 of the 182 MDS, and 40 of the 81 CLL using conventional banding techniques. Complex cytogenetic abnormalities were defined by the presence of at least three chromosome rearrangements. Cytogenetic results, in patients with p53 mutations, have been published with SSCP and sequencing data?”9.10.19.20 DNA was extracted from circulating leukocytes in acute leukemias with greater than 60% blasts and in CLL, and from bone marrow (BM) cells in other cases of acute leukemia and in MDS. DNA samples were obtained at diagnosis in all cases of AML and MDS. In CLL, DNA samples were obtained at diagnosis in 43 cases, and during the disease course in 38 cases; 18 of the CLL had received (or were receiving) chemotherapy when DNA samples were taken. Treatment AML. Patients were generally treated by conventional intensive anthracyclin-cytosine arabinoside (Ara C) chemotherapy, according to successive multicenter trials (LAM 86 and LAM 90 trials). Patients entering complete remission (CR) received consolidation chemotherapy with an anthracycline (or derivative) and Ara C, but a few patients with an identical HLA sibling were allografted in first CR. Elderly patients often received less intensive chemotherapy with low-dose Ara C (10 mg/m2/12 h subcutaneously during 3 weeks, followed by identical 14-day courses in case of response), but a few of them in poor general condition received no treatment apart from supportive care. MDS. Treatment was not randomized, but based on age, general condition, and disease course. Some relatively young patients with refractory anemia with excess blasts (RAEB), RAEB in transformation, or chronic myelomonocytic leukemia (CMML) received intensive anthracyclin-Ara C chemotherapy before or after progression toAML. Some older patients with RAEB, RAEB-T, or CMML received low-dose Ara C (same dosage as for AML), whereas the remaining patients received supportive care only or treatments other than chemotherapy (androgens, retinoids, or growth factors). In AML and MDS, complete remission (CR), partial remission (PR), resistance to chemotherapy, and death in aplasia were defined according to cancer and leukemia group B (CALGP) criteria?“ CLL. Stage A patients with stable disease were untreated. Stage B and C patients and stage A patients with progressive disease were treated by one ofthe following approaches: continuous or intermittent chlorambucil (with or without prednisone); cyclophosphamide, doxorubicin, vincristine, prednisone (CHOP) regimen with low -dose adriamycin (25 mg/m2on day 1 of each course)23;fludarabine (25 mg/m2/d, in 5-day courses). Stage B and C patients generally received “intensive” chemotherapy (CHOP or fludarabine), whereas stage A patients with progressive disease or elderly patients generally received chlorambucil (often followed by CHOP or fludarabine in the absence of response). In CLL, CR was defined by the absence of organomegaly, a lymphocyte count < 4 X lo9& a granulocyte count > 1.5 X lo9& and normal BM examination on core biopsies. PR was defined by a decrease of at least 50% in the diameter of enlarged lymph nodes and a decrease of the lymphocyte count by 75%.23 Analysis of p53 Gene Mutations The methods used for the detection of p53 mutations have been analyzed in detail elsewhere, and will only be summarized here.5.7.19.20 For exons 5 to 9 of the P53 gene, three genomic regions were amplified: region 1, encompassing exons 5 and 6 and intron 5 , and measuring 408 bp; region 2, encompassing exons 7 and 8 and intron 7, and measuring 610 bp. Because SSCP analysis seems to require fragments of less than 400 bp,I8 region 2 was digested after amplification and before SSCP analysis by Dra 1 enzyme because a Dra 1restriction site is present in intron 7. This led to two fragments encompassing exon 7 and exon 8, respectively, and measuring 392 and 218 bp;finally region 3, encompassing exons 8 and 9, and intron 8, and measuring 398 bp was amplified. Exons 4 and 10 were amplified separately. After amplification of the DNA segment considered, I pL of the reaction mixture for region 1, region 3,and exons 4 and IO was mixed with 19 p L of 0.1% sodium dodecyl sulfate (SDS) 20 mmol/ L EDTA solution. For region 2, 1 pL of the reaction mixture was first digested by 3 U of Dra 1 in 10 pL final-volume reaction, and diluted in 10 pL of SDS EDTA solution. Then 3 pL of the diluted reaction was mixed with 3 pL of a solution of 95% formamide 20 mmoVL EDTA, 0.05% bromophenol blue, and 0.05% xylene cyano], heated at 8 0 T , and applied (2 pL/lane) to a 5% polyacrylamide gel containing 90 mmoVL TRIS-borate pH 8.3, 4 mmoVl EDTA, and 10% glycerol. Electrophoresis was performed at 35 W for 5 to 6 hours at room temperature, with a fan for cooling. For direct sequencing, asymmetric polymerase chain reaction using a 50 to 100 reduction of one of the primers was performed. The resulting single-stranded DNA was purified and sequenced by the dideoxychain termination method, using the sequenase kit (US Biochemical, Cleveland, OH) and analyzed on a polyacrylamide gel containing 7 mol/L urea. Statistical Analysis The prognostic value of p53 mutations and other initial parameters on response to chemotherapy and survival was analyzed for each disorder (AML, MDS, CLL). Response rates to chemotherapy were compared by Student’s and chi-square tests. Survival curves were drawn using the Kaplan Meier method, and compared with the logrank test. Correlations between prognostic factors established by univariate analysis were studied by analysis of variance or chi-square test, depending on the nature of parameters. A multivariate analysis of factors that had shown prognostic value for survival in univariate analysis was also performed, using a Cox model.25 RESULTS Ident$cation of p53 Mutations AML. A P53 gene mutationwasdetectedby SSCP in 16 of the 107 (15%) patients analyzed by SSCP (Table 1). In those 16 cases, sequence analysis found a missense mutation in 11 cases, involving exon 4 (1 case), exon 5 (3 cases), exon 6(1 case), exon 7 ( 2 cases), and exon8 (4cases). In the remaining 5 cases, the mutation was astop codon mutation in exon 5 in 1 case, a l-bp deletion in 2 cases (exon 4, l case; exon 8, 1 case) a l-bp insertion in 1 case (in exon 7) and a mutation at the splicing acceptor site preceding exon 8 in the remaining case. In 10 of the 16 mutated cases, cytogenetic analysis found 17pmonosomy, resulting from monosomy 17, del17p, i(17q), or from unbalanced t(5;17)or t(7;17) translocations.26 Except in one case, 17p monosomywas part of complex cytogenetic abnormalities. In the remaining 6 mutatedcases, cytogenetic analysis found normal 17p in 3 cases and was not successfully performed in 3 cases. In 3 of those 6 cases (including two patients with cytogenetically normal 17p and one patient where no successful karyotype was obtained), SSCP and sequencing results showed complete disappearance of the residual germline bands, strongly suggesting loss From www.bloodjournal.org by guest on February 6, 2015. For personal use only. 3150 UPN WATTEL ET AL SexJAge FAB Type/ Binet's Stage p53 Mutations Loss of Normal p53 Allele Exon Codon Nucleotide Deleted C (CTA +TA) CGT TGT GTG + ATG AML 1209 541 20 F152 F167 F131 M2 M2 M2 8 8 8 264 273 272 C792 53 C961 F168 MI55 MI75 M4 M2 MO 4 5 5 110 175 166 111 410 FP3 MI54 M4 M2 5 7 1168 C319 498 1128 MI40 MI30 MI54 F180 MI85 MI61 M2 M2 M2 M1 M2 M2 CGT GGT CGC CAC TCA + TAA (stop codon) 7 237 ATG ATA Mutation at exon 8 splicing acceptor site: AG AT 8 273 CGT CTT 5 162 ATC + AGC 5 135 TGC AGC 238 TGT TAT 7 193 CAT CGT 6 122 Deleted G (GTG GT) 4 178 452 F160 MI79 M6 M5 8 7 MDS 1380 662 285 MI57 MI53 MI53 RAEB RAEB-T RAEB 7 8 MI40 F130 MI76 MI74 F128 MI57 F165 MI56 FP5 MI14 F165 MI57 FI75 MI63 FD9 F150 MI78 RAEB-T RAEB RAEB RAEB RAEB-T RAEB-T RAEB RAEB RAEB RAEB RAEB-T RAEB RAEB-T RAEB RAEB CMML RAEB 5 8 7 7 5 8 8 7 5 7 7 7 8 5 5 8 6 MI67 F155 MI63 MI63 MI74 M167 FP3 FP0 MI62 C B B C A C A C C 8 4 5 7 6 5 8 8 8 434 14 54 210 1005 11 12 31 6 1118 55 4 C641 c439 C1270 692 C1290 CLL 29 35 C1080 16 C l 005 C1013 28 52 C1066 - + -+ - + + - -+ + 282 255-256 - CGG TGG Inserted A between codon 255 and 256 + - 238 TGT TAT 273 CGT CAT p 53 rearrangement by Southern analysis CTG GTG 130 GAG + AAG 285 CGG CAG 285 TGC -t TAC 242 TGC + TGG 135 CGT CAT 273 CGT + CAT 273 ATG ATA 237 GTG CTG 173 CGG -t CAG 248 GGC AGC 245 246 ATG GTG CCT + CAT 278 ACC TCC 139 ATC AGC 162 CC insertion 301 TAT + TGT 220 + - + -+ + + + - + 281 130 239 219 135 273 273 273 GAC TAC 26-bp deletion CTC + GTC AAC AGC CCC CTC TGC TAC CGT .+CAT CGT CTT CGT + CTT + + + + + - + + + - + + + + + - + 34 8 1 LD Arac Anthr-AraC LD Arac LD Arac Anthr-AraC Resistance Resistance 3 7 No treatment Anthr-AraC Anthr-AraC LD Arac LD Arac Anthr-AraC Anthr-AraC Anthr-AraC LD Arac Resistance CR Resistance + + Anthr-AraC No treatment LD Arac No treatment Anthr-AraC Anthr-AraC No treatment Anthr-AraC No treatment Anthr-AraC LD Arac No treatment LD Arac No treatment No treatment LD Arac LD Arac Resistance CLB CHOP, Fludarabine CLB Fludarabine, CHOP No treatment CHOP, fludarabine CLB, CHOP Fludarabine CHOP, fludarabine Resistance Resistance Response Resistance + + + - + - + + + + - + + + - + + + + c 2 2 2 3 CR CR Resistance Resistance Death i n aplasia CR + + + + (mod Resistance Resistance Death in aplasia Resistance Resistance Resistance Anthr-AraC Anthr-AraC Anthr-AraC Anthr-AraC No treatment - Survival (mosl Response + + + Treatment Response Duration 4 8 4 6 2 3 1 5 6.5 2.5 3 1 8 2 2 8 2 8 3 5 6 3 2 3 3 5 3 3 Resistance Resistance Resistance Resistance Resistance Resistance Resistance Resistance Resistance Resistance Resistance Resistance Resistance Abbreviations: UPN, unique patient number; anthr-AraC, anthracycline-cytosine arabinoside; LD Arac, low-dose Ara C;CLB, 1 9 5 3+ 9 9 4+ 4 4+ 1 31 8 1 chlorambucil. From www.bloodjournal.org by guest on February 6, 2015. For personal use only. 3151 p53 MUTATIONS AND RESISTANCE TO CHEMOTHERAPY of the remaining nonmutated P53 allele. Thus, in 13 of the 16 mutated cases, it is highly probable that no normal p53 was synthesized in tumor cells. By contrast, 17p monosomy was seen in only 7 of the 90 nonmutated cases that were karyotyped. MDS. Twenty of the 182 MDS (1 1%) studied had a p53 mutation detected by SSCP (Table 1). Mutations consisted of a missense point mutation in 18 cases, involving exon 5 (5 cases), exon 6 ( 1 case), exon 7 (7 cases), and exon 8 (5 cases). One patient had a 2-bp (CC) insertion in exon 8. The remaining patient had a rearrangement of the P53 gene detectable by Southern analysis. Southern blot findings in this patient have previously been p~blished.~’ As for AML, 12 of the 20 mutated MDS cases had cytogenetically detectable 17p monosomy, through monosomy 17, del 17p, t(5;17), or t(7;17). In three additional patients, SSCP and sequencing results showed disappearance of the residual germline bands, also strongly suggesting loss of the remaining P53 allele in spite of cytogenetically normal 17p (1 case) or in the absence of cytogenetic data (2 cases). Thus, there was probably no normal p53 in the malignant cells in 15 mutated cases. All patients with 17p monosomy had complex cytogenetic findings. 17p monosomy was seen in only 4 of the 126 nonmutated cases that were karyotyped. CLL. Nine of the 81 patients (1 1%) had a mutation: missense mutation in 8 cases, involving exon 5 (2 cases), exon 6 ( l case), exon 7 (1 case), and exon 8 (4cases), and a 26-bp deletion in exon 4 (between codons 81 and 90) in the remaining patient (Table 1). Four of the 9 mutated cases had monosomy 17, and 3 additional mutated cases, where no cytogenetic analysis was performed, had no residual wild-type bands by SSCP and sequence analysis. This strongly suggested loss of the remaining P53 allele and the absence of normal p53 in tumor cells in those 7 cases. All patients with 17p monosomy had complex cytogenetic findings. None of the 35 nonmutated patients that were karyotyped had 17p monosomy. Patient Characteristics and Outcome AML. Comparisons between initial characteristics of the 16 mutated cases and the 91 nonmutated cases with followup data are shown in Table 2. Mutated cases, when compared with nonmutated cases, were characterized by significantly older age (mean, 60 v 49 years, P =.04), a higher incidence of complex cytogenetic abnormalities (84% of the cases v 19%in nonmutated cases, P = l X and of “unfavorable” cytogenetic abnormalities [ie, all cytogenetic abnormalities except t(8;21), inv(l6), and t(15;17)], 92% V 50% in nonmutated cases, P =.01. Of the 107 cases, 6 elderly patients in poor general condition received no chemotherapy and 101 were treated with chemotherapy, including 14 mutated and 87 nonmutated cases. Nine mutated cases received intensive chemotherapy, but only 3 (33%) achieved CR, of short duration (4, 4, and 5 months, respectively). By comparison, in nonmutated cases, 66 of the 81 (81%) patients treated by intensive chemotherapy achieved CR ( P =.005), and median CR duration was 13 months. Five mutated cases were treated with low- Table 2. Initial Characteristics and Outcome of AML Patients with a p53 Mutation, as Compared With Nonmutated Cases No. of Cases (%) Nonmutated Mutated Cases No. of patients Mean age (range) Male/female FAB type MO M1 M? M3 M4 M5 M.3 M7 Karyotype No. patients analyzed Normal t(8;21),inv(16),t(15;17) +8, -7 (single) Others (single) Complex abnormalities Results of treatment No. of treated patients Intensive chemotherapy CR (%) Resistance Death in aplasia Median CR duration (mod Low-dose Ara C CR PR Resistance Total responses (%) Median actuarial survival (mos) All treated patients Intensive chemotherapy Low-dose Ara C 16 60 2 17 (30-85) 9i7 1 1 10 0 2 1 1 0 (62.5%) P Value Cases 91 49 5 19 (3-81) 51l40 3 18 27 6 17 16 3 1 .04 NS NS (30%) 13 1 (8%) 0 0 1 1 1 (84%) 90 31 (34%) 14 (16%) 10 18 17 (19%) 14 9 3 (33%) 4 2 4 87 81 66 10 5 13 5 0 0 5 3 (21%) 6 2 1 3 69 2.5 5 3 15 15 8.5 (81%) 10-4 ,005 .06 (79%) 10-3 40-5 ,001 .03 Abbreviation: NS, not significant. dose Ara C, but none achieved CR or PR, as compared with 3 of the 6 nonmutated cases treated by this approach (P = .06). In the 101 patients who received chemotherapy, actuarial survival was significantly shorter in mutated cases (median, 2.5 months) than in nonmutated cases (median, 15 months) (P < (Fig 1). The difference was still significant when the analysis was restricted to patients treated by intensive chemotherapy and to patients treated by low-dose Ara C, respectively (Table 2). Apart from p53 mutations, age and karyotype were the only prognostic factors of response to chemotherapy and of survival in treated patients; older age and complex cytogenetic abnormalities (versus other karyotypes) were associated with a lower response rate to chemotherapy (P < and P < respectively) andwith shorter survival (P < From www.bloodjournal.org by guest on February 6, 2015. For personal use only. WATTEL ET AL 3152 Table 4. Initial Characteristics and Outcome of MDS Patients With a p53 Mutation, as Compared With Nonmutated Cases lil loo 00 !S All patients No. of patients Median age (range) 20 - 7 ””-”,Mutation I I 0 0 1 I 1 10 20 30 I , 40 , , , , 50 60 70 80 , I 90 100 Time (months) Fig 1. Actuarial survival of the l01 AML patients treated by chemotherapy; mutated cases (n = 14) versus nonmutated cases (n = 87) ( P < 10-9. and P < On the other hand, cytogenetics hadno significant prognostic value for response to chemotherapy and survival if patients with “unfavorable” karyotypes (as defined above) were compared with patients withnormal karyotype or t(8;21), inv(16), t(15;17). FAB classification also had no prognostic value. In treated patients, a significant correlation was found between p53 mutations and a complex karyotype ( P < and to a lesser extent between p53 mutations and age ( P =.03). In Cox’s multivariate analysis, presence versus absence of a complex karyotype emerged as the most powerful prognostic factor of survival, followed by presence of a p53 mutation and age (Table 3). MDS. As seen in Table 4, mutated cases of MDS were characterized by significantly lower age (mean, 57 v 65 years) ( P =.04); a higher incidence of high-risk MDS, ie, RAEB and RAEB-T ( P = 5 X a higher incidence of unfavorable karyotypes, ie, all abnormal karyotypes except isolated del 5q (89% v 34%) ( P and a higher incidence of complex cytogenetic abnormalities (83% v 16%) (P < Table 3. Multivariate Analysis of Prognostic Factors for Survival (Cox Model) Characteristic and Order of Entrance in Regression PValue Chi-square Model AML (treated patients) ( 1 ) karyotype (2) p53 mutations (3)age MDS (treated patients) ,008 ( 1 ) karyotype (2)p53 mutations .02 22.9 20.1 5q+8, (single) -7 Others (single) Complex abnormalities Progression to AML (%) Median actuarial survival (mod Patients treated with chemotherapy No. of patients Mean age Male/female FAB type RA RARS CMML RAEB RAEB-T Karyotype No. cases analyzed Normal Nonmutated Cases 20 57 t 18 ( 14-79) 1218 162 65 2 14 ( 19-89) 98/64 0 0 1 13 6 18 2 0 0 1 15 (83%) 1 1 (55%) 3 13 54 2 18 914 5q +8, -7 (single) Others (single) Complex abnormalities Results of treatment Intensive chemotherapy CR Resistance Death in aplasia Median CR duration Low dose Ara C CR PR Resistance Total responses (%) Median actuarial survival (mod 7 1 6 0 6 0 0 6 1 (8%) 2.5 P Value .04 NS 29 7 57 50 19 5x10‘ 126 78 5 10 13 20 29 27 10 (16%) <l0 (18%) .02 <l0 38 57 -t 15 2411 4 NS NS 0 0 9 18 11 NS 31 15 0 4 1 11 .01 21 13 7 1 10 17 3 7 7 23 (60%) 13.5 .03 .01 ,004 Abbreviation: NS, not significant. 13.1 6.9 5.2 CLL (all patients) 10(1)p53 mutations ,005 (2)karyotype 1.2 x 1 ob 3x Malelfemale FAB type RA RARS CMML RAEB RAEB-T Karyotype No. cases analyzed Normal Mutated Cases 24 7.8 Seven of the mutated cases received noChemotherapy. Seven received intensive anthracyclin-Ara C chemotherapy: one (14%) achieved CR, of 3-month duration, but six had resistant disease. By comparison, 21 of the nonmutated cases From www.bloodjournal.org by guest on February 6, 2015. For personal use only. 3153 p53 MUTATIONS AND RESISTANCE TO CHEMOTHERAPY received intensive chemotherapy, of whom 13 (62%) achieved CR (P =.03), and median CR duration was 10 months. Six of the mutated cases were treated with low-dose Ara C, but they all had resistant disease, whereas 10 of the 17 nonmutated cases (59%) treated with low-dose Ara C achieved CR or PR (P =.01). Overall, one mutated case (8%) responded to chemotherapy, as compared with 23 of 38 (60%) of the nonmutated cases (P =.W). Eleven of the mutated cases (55%) progressed to AML, as compared with 32 (18%) of the nonmutated cases (P = .02). Actuarial survival was significantly shorter in mutated cases, as compared with nonmutated cases, for all patients Table 5. Initial Characteristics and Outcome of CLL With a p53 Mutation, as Compared With Nonmutated Cases No. of Patients (%) Nonmutated Mutated Cases All patients No. of patients Mean age (range) M/F Binet’s stage A B C Karyotype (40 cases) Normal Single abn Complex abn Median actuarial survival (mod Patients treated with chemotherapy No. of patients Mean age M/F Binet‘s stage A B C Karyotype (20 cases) Normal Single abnormalities Complex abnormalities Results of treatment Chlorambucil PR No response CHOP and/or fludarabine CR PR No response Total responses (%) Median actuarial survival (mod 9 66 ? 6 (55-73) 6/3 2 Cases 72 64 ? 10 (37-85) 4713 1 NS NS 52 7 13 .01 27 5 2 X 10-4 1 4 3 2 5 0 8 64 rt 5 513 1 -30-5 36 63 ? 9 21/15 NS NS .03 2 5 23 5 8 0 14 10-3 0 4 2 3 18 14 1 2 6* 0 0 6 1 (125) 6.5 I 0 2 2 4 3 n 4 8 ~ ? 1 ~ Time (months) 100 NR 7 A 1 20 No mutation !, Mutation 0 B 0 10 20 30 40 50 60 70 80 90 Time (months) Fig 2. (A) Actuarial survival of the 182 MDS cases (treated or untreated); mutated cases (n = 20) versus nonmutated (n = 162) cases ( P lo-‘). (B) Actuarial survival of the 51 MDS patients who received chemotherapy; mutated cases (n = 13) versus nonmutated cases (n = 38) ( P < 0 4 21t 3 12 6 29 (80) 34 .02 <10-4 Abbreviations: NR, not reached; NS, not significant. One patient receivedCHOP after resistance to chlorambucil. t Three patients received CHOP or fludarabine after resistance to chlorambucil. (median, 3 v 27 months; P < lo-’)and for patients who received chemotherapy (median, 2.5 v 13.5 months; P < lo-’) (Fig 2, A and B). In the patients who received chemotherapy, presence of a complex karyotype was the only other prognostic factors of response to treatment (P =.04) and of survival (P < However, cytogenetic analysis had no prognostic value for response to treatment and survival if patients with “unfavorable” karyotypes (as defined above) were compared to patients with normal karyotype or del 5q. Age and FAB classi- From www.bloodjournal.org by guest on February 6, 2015. For personal use only. WATTEL ET AL 3154 fication also hadno prognostic value for response to treatment and survival in the patients who received chemotherapy. As for AML, p53 mutations were highly correlated In Cox’s multivariate to a complex karyotype ( P < analysis, complex cytogenetic findings also emerged as the most powerful prognostic factor of survival in MDS patients who received chemotherapy (Table 3). In all the 182 MDS patients, FAB classification ( P < IO-‘) and complex karyotype ( P < lo-‘) had prognostic value for survival in addition to p53 mutations. p53 mutations were strongly correlated to karyotype and FAB classification, as seen above. CLL. Three of the nine mutations were found at diagnosis, and six in DNA samples obtained 9 to 48 months after diagnosis (median, 21 months). Before DNA analysis, two of the six cases had received chlorambucil, and in two cases, progression from stage A to C had occurred. In nonmutated cases, DNA samples were taken at diagnosis in 40 cases, and after 6 to 196 months (median, 30) in the other 32 patients. Sixteen of them had received, or were receiving treatment (chlorambucil in 12 cases and CHOP in 4 cases) when DNA samples were collected. As seen in Table 5 , mutated CLL were characterized at the time of DNA analysis by a higher incidence of B and C Binet’s stages (78% v 28% in nonmutated cases, P =.01) and by a higher incidence of abnormal karyotypes (100% v 23%, P = 2 X IO-‘). One of the nine mutated cases remained stable and required no treatment. The other patients received chlorambucil and/or CHOP, andor fludarabine. Only one of the eight mutated cases who received chemotherapy responded (to chlorambucil). By comparison, 36 nonmutated cases did not require therapy. Thirty-six cases required therapy, and29 cases (80%)responded. The difference in response rate with mutated cases was significant ( P =.02). In the 8 1 CLL cases, median actuarial survival from DNA analysis was 7 months in mutated cases and not reached in nonmutated cases ( P < (Fig 3). The difference was l00 00 “p’... I l - L- . . l I I “l - 80 - 5 40 - I - I I Mutation I I”””“” I I E No mutation l I A .-> m v) 20 I ~ 0 , 0 I I 5 10 15 I I I 20 25 30 35 ,’ I 1 I I 40 45 50 55 I 1 60 Time (months) Fig 3. Actuarial survival of the 81 CLL patients (treated oruntreated); mutated cases (n = 9) versus nonmutated cases In = 72) (P < 10-5). also significant when the analysis was restricted to treated cases (Table 5). No prognostic factor of response to treatment other than the presence of a p53 mutation was seen. However, abnormal cytogenetic findings were correlated with shorter survival ( P = 2 X 10”) in treated patients. In the 81 CLL cases, Binet’s stage C ( P =.04) and abnormal karyotype ( P = 1 X were significantly associated with short survival. Correlations between p53 mutations and advanced Binet’s stage ( P =.01) and p53 mutations and abnormal karyotype ( P = l X were seen. In Cox’s multivariate analysis, p53 mutations emerged asthemost significant prognostic factor of survival inall CLL cases, followed by karyotype (Table 3). DISCUSSION In the present study, with additional patients tested, the incidence of p53 mutations remained similar to thatobserved in our initial papers, and reported by other groups: 10% to 15% in AML and CLL,3.s.’9.27.2R 14o to 3% in ALL (if Burkitt’s ALL and relapsing patients are not included), and myeloma.y~’0~2Y In MDS, the incidence of 11% of mutations was higher than the 3% incidence we had initially reported.’ This was probably because of the fact that, after our first report, we analyzed almost exclusively high-risk MDS cases (RAEB and RAEB-T). As in our earlier reports and in the literature, p53 mutations were generally missense mutations involving exons 4 to 8 of the gene. Because p53 mutations were rare in multiple myeloma and ALL, analysis of correlations between p53 mutations and response to chemotherapy and survival was restricted to AML, MDS, and CLL. Twenty-six of the 45 mutated cases of AML, MDS and CLL had cytogenetically detectable 17p monosomy andthus, probable loss of the normal residual P53 allele. In 9 additional mutated cases where no cytogenetic analysis was performed or no 17p monosomy was detected by cytogenetic analysis, SSCP, and sequence analysis showed loss of bands corresponding to the nonmutated P53 allele, also strongly suggesting loss of this allele. These findings confirmed the correlation between p53 mutationand deletion of the remaining P53 allele our group and other groups had observed in hematologic malignan~ies.~”.~~.~”.’~ As a consequence, in those disorders, no normal p53 is synthesized by the malignant clone in most of the mutated cases. In AML, MDS, and CLL, p53 mutations were significantly associated toknown high-risk factors. These included, in AML, the absence of “favorable” karyotypes [ie, t(8;21), t( 15;17), inv( 16)],and a much higher incidence of “unfavorable” karyotypes, particularly of complex cytogenetic abnormalities. In MDS, mutated cases were characterized by a higher incidence of RAEB and RAEB-T, the absence of RA and RARS, and also a much higher incidence of abnormal karyotypes, particularly of complex cytogenetic findings. In CLL, mutated cases predominantly had Binet’s stage B and C disease, and also complex cytogenetic findings. In other reports that correlated p53 mutations with clinical and hematologic features, mutations also predominated inpatients with high-risk features, particularly in CLL, large cell lymphoma and MDS.3.X,i2 Furthermore, in CML, p53 muta- From www.bloodjournal.org by guest on February 6, 2015. For personal use only. p53 MUTATIONS AND RESISTANCETOCHEMOTHERAPY tions were almost exclusively seen after progression to AML4; in follicular lymphoma, they were rarely seen before progression to large cell lymphoma''; in ALL (with the exception of Burkitt's ALL), they predominated in relapsing patient^.'^.^' The fact that p53 mutations are mainly seen in advanced or relapsing hematologic malignancies suggests that they are associated with poor response to chemotherapy. However, to our knowledge, very few studies have addressed this issue. In several types of solid tumors, p53 mutations (or p53 overexpression detected by immunocytochemistry) have been associated with poor prognostic factors, including a large tumor mass and/or a highly proliferative tumor, and short s ~ r v i v a l . ' ~ "However, ~ . ~ ~ if two reports correlated p53 overexpression to resistance to hormone therapy in prostatic carcinomaI4and radiation therapy in breast car~inoma:~respectively, no analysis of response to chemotherapy in relation to p53 mutation or overexpression was made in those papers. Recently, El Rouby et all7 found that in CLL, the response rate to chemotherapy (chlorambucil, fludarabine, or combination chemotherapy) was very low in patients with a p53 mutation (one of seven responses) as compared with patients without p53 mutation (27 of 29 responses). The prognostic value of p53 mutations for response to chemotherapy persisted after adjustment for risk factors (including age, sex, and Rai's stage). In this report, we clearly confirmed the prognostic value of p53 mutations for response to chemotherapy in CLL. p53 mutations were correlated with disease stage (according to Binet's classification) and with abnormal karyotypes (especially complex cytogenetic findings), but p53 mutations emerged as the strongest prognostic factor for survival in Cox's multivariate analysis. In AML, p53 mutations were associated with significantly poorer response to intensive chemotherapy and to low-dose Ara C, and the only three mutated cases that responded to chemotherapy had short remission. The survival difference between mutated and nonmutated cases was highly significant. In the mutated group, which included more elderly patients, a higher proportion of cases received low-dose Ara C, which is less effective than intensive chemotherapy in AML.34However, the survival difference between mutated and nonmutated cases persisted when patients treated by intensive chemotherapy and low-dose Ara C were analyzed separately. A high correlation between p53 mutations and complex cytogenetic findings was found, and in Cox's multivariate analysis, complex karyotype emerged as the most powerful prognostic factor for survival before p53 mutations. Previous studies had established the prognostic value of cytogenetics in AML, and especially the poor prognosis of complex cytogenetic finding^.^^.^^ As for AML, MDS with a P53 gene mutation had significantly lower response rates to chemotherapy and shorter survival than nonmutated cases. p53 mutations were also strongly correlated to the presence of a complex karyotype, and complex cytogenetic findings emerged as the strongest prognostic factor of survival by multivariate analysis. Our previous experience had shown that karyotype was a major independent prognostic factor of response to intensive chem ~ t h e r a p yand ~ ~ of survival3sin MDS. 3155 Our present findings showed that the presence of p53 mutations in the hematologic malignancies we studied was a strong prognostic factor of response to chemotherapy, whichwas highly correlated to the presence of complex cytogenetic findings. Thus, it is unclear whether p53 mutations were one of the causes of resistance to chemotherapy, because they occurred in a context of numerous other genetic abnormalities that could have played, rather than p53 mutations, a major role in this resistance. On the other hand, p53 protein seems to be involved in DNA repair, and its inactivation increases the probability of mutations of other genes.39Therefore, p53 mutations could have been the cause rather than the consequence of the multiple chromosomal abnormalities to which they were associated. If p53 mutations were one of the factors of resistance to chemotherapy in the diseases we studied, the mechanisms whereby p53 mutations induced resistance to chemotherapy can only be hypothesized. First, it has been shown that normal p53 suppressed the multidrug resistance (mdrl) gene promoter, whereas mutated p53 could stimulate it.40Expression of the mdr, gene has been correlated to resistance to chemotherapy inmany tumor types, including AML4' and MDS.4' Therefore mutated p53, by activating mdr, expression, could interfere with response to chemotherapy. However two recent reports in AML43 and CLL" and our report in MDSMfailed to show a correlation between p53 mutations and mdr, gene expression. A second hypothesis can be made by considering the role of p53 in programmed cell death (apoptosis). It has recently been suggested that some chemotherapeutic agents, including anthracycline derivative^^^ and Ara CM could induce leukemic cell death, at least in part, by triggering apoptosis. p53 appears to be required for the induction of apoptosis induced by irradiation or heat shock in cell lines.47Total absence of p53 through mutation of one P53 allele and loss of the other P53 allele, as found in most of our mutated cases, could have explained their resistance to chemotherapy. Because loss of only one allele of the wild-type p53 already can induce increased resistance to apoptosis>' this explanation could also hold for patients who had retained one normal P53 allele. Finally, the role of p53 mutations in drug resistance could be regarded as minor in hematologic malignancies because p53 mutations are, overall, relatively rare in those disorders. On the other hand, p53 mutations are frequently seenin relapsing hematologic malignancies or in cell lines etablished from leukemic patients in relapse.48Using a very sensitive method of p53 mutation detection, Wada et a148 found that the p53 mutations present in several leukemic cell lines were already present at diagnosis invery small proportion of cells andin a larger percentage of cells in relapse. The same type of clonal expansion of p53 mutant cells during disease course had also been observed in brain tum0rs.4~Therefore, the possibility exists that a relatively large number of leukemias (and possibly of other hematologic malignancies) carry a very small cell population with mutated p53 at diagnosis, undetectable by conventional methods (especially SSCP). This population could be resistant to chemotherapy, which would facilitate relapse with a predominantly p53 mutated cell population. If those findings From www.bloodjournal.org by guest on February 6, 2015. For personal use only. 31 56 WATTEL ET AL were confirmed, therole of p53 mutations in drug resistance in hematologic malignancies wouldbe greater than expected. REFERENCES 1. Hams CC,Hollstein M: Clinical implications of the p53 tumorsuppressor gene. N Engl J Med 329: 1318, 1993 2. Levine A, Momand J, FinlayC: The PS3 tumour suppressor gene. Nature 3S1:453, 1991 3. Gaidano G, Ballerini P, Gong J, Inghirami G, Neri A, Newcomb E, Magrath I, Knowles D, Dalla Favera R: p53 mutations in human lymphoid malignancies: Association with Burkitt lymphoma USA and chronic lymphocytic leukemia. Proc Natl AcadSci 88:5413, 1991 4. Ahuja H, Bar-eli M, Arlin Z, Advani S, Allen SL, Goldman J, Snyder D, Foti A, ClineM: The spectrum of molecular alterations in the evolution of chronic myelocytic leukemia. J Clin Invest 87:2042, 1991 5. Fenaux P, Preudhomme C, Lai JL, Quiquandon I, Jonveaux PH, Vanrumbeke M, Sartiaux C, Morel P, Loucheux-Lefebvre MH, Bauters F, Berger R, Kerckaert JP: Mutations of the P 53 gene in B cell chronic lymphocytic leukemia. A report on 39 cases with cytogenetic analysis. Leukemia 6:246, 1992 6. Fenaux P, Jonveaux P, Quiquandon I, Lai JL, Pignon JM, Loucheux-Lefebvre MH, Bauters F, Berger R, Kerckaert JP: p53 gene mutations in acute myeloid leukemia with17p monosomy. Blood 78:1652, 1991 7. Jonveaux P, Fenaux P, Pignon JM, Lai JL, Quiquandon 1, Kerckaert JP, Loucheux-Lefebvre MH, Goossens M, Bauters F, Berger R: Mutations of the P53 gene in myelodysplastic syndromes. Oncogene 6:2243, 1991 8. Ichikawa A, Hotta T, Takagi N, Tsushita K, Kinoshita T, Nagai H, Murakami Y, Hayashi K, Saito H: Mutations of P53 gene and their relation to disease progression in B-cell lymphoma. Blood 792701, 1992 9. Fenaux P, Jonveaux P, Quiquandon I, Preudhomme C, Lai JL, Vanrumbeke M, Loucheux-Lefebvre MH, Bauters F, Berger R, Kerckaert JP: Mutations of the p53 gene in B cell acute lymphoblastic leukemia. A report on 60 cases. Leukemia 6:42, 1992 IO. Preudhomme C, Facon T, Zandecki M, Vanrumbeke M, Lai JL, Nataf E, Loucheux-Lefebvre MH, Kerckaert JP, Fenaux P: Rare occurrence of PS3 gene mutations in multiple myeloma. Br J Haemato1 81:440, 1992 1 1 . Sander CA, Yano T, Clark HM, Harris C, Longo DL, Jaffe ES, Raffeld M: p53 mutation is associated with progression in follicular lymphomas. Blood 82:1994, 1993 12. Caron De Fromentel C, Soussi T: p53tumor suppressor gene: A mode for investigating human mutagenesis. Genes Chromosom Cancer 4: 1, 1992 13. Silvestrini R, Benini E, Daidone MG: p53 as an independant prognostic marker in lymph node-negative breast cancer patients. J Natl Cancer Inst 95:96S, 1993 14. Visakorpi T, Kallioniemi OP, Heikkinen A, Koivula T, Isola J: Small subgroup of aggressive, highly proliferative prostatic carcinomas defined by p53 accumulation. J Natl Cancer Inst 84383, 1992 15. Martin HM, Filipe MI, Morris RW, Lane DP, Silvestre F: p53 expression and prognosis in gastric carcinoma. Int J Cancer S0:8S9, 1992 16. Marchetti A, Buttitta F, Merlo G, Diella F, Pellegrini S, Pepe S, Macchiarini P, Chella A, Angeletti A, Callahan R, Bistacchi M, Squartini F: p53 alterations in non-small cell lung cancers correlate with metastatic involvement of hilar and mediastinal lymph nodes. Cancer Res S3:2846, 1993 17. El Rouby S, Thomas A, Costin D, Rosenberg CR. Potmesil M, Silber R, Newcomb EW: p53 gene mutation in B-cell chronic lymphocytic leukemia is associated with drug resistance and is independent of MDRlMDR3 gene expression. Blood 82:3452, 1993 18. Orita M, Suzuki Y, Sekuja T, Hayashi K: Rapid and sensitive detection of point mutations and DNA polymorphisms usingthe PCR. Genomics 5:874, 1989 19. Fenaux P, Preudhomme C, Quiquandon I, Jonveaux P,Lai JL, Vanrumbeke M, Loucheux-Lefebvre MH, Bauters F, Berger R, Kerckaert J P Mutations of the PS3 gene in acute myeloid leukemia. Br J Haematol 80: 178, 1992 20. Lepelley P, Preudhomme C, Vanrumbeke M, Quesnel B, Cosson A, Fenaux P: Detection of p53 mutations in hematological malignancies: Comparison between immunocytochemistry and DNA analysis. Leukemia (in press) 21. Bennett JM, Catovsky D, Daniel MT, Flandrin G, Galton DAG, Gralnick HR, Sultan C: Proposed revised criteria for the classification of acute myeloid leukemia. A report of the French-Amencan-British Cooperative Groups. Ann Int Med 103:626, 1985 22. Bennett J, Catovsky D, Daniel MT, Flandrin G, Galton D, Gralnick H, Sultan C: Proposals for the classification of myelodysplastic syndromes. Br J Haematol 51:189, 1982 23. French Cooperative Group on Chronic Lymphocytic Leukemia: A randomized clinical trail of' chlorambucil versus CHOP in stage B chronic lymphocytic leukemia. Blood 75:1422, 1990 24. Ellison RR, Holland JF. Weil M: Arabinosyl cytosine: A useful agent in the treatment of acute leukemia in adults. Blood 32:507, 1968 25. Cox DR: Regression models and life-tables (with discussion). J R Stat Soc B 34:487, 1972 26. Lai JL, Zandecki M, Fenaux P, Le Baron F, Bauters F, Cosson A, Deminatti M: Translocations (5;17) and (7;17) in patients with de novo or therapy related myelodysplastic syndromes. Cancer Genet Cytogenet 46:173, 1990 27. Fenaux P, Collyn D'hooghe M, Lai JL, Bauters F, Loucheux MH, Kerckaert JP: Rearrangement and expression of the p 53 gene in myelodysplastic syndrome and acute myeloid leukemia. Nouv Rev Fr Hematol 32541, 1990 28. Hu G, Zhang W, Deisseroth AB: P53 gene mutations in acute myelogenous leukaemia. Br J Haematol 81:489, 1992 29. Wada M, Bartram CR, Nakamura H, Hachiya M, Chen DL, Borenstein J, Miller CW, Ludwig L, Hansen-hagge TE, Ludwig WD, Reiter A, Mizoguchi H, Koeffler P: Analysis of p53 mutations in a large series of lymphoid hematologic malignancies of childhood. Blood 82:3163, 1993 30. Nakai H, Misawa S, Tanaka S: p53 gene mutations and loss of a chromosome 17p in Philadelphia chromosome (Ph')-positive acute leukemia. Leukemia 7:1S47, 1993 31. Felix CA, Nau MM, Takahashi T: Hereditary and acquired p53 gene mutations in childhood acute lymphoblastic leukemia. J Clin Invest 89:640, 1992 32. Ludwig L, Schulz AS, Janssen JWG, Grunewald K,Bartram CR: p53 mutations in myelodysplastic syndromes. Leukemia 6: 1302, I992 33. Thor AD, Moore DH, Edgerton SM, Kawasaki M, Rechsaus E, Lynch E, Marcus J , Schwartz J , Chen L, Maya UB, Smith H: Accumulation of p53 tumor suppressor gene protein: An independent marker of prognosis in breast cancers. J Natl Cancer Inst 84:845, 1992 34. Cheson BD, Jasperse DM, Simon R, Friedman MA: A critical appraisal of low-dose cytosine arabinoside in patients with acute non-lymphocytic leukemia and myelodysplastic syndromes. J Clin Oncol 4: 1857, 1986 35. Fenaux P, Preudhomme C, Lai JL, Morel P, Beuscart R, Bauters F Cytogenetics and their prognostic value in de novo ANLL: A repon on 283 cases. Br J Haematol 73:61, 1989 36. Schiffer CA, Lee EJ, Tomiyasu T, Wiernik PH, Testa JR: From www.bloodjournal.org by guest on February 6, 2015. For personal use only. p53 MUTATIONS AND RESISTANCE TO CHEMOTHERAPY Prognostic impact of cytogenetic abnormalities in patients with de novo acute nonlymphocytic leukemia. Blood 73:263, 1989 37. Fenaux P, Morel P, Rose C, Lai JL, Jouet JP, Bauters F: Prognostic factors in adult de novo myelodysplastic syndromes treated by intensive chemotherapy. Br J Haematol 77:497, 1991 38. Morel P, Hebbar M, Lai JL, Duhamel A, Preudhomme C, Wattel E, Bauters F, Fenaux P: Cytogenetic analysis has strong independant prognostic value in de novo myelodysplastic syndromes and can be incorporated in a new scoring system: A report on 408 cases. Leukemia 7:1315, 1993 39. Hartwell L: Defects in a cell cycle checkpoint may be responsible for the genomic instability of cancer cells. Cell1 71543, 1992 40. Chin KV, Ueda K, Pastan I, Gottesman MM: Modulation of activity of the promoter of the human MDRl gene by ras and p53. Science 255:459, 1992 41. Campos L, Guyotat D,Archimbaud E, Calmard-Otiol P, Tsuruo T, Troncy J, Treille D, Fiere D, Fiere D: Clinical significance of multidrug resistance p-glycoprotein expression in acute nonlymphoblastic leukemia cells at diagnosis. Blood 79:473, 1992 42. Lepelley P, Soenen V, Preudhomme C, Lai JL, Cosson A, Fenaux P: Expression of the multidrug resistance P glycoprotein and its relationship to hematological characteristics and response to treatment in myelodysplastic syndromes. Leukemia 8:998, 1994 43. Zhao B, Drach D, Hu G, Squires J, Drach J, Deisseroth A, Andreeff M: Absence of regulation of MDRl by p53 in normal 3157 hematopoiesis and acute myelogenous leukemia. Blood 80:202a, 1992 (abstr, suppl) 44. Preudhomme C, Lepelley P, Vachee V, Soenen V, Quesnel B, Cosson A, Fenaux P: Relationship between P53 gene mutations and multidrug resistance (mdrl) gene expression in myelodysplastic syndromes. Leukemia 7:1888, 1993 45. Bhalla K, Ibrado AM, Tourkina E, Tang C, Grant S, Bullock G, Huang Y, Ponnathpur V, Mahoney ME: High-dose mitoxantrone induces programmed cell death or apoptosis in human myeloid leukemia cells. Blood 82:3133, 1993 46. Gunji H, Kharbanda S, Kufe D: Induction of internucleosomal DNA fragmentation inhuman myeloid leukemia cells by I-B-Darabinofuranosylcytosine. Cancer Res 51 :741, 1991 47. Lotem J, Sachs L: Hematopoietic cells from mice deficient in wild-type p53 are more resistant to induction of apoptosis by some agents. Blood 82:1092, 1993 48. Wada H, Asada M, Nakazawa S, Itoh H, Kobayashi Y, lnoue T, Fukumuro K, Chon Chan L, Sugita K, Hanada R, Akuta N, Kobayasbi N, Mizutani S: Clonal expansion of p53 mutant cells in leukemia progression in vitro. Leukemia 853, 1994 49. Sidransky D, Mikkelsen T, Schwechheimer K, Rosenblum M.L, Cavanee W, Vogelstein B. Clonal expansion of p53 mutant cells is associated with brain tumour progression. Nature 355346, 1992 From www.bloodjournal.org by guest on February 6, 2015. For personal use only. 1994 84: 3148-3157 p53 mutations are associated with resistance to chemotherapy and short survival in hematologic malignancies E Wattel, C Preudhomme, B Hecquet, M Vanrumbeke, B Quesnel, I Dervite, P Morel and P Fenaux Updated information and services can be found at: http://www.bloodjournal.org/content/84/9/3148.full.html Articles on similar topics can be found in the following Blood collections Information about reproducing this article in parts or in its entirety may be found online at: http://www.bloodjournal.org/site/misc/rights.xhtml#repub_requests Information about ordering reprints may be found online at: http://www.bloodjournal.org/site/misc/rights.xhtml#reprints Information about subscriptions and ASH membership may be found online at: http://www.bloodjournal.org/site/subscriptions/index.xhtml Blood (print ISSN 0006-4971, online ISSN 1528-0020), is published weekly by the American Society of Hematology, 2021 L St, NW, Suite 900, Washington DC 20036. Copyright 2011 by The American Society of Hematology; all rights reserved.
© Copyright 2026