Myeloid and Erythroid Progenitor Cells From Normal Bone
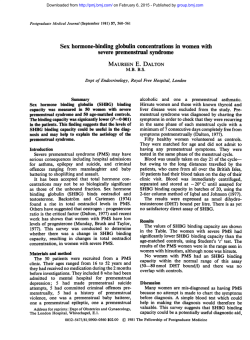
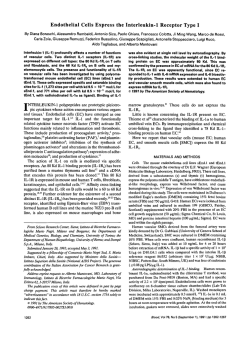
From www.bloodjournal.org by guest on February 6, 2015. For personal use only. Myeloid and Erythroid Progenitor Cells From Normal Bone Marrow Adhere To Collagen Type I By Michael Koenigsmann, James D. Griffin, Jennifer DiCarlo, and Stephen A. Cannistra One of the mechanisms by which normal hematopoietic progenitor cells remain localized within the bone marrow microenvironment is likely t o involve adhesion of these cells t o extracellular matrix (ECM) proteins. For example, there is evidence that uncommitted, HLA-DR-negative progenitor cells and committed erythroid precursors (BFU-E) bind t o fibronectin. However, fibronectin is not known t o mediate binding of committed myeloid (granulocyte-macrophage) progenitors, raising the possibility that other ECM proteins may be involved in this process. We investigated the binding of the M 0 7 myeloid cell line t o a variety of ECM proteins and observed significant specific binding t o collagen type I (56% 2 5%). minimal binding t o fibronectin (18% k 4%) or t o laminin (19% 2 5%). and no binding to collagen type 111, IV, or V. Similarly, normal bone marrow myeloid progenitor cells (CFU-GM) demonstrated significant specific binding t o collagen type I(46% f 8% and 47% f 12% for day 7 CFU-GM and day 14 CFU-GM, respectively). The ability of collagen t o mediate bidding of progenitor cells was not restricted t o the myeloid lineage, as BFU-E also showed significant binding t o this ECM protein (40% f 10%). The binding of M 0 7 cells and CFU-GM was collagen-mediated, as demonstrated by complete inhibition of adherence after treatment with collagenase type VII, which was shown t o specifically degrade collagen. Binding was not affected by anti-CD29 neutralizing antibody (anti-p-I integrin), the RGD-containing peptide sequence GRGDTP, or divalent cation chelation, suggesting that collagen binding is not mediated by the p-1integrin class of adhesion proteins. Finally, mature peripheral blood neutrophils and monocytes were also found t o bind t o collagen type I (25% f 8% and 29% 2 6%, respectively). These data suggest that collagen type Imay play a role in the localization of committed myeloid and erythroid progenitors within the bone marrow microenvironment. o 1992by The American Society of Hematology. H providing a potential mechanism for the release of mature red blood cells (RBCs) from the bone marrow into the peripheral Thus, both the pattern of progenitor cell binding to fibronectin as well as the recognition sites for binding to this molecule change as the progenitor cell acquires a more committed phenotype. Although fibronectin may partly mediate the binding of uncommitted, HLA-DR-negative progenitors and committed erythroid precursors, it is likely that this protein does not play a major role in the localization of committed myeloid progenitors such as CFU-GM within the bone marrow. However, other ECM proteins in the bone marrow that could be involved in the binding of committed myeloid progenitors include hemonectin, collagen types I, 111, and IV, and laminin. Hemonectin is a 60-Kd protein purified from rabbit ECM that has been observed to support the binding of murine CFU-GM and, to a lesser extent, erythroid burst forming units (BFU-E) in vitro.8 Myeloid binding to hemonectin appears to be differentiationassociated, with more mature cells such as bands and polymorphonuclear leukocytes exhibiting decreased adhe- EMATOPOIESIS OCCURS through a series of orderly steps involving proliferation, commitment, and differentiation of early bone marrow progenitor cells, ultimately leading to the release of mature cells into the peripheral blood. To ensure that hematopoietic progenitors are provided with appropriate conditions for development, including the availability of humoral growth factors, it is likely that specific mechanisms exist for the adhesion of these cells to bone marrow stromal cells or to extracellular matrix (ECM) proteins during maturation. For example, early murine progenitors with high proliferative capacity are preferentially located in the adherent cell layer of long-term marrow cultures.’ In human studies, uncommitted, HLA-DR-negative progenitors capable of repopulating long-term marrow cultures have been shown to avidly bind to the stromal cell layer, whereas more committed progenitors exhibit significantly reduced binding.’ Although the mechanism for the adhesion of early progenitors to the stromal cell layer is not fully understood, there is increasing evidence that the ECM protein fibronectin plays an important role in this process. For example, uncommitted, HLADR-negative progenitors selectively bind in vitro to the heparin binding domain I1 of fibronectin, an epitope that is recognized by the VLA-4 molecule of the p-1 integrin family.”4 Interestingly, as early progenitors become more committed, as indicated by expression of HLA-DR, their binding to fibronectin is altered in two major ways. First, binding of committed progenitors appears to be mediated through an additional region of the fibronectin molecule termed the cell binding domain, an area recognized by the VLA-5 integrin. Second, only the erythroid subset of committed progenitors appears to maintain significant binding avidity for fibronectin, with other committed progenitors such as granulocyte-macrophage colony-forming units (CFU-GM) demonstrating significantly reduced binding to this ECM p r ~ t e i nThe . ~ binding of erythroid progenitors to fibronectin is differentiation-dependent, with progressive loss of binding as the cells mature into erythrocytes, thereby Blood, Vol79, No 3 (February I), 1992: pp 657-665 From the Divisions of Tumor Immunology and Medical Oncology, Dana-Farber Cancer Institute, Harvard Medical School, Boston, MA. Submitted June 13, 1991; accepted September 30, 1991. Supported in part by Public Health Service Grant Nos. CA 36167, CA 42802, and CA 34183, Biomedical Research Support Grant No. SO7RRO5526-26, and by the US Cancer Research Council. M.K. is a grant recipient of the Deutsche Forschungsgemeinschap. J.D.G. is a scholar of the Leukemia Society ofAmerica. Address reprints to Stephen A . Cannistra, MD, Division of Tumor Immunology, Dana-Farber Cancer Institute, 44 Binney St, Boston, MA 02115. The publication costs of this article were defrayed in part by page charge payment. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C. section 1734 solely to indicate this fact. 0 1992 by The American Society of Hematology. 0006-4971I9217903-0005$3.00/0 657 From www.bloodjournal.org by guest on February 6, 2015. For personal use only. KOENIGSMANN ET AL 658 sion to this molecule when compared with undifferentiated blasts. Although the molecular structure of hemonectin and its relationship to other adhesion proteins are unknown, the ability of this protein to support the binding of CFU-GM in a differentiation-associated fashion deserves further investigation. The role of collagen in the localization and development of progenitor cells within the bone marrow is of interest for several reasons. Collagen types I, 111, and IV are major constituents of the bone marrow ECM,'.'' and hematopoietic precursor cells express molecules such as CD44I3that are known to recognize ~ o l l a g e n . Furthermore, ~~~'~ inhibition of collagen synthesis by cis-4-hydroxyprolineinterferes with the generation of a functional stromal microenvironment in vitro.16 In view of these considerations, the goal of the present study was to assess the binding of hematopoietic cells to a variety of ECM proteins to determine possible mechanisms by which committed myeloid progenitor cells remain localized within the bone marrow during development. We report that collagen type I supports significant binding of normal myeloid and erythroid progenitor cells, and that this binding is not mediated by the p-1 integrin family of adhesion proteins; furthermore, mature myeloid cells also bind to collagen type I. The implications of these results for the mechanism of progenitor cell localization to the bone marrow are discussed. MATERIALS AND METHODS Reagents. Purified ECM proteins were obtained as follows: collagen type I (bovine), collagen type IV (murine), and laminin (murine) from Collaborative Research (Bedford, MA); collagens type I11 (human) and V (human) from Sigma (St Louis, MO) (Sigma designations X and IX); fibronectin (human) from Telios (San Diego, CA). Recombinant human granulocyte-macrophage colony-stimulating factor (GM-CSF), interleukin-3 (IL-3), and erythropoietin were kindly provided by Dr Steven Clark (Genetics Institute, Cambridge, MA). The following murine monoclonal antibodies that recognize adhesion proteins were used as part of this study: 4B4 (anti-CD29, pl integrin), 8F2 (anti-VLA-4), 2H6 (anti-VLA-5), and IF7 (anti-CD26) were gifts of Dr Chikao Morimoto (Dana Farber Cancer Institute [DFCI], Boston, MA); TS2/7 (anti-VLA-1) was a gift of Dr Martin Hemler (DFCI); 12F1 (anti-VLA-2) was a gift of Dr Virgil Woods (University of San Diego, San Diego, CA); 5143 (anti-VLA-3) was a gift of Dr Anthony Albino (Memorial Sloan Kettering Institute, New York, NY); GoH3 (anti-VLA-6) was a gift of Dr Arnoud Sonnenberg (University of Amsterdam, Amsterdam, The Netherlands); and 515 (anti-CD44) was a gift of Dr Goeffrey Kansas (DFCI). Fetal calf serum (FCS) for colony cultures was purchased from HyClone (Logan, UT). Materials used for serum-free cell culture were obtained as follows: crystalline bovine serum albumin (BSA) (globulin-free), bovine insulin, and cholesterol from Sigma; human iron-saturated transferrin from Boehringer-Mannheim (Indianapolis, IN); Dulbecco's minimal essential medium (DMEM) from Whittacker (Walkersville, MD). Serum-free medium (SFM) consisted of DMEM containing BSA 15 mg/mL, insulin 1 p,g/mL, transferrin 7.7 x mol/L, cholesterol 7.8 & n L . Highly purified collagenase type VI1 from Clostridium histolyticum was obtained from Sigma. The synthetic peptides GRGESP and GRGDTP were from Telios. "Chromium (1 mCi/mL, 200 Ci/g) and tritiated thymidine (1 mCi/mL, 2 Ci/mmol) were purchased from New England Nuclear (Boston, MA). Source of cells. The GM-CSF- and IL-34ependent cell line, M07, was obtained from Dr Steven Clark, and was originally derived by Avanzi et all7 from the peripheral blood of an infant with acute megakaryocytic leukemia. This line was maintained in DMEM supplemented with 20% FCS (20% DMEM) and 10 ng/mL of both GM-CSF and IL-3. Bone marrow progenitor cells were obtained from healthy donors after informed consent by posterior iliac crest aspiration into heparinized syringes. Mononuclear cells were recovered by Ficoll density centrifugation, and macrophages were removed by plastic adherence for 1 hour at 37°C as previously described." Neutrophils and monocytes were simultaneously prepared from heparinized peripheral blood donated by healthy volunteers. After Ficoll density centrifugation, neutrophils were isolated from the RBC pellets by dextran sedimentation. Monocytes were obtained from the mononuclear cell fraction by plastic adherence for 1 hour at 37T, as previously described.Ix Both neutrophil and monocyte preparations were greater than 90% pure as assessed by Wright-Giemsa staining. Immunophenotyping. M 0 7 cells were screened for the expression of known collagen adhesion receptors and for the myeloid marker CD33 by indirect immunofluorescent staining. Briefly, 1 x lo6cells were stained for 30 minutes, 4°C with 100 FL of either an irrelevant control antibody (3CllC8, anti-y-interferon antibody), or with the previously described antibodies that recognize CD29, VLA-1, VLA-2, VLA-3, VLA-4, VLA-5, VLA-6, CD44, or 1F7. After washing two times in phosphate-buffered saline (PBS), the cells were labeled with fluorescein-conjugated goat antimouse Ig (FITC) (Tago, Burlingame, CA) for 30 minutes, 4°C. After two additional washes, the cells were analyzed on a Coulter Epics C flow cytometer (Coulter, Hialeah, FL). SIChromiumassay for cell adhesion. The binding of M 0 7 cells, neutrophils, and monocytes to ECM proteins was quantitated by assessing "chromium release of adherent cells. Cells, lo6, were labeled with 100 KCi of "chromium (200 Ci/g) for 1 hour at 37T, and then washed two times in PBS and resuspended at 0.5 to 1 x 106/mL of SFM. Flat-bottom 96-well microtiter wells (Falcon, Oxnard, CA) were coated with 10 to 20 p,L of individual ECM proteins (20 to 70 p,g/well, 0.28 cm2/well)and allowed to air dry for 1 to 3 hours at room temperature. Control coating was performed with either the respective solvents (0.1N acetic acid for collagen preparations, Tris/NaCI for laminin, H,O for fibronectin) or with 1.5% BSA. BSA was used as a control to ensure that cells were not adhering to protein in a nonspecific fashion in these experiments. None of the cell types used in this study was observed to bind to BSA. "Chromium-labeled cells (50 to 100 x lo3) were added to each well in a total of 100 p,L of SFM, and binding was allowed to occur for 2 to 4 hours at 37°C. The nonadherent cells were then removed by three washes with PBS, followed by lysis of bound cells with 0.1% NP40. The radioactivity of each lysate was measured in a gamma counter. The percentage of cells adhering to an individual ECM protein (percent specific binding) was calculated as follows: percent specific binding = 100 x (mean cpm [ECM-coated surface] - mean cpm [control surface])/CPM (total). For some experiments, ''chromium-labeled cells were pretreated with anti-CD29 antibody (1:200 dilution) or control antibody (anti-CD33, which reacts with M 0 7 cells) for 30 minutes at 4°C before performing the bind, with continued presence of antibody during the duration of the bind. Likewise, the effects of RGDcontaining peptides was determined by preincubation of cells in 200 p,g/mL of either GRGESP or GRGDTP for 30 minutes at room temperature, followed by binding in the continued presence of peptide. The effects of divalent cation chelation were assessed by performing the bind in EDTA (10 mmol/L final concentration per well) in some studies. Finally, collagen-coated wells were pretreated with collagenase in some experiments to determine the From www.bloodjournal.org by guest on February 6, 2015. For personal use only. PROGENl'iOR CELL BINDING TO COLLAGEN TYPE I specificityof binding to collagen. For these studies, collagen-coated or control wells were pretreated with 20 pL of either collagenase buffer (50 nlthol/L Tris, 2.5 mmol/L CaCI,, pH 7.5) or collagenase (0.5 U/mL) at room temperature and allowed to air dry before adding 5'chfomium-labeled cells. Assay for pkogenitor cell adhesion. Nonadherent bone marrow mononuclear cells from healthy donors were added to 96-well plates coated with either ECM protein, control solvent, or with 1.5% BSA as described. To ensure that a reasonable number of colonies Would be obtained per well after binding, cell numbers were added in a range of 10 to 100 x 10' per well. Progenitor cells were allolell to bind for 4 hours at 3 7 T , followed by removal of nonadherdnt cells by washing three times in PBS. For determination of CPb-GM binding, each well was overlayed with 0.3% agar in Iscove'S modified Dulbecco's MEM (IMDMEM) containing 10% (vol/vol) 5637 conditioned medium as a source of CSFs. Myeloid progenitor cells were scored using an inverted microscope. Clusters (8 to 40 cells) were counted on day 7 and colonies ( > 4 0 cells) were counted on day 14. For determination of CFU-mix and BFU-E binding, each well was overlayed with 0.9% methylcellulose in IMDMEM containing 4 U/mL erythropoietin, and 5 ng/mL of both GM-CSF and IL-3. CFU-mix and BFU-E were enumerated on day 14. The total number of CFUs added per well was determined under identical growth conditions in collagen- or control-coated plastic wells. It should be noted that there was no difference in the growth of CFU-GM in the presence or absence of collagen in any of the experiments performed in this study. The percentage of CFUs adherent to ECM (percent specific binding) was calculated as follows: percent specific binding = 100 x (mean CFU [ECM-coated surface] - mean CFU [control surface])/total CFU. To establish consistency between experiments, all data were corrected to reflect cluster or colony number per 10s cells added. For some experiments, the effects of control antibody (anti-CD33), anti-CD29, EDTA, and collagenase on progenitor cell binding to collagen type I were assessed under the same incubation conditions as described for 5'chromium-labeled cells. Specifically, bone marrow mononuclear cells were first pretreated with either control or anti-CD29 antibody, with continuous exposure to antibody during the binding period. Cell proliferation assay. The effect of ECM proteins on the proliferation of M 0 7 cells was examined in 96-well plates coated with either ECM protein or control solvent. M 0 7 cells, 20 x 10' per well, were incubated for 60 hours at 37°C in the presence or absence of 5 to 25 ng/mL of GM-CSF in either 20% FCS or in SFM. Tritiated thymidine (1.6 $3, 2 Ci/mmol) was added to each well for the last 12 hours of incubation, followed by cell harvesting and determination of radioactivity with a beta counter (Packard Liquid Scintillation Analyzer 2000 CA). Assessment of collagenase activity. To determine the specificity of collagenase VI1 for collagen type I, 7 pL of either laminin, fibronectin, or collagen (approximately 20 pg of each protein) were treated with 43 pL of either control buffer (50 mmol/L Tris, 2.5 mmol/L CaCI,, pH 7.5) or with collagenase type VI1 (approximately 430 m u ) in a total volume of 50 pL at room temperature for 1 hour. In some experiments, 7 pL of collagen was treated with 43 pL of neutrophil supernatant (86% vol/vol) under the same conditions to test for the possibility of endogenous collagenase production by neutrophils. After addition of 50 pL of 2X sample buffer with mercaptoethanol, the samples were boiled at 100°C for 5 minutes and loaded onto a 7.5% sodium dodecyl sulfate (SDS) polyacrylamide gel. After electrophoresis, the protein bands were visualized by Coomassie blue staining. Statistical analysis. Significance levels for comparison between treatment groups were determined using the two-sided Student's ttest for paired samples. 659 RESULTS Adhesion receptor expression andpattem of ECM binding of M 0 7 cells. Initial binding experiments were performed using the factor-dependent myeloid leukemic cell line, M07. Immunophenotyping analysis was initially performed to determine whether these cells expressed receptors for collagen (VLA-1, -2, and -3, CD44, and CD26), fibronectin (VLA -3, and -4), and laminin (VLA-1, -2, and -6).19 The percentage of M 0 7 cells specifically positive for each adhesion protein was: VLA-1 = 0%, VLA-2 = 41%, VLA-3 = 0%, VLA-4 = 48%, VLA-5 = 94%, VLAd = 64%, CD29 (VLA-p1-chain) = 95%, CD44 = 89%, and CD26 = 0%. The cells also expressed the CD33 molecule (90%). These data suggest that M 0 7 cells express adhesion proteins for collagen, fibronectin, and laminin. Therefore, 5'chromium-labeled M 0 7 myeloid cells were allowed to bind to microtiter wells previously coated with 20 to 70 kg of either collagen types I, 111, IV, and V, fibronectin, or laminin for 4 hours at 37"C, with subsequent washing and measurement of specifically bound cells as previously described. As shown in Table l, M 0 7 cells demonstrated significant binding to bovine collagen type I (56% +- 5%), with a significantly lesser amount of binding to human fibronectin (18% c 4 % ) and to murine laminin (19% 2 5%). There was no appreciable binding of M 0 7 cells to collagen type 111, IV, or V. Increasing the absolute amounts of any coated ECM protein did not increase binding further. The kinetics of binding of M 0 7 cells to collagen type I showed peak binding at 2 hours of incubation. Adhesion of normal bone marrow progenitor cells to collagen type I. In view of the significant degree of M 0 7 binding to collagen type I, the remainder of our studies were designed to assess the relevance of this observation for normal bone marrow progenitor cells. Adherence-depleted bone marrow mononuclear cells were allowed to bind to collagen type I-coated microtiter wells for 4 hours at 37"C, followed by washing and overlaying the bound cells with either 0.3% agar or 0.9% methycellulose under conditions Table 1. Adhesion of the Myeloid Leukemic Cell Line M 0 7 to ECM Proteins Range Specific Binding (%)t ECM Protein* Collagen type I Collagen type 111 Collagen type IV Collagen type V Laminin Fibronectin ~ ~ (%) 56 f 5 48-63 2 2 2 0 0 19 f 5 0-2 ~ 5 3 3 3 5 5 - 14-28 14-21 18 2 4 ~ No. of Experiments* ~ ~~ ~ ~ *Microtiter wells were coated with either control solvent or extracellular matrix proteins as described in text before performing bind with 50 x lo35'chromium-labeled M07 cells for 4 hours at 37°C. tPercent specific binding of cells adhering to each ECM protein was calculated for each experiment using mean values from quadruplicate wells as described in text. Background binding was 3% ? 2% for all experiments. The value shown is mean IT SD percent specific binding from the indicated number of experiments. *Indicates number of separate experiments performed for each ECM protein. From www.bloodjournal.org by guest on February 6, 2015. For personal use only. 660 KOENIGSMANN ET AL that would support maximum colony growth of CFU-GM, CFU-GEMM, and BFU-E as described. Bone marrow progenitors were depleted of accessory cells to reduce the potential for simultaneous accessory cell binding that might alter the pattern of colony formation due to the secretion of endogenous growth factors. As shown in Table 2, significant binding of day 7 CFU-GM (46% f 8%, n = 6), day 14 CFU-GM (47% f 12%, n = 4), and BFU-E (40% f lo%, n = 5) to collagen type I was observed (P < .001). Interestingly, there were no quantitative differences between the binding of early (ie, day 14 CFU-GM or CFU-GEMM) versus later (day 7 CFU-GM) progenitor cells to collagen type 1.Although CFU-mix tended to bind to collagen type I, this effect was not statistically significant, possibly due to the small numbers of colonies observed. SpeciJcity of myeloid cell binding to collagen I. To confirm that the observed binding of M 0 7 cells or normal bone marrow progenitors was mediated by collagen type I, as opposed to a contaminating protein present in the collagen preparation, we studied the effects of pretreatment of collagen-coated microtiter wells with highly purified collagenase type VII. As shown in Fig 1, collagenase pretreatment significantly reduced the binding of both M 0 7 cells and CFU-GM to collagen type I, whereas similar pretreatment with collagenase buffer had no effect. To determine whether the collagenase effect was specific for collagen, we treated fibronectin, laminin, and collagen type I with collagenase for 1 hour at room temperature, with subsequent visualization of the protein products by polyacrylamide gel electrophoresis (PAGE) followed by Coomassie blue staining. As show in Fig 2, collagenase had no effect on the integrity of laminin or fibronectin, whereas it completely degraded the three major bands associated with collagen type I(115,125, and 212 Kd). Effects of anti-CD29 antibody, RGD-containing peptide, or divalent cation chelation on the binding of myeloid cells to collagen type I. The 6-1 integrin family of adhesion proteins is comprised of heterodimers containing a common Table 2. Adhesion of Normal Myeloid Progenitor Cells to Collagen Type I Donor* Treatmentt CFU-GM D7 1 Control Collagen Total CFU added % Specific binding Control Collagen Total CFU added % Specific binding Cont roI Collagen Total CFU added % Specific binding Control Co IIage n Total CFU added YOSpecific binding Cont ro I Collagen Total CFU added % Specific binding Control Collagen Total CFU added O h Specific binding Control Collagen Total CFU added O h Specific binding 7* 7I 57 6 158 + 32 32 4 2 1 22 -c 6 31 58 1 2 1 8+2 12 67 020 020 4+2 9 2 4 44 1 2 0 2+1 50 020 020 OtO o+o 49 + 10 109 45 422 25 + 4 44 + 6 48 9+3 22 2 1 41 1 2 0 7+2 1426 43 7+3 25 4 28 + 2 f 1 20 10 o+o o+o 9 r 4 22 + a 41 221 422 50 2 3 7 Mean % specific binding11 + CFU-GM D14 ND§ BFU-E Or0 5+2 16 + 4 31 CFU-mix ND 020 22 f 5 44 50 ND ND ND 222 74 + 6 167 + 19 43 46 + 8 17 + 4 46 2 a 37 47 + 12 ND ND 020 o+o 4+2 7+4 57 1+0 3+ 1 33 ND ND o+o 40 2 10 3 4 + 17 "Bone marrow progenitor cells from seven different normal donors were depleted of monocytes by plastic adherence before performing binding assay. tCells (10-100 x 10') were added t o flat bottom 96-well plates precoated with either 0.1% acetic acid (control) or collagen type I (60 pg). After 4 hours at 37"C, the wells were washed to remove nonadherent cells, followed by addition of either agar or methylcellulose as described in text. Appropriate controls were performed in order to assess the total number of CFU-GM and BFU-E added to each well. *Data expressed as mean + SD of colony number from quadruplicate wells. To establish consistency between experiments, all data are expressed as cluster (day 7) or colony (day 14) number per 1O'totaI cells added. OND, not determined. IlCumulative mean + SD of percent specific binding from individual experiments. For each experiment shown, highly significant binding (P < .001, Student's t-test), of CFU-GM and BFU-E to collagen type Iwas observed. Although CFU-mix tended t o bind to collagen-coated wells, this binding was not statistically significant, possibly due t o the small number of colonies observed. From www.bloodjournal.org by guest on February 6, 2015. For personal use only. PROGENITOR CELL BINDING TO COLLAGEN TYPE I 70 66 1 BUFFER COLLAGENASE z E 50 0 u. w L 0 + 0 U w n 40 30 20 10 0 M07 CFU-GM Fig 1. Effects of collagenase on binding of M 0 7 cells or normal bone marrow CFU-GM t o collagen type 1. Control or collagen-coated wells were incubated for 1 hour at room temperature with 20 pL of either buffer (50 mmol/L Tris, 2.5 mmol/L CaCI,, pH 7.5) or with collagenase type VI1 (0.5 U/mL) before adding either 6’chromiumlabeled M 0 7 cells or adherence-depletednormal bone marrow progenitor cells for determination of specific binding as described in text. Data are expressed as mean 2 SD of percent specific binding from two separate experiments for M07 cells and for day 7 CFU-GM. B-1 chain (CD29) and at least six different a subunits. These six distinct heterodimers are referred to as VLA-1 to VLA-6, and they are known to bind to a variety of ECM proteins.IYVLA proteins -1, -2, and -3 have been determined to bind to collagen in a calcium-dependent fashion that may be partially blocked by peptides containing the RGD Because immunophenotypicanalysis of the M07 cell line showed expression of VU-2, we were interested in determining whether collagen binding of this cell line was mediated through this adhesion protein. Therefore, we studied the effects of a neutralizing antiCD29 antibody (4B4), RGD-containing peptide, or divalent cation chelation with EDTA, on the ability of M07 cells or normal bone marrow CFU-GM to bind to collagen Fig 2. Specificity of collagenase for collagen type 1. Twenty micrograms of either laminin (lanes 1 and 4). fibronectin (lanes 2 and 5). or collagen type I(lanes 3 and 6) was incubated with either buffer (lanes 1 through 3) or 20 mU of collagenase type VI1 (lanes 4 through 6) for 1 hour at room temperature. After boiling in sample buffer under reducing conditions, the proteins were resolved by 7.5% SDS-PAGE, followed by visualization by Coomassie blue staining. Three bands representing collagenase species are indicated in lanes 4 through 6. Note that the 115-Kd, 125-Kd, and 212-Kd bands of collagen type I (lane 3) are selectively degraded by collagenase type I, whereas this enzyme has not degraded either laminin or fibronectin. type I. The 4B4 antibody has been previously shown to block VLA-4lVCAM-1 interactions,=to neutralize collageninduced proliferation of T cells? and to neutralize binding of the ovarian cancer cell line OVCAR-3 to both laminin and fibronectin (S.A.C., unpublished observations, June 1991). As shown in Table 3, neither antibody 4B4 nor RGD-containing peptide altered adhesion to collagen type I. Also, divalent cation chelation caused no significant change in collagen binding of M07 cells or of CFU-GM. These results suggest that binding of M07 cells or of CFU-GM to collagen type I occurs through a VLAindependent mechanism. Because CD44 is also expressed by M07 cells and is known to mediate collagen binding,I4.”we next tested the effects of antLCD44 antibody (515) on the adherence of M07 cells to collagen type I. However, no inhibitory effect of anti-CD44 on M07 binding was observed (data not shown). Because the 515 antibody used in these studies is not known to be neutralizing, M07 cells were continuously exposed to 515 antibody for 72 hours at 37°C in an attempt to study the effects of CD44 downregulation on subsequent binding. However, CD44 expression was not downregulated despite a 72-hour exposure to the 515 antibody (data not shown). Comparative binding of normal neutrophils, monocytes, and M 0 7 cells to collagen ype I. These data suggest the possibility that binding to collagen I may represent one of the mechanisms by which committed myeloid cells remain within the bone marrow microenvironment during development. In an attempt to determine whether mature myeloid cells also bind to collagen, we investigated the ability of S’chromium-labeledneutrophils, monocytes, and M07 cells to bind to collagen type I, with cumulative results shown in Fig 3. These experiments were performed over a 2-hour incubation (as opposed to 4 hours) at 37°C to maintain neutrophil viability at greater than 90%. In the absence of 116- COLLAGENASE ,$ 77- 1 2 3 4 5 6 From www.bloodjournal.org by guest on February 6, 2015. For personal use only. KOENIGSMANN ET AL 662 Table 3. Effects of Anti-CD29 Antibody, RGD Peptide, or EDTA on Binding of M 0 7 Cells of CFU-GM to Collagen Type I Cell Type CFU-GM Treatment M07 (day 7) Antibody or RGD peptide:* Controlt Anti-CD29 loo%§ (n = 3) 118% (n = 3) 100% (n = 1) 114% (n = 3) ND 100% (n = 5) 100% (n = 3) 97% (n = 6) RGD Divalent cation chelation:* Control EDTA 79%11 (n = 9) 96% (n = 1) Abbreviation: ND, not done. *Binding was performed in quadruplicate wells in the continuous presence of either anti-CD29, which is a neutralizing antibody recognizing the p-I integrin molecule, or RGD peptide (GRGDTP), with details as described in Materials and Methods. Cells were pretreated with either antibody or peptide prior to binding as previously described. tFor experiments using the anti-CD29 antibody, the control antibody was anti-CD33, which recognizesa surfaceprotein with no known adhesion properties. For experiments using RGD peptide, the control peptide was GRGESP. Neither anti-CD33 nor GRGESP peptide altered binding when compared to treatment with media alone. Sln a separate set of experiments, binding was performed in quadruplicate wells under serum-free conditions with either 20% vol/vol PBS (control) or 20% vol/vol EDTA in PBS (for a final concentration of 10 mmol/L EDTA in SFM). §Data for each treatment group are expressed as percent of control specific binding (SB)as determined from the indicated number of experimentsasfollows: % of control SB = 100 x (mean SB [treatment])/ (mean SB [control]). l/Not significantly different when compared with control (P = .06). EDTA, background binding of monocytes to control wells was significant (20% to 50% adhesion), precluding an accurate assessment of specific binding to collagen type I under these conditions. Because pilot experiments showed that the binding of monocytes to plastic was significantly blocked by 10 mmol/L EDTAwithout affecting corresponding binding to collagen I, we performcd binding experiments using neutrophils, monocytes, and M 0 7 cells in the presence of 10 mmol/L EDTA to achieve acceptable levels of background binding (5% to 10%). As shown in Fig 3, the binding of both neutrophils and monocytes to collagen type I was significantly less than that of M 0 7 cells (25% ? 8% and 29% 2 6% v 40% 7%, P = .001). In addition, comparison of percent specific binding to collagen type I obtained with neutrophils, monocytes, and CFU-GM (Table 2) showed significantly lowcr levels for either neutrophils or monocytes when compared with either day 7 (46% ? 8%) or day 14 CFU-GM (47% 12%) ( P < ,001). Although CFU-GM binding was typically performed Over a 4-hour period, as opposed to 2 hours for neutrophils and monocytes, we have performed additional experiments which show that peak CFU-GM binding is achieved after a minimum Of 1 hour Of inCubation at 37"c (data not shown). Thus, it is unlikely that the lower binding of neutrophils or monocytes compared with that of CFU-GM is due to differences in binding duration. During terminal differentiation, myeloid cells acquire the ability to produce co~~agenase.24.2S Therefore, we considered the possibility that the obse,.,ed decrease in neutrophil and monocyte adhesion to collagcn might result from endogenous collagenase secretcd by these cells during the incubation period. To evaluate this possibility, media were conditioned by either neutrophils, monocytes, or M 0 7 cells for 2 hours at 37"C, (5 x 10' cells/mL SFM). Ccll-free supernatant was collected and used to treat 20 pg of collagen type I in a total volume of 50 pL (86% vol/vol supernatant) for 1 hour at room temperature, followed by analysis by SDSPAGE as described. NO collagen degradation was observed in any treatment group (data not shown). Effects Of collagen lype I on Progenitor cell Proliferation. To examine whethcr progenitor cells derive a proliferative advantage during binding to collagen typc I, we evaluated thymidine incorporation of M 0 7 cells (n = lo), as well as colony growth of bone marrow progenitors (n = 9), in thc presence or absence of collagen. Experiments were conducted in the presence or absence of GM-CSF or IL-3 over a dose range of 5 to 25 ng/mL. No collagen-induced enhancement of proliferation was observed (data not shown). * * DISCUSSION Fig 3. Binding of M 0 7 cells, neutrophils, and mohocytes to collagen type I. 5'Chromium-labeled cells were bound to collagen type I-coated plates for 2 hours at 37°C and processed as described in text for assessment of percent specific binding, Binding was performed in the presence of IO mmol/L EDTAfor all cell types as described in text to reduce nonspecific binding of neutrophils and monocytes to plastic. Data are expressed as mean 2 SD of specific binding of each cell type from the indicated number of experiments. A statistically significant decrease in the binding of both neutrophils and monocytes to collagen type I when compared with that of M 0 7 cellS was observed (P < ,001. Student's t-test). This study was initially undertaken in an attempt to investigate the ability of several ECM proteins to support the adherence of the M 0 7 myeloid leukemia cell line. This line was chosen for these experiments in view of its hematopoietic origin and its expression of several potcntial adhesion proteins, inc1uding vLA-2, vLA-4, VLA-6, CD29, and CD44. We observed that collagen type I mediated significant binding of M 0 7 cells, whereas these cells bound to a considerably lesser degree to fibronectin and laminin, In view of the high level of M 0 7 binding to collagen type I, we further investigated thc role that this ECM protcin might play in thc binding of normal bonc marrow cells. From www.bloodjournal.org by guest on February 6, 2015. For personal use only. PROGENITOR CELL BINDING TO COLLAGEN TYPE I Both normal CFU-GM and BFU-E were found to significantly bind to collagen type I, and this interaction was completely abolished by pretreatment of collagen-coated plates with collagenase. In contrast to the results of other investigators, who report proliferative effects of collagen type I on T lymphocytes? we found no evidence for a mitogenic effect of collagen type I on myeloid cells in the presence or absence of exogenous GM-CSF or IL-3. This observation makes it unlikely that our results are due to a selective growth advantage of cells exposed to collagencoated wells. We also observed that mature neutrophils and monocytes bind to collagen type I (Fig 3). Interestingly, this binding was significantly less when compared with that of M 0 7 cells (Fig 3), suggesting the possibility that adhesion to collagen may decrease with myeloid maturation. It is important to note that although M 0 7 cells have a blast morphology and represent a less differentiated phenotype when compared with neutrophils or monocytes, the M 0 7 cell line is leukemic, as well as megakaryocytic,in origin and may not accurately reflect the binding of normal bone marrow progenitors. However, the binding of neutrophils and monocytes to collagen type I was also observed to be significantly lower when compared with that of normal CFU-GM (Table 2). It must be pointed out that these data are not strictly comparable due to technical differences between the measurement of mature cell binding (”chromium-labeling) and the measurement of CFU-GM binding (colony assay). Unfortunately, in view of the low number of CFU-GM present in normal bone marrow, it is difficult to obtain highly purified progenitor cell populations for use in 51chromium-labelingstudies. Collagen binds to a heterogenous group of cell surface receptors. These include the p-1 integrin family of heterodimers (VLA-1, -2, and -3) (24), the CD44 molecule, also known as the class I11 collagen r e ~ e p t o r , ~and ~ . ’ ~a 110-Kd protein known as dipeptidyl peptidase IV (CD26).23 Although VLA-1, VLA-3, and CD26 were not expressed by the M 0 7 cell line, both VLA-2 and CD44 were strongly expressed. The interaction of collagen with p-1 integrins is known to be inhibited by RGD-containing by divalent cation chelation,27and by neutralizing antibody against the common p-1 chain.” However, as shown in Table 3, these interventions did not alter the binding of M 0 7 cells or of CFU-GM to collagen type I. The concentration of RGD peptide used in this study was based on previous work which demonstrated that this dose is capable of blocking collagen-induced T-cell proliferation as well as HeLa cell attachment to a collagen-based gelatin matrix.23328 However, higher concentrations of RGD peptide have been required for maximal inhibition of binding in other cell systems.” Nevertheless, our data suggest that the binding of myeloid cells to collagen type I is not mediated by the p-1 integrins, despite the expression of VLA-2 by M 0 7 cells. Although VLA expression is sometimes necessary for the binding of cells to ECM proteins such as collagen, it is clear that such expression is not sufficient for binding to occur. For instance, it has been recently shown that activated B 663 cells bind to germinal center follicles through an interaction between B-cell-expressed VLA-4 and the VCAM-1 molecule expressed within the germinal center.22 However, B-cell lines which express VLA-4 do not necessarily bind to germinal centers, suggesting that VLA-4 must be activated (through a conformational change or through association with another surface protein) to recognize the VCAM-1 molecule. A similar requirement for activation has been recently shown for the binding of LFA-1 to ICAM-1F and for the binding of LAM-1 to mannose residues3’ Therefore, VLA expression may be necessary, but not sufficient, for binding in some situations. The fact that the M 0 7 cell line expresses VLA-2 but does not bind to collagen through this molecule is consistent with this hypothesis. Our studies do not exclude the possibility that CD44 is responsible for mediating the binding of M 0 7 cells or committed progenitor cells to collagen type I. CD44 expression was noted on greater than 90% of M 0 7 cells in this report, and it has also been observed in highly purified populations of normal human bone marrow progenitor cells.1331 In addition, CD44 expression has been shown to diminish as myeloid cells differentiate toward mature neutrophil~.’~ Because it is not known whether the anti-CD44 antibody used in this study is able to neutralize collagen binding, and because the CD44 molecule could not be downregulated from the surface of M 0 7 cells, the role of CD44 in mediating the binding of progenitor cells to collagen type I remains unclear. It is likely that the binding of hematopoietic progenitor cells to ECM proteins involves the coordinate interaction of several types of adhesion proteins. Thus, uncommitted, HLA-DR-negative progenitors bind to f i b r ~ n e c t i n , ~ . ~ whereas committed erythroid progenitors bind to both fibronectinS7and collagen type I, and committed myeloid progenitors bind to both hemonectin’ and collagen type I. The presence of alternative mechanisms of erythroid progenitor cell binding that do not involve fibronectin was also suggested by Coulombel et a17 who demonstrated that BFU-E adherence to stromal cell-derived ECM could only be partially blocked by antifibronectin antibody. Based on our studies, it is possible that collagen type I may have partly contributed to the fibronectin-independent binding of BFU-E observed by these investigators. Although not specifically addressed in this study, the role of other collagens such as the type 111 and type IV species in the binding of normal progenitor cells deserves further investigation. Our data suggest the possibility that collagen type I may partly mediate the adhesion of committed myeloid and erythroid progenitor cells within the bone marrow microenvironment. In addition, mature myeloid cells such as neutrophils and monocytes retain the capacity to bind to collagen type I, with a suggestion that this binding may be decreased compared with that of CFU-GM. Under certain conditions, higher levels of bone marrow progenitor cells circulate in the peripheral blood, such as during rebound myelopoiesis after ~hemotherapy,~’ during hematopoietic growth factor administration? or during pathologic condi- From www.bloodjournal.org by guest on February 6, 2015. For personal use only. KOENIGSMANN ET AL 664 tions such as the stem cell expansion characteristic of chronic myeloid leukemia?' The ability of hematopoietic growth factors such as GM-CSF or G-CSF to mobilize bone marrow progenitors into the circulating white blood cell pool is particularly noteworthy, because these agents are also known to alter the expression of several adhesion proteins on the surface of myeloid cells?6 A comparison of the binding of circulating versus bone marrow progenitor cells to collagen type I may permit a better understanding of the physiologic role of this ECM protein in progenitor cell adhesion. ACKNOWLEDGMENT We thank Dr Martin Hemler for his helpful advice during the study. -- REFERENCES 1. Coulombel L, Eaves AC, Eaves CJ: Enzymatic treatment of long-term human marrow cultures reveals the preferential location of primitive progenitors in the adherent layer. Blood 62:291,1983 2. Verfaille C, Blakolmer K, McGlave P: Purified primitive human hematopoietic progenitor cells with long-term in vitro repopulating capacity adhere selectively to irradiated bone marrow stroma. J Exp Med 172:509,1990 3. Verfaille C, McCarthy J, McGlave P Differentiation of primitive human Lin-34+DR- hematopoietic progenitors is accompanied by transition of adhesion from the heparin-binding domain to the cell-binding domain of fibronectin. Blood 76:125a, 1990 (abstr) 4. Williams DA, Stephen C, Rios M, Patel V: Interactions of primitive hematopoietic stem cells with the hematopoietic microenvironment: role of fibronectin and V U - 4 integrin. Blood 76:126a, 1990 (abstr) 5. Tsai S, Patel V, Beaumont E, Lodish HF, Nathan DG, Sieff CA. Differential binding of erythroid and myeloid progenitors to fibroblasts and fibronectin. Blood 69:1587,1987 6. Patel VP, Ciechanover A, Platt 0, Lodish HF: Mammalian reticulocytes lose adhesion to fibronectin during maturation to erythrocytes. Proc Natl Acad Sci USA 82440,1985 7. Vuillet-Gaugler MH, Breton-Gorius J, Vainchenker W, Guichard J, Leroy C, Tchernia G, Coulombel L Loss of attachment to fibronectin with terminal human erythroid differentiation. Blood 76:865,1990 8. Campbell AD, Long MW, Wicha MS: Developmental regulation of granulocytic cell binding to hemonectin. Blood 76: 1758, 1990 9. Zuckerman KS, Wicha MS: Extracellular matrix production by the adherent cells of long-term murin bone marrow cultures. Blood 61540, 1983 10. Waterhouse EJ, Quesenberry PJ, Balian G: Collagen synthesis by murine bone marrow cell culture. J Cell Physiol127:397,1986 11. Liesveld JL, Abboud CN, Duerst RE, Ryan DH, Brennan JK, Lichtman MA: Characterization of human marrow stromal cells: Role in progenitor cell binding and granulopoiesis. Blood 73:1794,1989 12. Paul SR, Yang RE, Donahue RE, Goldring S, Williams D A Stromal cell-associated hematopoiesis: Immortalization and characterization of a primate bone marrow-derived stromal cell line. Blood 77:1723,1991 13. Kansas GS, Muihead MJ, Dailey MO: Expression of the CDllKD18, leukocyte adhesion molecule 1, and CD44 adhesion molecules during normal myeloid and erythroid differentiation in humans. Blood 76:2483,1990 14. Carter WG, Wayner EA: Characterization of the class 111 collagen receptor, a phosphorylated, transmembrane glycoprotein expressed in nucleated human cells. J Biol Chem 263:4193,1988 15. Brown TA, Bouchard T, St-John T, Wayner E, Carter WG: Human keratinocytes express a new CD44 core protein (CD44E) as a heparan-sulfate intrinsic membrane proteoglycan with additional exons. J Cell Biol113:207, 1991 16. Zuckerman KS, Rhodes RK, Goodrum DD, Patel VR, Sparks B, Wells J, Wicha MS, Mayo LA. Inhibition of collagen deposition in the extracellular matrix prevents the establishment of a stroma supportive of hematopoiesis in long-term murine bone marrow cultures. J Clin Invest 75:970,1985 17. Avanzi GC, Lista P, Giovinazzo B, Miniero R, Saglio G, Benetton G, Coda R, Catorretti G, Pegoraro L Selective growth response to IL-3 of a human leukemic cell line with megakaryoblastic features. Br J Haematol69:359,1988 18. Cannistra SA, Groshek P, Griffin JD: Monocytes enhance gamma-interferon-induced inhibition of myeloid progenitor cell growth through secretion of tumor necrosis factor. Exp Hematol 16:865,1988 19. Hemler ME: VLA proteins in the integrin family: Structures, functions, and their role on leukocytes. Annu Rev Immunol 8:365,1990 20. Ruoslahti E, Pierschbacher MD: New perspectives in cell adhesion: RDG and integrins. Science 238:491, 1987 21. Dedhar S, Ruoslahti E, Pierschbacher MD: A cell surface receptor complex for collagen type I recognizes the Arg-Gly-Asp sequence. J Cell Biol 104:585,1987 22. Freedman AS, Munro JM, Rice GE, Bevilacqua MP, Morimoto C, McIntyre BW, Rhynhart K, Pober JS, Nadler LM: Adhesion of human B cells to germinal centers in vitro involves VLA-4 and INCAM-1 10. Science 349:1030,1990 23. Dang NH, Torimoto Y, Schlossman SF, Morimoto C Human CD4 helper T cell activation: Functional involvement of two distinct collagen receptors, 1F7 and VLA integrin family. J Exp Med 172:649,1990 24. Hasty KA, Hibbs MS, Kang AH, Mainardi C L Secreted forms of human neutrophil collagenase. J Biol Chem 261:5645, 1986 25. Campbell EJ, Cury JD, Lazarus CJ, Welgus HG: Monocyte procollagenase and tissue inhibitor of metalloproteinases. Identification, characterization, and regulation of secretion. J Biol Chem 262:15862,1987 26. Gehlsen KR, Argraves WS, Pierschbacher MD, Ruoslahti E: Inhibition of in vitro tumor cell invasion by Arg-Gly-Aspcontaining synthetic peptides. J Cell Biol106:925,1988 27. Springer T A Adhesion receptors of the immune system. Nature 346:425,1990 28. Beacham DA, Jacobson BS: Mg2' mediates the cellsubstratum interaction of Arg-Gly-Asp-dependent HeLa cell collagen receptors. Exp Cell Res 189:69,1990 29. Hibbs ML, Xu H, Stacker SA, Springer T A Regulation of adhesion to ICAM-1 by the cytoplasmic domain of LFA-1 integrin subunit. Science 251:1611, 1991 30. Spertini 0, Kansas GS, Munro JM, Griffin JD, Tedder T F Regulation of leukocyte migration by activation of the leukocyte adhesion molecule-1 (LAM-1) selectin. Nature 349:691,1991 31. Lewinsohn DM, Nagler A, Ginzton N, Greenberg P, Butcher EC: Hematopoietic progenitor cell expression of the H-CAM (CD44) homing-associated adhesion molecule. Blood 75589, 1990 From www.bloodjournal.org by guest on February 6, 2015. For personal use only. PROGENITOR CELL BINDING TO COLLAGEN TYPE I 32. Coulombel L, Vuillet MH, Leroy C, Tchernia G: Lineageand stage-specific adhesion of human hematopoietic progenitor cells to extracellular matrices from marrow fibroblasts. Blood 71:329, 1988 33. Richman CM, Weiner RS, Yankee RA: Increase in circulating stem cells following chemotherapy in man. Blood 47:1031, 1976 34. Socinski MA, Cannistra SA, Elias A, Antman KH, Schnipper L, Griffin JD: Granulocyte-macrophage colony stimulating 665 factor expands the circulating haemopoietic progenitor cell compartment in man. Lancet 1:1194,1988 35. Cannistra S A Chronic myelogenous leukemia as a model for the genetic basis of cancer. Hematol Oncol Clin North Am 4:337, 1990 36. Demetri GD, Spertini 0,Pratt ES, Kim E, Elias A, Antman K, Tedder TF, Griffin JD: GM-CSF and G-CSF have different effects on expression of the neutrophil adhesion receptors LAM-1 and CDllb. Blood 76:178a, 1990 (abstr) From www.bloodjournal.org by guest on February 6, 2015. For personal use only. 1992 79: 657-665 Myeloid and erythroid progenitor cells from normal bone marrow adhere to collagen type I M Koenigsmann, JD Griffin, J DiCarlo and SA Cannistra Updated information and services can be found at: http://www.bloodjournal.org/content/79/3/657.full.html Articles on similar topics can be found in the following Blood collections Information about reproducing this article in parts or in its entirety may be found online at: http://www.bloodjournal.org/site/misc/rights.xhtml#repub_requests Information about ordering reprints may be found online at: http://www.bloodjournal.org/site/misc/rights.xhtml#reprints Information about subscriptions and ASH membership may be found online at: http://www.bloodjournal.org/site/subscriptions/index.xhtml Blood (print ISSN 0006-4971, online ISSN 1528-0020), is published weekly by the American Society of Hematology, 2021 L St, NW, Suite 900, Washington DC 20036. Copyright 2011 by The American Society of Hematology; all rights reserved.
© Copyright 2026