Leukemic Cell Growth in SCID Mice as a Predictor of
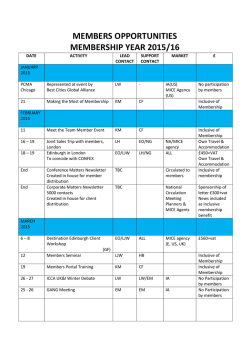
From www.bloodjournal.org by guest on February 6, 2015. For personal use only. RAPID COMMUNICATION Leukemic Cell Growth in SCID Mice as a Predictor of Relapse in High-Risk B-Lineage Acute Lymphoblastic Leukemia By Fatih M. Uckun, Harland Sather, Gregory Reaman, Jonathan Shuster, Vita Land, Michael Trigg, Roland Gunther, Lisa Chelstrom, A. Bleyer, Paul Gaynon, and William Crist Mice with severe combined immunodeficiency (SCID) provide a model system t o examine the in vivo homing, engraftment, and growth patterns of normal and malignant human hematopoietic cells. The relation between leukemic cell growth in this model and the treatment outcome in patients from whom cells were derived has not been established. Leukemic cells from 42 children with newly diagnosed high-risk B-lineageacute lymphoblastic leukemia were inoculated intravenously into CB.17 SCID mice. Mice were killed at 12 weeks or when they became moribund as a result of disseminated leukemia. All mice were necropsied and subjected to a series of laboratory studies to assets their burden of human leukemic cells.Twenty-three patients whose leukemic cells caused histopathologically detectable leukemia in SCID mice had significantly a higher relapserate did not (estimated than the 19 patients whose leukemic cells 5-year event-free survival: 29.5% Y 94.7%; 95% confidence intervals, 11.2% t o 50.7% v 68.1% t o 99.2%; P < .OOO1 by log-ranktest). The occurrenceof overt leukemia in SCID mice was was highly a significant predictor of patient relapse. The estimated instantaneous risk of relapse for patients whose leukemic cells caused overt leukemia in SCID mice was 21.5fold greater than that for the remaining patients. Thus, growth of human leukemic cells in SCID mica is a strong and independentpredictor of relapsein patients with newly diagnosed high-risk B-lineageacute lymphoblastic leukemia. Q 1995 by The American Society of Hematology. A Pathologic Specimens) in accordance with DHHS guidelines. Patient characteristics are detailed in Table 1. All 42 patients had high-risk ALL, as identified by age (ie, < l or = l 0 years), white blood cell count (WBC; ie, z50,000/pL), or cytogenetics (ie, presence of a 4; 1 1 , 1; 11, or 9;22 translocation) according to the uniform highrisk criteria of the National Cancer Institute (NCI)/Cancer Treatment Evaluation Program (CTEP) Workshop for B-lineage ALL patients. All patients received intensive treatment for high-risk ALL. CCG patients were treated with a Berlin-Frankfurt-Munster (BFM)-based or New York-based intensive multiagent chemotherapy regimen,”.I6 whereas POG patients were treated with primarily antimetabolitebased intensive chemotherapy.*’ Fourteen patients were treated on CCG regimens and 28 patients on FOG regimens. Follow-up on patients still surviving without the occurrence of leukemic relapse events ranges from 6 to 66 months, with a median follow-up of 32 months. Laboratory studies. Specimens for this study were obtained by routine diagnostic bonemarrow aspirates. Highly blast enriched CUTE LYMPHOBLASTIC leukemia (ALL) is the most common childhood malignancy, comprising about 25% of all pediatric cancer Eighty-five percent of cases arise in B-progenitor cells and can be identified as B-lineage ALL by diagnostic immunophenotyping.Is2Approximately 70% of these patients are cured with intensive multiagent chemotherapy. Hence, current research is aimed at improving therapy for children who are at risk for relapse, while minimizing treatment intensity in those who have a favorable prognosis. The risk-directed approach has the potential to decrease late effects of treatment (a major concern in these young patients) while intensifying treatment in appropriate cases to improve cure rates even further. Clearly, accurate methods of identifying prognostic features at diagnosis are crucial to avoid unnecessarily intensive treatment or inadequate therapy. We and others have used mutant C.B.17 mice with severe combined immunodeficiency (SCID) as a model system to examine the in vivo homing, engraftment, and growth patterns of n o d and malignant human hematopoietic cells.%” These mice lack functional T and B cells and are unable to reject allogeneic or xenogeneic grafts.23We compared the ability of leukemic cells from 42 children with newly diagnosed high-risk B-lineage ALL to cause leukemia in SCID mice and assessed these findings in relation to the patients’s response to treatment. Our findings suggest that the outgrowth of a patient’s leukemic cells in the SCID mouse is a strong and independent predictor of relapse after chemotherapy. MATERIALS AND METHODS Patient population. Forty-two children with newly diagnosed untreated B-lineage ALL treated at member institutions of the Childrens Cancer Group (CCG) or Pediatric Oncology Group (POG) were studied. Informed consent for treatment was obtained from parents, patients, or both based on Department of Health and Human Services (DHHS) guidelines. Bone marrow specimens were used in the SCID mouse assay system under the exemption category (45 CFR Part 46.101;b category #4 Existing Data; Records review; Blood, Vol 85, No 4 (February 15). 1995: pp 873-878 From rhe University of Minnesota Biotherapy Program, the Departments of Therapeutic Radiology and Pediatrics, Minneapolis, MN; the Childrens Cancer Group, Arcadia, CA; and the Pediatric Oncology Group, Chicago. Submitted September 8, 1994; accepted November 2, 1994. Supported in partby research grants (CA-60437,CA-51425, CA-21737, CA-4211 I , CA-42633,CA-21765[COREl,CA-30969, CA-31566, and CA-13539)from the National Cancer Institute, Department of Health and Human Services, the National Cancer Foundation, and the American Lebanese Syrian Associated Charities (ALSAC). F.M.U. is a Stohlman Scholar of the LPukemia Society of America. This is publication #l30 from the Tumor ImmunologyLaboratory, University of Minnesota. Address reprint requests to Fatih M. Uckun, MD, PhD, CCG ALL Biology Reference Laboratory and University of Minnesota Biotherapy Program, 2685 Patton Rd, Roseville, MN 551 13. The publication costs of this article were defrayed in p a n by page charge payment. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C. section 1734 solely to indicate this fact. Q 1995 by The American Society of Hematology. ooW-4971/95/8504-0031$3.00/0 873 From www.bloodjournal.org by guest on February 6, 2015. For personal use only. 874 UCKUN ET AL Table 1. Characteristics of 42 High-Risk B-LineageALL Patients Whose Leukemic Cells Were Studied in the SClD Mouse System Characteristic Distribution No. (%) Age (yr) <l 1-9 210 Male sex WBC 2 5 0 X 1 0 ~ ~ DNA index (n = 28) 21.16 <1.16 Cytogenetics (n = 28) Normal t(9;22), or t(411) or t(1;19) Splenomegaly Hepatomegaly CNS leukemia Outcome in SClD mice Leukemia detectable by histopathology Occult leukemia No evidence of leukemia 6 (21) 22 (79) 17 (40) 14 (33) 3 (7) 23 (55) 11 (26) 8 (19) Occult leukemia is ~ 1 0 % of cells from SClD mouse bone marrow, spleen, or liver positive for human CD19 antigen by flow cytometry or human &globin gene sequences detected by PCR analysis of DNA from SClD mouse bone marrow, liver, spleen, or brain. mononuclear cell fractions containing more than 90% leukemic cells were isolated by Ficoll Hypaque density gradient separation. Immunophenotyping was performed on these fractions by indirect immunofluorescence andflow cytometry using appropriate monoclonal antibodies directed against CD5, CD7, CDlO, CD13, CD19, CD20, CD21, CD22, CD24, CD34, sIg, and MHC-11, as previously described.” Cytogenetic studies and DNA flow cytometry were performed, as previously reported.’ All SCID mice (age, 7 to 10 weeks; sex, female) were produced by specific pathogen-free (SPF) CB-l7 scidscid breeders and maintained in an SPF environment in Micro-Isolator cages (Lab Products, Inc. Maywood, NY), as previously reported.2426Mice (1 to 3, depending on the availability of sufficient cell numbers) were inoculated with 5 X lo6 leukemic cells via tail vein injections. Mice were killed at 12 weeks or when they became moribund as a result of disseminated leukemia. Mice were necropsied at the time of death or euthanization, and histopathology, flow cytometry, and polymerase chain reaction (PCR) analyses were performed to assess their burden of human leukemia cells, as previously reported.2426For each mouse, multiple tissues, including brain, lung, heart, thymus, liver, kidney, spleen, gut, pancreas, urinary bladder, uterus, ovary, sagittal sections of a femur, and several vertebrae, were histologically evaluated. All histopathologic studies of SCID mouse tissues were performed by a veterinary pathologist (ie, R.G.) without any knowledge of patient outcome. Multiparameter flow cytometric analyses of single-cell suspensions from SCID mouse bone marrow, liver, and spleen were performed using two-color immunofluorescence staining techniques and pairwise combinations of a selected panel of fluorochromelabeled (fluorescein isothiocyanate W C ] or phycoerythrin [PE]) monoclonal antibodies to identify human B-lineage ALL blasts.w26 The following monoclonal antibodies were included in the analyses: B43 (anti-CD19)-PE, Leu12 (anti-CD19)-FITC, J5 (anti-CDlO)-PE, Leu16 (anti-CD20)-FITC, 9.4 (anti-CD45)-PE, 9.4 (anti-CD45)FITC, and 2C3 (anti-1gM)-FITC. Human DNA was detected by amplifying a 110-bp fragment from the first exon of the human 0- globin gene using two 20-base oligonucleotide primers, PC03 and that flank the region to be amplified, as previously described in All evaluations of SCID mouse tissues were conducted in a prospective fashion andthey were blinded to knowledge of treatment outcome. Statistical analysis. Possible associations of leukemic cell outgrowth in SCID mice with clinical, demographic, and laboratory features of thepatients from whom cells were derived were examined by using x’ analyses of categorical groupings. The primary outcome measure was event-free survival (EFS), definedas the time from study entry to the first major event (failure to achieve remission, relapse at any site, or death). For patients who did not experience an event, EFS was defined as the time to last follow-up and treated as a censored life table observation. Estimates of EFS were based on the Kaplan-Meier life table method for censored data.35Standard errors for the life table estimates were calculated using Greenwood’s formula. Comparisons of outcome between patient subsets were performed by the log rank test for univariate comparisons and for those that were stratified on a single additional fa~tor.~’,~’ Calculations of the relative event rate (ie, hazard rate) used the O/E method for univariate or stratified analysis and the exponent of the regression coefficient procedure for the proportional hazards regression.38Confidence intervals (95%) were calculated using the log-log transformationof the survival function together with Greenwood’s formula because EFS outcome for one patient group was almost 100%.Multivariate analysis was performed using the Cox proportional hazards regression model for all factors with reasonably complete data (ie, leukemic cell growth in SCID mice, WBC, age, sex, hepatomegaly, splenomegaly, platelet count, hemoglobin level, and central nervous system [CNS] disease at diagnosis). All statistical analyses were performed by the Group Statistician of the Childrens Cancer Group (ie, H.S.). PCO4. RESULTS Human leukemiacells are found in aggregates in the SCID mouse organs other than bone marrow and they almost always destroy the normal organ architecture. Therefore, extramedullary human leukemia is easily detected in SCID mouse tissues. The sensitivity of histopathologic determinations in SCID mouse bone marrow is comparable with that of standard morphologic determinations ofleukemic cell burden in human bone marrows. O n e percent to 5% involvement is readily detectable; sometimes even a 0.1 % involvement can be detected by histopathology if leukemic cells are found in aggregates. In the present study, a marked interpatient variation existed in the extent of leukemic cell engraftment and outgrowth in SCID mice challenged with primary bonemarrow blast cells from children with high-risk B-lineage ALL. However, there were no intrapatient inconsistencies; in each case in which cells were inoculated into two or more mice, each of the animals exhibited the same pattern of leukemic cell growth (or lack thereof). No histopathologic evidence of leukemia was found in SCID mice inoculated with leukemic cells from 19 of 42 (45%) patients (Table 1). However, in 11 of these 19 cases, occult human leukemia could be detected in SCID mouse tissues by multiparameter flow cytometric analysis of bone marrow, liver, and spleen mononuclear cell suspensions for CD19+CDlO+”sIgM-B-lineage ALL cells (2 cases only; the fraction of flow cytometrically detectable human B-lineage ALL cells among the mononuclear cells obtained from bone marrow, liver, or spleen of these mice did not exceed 10%) and/or PCR analysis of From www.bloodjournal.org by guest on February 6, 2015. For personal use only. HUMAN ALL IN SCID 875 Table 2. Relationship Between Patients' Presenting Clinicalor Laboratory Features and Development of Histopathoiogically Detectable Leukemia in SCiD Mice ~~ ~ ~~~ Age (yr) Splenomegaly Hepatomegaly CNS involvement WBC ( ~ 1 0 9 1 ~ ) (69.6%) 16 Platelet count (xlOg/L)* Hgb level (g/dL)* Cytogeneticst (N = 191 ~ ~~ 1 (5.3%) 2 (8.7%) (65.2%) 15 .21 8 (42.1%) (52.6%) 6 10 (26.1%) Male .32 (63.2%) 12 1 1 (47.8%) Female (52.2%) 12 7 (36.8%) (56.5%) 13 .02 4 (21.1%) Absent (78.9%) 15 (43.5%) 10 Present 8 (34.8%) .83 6 (31.6%) Absent (68.4%) 13 (65.2%) 15 Present 2 (8.7%) .67 1 (5.3%) 18 (94.7%) Absent (91.3%) 21 <50 7 (30.4%) .66 7 (36.8%) 2 50 12 (63.2%) 9 (50.0%) <50 (73.9%) 17 9 (50.0%) 250 6 (26.1%) .04 6 (33.3%) <8 (65.2%) 15 2 8 (66.7%) 12 8 (34.8%) 1 1 (57.9%) <1.16 21.16 1 (5.3%) 0 (0.0%) 7 (36.8%) Unknown 7 (30.4%) Normal 3 (13.0%) .83 3 (15.8%) 8 142.1%) 14 (60.8%) Pseudodiploid Unknown 8 (42.1%) 6 (26.1%) ~ ~ <l 1-9 =l0 Sex DNA indext (69.6%) ~~ P Value SCID- Patients SCID' Patients (N = 231 Category Features -~ 16 .l 1 .88 Diagnostic values for Hgb level or platelet count were not available for one of the SCID- patients. t DNA flow cytometry and karyotyping were each performed in 28 cases. DNA from bone marrow, liver, spleen, or brain for human @-globingene sequences (all 11 cases), which has previously been shown to detect a 0.1% human leukemic cell contamination in SCID mouse tissuesz5 (Table 1). By comparison, leukemic cells from the remaining 23 (55%) patients caused histopathologically detectable overt leukemia in SCID mice (Table 1). In these mice, bone marrow was always involved, whereas the involvement of other organs showed interpatient variations. Bone marrow, spleen, and ovarian involvement was manifested as replacement of normal tissue elements by diffuse sheets of densely packed leukemic cells with up to 20 mitotic figures per high power field. When involved, livers showed infiltration in the subcapsular region, portal spaces, and sinusoids. Infiltrated kidneys had variably sized cortical, interstitial, and perivascular accumulations of leukemic cells and often had large masses in the pelvic fat. The leptomeninges of the brain contained thin rafts of leukemic cells. Affected lungs contained a light infiltrate in the alveolar septa, small rafts of leukemic cells in the intrapulmonary veins, or perivascular cuffs of leukemic cells. Multiparameter flow cytometric analyses of bone marrow mononuclear cells from SCID mice with histopathologic evidence of marTOW involvement confirmed the abundance of a 1 0 + " CD19+CD45+sIgM- human B-lineage ALL cells. PCR amplification of a 110-bp DNA fragment from the first exon of the human @-globingene confirmed the presence of human origin DNA in bone marrow, liver, spleen, and brain of SCID mice with disseminated B-lineage ALL. When we examined the possible association of leukemic cell growth in SCID mice with high-risk ALL patients' clini- cal, demographic, and laboratory features, we found that leukemic cells from patients with splenomegaly (P = .02) and with low hemoglobin levels (P = .W)were slightly more likely to cause histopathologically detectable leukemia in SCID mice (Table 2). By comparison, age, sex, hepatomegaly, CNS disease, leukocyte count, platelet count, DNA index, or specific chromosomal translocations did not correlate significantly with leukemic cell growth in SCID mice (Table 2). The 23 patients whose leukemic cells caused histopathologically detectable leukemia in SCID mice had a significantly higher failure rate than those patients whose leukemic cells did not (N = 19; 14 relapses and one induction failure v 1 relapse; log rank test, P = .OOOl; univariate life table estimated relative hazard, 21.5). Consequently, the former group had a significantly worse 5-year EFS (29.5% v 94.7%; 95% confidence intervals, 11.2% to 50.7% v 68.1% to 99.2%; P = .OOO1 by log rank test; Fig 1). Stratified log rank analyses were conducted to adjust individually for potentially important clinical and laboratory features, such as W C , cytogenetics, age, sex, hepatomegaly, splenomegaly, CNS involvement, platelet count, hemoglobin, immunophenotype (ie, percent positivity of leukemic cells for surface CD10, CD19, CD24, or CD34 antigen expression), and DNA index. Histopathologically detectable leukemia in SCID mice remained a verystroKg predictor of patient relapse after adjusting individually for the effects of each of these factors. All significance levels for the SCID model predictor were less than or equal to .006.Multivariate Cox regression analysis was also performed and only two factors, namely histo- From www.bloodjournal.org by guest on February 6, 2015. For personal use only. UCKUN ET AL 876 1.oo only byflow cytometry and/or PCR or failed to engraft in SCID mouse tissues. Notably, the ability of leukemic cells Q, to cause histopathologically detectable leukemia in SCID 9? mice was associated with poor EFS in patients from whom 5 the cells were obtained. Adjustment for numerous traditional E 0.75 prognostic factors in bivariate stratified log-rank analyses W and multivariate analysis using the Cox proportional hazards regression modelhadvery little attenuating effect on the .prognostic significance of occurrence of overt leukemia in .-> 2 0.50 LeLkemhin SCID mice for this patient population with high-risk ALL. SClD mice, Biologic data generated in the SCID mouse model system may thus improve our ability to predict treatment response C 0 .-c in high-risk B-lineage ALL, permitting accurate segregation of patients into distinct prognostic subgroups. 0.25 Histopathologic examinations showed no evidence of leuP=0.0001 kemic infiltrates in the organs of SCID mice challenged with a primary blasts from19of the 42 patients. In 11 of these I I I I I I I I I I patients, occult leukemia cells were detected by multipa0.0 1 2 3 4 5 rameter flow cytometry and/or PCR in SCID mouse bone marrow, liver, spleen, andor brain. However, none of these Years F m Study Entry 11 patients have relapsed. Thus, occult leukemia in SCID mice, in the absence of histopathologic evidence of leukemic Fig 1. EFSofB-lineage ALL patients in relation to development of human Iaukemiain SClD mice inoculatedwith their leukemic cells. infiltrates in any of the SCID mouse organs, did not have Patients whose leukemic cells didnot cause histopathologically dean apparent prognostic impact. Larger studies with longer tectable leukemia in SClD mice In = 19) fared significantly better than follow-up are needed to determine whether this subgroup of those whose leukemic cells produced histopathologically detectable patients may be at increased risk of late relapses. leukemia in this model (n = 23). Tick marks on the curves indicate the last follow-up time for patients who have not experienceda disThe reasons for the observed interpatient heterogeneity ease event. The one relapse in the group of patients whose leukemic and prognostic impact of leukemic cell growth in SCID mice cells failed to causeleukemiain SClD mice occurred at 6 months remain unclear. Kamel-Reid et a1," Cesano etal,"and postdiagnosis (95% confidence interval estimate for EFS = 68.1%. Uckun et a124,2s have reported that leukemic B-cell precursors 99.2%). The latest relapse to date for the group of patients whose from established pre-B ALL cell lines cause disseminated leukemic cells caused leukemiain SClD mice was at 30 months. For this group of patients, the 95% confidence intervals for EFSat 6,18, leukemia in SCID mice. Recently, Kamel-Reid et a13' also and 30 months of follow-up are 46.6%to 84.2%. 26.8% to 66.1%. and reported that leukemic cells from five patients with relapsed 11.2% to 50.7%. respectively.Theestimatedmedian EFS for the B-lineage ALL proliferated rapidlyin SCID mouse bone group whose leukemic calls caused overt leukemia in SClD mice is marrow, spleen, thymus, and peripheral organs, leading to 9.5 months. morbidity and mortality. It is possible that the SCID mouse model system favors the in vivo expansion of drug resistant blast populations and/or highly clonogenic blast populations pathologically detectable leukemic cell growth in SCID mice capable of rapid self-renewal and clonal expansion after es( P = .004) and hepatomegaly ( P = .05) had predictive value caping the lethal actions of multiagent chemotherapy. in this subset of poor prognosis patients. Of the numerous clinical and biologic factors reported to Unlike the development of histopathologically detectable be of prognostic value in assessing the risk of relapse after leukemia in SCID mice, detection of occult leukemia in the contemporary therapy for ALL,'.',9.1',,'7.'8 the most consistent absence of histopathologic evidence of leukemic infiltrates are age and leukocyte count at diagnosis. However, these in any of the SCID mouse organs did not have an apparent features alone or in combination are not sufficient to identify prognostic impact. None of the 11 patients whose leukemic all patients at increased risk of relapse.' Genetic features cells caused occult leukemia in SCID mice as detected by of leukemic cells (tumor cell DNA content or ploidy and multiparameter flow cytometry and/or PCR have relapsed karyotype) have also been shown to provide additional progand all remain alive and disease free at 23 to 60 months nostic inf~rmation.~ Flow cytometric assessment of ploidy is (median, 42 months) after diagnosis. rapid, relatively easy and inexpensive, and produces accurate results in almost allcases.' Leukemic cell hyperdiploidy DISCUSSION (DNA index 2 I . 16) identifies a subgroup of B-lineage ALL patients withan estimated 4-year disease-free survival of We found a pronounced variation in the ability of leukegreater than 90%in the context of antimetabolite-based treatmic cells from children with newly diagnosed high-risk Bm e ~ ~However, t.~ ploidy is useful in identifying only the 20% lineage ALL to engraft and cause leukemia in SCID mice. of patients who are at lowrisk of treatment failure and cannot Leukemic cells from some patients caused disseminated hupredict a high risk of relapse.' The SCID mouse system man leukemia in SCID mice, as detected by histopathology described here eliminates some of the problems associated and confirmed by flow cytometry as well as PCR. Leukemic with other prognostic tools, appears to complement the progcells from other patients produced occult leukemia detectable 2 P 8 g e "i From www.bloodjournal.org by guest on February 6, 2015. For personal use only. HUMAN ALL IN SCID MICE nostic value of conventional risk features such as age and leukocyte count, and holds potential for large-scale evaluation of newly diagnosed cases of B-lineage ALL. Results from this assay could be very useful for determining the intensity of further therapy after remission induction in highrisk B-lineage ALL. In addition to providing information of independent prognostic value for patients with high-risk features, this SCID mouse model of human B-lineage ALL may also permit assessment of the “in vivo” activity of individual therapeutic agents against the patient’s leukemic cells. Such information could be highly useful for planning the components of intensification as well as maintenance chemotherapy in high-risk B-lineage ALL. REFERENCES 1. Champlin R, Gale RP. Acute lymphoblastic leukemia: Recent advances in biology and therapy. Blood 73:2051, 1989 2. Crist WM, Pullen DJ, Rivera GK: Acute lymphoid leukemias, in Fembach DJ, Vietti T (eds): Clinical Pediatric Oncology fed 4). St Louis, MO, Mosby, 1991, p 305 3. Pui C-H, Crist WM, Look AT: Biology and clinical significance of cytogenetic abnormalities in childhood acute lymphoblastic leukemia. Blood 76:1449, 1990 Clinical and biologic relevance 4. Pui C-H, Behm F, Crist W: of immunologic marker studies in childhood acute lymphoblastic leukemia. Blood 82:343, 1993 5. Trueworthy R, Shuster J, Look T, Crist W, Borowitz M, Carroll A, Frankel L, Harris M, Wagner M, Haggard A, Mosijczuk A, Pullen J, Steuber P, Land V: Ploidy of lymphoblasts is the strongest predictor of treatment outcome in progenitor cell acute lymphoblastic leukemia in childhood: A Pediatric Oncology Group Study. J Clin Oncol 10:606, 1992 6. Uckun FM, Kersey JH, Gajl-Peczalska KJ, Heerema NA, Provisor AJ, Haag D, Gilchrist G, Song CW, Arthur DC, Roloff J, Lampkin B, Greenwood M, Dewald G, Vallera DA: Heterogeneity of cultured leukemic lymphoid progenitor cells from B-cell precursor ALL patients. J Clin Invest 80:639, 1987 7. Crist W, Boyett J, Jackson J, Vietti T, Borowitz M, Chauvenet A, Winick N, Ragab A, Mahoney D, Head D, Iyer R, Wagner H, Pullen J: Prognostic importance of the pre-B cell immunophenotype and other presenting features in B-lineage acute lymphoblastic leukemia: A Pediatric Oncology Group Study. Blood 741252, 1989 8. Abshire TC, Buchanan GR, Jackson JF, Shuster JJ, Brock B, Head D, Behm F, Crist WM, Link M, Borowitz M, Pullen DJ: Morphologic, immunologic, and cytogenetic studies in children with acute lymphoblastic leukemia at diagnosis and relapse: A Pediatric Oncology Group Study. Leukemia 6:357, 1992 9. Sullivan MP, Pullen DJ, Crist WM, Brecher M, Ramirez I, Sabio H, Borowitz MJ, Head DR, Cerezo L, Shuster JJ, Murphy SB: Clinical and biological heterogeneity of childhood B-cell acute lymphocytic leukemia: Implications for clinical trials. Leukemia 4 5 , 1990 10. Uckun FM, Gajl-Peczalska K, Myers DE, Jaszcz W, Haissig S, Ledbetter JA: Temporal association of CD40 antigen expression with discrete stages of human B-cell ontogeny and the efficacy of anti-CD40 immunotoxins against clonogenic B-lineage acute lymphoblastic leukemia as wellas B-lineage non-Hodgkin’s lymphoma cells. Blood 76:2449, 1990 11. Bleyer WA, Sather H, Coccia P, Lukens J, Siegel S, Hammond D: The staging of childhood acute lymphoblastic leukemia: Strategies of the Childrens Cancer Study Group and a three-dimensional technique of multivariate analysis. Med Pediatr Oncol 14:271, 1986 12. Gaynon P, Bleyer WA, Steinherz P, Finkelstein J, Littman P, Miller D, Reaman G, Sather H, Hammond D: Modified BFMtherapy for children with previously untreated acute lymphoblastic leukemia and unfavorable features. Am J Pediatr Hematol Oncol 10:42, 1988 13. Gaynon P, Steinherz P, Bleyer WA, Ablin A, Albo V, Finkelstein J, Grossman N, Littman P, Novak L, Pyesmany A, Reaman G, Sather H, Hammond D: Intensive therapy for children with acute lymphoblastic leukemia and unfavorable presenting features. Lancet 2:921, 1988 14. Tubergen D, Gilchrist G, OBrien R, Coccia P, Sather H, Waskenvitz M, Hammond D: Prevention of central nervous system disease in intermediate risk acute lymphoblastic leukemia: Comparison of cranial radiation and intrathecal methotrexate and the importance of systemic therapy. J Clin Oncol 11:527, 1993 15. Crist W, Boyett J, Jackson J, Vietti T, Borowitz M, Chauvenet A, Winick N, Ragab A, Mahoney D, Head D, Iyer R, Wagner H, Pullen J: Prognostic importance of the pre-B-cell immunophenotype and other presenting features in B-lineage acute lymphoblastic leukemia: A Pediatric Oncology Group Study. Blood 74:1252, 1989 16. Cherlow J, Steinherz P, Sather H, Gaynon P, Grossman N, Kersey J, Maurer H, Brenneman J, Trigg M, Hammond D: The role of radiation therapy in the treatment of acute lymphoblastic leukemia with lymphomatous presentation. Int J Radiat Oncol Biol Physics 27:1001, 1993 17. Steinherz P, Gaynon P, Miller D, Reaman G, Bleyer WA, Finkelstein J, Evans R, Meyers P, Steinherz L, Sather H, Hammond D: Improved disease-free survival of children with acute lymphoblastic leukemia at high risk for early relapse with the New York Regimen-A new intensive therapy protocol. J Clin Oncol 4:744, 1986 18. Bleyer A, Sather H, Nickerson J, Coccia P, Finkelstein J, Miller D, Littman P, Lukens J, Siegel S, Hammond D Monthly pulses of vincristine and prednisone prevent bone marrow and testicular relapse in childhood acute lymphoblastic leukemia. J Clin Oncol 9:1012, 1991 19. Uckun FM, Kersey JH, Haake R, Weisdorf D, Nesbit M, Ramsay NKC: Pretransplant leukemic progenitor cell burden as a predictor of relapse after autologous bone marrow transplantation for high risk remission acute lymphoblastic leukemia. N Engl J Med 329:1296, 1993 20. Crist W, Carroll A, Shuster J. Jackson J, Head D, Borowitz M, Behm F, Link M, Steuber P, Ragab A, Hirt A, Brock B, Land V, Pullem J: Philadelphia chromosome positive childhood acute lymphoblastic leukemia: Clinical and cytogenetic characteristics and treatment outcome. A Pediatric Oncology Group Study. Blood 76:489, 1990 21. Pui C-H, Crist WM: Cytogenetic abnormalities in childhood acute lymphoblastic leukemia correlate with clinical features and treatment outcome. Leuk Lymphoma 7:259, 1992 22. Crist WM, Carroll AJ, Shuster JJ, Behm FG, Whitehead M, Vietti TJ, Look AT, Mahoney D, Ragab A, Pullen DJ, Land VJ: Poor prognosis of children with pre-B acute lymphoblastic leukemia is associated with the t(1; 19)(q23;p13): A Pediatric Oncology Group Study. Blood 76:117, 1990 23. Dorshkind K, KeIler GM, Philips RA, Miller RG, Bosma GC, O’Toole M, Bosma MJ: Functional status of cells from lymphoid and myeloid tissues in mice with severe combined immunodeficiency disease. J Immunol 132:1804, 1984 24. Uckun FM, Manivel C, Arthur D, Chelstrom L, Finnegan D, Irvin JD, Myers DE, Chelstrom LC: In vivo efficacy of B43 (antiCD19)-pokeweed antiviral protein (PAP) immunotoxin against human pre-B cell acute lymphoblastic leukemia (ALL) in mice with severe combined immunodeficiency (SCID). Blood 79:2201, 1992 25. UckunFM, Chelstrom LM, Finnegan D, Tuel-Ahlgren L, Irvin JD, Myers DE, Gunther R: Effective immunochemotherapy of From www.bloodjournal.org by guest on February 6, 2015. For personal use only. 878 CALLA'++ human pre-B acute lymphoblastic leukemia in mice with severe combined immunodeficiency using B43 (anti-CDI9) pokeweed antiviral protein (PAP) immunotoxin plus cyclophosphamide. Blood 79:3116, 1992 26.Uckun F M , Downing JR, Gunther R, Chelstrom LM, Finnegan D, L and VJ, Borowitz MJ, Carroll AJ, Crist WM: Human t( 1; 19)(q23;p13) pre-B acute lymphoblastic leukemia in mice with severe combined immunodeficiency. Blood 81 :3052, 1993 27. McCune JM, Namikawa R, Kaneshima H, Schultz LD, Lieberman M, Weisman IL: The SCID-hu mouse: Murine model for the analysis of human hematolymphoid differentiation and function. Science 241:1632, 1988 28. Mosier DE, Golizia M,Baird SM, Wilson DB: Transfer of a functional human immune system to mice with severe combined immunodeficiency. Nature 335256, 1988 29. Barry TS, Jones DM, Richter CB, Haynes BF: Successful engraftment of human postnatal thymus in severe combined immunodeficient mice. Differential engraftment of thymic components with irradiation versus anti-asialo GM-l immunosuppressive regimens. J Exp Med 173:167, 1991 30. Kamel-Reid S, Letarte M, Sirard C, Doedens M, Grunberger T, Fulop G, Freedman MH, Phillips RA, Dick JE: A model of human acute lymphoblastic leukemia in immune-deficient mice. Science 246: 1597, 1989 3 I . Cesano A, O'Connor R, Lange B, Finan J, Rovera G, Santoli D: Homing and progression patterns of childhood acute lymphoblas- UCKUN ET AL tic leukemias in severe combined immunodeficiency mice.Blood 77:2463, 1991 32. Kamel-Reid S, Letarte M, Doedens M, Greaves A, Murdoch B, Grunberger T, Lapidot T, Thorner P, Freedman MH, Phillips RA, Dick JE: Bone marrow from children in relapse with pre-B acute lymphoblastic leukemia proliferates and disseminates rapidly in SCID mice. Blood 78:2973, 1991 33. Uckun FM, Downing JR. Chelstrom LM, Gunther R. Chardan-Langlie M, Crist WM: Human t(4; 1 l)(q21;q23)acute lymphoblastic leukemia in mice with severe combined immunodeficiency. Blood 84: I , 1994 34.Dick JE, Lapidot T, Pflumio F: Transplantation of normal and leukemic human bone marrow into immuno-deficient mice: Development of animal models for human hematopoiesis. Immunol Rev 124:2543, 1991 35. Kaplan E, Meier P: Non-parametric estimation from incomplete observations. J Am Stat Assoc 53:457, 1958 36. Mantel N: Evaluation of survival data and two new rank order statistics arising in its consideration. Cancer Chem Rep 50: 163, 1966 37. Pet0 R, Pike MC, Armitage P, Breslow NE, Cox DR, Howard SV, Mantel N, McPherson K, Pet0 J, Smith PG: Design and analysis of randomized clinical trials requiring prolonged observation of each patient. 11. Analysis and examples. Br J Cancer 35:1, 1977 38. Breslow N: Analysis of survival data under the proportional hazards model. Int Stat Rev 43:45, 1975 From www.bloodjournal.org by guest on February 6, 2015. For personal use only. 1995 85: 873-878 Leukemic cell growth in SCID mice as a predictor of relapse in highrisk B-lineage acute lymphoblastic leukemia FM Uckun, H Sather, G Reaman, J Shuster, V Land, M Trigg, R Gunther, L Chelstrom, A Bleyer and P Gaynon Updated information and services can be found at: http://www.bloodjournal.org/content/85/4/873.full.html Articles on similar topics can be found in the following Blood collections Information about reproducing this article in parts or in its entirety may be found online at: http://www.bloodjournal.org/site/misc/rights.xhtml#repub_requests Information about ordering reprints may be found online at: http://www.bloodjournal.org/site/misc/rights.xhtml#reprints Information about subscriptions and ASH membership may be found online at: http://www.bloodjournal.org/site/subscriptions/index.xhtml Blood (print ISSN 0006-4971, online ISSN 1528-0020), is published weekly by the American Society of Hematology, 2021 L St, NW, Suite 900, Washington DC 20036. Copyright 2011 by The American Society of Hematology; all rights reserved.
© Copyright 2026