Favorable Prognosis of Hyperdiploid Common
From www.bloodjournal.org by guest on February 6, 2015. For personal use only.
Favorable Prognosis of Hyperdiploid Common Acute Lymphoblastic
Leukemia May Be Explained by Sensitivity to Antimetabolites
and Other Drugs: Results of an In Vitro Study
By G.J.L. Kaspers, L.A. Smets, R. Pieters, C H . Van Zantwijk, E.R. Van Wering, and A.J.P. Veerman
DNA hyperdiploidy is a favorable prognostic factor in childhood acute lymphoblastic leukemia (ALL). The explanation
for this prognostic significance islargely unknown. Wehave
studied whether DNA ploidy was related to cellular resistance to 12 drugs, assessed with themethyl-thiazol-tetrazolium assay, in samples of 74 children with common (CD10'
precursor B-cell)ALL. Sixteen patients had hyperdiploid ALL
cells and 58 patients hadnonhyperdiploid ALL cells. Hyperdiploid ALLcells were more sensitive to mercaptopurine
(median, 9.0-fold; P = .000003),to thioguanine (1.4-fold; P =
.023),to cytarabine (1.8-fold; P = .016), and to l-asparaginase
(19.5-fold; P = .022) than werenonhyperdiploid ALL cells. In
contrast, these two ploidy groups did notdiffer significantly
in resistance to prednisolone, dexamethasone, vincristine,
vindesine,daunorubicin,doxorubicin,
mitoxantrone, and
teniposide. The percentage of S-phase cells was higher ( P
= .05) in the hyperdiploid ALL samples (median, 8.5%) than
in the nonhyperdiploid ALL samples (median, 5.7%). However, the percentage of cellsin S-phase was notsignificantly
related to in vitro drug resistance. We conclude that the
favorable prognosis associated with DNA hyperdiploidy in
childhood common ALL may be explained by a relative sensitivity of hyperdiploid common ALL cells to antimetabolites,
especially to mercaptopurine and to l-asparaginase.
0 1995 by The American Societyof Hemstology.
T
sala, Sweden) for 15 minutes (room temperature, 1,OOOg). Immunofluorescence techniques were used for terminal deoxynucleotidyl
transferase (TdT) and cytoplasmic and surface Ig M heavy chain
staining, whereas an indirect immunoperoxidase staining technique
on cytocentrifuge preparations was used for all other antibodie~.'~
A leukemia was considered to be a precursor-B common-ALL (cALL) if the malignant cells were positive for TdT, CDlO, CD19,
andHLA-DRand negative for cytoplasmic and/or surface Ig M
heavy chain.
Materials. Prednisolone sodium phosphate (PRD), dexamethasone sodium phosphate (DXM), daunorubicin hydrochloride (DNR),
l-asparaginase (ASP), cytarabine (ARA-C), vindesine sulphate
(VDS), vincristine sulphate (VCR), mitozantrone hydrochloride
(MIT), teniposide (TEN), and acidified (0.04 N HCl) isopropanol
were obtained from the hospital pharmacy. Thioguanine (6TG), mercaptopurine (6MP), and doxorubicin hydrochloride (DOX) were obtained from Sigma Chemical CO (St Louis, MO).
PRD was dissolved in saline. DNR, ASP, VDS, and DOX were
dissolved in distilled water. 6MP and 6TG were dissolved in 0.1 N
NaOH. DXM, ARA-C, VCR, MIT, and TEN were obtained in soluble form.
Cells were cultured in suspension inRPM1 1640 (GIBCO, Uxbridge, UK) containing fetal calf serum (Flow Laboratories, Irvine,
UK) and supplements as described previously.i6 MTT (3-[4,5dimethyl-thiazol-2-yI]-2,5-diphenyltetrazolium-bromide)
was obtained from Sigma.
Drug resistance assay. The MTT assay was performed at the
research laboratory for pediatric hemato-onco-immunology ofthe
HE IDENTIFICATION OF prognostic factors in childhood acute lymphoblastic leukemia (ALL) has allowed
the use of risk-group stratification and subsequent risk-group
adapted treatment. This approach is likely to have contributed to the marked improvement in the prognosis of this
disease in children.' DNA ploidy, as determined by karyotyping or flow cytometric measurement of DNA content,
has strong and independent prognostic Significance.' DNA
hyperdiploidy is especially associated with a favorable prognosis in B-lineage
The explanation for the good
prognosis associated with DNA hyperdiploidy in B-lineage
ALL is unknown. However, Whitehead et a l l ' recently reported that DNA hyperdiploid ALL cells accumulated higher
levels of methotrexate polyglutamates than did other aneuploid and diploid ALL cells, which suggests that DNA hyperdiploid ALL cells are more sensitive to methotrexate.
We studied the relationship between DNA ploidy, percentage of cells in S-phase, and cellular resistance to 12 drugs
assessed using the methyl-thiazol-tetrazolium (Mm)assay
in 74 samples of children with newly diagnosed common
ALL. The MTT assay is an objective and reliable cell culture
drug-resistance assay, suited for large-scale testing of leukemia and lymphoma samples." Using this assay, we showed
that in vitro resistance to certain drugs is related to the clinical outcome in childhood ALL.13
PATIENTS AND METHODS
Patients. Bone marrow or peripheral blood samples were sent
by local institutions to the Dutch Childhood Leukemia Study Group
laboratory for confirmation of the new diagnosis ALL by classification according to the criteria of the French-American-British (FAB)
groupi4and imm~nophenotyping.'~
Samples of 88 children with nonB ALL were sent by the Dutch Childhood Leukemia Study Group
laboratory to the research laboratory for pediatric hemato-onco-immunology of the Free University Hospital for cellular drug resistance
testing and to the Department of Experimental Therapy of the Netherlands Cancer Institute for DNA ploidy and percentage of S-phase
cells measurements. Informed consent was obtained. Cellular drug
resistance and DNA ploidy assays were successfully performed in
74 patients. Table 1 summarizes the clinical and cell biologic features
of these patients.
Cells. Mononuclear cells were isolated by Ficoll density gradient
centrifugation (Ficol Paque; density, 1.077 g/mL; Pharmacia, UppBlood, Vol 85, No 3 (February l ) , 1995: pp 751-756
Fromthe Department of Pediatrics, Free University Hospital,
Amsterdam; the Department of Experimental Therapy, The Netherlands Cancer Institute, Amsterdam; and the Dutch Childhood Leukemia Study Group, The Hague, The Netherlands.
Submitted September 13, 1994; accepted September 27, 1994.
Supported by the Dutch Cancer Society ( I K A 89-06) and by the
project VONK (VU Onderzoek Naar Kinderkanker).
Address reprint requests to G.J.L. Kaspers, MD, PhD, Department
of Pediatrics, Free University Hospital, De Boelelaan 1117, l081
HV Amsterdam, The Netherlands.
The publication costs of this article were defrayed in part by page
charge payment. This article must therefore be hereby marked
"advertisement" in accordance with 18 U.S.C. section 1734 solely to
indicate this fact.
0 1995 by The American Society of Hematology.
0006-4971/95/8503-0117$3.00/0
751
From www.bloodjournal.org by guest on February 6, 2015. For personal use only.
752
KASPERS ET AL
Table 1. Features of 74 Children With Newly Diagnosed c-ALL
DNA Ploidy
Nonhyperdiploid
No. of patients
58
Malefiemale ratio
27/31
Median
age
in
mo (range)
54 (3-190)
Median WBC x109/L
25.5 (3.6-729) 39.2
(range)(2.5-149.4)
FAB type
L1
47
L2
11
Median percentage of cells
in S-phase (range)
(4.2-20)
(0.2-30)
8.5
5.7
Hyperdiploid
16
1214
(17-190)
44
14
2
thusattemptedtoexcludenear-triploidandnear-tetraploidcases
(with a DNA index of > 1.35) from the hyperdiploid group,because
these patients have a less favorable prognosis? The percentage of
S-phase cells was determined by planimetry of DNA cell readings,
and was expressed as a percentage of all cells, irrespective of DNA
content.
Statistics. Computer equipment was provided by Olivetti NederlandBV (Leiden, The Netherlands). The Wilcoxon's ranking test
for unpaired data and thex' test were used for two-tailed testing at
a level of significance of .05. The Spearman's rank correlation test
(parameterp ) was used to study the relation between the percentage
of S-phase cells and LC50 values.
RESULTS
Sixteen (22%) of the 74 patients had hyperdiploid ALL
cells and 58 patients had nonhyperdiploid ALL cells. Patient
Free University Hospital within 36 hours after collection of the bone characteristics of the two groupsare shown in Table1. These
characteristics did not differsignificantly, except that hypermarrow or peripheral blood sample. Samples from these sources do
not differ in drug resistance and were therefore evaluated together." diploidy was more frequentin male patients ( P = .M).HowAll samples tested with the MlT assay contained 280% leukemic
ever, for 14 nonevaluable cases, the white blood cell counts
in case of doubt,
cells after isolation (assessed morphologically and,
( M C ) of the 9 hyperdiploid cases were lower (median, 6.2
also immunologically), which has proven to give reliable test reX 109/L; range, 3.2 to 41.9 X 109/L) than those of the 5
s u l t ~ . 'In
~ allsamples,thecellviability,assessed
by trypanblue
nonhyperdiploid cases (median, 23.8 X 109/L; range, 4.8 to
exclusion, was 295% at the start of the culture.
89.3 X 109/L). Patient characteristics other then WBC did
Eighty microliters ofcell suspension (2X lo6cells/mL)was added
not differ between the ploidy groups in these nonevaluable
to 20pL of the various drugsolutions in 96-well microculture plates.
cases. The MTT assay results of these 14 samples were not
Each drug was tested in 6 concentrations in duplicate, with concenevaluable because of an optical density of less than 0.050
tration ranges as reported previously.'6 These concentrationsdo not
(n = 7) or because of less than 70% of leukemic cells in the
necessarily stay the same during the 4 days of incubation. Expericontrol wells (n = 7). The failure rate was thus significantly
ments (not shown here) showed no differences between 6MP and
to the
( P = ,001)higherin hyperdiploid c-ALLsamples (9/25)
6TG regarding their in vitro behavior (stability and adherence
walls of the plates). Wells with culture medium only (for 6MP and than in nonhyperdiploid c-ALL samples
(5/63). In agreement
6TGwith drug) were used to blank the reader, and
6 wells with
with this observation, we found thatthe control cell survival
cells in medium without drugs were used to determine the control
in the successfully tested samples was lower ( P = .003) in
cell survival and to calculate the coefficient of variation of control
hyperdiploid samples (median, 46%; range, 26% to 69%)
wells. The plates were incubated in humidified air containing
5%
than in nonhyperdiploid samples (median, 68%; range, 23%
CO2 for 4 days at 37°C. Then, 10 pL of MTT solution (5 mg/mL)
was added to the plates. After shaking the plates until the cell pellet to 135%).Similarly, the percentage of leukemiccells in
control wells after 4 days of culture was lower ( P = .005)
was resuspended, they were incubated for 6 hours. The tetrazolium
in hyperdiploid samples (median, 80%; range, 71% to 95%)
salt MTT is reduced to a colored formazan by living cells but not
than in nonhyperdiploid samples (median, 92%; range,71%
by dead cells. The formazan crystals formed were dissolved with
100 pL acidified isopropanol. The optical density of the wells, which to 99%). At the start of culture, these median percentages
is linearily related to the cell number," was measured with an ELwere both 94%.
312 microplate spectrophotometer (Bio-tek Instruments Inc. WinooThe hyperdiploid and nonhyperdiploidc-ALL samples
ski, VT) at 562 nm. Leukemic cell survival (LCS) was calculated
showed a large overlap of individual LC50 values for all
by the equation: LCS = (mean optical density treated wellslmean
drugs, except for 6MP. Hyperdiploid c-ALL samples were
optical density control wells) X 100%. The LC50, the drug concensignificantly more sensitive to 6MP (median, 9.0-fold; P =
tration lethal to 50% ofthe cells, wascalculatedfromthedose.00OOO3), to 6TG (1.4-fold; P = .023), to ARA-C (1.8-fold;
responsecurveandusedasmeasure
of resistance.Resultswere
P
= .016), and to ASP
(19.5-fold; P = .022) thanwere
considered evaluable in case of an optical density of
20.050 and
nonhyperdiploid c-ALL samples. Figure 1 shows these dif270% leukemic cells in the control wells (leukemic cells without
ferences for individual patients. In addition to these signifidrug), which assures reliable test result^.'"'^
cant differences, hyperdiploid c-ALL samples were not sigThe intra-assay (duplicates) and inter-assay (repeated testing
of a
frozen sample) variation in LC50 values is less than 1 dilution step
nificantly moresensitivetothe
structurallyrelated drugs
for each drug. The median coefficient
of variationofthecontrol
PRD (6.3-fold) andDXM (8.6-fold). Fortheremaining
wells was 5.2% (range, 0.9% to 15.3%).
drugs, small and nonsignificant differences were observed
DNA ploidy and S-phase deferminafion. Flow cytometric analy(Table 2). In some samples, not all drugs could be tested
sis of cellular DNA content and cell cycle distribution was performed because of the lack of material. However, 6MP and 6TG
withanimpulsecytophotometer
(ICP-11; Phywe AG, Gottingen,
were successfully tested in the same specimens. Moreover,
Germany)onethidiumbromide-stained
cells asdescribedprean analysis including only those samples in which all three
viously.* The DNA index was definedas the modal DNA content of
antimetabolites (6MP,6TG,andARA)were
successfully
leukemic cells compared with
that of reference normal lymphocytes.
tested gave results very similar to those shown in Table 2
Patientsweredividedinhyperdiploid(DNAindex,
2 1.16and
(data not shown).
c 1.35) and nonhyperdiploid (DNA index,
t1.16 or > l .35). We
From www.bloodjournal.org by guest on February 6, 2015. For personal use only.
DNAPLOIDYANDDRUG
A
753
RESISTANCE IN CHILDHOODALL
po.oooooa
t
=E
P
p.o.02
P
00
0"
l00
0
10
S
u-
t
C
DIPLOID
D
p-0.04
k
0
NON-HYPER
DIPLOID
DIPLOID
HYPER
NON-HYPER
DlpLOlD
0
8
0
HYPER
jP0.04
n
1
v
0
16
Y
0.01
1
W
O
+
i
P
8
00
Qx)
0.00 l
"
1
NON-HYPER
DIPLOID
HYPER
DIPLOID
N01J-HWER
DIPLOID
0
HYPER
DIPLOD
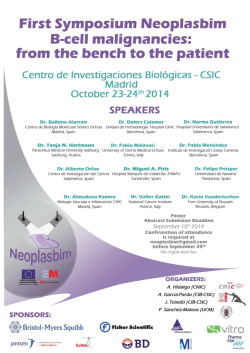
Fig l. Relationship betweenDNA ploidy determined byflow cytometry and cellular drug resistance determinedwith the colorimetric MlT
assay in childhood c-ALL. Cases were classified as hyperdiploid [DNAindex, 1.16 to 1.35) or nonhyperdiploid (DNAindex, <1.16 or >1.35). {A)
Mercaptopurine, (B) thioguanine, (C) cytarabine, and (D)L-asparaginase. (0)Individual and I+)median LC50 values.
The median percentage of S-phase cells was 8.5% in 13
hyperdiploid c-ALL samples (range, 4.2%to 20%)and 5.7%
(range, 0.2% to 30%)in the nonhyperdiploid c-ALL samples
( P = .OS; Fig 2). There was no significant correlation (all P
values >.20) between the percentage of S-phase cells and
LC50 values for PRD ( p .M), DXM ( p -.M), VCR ( p .15),
VDS ( p -.03), DNR ( p -.Ol), DOX ( p .12), MIT ( p .20),
TEN ( p .OS), ASP ( p -.lo), 6TG ( p -.05), and ARA-C ( p
- .06). Only for 6MP was a statistically borderline significant
correlation observed ( p -.30;P = .OS).
DISCUSSION
DNA hyperdiploidy is strongly and independently associated with a good prognosis in childhood ALL."" The reason
for this prognostic significance is largely unknown, but it
may be related to differences in cellular drug resistance.
Cellular drug resistance is one of the main determinants of
the clinical outcome after chemotherapy, together with the
pharmacokinetics of the administered drugsz0and with the
regrowth or relapse potential of minimal residual cells.21
Recently, Whitehead et all' reported that lymphoblasts of 13
children with hyperdiploid ALL accumulated higher levels
of methotrexate polyglutamates (MTXPG) than those in Blineage lymphoblasts of 34 children with other ploidy. The
investigators suggested that these high levels may increase
the cytotoxicity of MTX. Previously, the same investigators
had reported that children with B-lineage ALL, whose
lymphoblasts accumulated high levels of MTXPG in vitro,
had a better prognosis than did children with lower levels."
Otherwise, PinkelZ3reported in 1987 already that hyperdiploid c-ALL had a high cure rate with methotrexate and mercaptopurine.
To the best of our knowledge, the present study is the first
to report on a direct relation between DNA ploidy and cellular drug resistance in childhood ALL. Resistance to 12 drugs,
commonly used in the treatment of this disease, was investi-
From www.bloodjournal.org by guest on February 6, 2015. For personal use only.
754
KASPERS ET AL
Table 2. Relationship Between DNA Ploidy Determined by Flow
Cytometry and Cellular Drug Resistance Determined
With the Colorimetric MlT Assay in Untreated Childhood c-ALL
LC50 Values (WglrnL,
ASP IU/rnL)
Drug
PRD
DXM
VCR
VDS
DNR
DOX
MIT
TEN
ASP
6MP
6TG
ARA-C
DNA Ploidy
Median
Range
N
PValues
Nonhyperdiploid
Hyperdiploid
Nonhyperdiploid
Hyperdiploid
Nonhyperdiploid
Hyperdiploid
Nonhyperdiploid
Hyperdiploid
Nonhyperdiploid
Hyperdiploid
Nonhyperdiploid
Hyperdiploid
Nonhyperdiploid
Hyperdiploid
Nonhyperdiploid
Hyperdiploid
Nonhyperdiploid
Hyperdiploid
Nonhyperdiploid
Hyperdiploid
Nonhyperdiploid
Hyperdiploid
Nonhyperdiploid
Hyperdiploid
2.20
0.35
0.25
0.03
1.48
0.72
2.59
1.56
0.12
0.13
0.39
0.33
0.06
0.05
0.32
0.25
0.39
0.02
216.7
24.2
7.7
5.7
0.51
0.29
0.05-1500
0.05-134
0.003-6
0.0002-6
0.05-50
0.09-38.3
0.05-50
0.05-37.8
0.003-1.3
0.002-1.1
0.10-1.33
0.06-1.28
0.001-1.0
0.001-1.0
0.12-3.34
0.14-3.09
0.002-10
0.002-0.8
15.6-500
15.6-42.8
1.6-50
2.2-11.0
0.07-2.5
0.03-2.5
51
15
47
12
53
13
40
8
52
11
41
11
42
12
41
12
48
12
47
12
47
12
45
14
.l7
.09
.63
.35
.32
.34
.65
21
,022
.000003
,023
,016
Cases were classified as hyperdiploid ifthe DNA index was 1.16 to
1.35 and as nonhyperdiploid if the DNA index was <1.16 or >1.35.
gated in samples of 74 children with newly diagnosed cALL. Hyperdiploidy is found mainly in this immunophenotypic subgro~p.~".".*~
An analysis stratified for immunophenotype is also indicated because immunophenotype itself is
related to cellular drug resistance in childhood ALL.26MTX
was not included in the panel because this drug shows no
dose-dependent cytotoxicity in ALL patient samples in nonclonogenic cell culture drug resistance assays. A possible
explanation for this is described el~ewhere.'~
Hyperdiploid
c-ALL samples were more sensitive to all antimetabolites
tested (6MP, 6TG, and A M - C ) than were nonhyperdiploid
c-ALL samples. Hyperdiploid samples were also more sensitive to ASP. Resistance to each of the 8 other drugs did not
differ significantly between both ploidy groups. However, it
should be noted, that a limited number of samples has been
tested, especially in the hyperdiploid group. Some of the
nonsignificant differences might be clinically relevant and
need confirmation in a larger study.
The reason for the relative sensitivity of hyperdiploid cALL cells to antimetabolites is unknown. It has been attributed to a higher percentage of S-phase cells in hyperdiploid
than in nonhyperdiploid ALL.4 In the present study, the percentages of S-phase cells in the hyperdiploid c-ALL samples
were higher than those in the nonhyperdiploid c-ALL samples. However, in a limited number of samples (up to 38),
there was no significant and strong relation between the
percentage of S-phase cells and in vitro resistance to any of
the drugs tested.
It has been suggested that hyperdiploid ALL cells are
more sensitive to glucocorticoids, because of their tendency
towards terminal differentiation.' Both in vitro and in vivo
sensitivity to glucocorticoids is associated with a favorable
prognosis.'"28,29We found indeed that hyperdiploid c-ALL
samples were more sensitive to PRD (median, 6-fold) and
DXM (median, 9-fold) than were nonhyperdiploid samples.
However, the differences were not statistically significant.
The difference in resistance to ASP was significant, with
hyperdiploid c-ALL cells being a median of 19.5-fold more
sensitive. It seems of interest to study whether there are
differences in asparagine synthetase betweenhyperdiploid
and nonhyperdiploid c-ALL cells.
Hyperdiploid c-ALL samples were a median of 9.0-fold
more sensitive to 6MP, but were only 1.4-fold moresensitive
to 6TGthan were nonhyperdiploid c-ALL samples. This
discrepancy between 6MP and 6TG, two closely related thiopurines, is interesting. Both drugs are intracellularly metabolized into thioguanine nucleotides, which are subsequently
incorporated inDNAandRNA.
However, the conversion
of 6MP requires two enzymes more than the conversion of
6TG, namely inosinate (IMP) dehydrogenase and guanosylate synthetase. The rate-limiting enzyme is IMP dehydrogenase." In addition, both 6TG and 6MP are catabolized by
thiopurine methyltransferase, but this enzyme has a higher
affinity for 6MP." It is tempting to speculate that hyperdiploid and nonhyperdiploid c-ALL cells differ in the activity
of one or more of these enzymes. The favorable prognostic
value of hyperdiploidy is associated with nonrandom numerical chromosome gains, including chromosomes 4, 6, 10,
and 2 1 .',32,3' The genes encoding for the enzymes involved
in the intracellular metabolism of antimetabolites may localize to these chromosomes. However. an extensive literature
p=O.06
ao
0
¶6
Q
0'
-0
NON-HDROID
HYPeR
DlPLolo
Fig 2. Percentages of S-phase cells in hyperdiiloidand nonhyperdiploid childhood c-ALL samples. (0)Percentage of S-phase cells; ( + l
median value.
From www.bloodjournal.org by guest on February 6, 2015. For personal use only.
DNA PLOIDY AND DRUGRESISTANCE IN CHILDHOOD ALL
search did not show the chromosomal locations of the enzymes mentioned above.
One concern in our study is that the success rate of the
MTT assay was lower in hyperdiploid samples. Moreover,
the control cell survival and the percentage of leukemic cells
after 4 days of culture were lower in successfully tested
hyperdiploid samples than in nonhyperdiploid samples. This
finding is in agreement with preliminary results presented
by Campana et al,34 who reported that hyperdiploid ALL
cells were more likely to die in vitro, via induction of
apoptosis. Thus, it may be that hyperdiploid c-ALL samples
are actually even more drug sensitive than are nonhyperdiploid c-ALL samples than our study shows, because leukemic
cells that die spontaneously (not drug-induced) by apoptosis
may also be relatively sensitive to the cytotoxicity of anticancer agents. Most anticancer agents appear to kill malignant
cells by a p o p t ~ s i s . ~ ~
We conclude that hyperdiploid c-ALL samples are more
sensitive to antimetabolites (especially to 6MP) and to ASP
than are nonhyperdiploid c-ALL samples. This difference
may contribute to the more favorable prognosis associated
with DNA hyperdiploidy. The observation of other investigators that hyperdiploid ALL cells, compared to ALL cells
of other ploidy, accumulate higher levels of MTXPG and
therefore are likely to be more sensitive to MTX supports
the general conclusion that the prognostic significance of
DNA ploidy in childhood ALL is most likely to be mainly
explained by its relation with antimetabolite resistance.
ACKNOWLEDGMENT
Computer equipment was provided by Olivetti Nederland BV. The
laboratory of the Dutch Childhood Leukemia Study Group (DCLSG)
provided the patient samples. Board members of the DCLSG are H.
Van Den Berg, M.V.A. Bruin, J.P.M. Bokkerink, P.J. Van Dijken,
K. Hiihlen,W.A. Kamps, F.A.E. Nabben, A. Postma, J.A.Rammeloo, I.M. Risseeuw-Appel, A.Y.N. Schouten-Van Meeteren,
G.A.M. De Vaan, E. Th. Van’t Veer-Korthof, A.J.P. Veerman, M.
Van Weel-Sipman, and R.S. Weening.
REFERENCES
1. Hammond GD: Leukemia cell DNA content: Predictor of late
relapse in acute lymphoblastic leukemia. J Clin Oncol 9:1332, 1991
2. Pui C-H, Crist WM, Look A T Biology and clinical significance of cytogenetic abnormalities in childhood acute lymphoblastic
leukemia. Blood 76:1449, 1990
3. Jackson JF, Boyett J, Pullen J, Brock B, Patterson R, Land V,
Borowitz M, Head D, Crist W: Favorable prognosis associated with
hyperdiploidy in children with acute lymphocytic leukemia correlates with extra chromosome 6. A Pediatric Oncology Group study.
Cancer 66:1183, 1990
4. Look AT, Roberson PK, Williams DL, Rivera G , Bowman
WP, Pui C-H, Ochs J, Abromowitch M, Kalwinsky D, Dahl GV,
George S , Murphy SB: Prognostic importance of blast cell DNA
content in childhood acute lymphoblastic leukemia. Blood 65: 1079,
1985
5 . Pui C-H, Dodge RK, Look AT, George SL, Rivera GK, Abromowitch M, Ochs J, Evans WE, Crist WM, Simone JV: Risk of
adverse events in children completing treatment for acute lymphoblastic leukemia: St Jude Total Therapy Studies VIII, IX, and X. J
Clin Oncol 9:1341, 1991
6. Secker-Walker LM, Lawler SD, Hardisty RM: Prognostic im-
755
plications of choromosomal findings in acute lymphoblastic leukaemia at diagnosis. Br Med J 2:1529, 1978
7. Secker-Walker LM, Chessels JM, Stewart EL, Swansbury GJ,
Ricards A, Lawler SD: Chromosomes and other prognostic factors
in acute lymphoblastic leukaemia: A long-term follow-up. Br J
Haematol 72:336, 1989
8. Smets LA, Homan-Blok, Hart A, De Vaan G , Behrendt H,
H&len K, De Waal FC: Prognostic implication of hyperdiploidy as
based on DNAflow cytometric measurement in childhood acute
lymphocytic leukemia-A multicenter study. Leukemia 1:163,1987
9. Trueworthy R, Shuster J, Look T, Crist W, Borowitz M, Carroll
A, Frankel L, Harris M, Wagner H, Haggard M, Mosijczuk A,
Steuber P, Land V: Ploidy of lymphoblasts is the strongest predictor
of treatment outcome in B-progenitor cell acute lymphoblastic leukemia of childhood: A Pediatric Oncology Group study. J Clin Oncol
10:606, 1992
10. Williams DL, Tsaiatis A, Brodeur GM, Look AT, Melvin
SL, Bowman WP, Kalwinsky DK, Rivera G, Dahl GV: Prognostic
importance of chromosome number in 136 untreated children with
acute lymphoblastic leukemia. Blood 60:864,1982
11. Whitehead VM, Vuchich MJ, Lauer SJ, Mahoney D, Carroll
AJ, Shuster JJ, Esseltine DW, Payment C, Look AT,Akabutu J,
Bowen T, Taylor LD, Camitta B, Pullen DJ: Accumulation of high
levels of methotrexate polyglutamates in lymphoblasts from children
with hyperdiploid (>SO chromosomes) B-Lineage acute lymphoblastic leukemia: A Pediatric Oncology Group study. Blood 801316,
1992
12. Veerman AJP, Pieters R: Drug sensitivity assays in leukaemia
and lymphoma. Br J Haematol 74:381, 1990
13. Pieters R, Huismans DR, Loonen AH, Hiihlen K, Van Der
Does-Van Den Berg A, Van Wering ER, Veerman AJP: Relation
of cellular drug resistance to long term clinical outcome in childhood
acute lymphoblastic leukaemia. Lancet 338:399, 1991
14. Bennett JM, Catovsky D, Daniel MT, Flandrin G, Galton
DAG, Gralnick HR. Sultan C: The morphological classification of
acute lymphoblastic leukaemia: Concordance among observers and
clinical correlations. Br J Haematol 47:553, 1981
15. Van Wering ER, Brederoo P, Van Staalduinen GI. Van Der
Meulen J, Van Der Linden-Schrever BEM, Van Dongen JJM: Contribution of electron microscopy to the classification of minimally
differentiated acute leukemias in children. Recent Results Cancer
Res 131:77, 1993
16. Kaspers GJL, Pieters R, Van Zantwijk CH, De Laat PAJM,
De Waal FC, Van Wering ER, Veerman AJP In vitro drug sensitivity
of normal peripheral blood lymphocytes and childhood leukaemic
cells from bone marrow and peripheral blood. Br J Cancer 64:469,
1991
17. Pieters R, Huismans DR, Leyva A, Veerman AJP: Comparison of the rapid automated MTT-assay with a dye exclusion assay
for chemosensitivity testing in childhood leukemia. Br J Cancer
59:217, 1989
18. Pieters R, Huismans DR. Leyva A, Veerman AJP: Adaptation
of the rapid automated tetrazolium dye based MTT assay for chemosensitivity testing in childhood leukemia. Cancer Lett 41:323, 1988
19. Kaspers GJL, Veerman AJP, Pieters R, Broekema GJ, Huismans DR, Kazemier KM, Loonen AH, Rottier MAA, Van Zantwijk
CH, Hiihlen K, Van Wering ER: Mononuclear cells contaminating
acute lymphoblastic leukaemic samples tested for cellular drug resistance using the methyl-thiazol-tetrazolium assay. Br J Cancer 1994
(in press)
20. Evans WE, Petros W,Relling MV, Crom WR, Madden
T, Rodman JH, Sunderland M: Clinical pharmacology of cancer
chemotherapy in children. Pediatr Clin North Am 36: 1199, 1989
21. Preisler HD, Raza A, Larson R, Goldberg J, Tricot G, Carey
M, Kukla C: Some reasons for the lack of progress in the treatment
From www.bloodjournal.org by guest on February 6, 2015. For personal use only.
756
of acute myelogenous leukemia: A review of three consecutive trials
of the treatment of poor prognosis patients. Leuk Res 15:773, 1991
22. Whitehead VM, Rosenblatt DS, VuchichM-J, Shuster JJ,
Witte A, Beaulieu D: Accumulation of methotrexate and methotrexate polyglutamates in lymphoblasts at diagnosis of childhood acute
lymphoblastic leukemia: A pilot prognostic factor analysis. Blood
7644, 1990
23. Pinkel D:Curing children of leukemia. Cancer 59:1683, 1987
24. Look AT, Melvin SL, Williams DL, Brodeur GM, Dah1 GV,
Kalwinsky DK, Murphy SB, Mauer AM: Aneuploidy and percentage
of S-phase cells determined byflow cytometry correlate with cell
phenotype in childhood acute leukemia. Blood 60:959, 1982
25. Pui C-H, Williams DL, Roberson PK, Raimondi SC, Behm
FG, Lewis SH, Rivera GK, Kalwinsky DK, Abromowitch M, Crist
WM. Murphy SB: Correlation of karyotype and immunophenotype
in childhood acute lymphoblastic leukemia. J Clin Oncol 6:56, 1988
26. Pieters R, Kaspers GJL, Van Wering ER, Huismans DR,
Loonen AH, H2hlen K, Veerman AJP: Cellular drug resistance profiles that might explain the prognostic value of immunophenotype,
age and sex in childhood acute lymphoblastic leukemia. Leukemia
7:392, 1993
27. Pieters R, Loonen AH, Huismans DR, Broekema GJ, Dirven
MWJ, Heyenbrok MW, HMen K, Veerman AJP: In vitro sensitivity
of cells from children with leukemia using the MTT assay with
improved culture conditions. Blood 76:2327, 1990
28. Kaspers GJL, Pieters R, Van Zantwijk CH, Van Wering ER,
Van Der Does-Van Den Berg A, Veerman AJP: Resistance to prednisolone (PRD) in vitro: A new prognostic factor in childhood acute
KASPERS ET AL
lymphoblastic leukemia (ALL) at initial diagnosis. Proc Am SOC
Clin Oncol 12:320, 1993 (abstr)
29. Riehm H, Reiter A, Schrappe M, Berthold F, Dopfer R, Gerein V, Ludwig R, Ritter J, Stollmann B, Heme G: Die CorticosteroidAbhangige Dezimierung der Leukamiezellzahl im Blut als Prognosefaktor bei der Akuten Lymphoblastischen Leukamie im
Kindesalter (Therapiestudie ALL-BFM 83). Klin Padiatr 199:151,
I986
30. Weber G: Biochemical strategy of cancer cells and the design
of chemotherapy: G.H.A. Clowes Memorial Lecture. Cancer Res
43:3466, 1983
3 1. Woodson LC, Weinshilboum RM: Human kidney thiopurine
methyltransferase purification and biochemical properties. Biochem
Pharmacol 32:819, 1983
32. Hams MB, Shuster JJ, Carroll A, Look AT, Borowitz MJ,
Crist WM, Nitschke R, Pullen J, Steuber CP, Land VJ: Trisomy of
leukemic cell chromosomes 4 and IO identifies children withBprogenitor cell acute lymphoblastic leukemia with a very low risk
of treatment failure: A Pediatric Oncology Group study. Blood
79:3316, 1992
33. Smets LA, Slater RM, Behrendt H, Van 'T Veer MB, HomanBlok J: Phenotypic and karyotypic properties of hyperdiploid acute
lymphoblastic leukaemia of childhood. Br J Haematol 61:l 13, 1985
34. Campana D, Kumagai M, Manabe A, Murti KG, Behm FG,
Mahmoud H, Raimondi SC: Hyperdiploid acute lymphoblastic leukemia (ALL): A distinct biological entity with marked propensity
to programmed cell death. Blood 82:49a, 1993 (abstr, suppl I )
35. Hickman JA: Apoptosis induced by anticancer drugs. Cancer
Metastasis Rev 1 l:121, 1992
From www.bloodjournal.org by guest on February 6, 2015. For personal use only.
1995 85: 751-756
Favorable prognosis of hyperdiploid common acute lymphoblastic
leukemia may be explained by sensitivity to antimetabolites and other
drugs: results of an in vitro study
GJ Kaspers, LA Smets, R Pieters, CH Van Zantwijk, ER Van Wering and AJ Veerman
Updated information and services can be found at:
http://www.bloodjournal.org/content/85/3/751.full.html
Articles on similar topics can be found in the following Blood collections
Information about reproducing this article in parts or in its entirety may be found online at:
http://www.bloodjournal.org/site/misc/rights.xhtml#repub_requests
Information about ordering reprints may be found online at:
http://www.bloodjournal.org/site/misc/rights.xhtml#reprints
Information about subscriptions and ASH membership may be found online at:
http://www.bloodjournal.org/site/subscriptions/index.xhtml
Blood (print ISSN 0006-4971, online ISSN 1528-0020), is published weekly by the American
Society of Hematology, 2021 L St, NW, Suite 900, Washington DC 20036.
Copyright 2011 by The American Society of Hematology; all rights reserved.
© Copyright 2026