Hematopoietic Growth Factors for Graft Failure After Bone
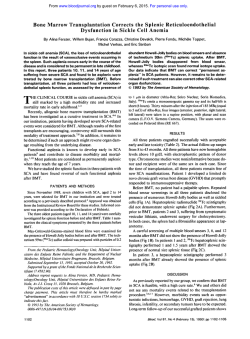
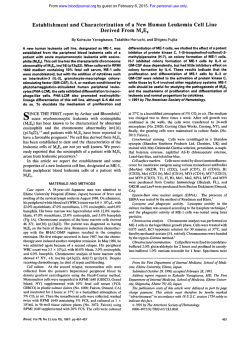
From www.bloodjournal.org by guest on February 6, 2015. For personal use only. Hematopoietic Growth Factors for Graft Failure After Bone Marrow Transplantation: A Randomized Trial of Granulocyte-Macrophage Colony-Stimulating Factor (GM-CSF) Versus Sequential GM-CSF Plus Granulocyte-CSF By Daniel J. Weisdorf, Catherine M. Verfaillie, Stella M. Davies, Alexandra H. Filipovich, John E. Wagner Jr, Jeffrey S. Miller, Jory Burroughs, Norma K.C. Ramsay, John H. Kersey, Philip B. McGlave, and Bruce R. Blazar Delay in hematologic recovery after bone marrow transplantation (BMT) can extend and amplify therisks of infection and hemorrhage, compromise patients' survival, and increase the duration and cost of hospitalization. Because current studies suggest that granulocyte-macrophage (GM) colony-stimulating factor (CSF) may potentiate the sensitivity ofhematopoietic progenitor cells t o G-CSF, we performed a prospective, randomized trial comparing GM-CSF (250 pg/m2/d x 14 days) versus sequential GM-CSF x 7 days followed by G-CSF (5 pg/kg/d x 7 days) as treatment for primary orsecondary graft failure afterBMT. Eligibility criteria included failure t o achieve a white bloodcell (WBC) count =lOO/pL by day +21 or r3OOlpL by day +28, no absolute neutrophil count (ANC) =2OO/pL by day +28, or secondary sustained neutropenia afterinitial engraftment. Forty-seven patients were enrolled: 23 received GM-CSF ( I O unrelated, 8 related allogeneic, and 5 autologous), and 24 received GMCSF followed by G-CSF (12 unrelated, 7 related allogeneic, and 5 autologous). For patients receiving GM-CSF alone, neutrophil recovery (ANC =500/pL) occurred between 2 and 61 days (median, 8 days) after therapy, while thosereceiving GM-CSF + G-CSF recovered at a similar rate of 1 t o 36 days (median, 6 days; P = .39). Recovery t o red blood cell (RBC) transfusion independence was slow, occurring 6 t o 250 days (median, 35 days) after enrollmentwithno significant difference between thet w o treatment groups (GM-CSF: median, 30 days; GM-CSF + G-CSF; median, 42 days; P = .24). Similarly, platelet transfusion independence was delayed until 4 t o 249 days (median, 32 days) after enrollment, with no difference between thetwo treatment groups (GM-CSF: median, 28 days; GM-CSF + G-CSF: median, 42 days; P = .38). Recovery times were not different between patients with unrelated donors andthose withrelated donors or autologous transplant recipients. Survival at 100 days after enrollmentwas superior after treatment with GM-CSF alone. Only 1of 23 patients treatedwith GM-CSF died versus 7 of 24 treated with GM-CSF + G-CSF who died 16 to 84 days (median, 38 days) after enrollment, yielding KaplanMeier 100-day survival estimates of 96% k 8% for GM-CSF versus 71% k 18% for GM-CSF + G-CSF ( P = ,026). These data suggest that sequential growth factor therapy with GM-CSF followed by G-CSF offers no advantage over GMCSF alone in accelerating trilineage hematopoiesis or preventinglethal complications in patients with poorgraft function after BMT. GM-CSF should still be considered the standard for graftfailure against which other, newer growth factors, sequential treatments, or combinationtherapies are tested. 0 1995 by The American Society of Hematology. I tion of their effectiveness in promoting engraftment after BMT.4"0 Onlylimited data are available assessing their value in accelerating recovery and improving survival for patients with delayed or poorly functioning grafts after transplantation.""' Preclinical data suggest that early-acting growth factors suchas GM-CSF, interleukin (IL)-3, or stem cell factor might increase the responsiveness of committed hematopoietic progenitors to later-acting factors such as G-CSF or erythropoietin."-**To evaluate the clinical value of this type of sequential growth factor therapy, we performed a formal, prospective, randomized, comparative trial of GM-CSF alone versus GM-CSF followed by G-CSF for stimulating hematologic recovery in patients with primary or secondary graft failure after BMT. This report describes the hematologic and clinical outcomes of this comparative trial. N THE EARLY pancytopenic period after bone marrow transplantation (BMT), infection, and hemorrhage are the major morbidand life-threatening complications observed.' Any delay in hematopoietic recoverycan extend and exaggerate this period of risk.*,' Poor graft function or secondary graft failure leading to secondary neutropenia may also increase these hazards and compromise patient survival. Delayed hematologic recoveryis a primary factor in extending hospitalization and markedly increasing the cost of BMT therapy. The availability of granulocyte macrophage colony-stimulating factor (GM-CSF) and granulocyte colony-stimulating factor (G-CSF) as licensed products for use in stimulating hematopoietic function has allowed investigaFrom the Departments of Medicine, Pediatrics, Laboratory Medicine, and Pathology and the Bone Marrow Transplantation Program, University of Minnesota, Minneapolis, MN. Submitted November 14, 1994; accepted January 31, 1995. Supported in part by a grant from the National Cancer Institute ( N U : CA21737). B.R.B. is a recipient of the Edward Mallinckrodt Jr Scholar Award, and J.H.K. is arecipient of an Outstanding Investigator Award (CA49721) fromthe NCI. Addresscorrespondenceto Daniel J. WeisdoffMD, Box 480, University of Minnesota Hospital, 420 DelawareSt SE, Minneapolis, MN 55455. The publication costsof this article were defrayedin part by page chargepayment. This article must therefore be hereby marked "advertisement" in accordance with 18 U.S.C. section 1734 solely to indicate this fact. 0 I995 by The American Society of Hematology. 0006-4971/95/85I2-0013$3.00/0 3452 PATIENTS AND METHODS All patients with graft failure after BMT at the University of Minnesota (Minneapolis, MN) were eligible for this trial. Patients had received either autologous bone marrow or peripheral blood stem cells or were allogeneic transplant recipients (from either related or unrelated donors). Patients were eligible for enrollment if they met the following definitions of graft failure: (1) failure to achieve a leukocyte count of >100/pL by day +21 after transplantation, (2) failure to achieve a leukocyte count 2300/pL or an absolute neutrophil count (ANC) 2200/pL by day + 28; or (3) failure to maintain a mean ANC 2500/pL for 7 days after having previously achieved an ANC =-5OO/pL at any time beyond day +28 (secondary neutropenia). Patients receiving recombinant cytokines under different study protocols at the University of Minnesota (including a trial of Blood, Vol 85, No 12 (June 15), 1995: pp 3452-3456 From www.bloodjournal.org by guest on February 6, 2015. For personal use only. 3453 GROWTH FACTORS FOR GRAFT FAILURE AFTER BMT Table 1. Patient Characteristics recombinant IL-laZ3and a trial of recombinant ~ 2 were ’ excluded ~ until day +28, after which time they could be enrolled still if eligible GM-CSF x 7 days GM-CSF becauseofgraft failure. Patients undergoing allogeneic BMT for + G-CSF x 7 days X 14 days severe combined immunodeficiency (SCID) or familial erythropha23 24 N gocyticlymphohistiocytosis (FEL), thosereceivinggranulocyte 32; 3-51 37; 4-51 Median age; range (yr) transfusions, and those undergoing autologousBMT for acute non14:9 17:l lymphocytic leukemia (ANLL) and treated under Children’s Cancer Sex (M:F) Type of transplant Group studies that specifically excluded cytokine use were ineligible. 7 8 Allogeneic related During the study period, seven eligible patients were not enrolled 10 12 Unrelated donor due to patient refusal (n = 3), attending physician preference (n = 5 5 Autologous 3). and prior adverse reaction to GM-CSF (n = 1). Diagnosis Eligible, consenting patients were assigned to receive either GM4 Acute leukemia 9 CSF (250 pg/m2/d over 2 hours intravenously X 14 days) or GM14 Chronic myelogenous leukemia 5 CSF (250 pg/m’/d over 2 hours intravenously X 7 days) followed 4 Other malignancy+ 6 immediately by G-CSF (5 pg/kg/d intravenously over 15 minutes 2 Nonmalianantt 3 x 7 days). This prospective, randomized enrollment was stratified Includes non-Hodgkin‘s lymphoma (n = 6). myelodysplastic synintogroupsof either unrelated donor marrow recipients or other dromes (n = 3). and neuroblastoma (n = 1). recipients that included recipientsof either related donor allogeneic or autologous transplantation. All patients except one were enrolled t Includes aplastic anemia (n = 4) and hypereosinophilic syndrome (n = 1). for treatment for primary graft failure. The primary endpoint for response to cytokine therapy was the development of a sustained ANC 2500/pL for 3 consecutive days. Secondary endpoints included recoveryof red cells and platelets to treated with GM-CSF alone and those treated with GM-CSF transfusion-independence, adverse reactions to cytokine infusions, + G-CSF (P = .39; Table 2). The neutrophil recovery times and 100-day survival. Patients not responding to the first 14 days were similar in the two patient strata: those receiving unreof therapy were eligible for retreatment, as previously assigned, for lated donor BMT (median, 8 days; range, 1 to 61 days) and a secondfullcourse. Ifgraft failure wasrefractorytotreatment, some patients subsequently received reinfusion of donor or back-up those receiving related donor or autologous BMT (median, 8 days; range, 2 to 36 days; P = .78). After 14 days, 75% autologous ma~row.’~ Inadditiontotheseretransplantedpatients, t 18% (95% confidence interval) of those treated with GMfive others (three in the GM-CSF a r m ; two in the GM-CSF + GCSF alone achieved neutrophil recovery compared with 79% CSF m ) continued their assigned growth factors beyond 14 days. The trial was performed using the commercially available products+. 16% of thosereceivingGM-CSF G-CSF ( P > S ) . (GM-CSF Immunex Corp, Seattle,WA; and G-CSF: Amgen, Thou- Recovery to red cell transfusion-independence was delayed sand Oaks, CA) withno external funding from the manufacturers. but occurred between 6 and 250 days after enrollment (meThe study protocol was reviewed and approved by the University dian, 35 days). There was no difference between the two of Minnesota Institutional Review Board: Human Subjects Committreatment arms (P = .24). Recovery to platelet transfusiontee, and all patients(or their parents) gave written informed consent. independence was also delayed and occurredbetween 4 and Statistical analysis. Times to hematologic recovery and survival 35 days), but the two 249 days after enrollment (median, were evaluated by Kaplan-Meier calculations, and differences betreatment arms were similarly effective ( P = .38; Fig 1). tween groups werecomparedusingtheMantel-Coxtest statistic. Survival. We next evaluated survival over the first 100 Short-term survival was evaluated censoringall patients at 100 days days after enrollment. We observed a statistically significant after enrollment. Comparisonsof patient characteristics betweenthe two study groups were performed using a x’ statistic. All analyses advantage ( P = .026) favoring GM alone versus GM-CSF were performed by intention-to-treat according to the randomized + G-CSF. Only 1 of 23 GM-CSF patients died(at day +34) assignment. after enrollment versus 7 of 24 GM-CSF G-CSF patients who died between days 16 and 84 (median, 38 days) after RESULTS enrollment (Fig2). The primary and secondary causes of Of 472 BMT procedures performed at the University of death in all eight patients who died were directly related to Minnesota between January 1992 and March 1994, 47 pagraft failure, including hemorrhage and infection in six of tients metthe criteria for entry, consented, and were enrolled eight patients (Table 3). Of the patients who died, the one in this randomized trial. Theirclinical characteristics are receiving GM-CSF alone had undergone an allogeneic reshowninTable 1. The groupsincluded 15 related-donor lated-donor transplant, while the seven GM-CSF + G-CSF allogeneic transplant recipients (of 167 transplanted within deaths occurred in one of five autologous and two of seven the same time interval); 22 unrelated-donorrecipients (of related-donor allogeneic transplants and 4 of 12 unrelated recipients (of 174 trans131 transplanted), and 10 autologous donor transplants. Deaths attributable to infection occurred planted). Of the 47 patients, 23 received GM-CSF for 14 20 to 84 days after study entry and cannot be ascribed to days, and 24 received GM-CSF for 7 days followed by Gdifferences in active infections at study entry. CSF for 7 days. Forty (85%) recovered (ANC 250O/pL) Adverse reactions and compliance with therapy. For all between 1 and 61 days after initiation of cytokine therapy 47 patients enrolled on the trial, we assessed completeness (median, 8 days). Seven patients were censored from analyof therapy and adverse reactions to treatment. Because treatsis at the time of reinfusion of supplemental marrow (three ment on both study arms was the same for the first 7 days recipients of allogeneic related donor and fourunrelated dooftherapy and the therapeuticinterventionsdiffered only nor marrow). between days 8 and 14 of treatment, we evaluated the 2 There were similar rates of neutrophil recovery in those weeks separately. Overall, 43 of 47 patients received at least + + From www.bloodjournal.org by guest on February 6, 2015. For personal use only. 3454 WEISDORF ET AL Table 2. Hematology Recovery After Cytokine Therapy for Graft Failure ~~~ ~~~~ - Median Time to Recovery; Range (d) GM-CSF + G-CSF GM-CSF x 14 days (N = 23) (N = 24) P ANC 2 500/pL .391-36 6; 8; 2-61 RBC transfusion-independence (first of 30+ d) 30; 6-12442;11-250.24 Platelet transfusion-independence (first of 15+ d) 28;6-127 42; 4-249 .38 ~~ ~~~ P values represent Mantel-Cox tests ~ of significance between the two groups. five of the seven planned doses of GM-CSF during the first treatment week, 19 of 23 received at least five of the seven randomly assigned GM-CSF doses, and 20 of the 24 received at least five of the planned seven G-CSF doses.Of those 10 patients who received less than the scheduled therapy, eight were stopped according to protocol because neutrophil recovery made cytokine therapy no longer necessary. No significant adverse reactions (eg, fevers, rash,serositis, bone pain) led to discontinuationof either GM-CSF or G-CSFon either treatment a r m . Graft-versus-host disease (GVHD)was similarly frequent in both treatment arms. Fourteen of the 18 allogeneic transplant recipientsreceiving GM-CSF and16 of 19 receiving GM-CSF G-CSF developed acute GVHD. + DISCUSSION Bone marrow graft failure or poor hematologic function after BMT is frequent, can contribute to greater post-BMT mortality, and often complicates and prolongs hospitaliza- tion,thusincreasingtreatment costs.'.' in a retrospective evaluation of delayed engraftment at ourinstitution that preceded initiation of this trial, of S91 patientstransplanted, 196 (33%) had not achieved an ANC ?SOO/yL by 28 days after BMT. Thisone-third rate of delayed hematologic recovery(defined by alessstringentendpoint than that of the current study) was similar in all three cohorts (autologous, related-donor, and unrelated-donor BMT) before hematopoietic growth factors were available as therapeutic tools. However, we also observed that 6-month survival was equivalent for those with or without neutrophil recovery to zS00/pL by day 28 (70% v 62%, respectively; P = . l 8). although hospitalstay was oftenprolongedsecondary to persisting neutropenia. With that institutional background data available,we initiatedthe current trial in which we evaluated sequentialtherapy of GM-CSF followed by G-CSF cornpared with GM-CSF alone to reduce the early morbidity and improve survival for patients with graft failure. Numerous reportssuggestthatseveralhematopoietic growth factors, including GM-CSF,G-CSF, 1L-la, 1L-3, and some growth factor combinations can accelerate engraftment whenusedimmediatelyafter BMT""".'X.''.27.'h.'7 although data demonstrating improvements insurvivalafter growth factor administration are limited. In contrast,onlya few reports describe the use of growth factors for treatment of delayed hematologic recovery or secondary graft failure. For example, Nemunaitis et all' first reported that 21 of 37 patients responded to GM-CSF administered for graft failure and suggested superior 100-day and l-year survival rates in the GM-CSF-treated patients compared withinstitutional historical controls. Similar results with growth factortherapy for delayed engraftment have been reported by others using either GM-CSF or G-CSF,'2"4 butno conclusive data are available comparing GM-CSF to G-CSF for acceleration of 1o .- RBC Recovery p=o2, 0.0 0 20 40 0.8 80 1W 120 140 160 GYCSftGCBF 1.o, 0.2 60 i 0.6 0.0 0 1 0 2 0 3 0 4 0 s o e o r n Days post treatment Platelet Recovery .~ p ;03 0.0 0 20 BO 80 100 120 ~ a y post s treatment 40 140 I 160 Fig 1. Shown are the hematologic recovery rates [time to ANC =500/1.~L;to red blood cell [RBC) independence, and to platelet independence) for graft failure patients treated with GMCSF x 14 days In = 23) or GMCSF x 7 davs followed bv G-CSF x 7 days In = 24). From www.bloodjournal.org by guest on February 6, 2015. For personal use only. GROWTHFACTORSFORGRAFT 3455 FAILURE AFTER B M 1 hematologic recovery after t r a n s p l a n t a t i ~ n . ~Therefore, ~~'~~~ we initiated the comparative trial reported herein. Current understanding of the physiologic maturation of hematopoietic cells suggests that GM-CSF-primed progenitors may be more susceptible to secondary stimulation with G-CSF. In addition to the early reports and Food and Drug Administration-licensed indications for the use of GM-CSF for graft failure, we reasoned that the known endogenous high circulating levels of G-CSF (but not GM-CSF) in the plasma accompanying post-BMT n e u t r ~ p e n i a *and ~ - ~the ~ sequential and potentially synergistic role these two factors have in stimulating hematopoietic differentiation and proliferation suggested that GM-CSF as primary therapy followed by G-CSF might effect superior recovery and reduce the morbidity and mortality associated with delayed engraftment. Somewhat disappointingly, within this trialboth treatments produced similar rates of trilineage hematologic recovery after initial graft failure. Compared with GM-CSF alone, sequential therapy with GM-CSF followed by G-CSF was of no advantage in stimulating more rapid or more frequent neutrophil recovery, while red cell and platelet transfusion-dependence persisted for a median of 5 weeks after enrollment. The observation that this delayed erythrocyte and platelet transfusion-dependence persisted for many weeks in many patients indicates that additional measures are needed beyond either single or sequential growth factor therapy to satisfactorily promote trilineage hematologic recovery in those with initially poor graft function. Importantly, a significant difference in 100-day survival was observed favoring GM-CSF alone as compared with sequential therapy with GM-CSF + G-CSF. The primary and secondary causes of death were related to graft failure in all patients and can in no way be attributed to treatment with G-CSF during the second therapeutic week, and we can offer no sound explanation for this observed difference. However, there were no findings observed in this trial that favored changing growth factor treatment to G-CSF after the first week of GM-CSF. Because neither hematologic recov- Table 3. Causes of Death Within 100 Days After Cvtokine Theraov for Graft Failure Day of Death PostEnrollment (days post-BMT) Primary; Secondary Causes of Death GM-CSF x 14 days 34 (54) GM-CSF + G-CSF 16 (37) 20 (46) 26 (47) 3% (59) 39 (61) 70 (90) 84 (140) Multisystem organ failure Pulmonan/ hemorrhage; hepato-renal failure, GVHD Cytomegalovirus pneumonitis Sepsis (Pseudomonas aeruginosa) Sepsis (Staphylococcus; Candida glabrata) Liver failure; DIC, GI bleeding, GVHD Multisystem organ failure Aspergillosis; GVHD All patients also had delayed engraftment as a contributing cause of death. Abbreviations: DIC, disseminated intravascular coagulation; GI, gastrointestinal. ery of red cells, neutrophils, or platelets nor survival favored GM-CSF + G-CSF, this sequential cytokine therapy cannot be accepted as advantageous, at least in this dose and schedule. GM-CSF treatment for delayed engraftment should remain the standard against which other, newer growth factors, sequential treatments, or combination therapies are tested. Finally, it must be remembered that in addition to hematopoieticgrowthfactorsthatshould be initiatedpromptlyif engraftment delay is suspected or observed, strong consideration must be given to second marrow infusion if engraftment delay persists. In the current report,80%+ of all patients who eventually respondedwithsatisfactoryneutrophilrecoverydid so within 21 days of growth factor therapy (usually by day +42 post-BMT). We have previously reported that second infusions of bone marrow after graft failure have led to successful engraftment in over half of patients, and24%of reinfused patients survive at 1 year.25Althoughstilldisappointing,these data show the demonstrable value of second marrow infusion as a legitimate therapeutic intervention when recombinant cytokine therapy is unsuccessful. REFERENCES g 0.41 0 10 20 30 40 50 60 70 80 90 100 Days post treatment Fig 2. Shown are 100-day survivalrates after cytokine therapy for graft failure with GM-CSF alone or GM-CSF followed by G-CSF (P= ,026). 1. Wingard JR: Advances in the management of infectious complications after bone marrow transplantation. Bone Marrow Transplant 6:371, 1990 2. Davies SM, Ramsay NKC, H a k e RJ, Kersey JH, Weisdorf DJ, McGlave PW, Blazar BR: Comparison of engraftment in recipients of matched sibling or unrelated donor marrow allografts. Bone Marrow Transplant 13:51, 1994 3. Chaplin RE, Horowitz MM, van Bekkum DW, Camitta BM, Elfenbein GE, Gale RP, Gluckman E, Good RA, Rimm AA,Rozman C, Speck B, Bortin MM: Graft failure following bone marrow transplantation for severe aplastic anemia: Risk factors and treatment results. Blood 73:606, 1989 4. Sheridan WP, Morstyn G, Wolf M, Lusk J, Layton JE, Souza L, Morstyn G, Dodd A, Maher D, Green MD, Fox RM: Granulocyte colony-stimulating factor and neutrophil recovery after high-dose chemotherapy and autologous bone marrow transplantation. Lancet 1:891, 1989 5. Lazarus HM, Andersen J, Chen MG, Variakojis D, Mansour From www.bloodjournal.org by guest on February 6, 2015. For personal use only. 3456 EG, Oette D, Arce CA, Oken MM, Gerson SL: Recombinant granulocyte-macrophage colony-stimulating factor after autologous bone marrow transplantation for relapsed non-Hodgkin’s lymphoma: Blood and bone marrow progenitor growth studies. A phase I1 Eastem Cooperative Oncology Group trial. Blood 78:830, 1991 6. Gorin NC, Coiffier B, Hayat M, Fouillard L, Kuentz M, Flesch M, Colombat P, Boivin P, Slavin S, Philip T: Recombinant human granulocyte-macrophage colony-stimulating factor after high-dose chemotherapy and autologous bone marrow transplantation with unpurged and purged marrow in non-Hodgkin’s lymphoma: A doubleblind placebo-controlled trial. Blood 80:1149, 1992 7. Peters WP, Rosner G, Ross M, Vredenburgh J, Meisenberg B, Gilbert C, Kurtzberg J: Comparative effects of granulocyte-macrophage colony-stimulating factor (GM-CSF) and granulocyte colonystimulating factor (G-CSF) on priming peripheral blood progenitor cells for use with autologous bone marrow after high-dose chemotherapy. Blood 81: 1709, 1993 8. Schriber JR, Negrin RS, Chao NJ,Long GD, Homing SJ, BlumeKG: The efficacy of granulocyte colony-stimulating factor following autologous bonemarrow transplantation for non-Hodgkin’s lymphoma with monoclonal antibody purgedbone marrow. Leukemia 7: l49 I , 1993 9. Nemunaitis J, Rabinowe SN, Singer JW, Bierman P, Vose JM, Freedman AS, Onetto N, Gillis S, Oette D, Gold M, Buckner CD, Hansen JA, Ritz J, Appelhaum FR, Armitage JO, Nadler LM: Recombinant granulocyte-macrophage colony-stimulating factor after autologous bone marrow transplantation for lymphoid cancer. N Engl J Med 324:1773, 1991 IO. Khwaja A, Mills W, Leveridge K, Goldstone AH, Linch DC: Efficacy of delayed granulocyte colony-stimulating factor after autologous BMT. Bone Marrow Transplant 11:479, 1993 11. Nemunaitis J, Singer JW, Buckner CD, Dumam D, Epstein C, Hill R, Storb R, Thomas ED, Appelbaum FR:Use of recombinant human granulocyte-macrophage colony-stimulating factor in graft failure after bone marrow transplantation. Blood 76:245, 1990 12. Ippoliti C, Przepiorka D, Giralt S, Anderson BS, Wallerstein RO, Gutterman J, Deisseroth AB, Champlin RE: Low-dose nonglycosylated rhGM-CSF is effective for the treatment of delayed hematopoietic recovery after autologous marrow or peripheral blood stem cell transplantation. Bone Marrow Transplant 11:55, 1993 13. Vose JM, Bierman PJ, Kessinger A, Coccia PF, Anderson J, Oldham FB, Epstein C, Armitage JO: The use of recombinant human granulocyte-macrophage colony stimulating factor for the treatment of delayed engraftment following high dose therapy and autologous hematopoietic stem cell transplantation for lymphoid malignancies. Bone Marrow Transplant 7: 139, 1991 14. Sierra J, Terol MJ, Urbano-Ispizua A, Rovira M, Marin P, Carreras E, Batle M, Rozman C: Different response to recombinant human granulocyte-macrophage colony-stimulating factor in primary and secondary graft failure after bone marrow transplantation. Exp Hematol 22566, 1994 15. Broxmeyer HE, Benninger L, Shreyaskumar RP, Benjamin myeloid RS, Vadhan-Raj S: Kinetic response ofhumanmarrow progenitor cells toin vivo treatment of patients with granulocyte colony-stimulating factor is different from the response to treatment with granulocyte-macrophage colony-stimulating factor. Exp Hemato1 22: 100, 1994 16. Boulad F, Gillio A, Small TN, Bonilla MA, Philips P, Ruggiero M, Emanuel D, Ghavimi F, Kernan NA: Correction of neutropenia with rHuG-CSF after loss of response to rHuGM-CSF following autologous bone marrow transplant. Bone Marrow Transplant 13:661, 1994 WEISDORF ET AL 17. Crump M, Couture F, KovacsM, Saragosa R, McCrae J , Brandwein J, Huebsch L, Beauregard-Zollinger L, Keating A: Interleukin-3 followed by GM-CSF for delayed engraftment after autologous bone marrow transplantation. Exp Hematol 2 1 :405, 1993 18. Fay JW, Lazarus H, Herzig R, Saez R, Stevens DA, Collins RH Jr, Piiieiro LA,Cooper BW, DiCesare J, Campion M. Felser JM, Herzig G, Bernstein SH: Sequential administration of recombinant human interleukin-3 and granulocyte-macrophage colony-stimulating factor after autologous bone marrow transplantation for malignant lymphoma: A phase H I multicenter study. Blood 84:2 15 I , 1994 19. Rapoport AP, Abboud CN, DiPersio JF: Granulocyte-macrophage colony-stimulating factor (GM-CSF) and granulocyte colonystimulating factor (G-CSF): Receptor biology, signal transduction, and neutrophil activation. Blood Rev 6:43, 1992 20. Welte K, Zeidler C, Reiter A, Muller W, Odenwald E, Souza L, Riehm H: Differential effects of granulocyte-macrophage colonystimulating factor and granulocyte colony-stimulating factor in children with severe congenital neutropenia. Blood 7S:1056, 1990 21. Weinthal J, Sender L, Briones G, Gillan E, van de Ven C. Cairo MS: The sequential combination of GM-CSF followed by GCSF significantly enhances myeloid engraftment compared to GMCSF alone following bone marrow transplantation. Blood 82:286a, 1993 (suppl) 22. Sonoda Y, Yang YC, Wong GG, Clark SC, Ogawa M: Analysis in serum-free culture of the targets of recombinant human hemopoietic growth factor: Interleukin 3 and granulocytelmacrophage colony-stimulating factor are specific for early development stages. Proc Natl Acad Sci USA 85:4360, 1988 23. Weisdorf D, Katsanis E, Verfaillie C, Ramsay NKC, Haake R, Garrison L, Blazar BR: IL- la administered after autologous transplantation. A phase I clinical trial. Blood 84:2044, 1994 24. WeisdorfDJ,Anderson P, Blazar B, Kersey JH, Ramsay NKC: Interleukin-2 immediately after autologous bonemarrow transplantation for acute lymphoblastic leukemia: A phase I study. Transplantation SS:61, 1993 25. Davies SM, Weisdorf DJ, Haake RJ, Kersey JH, McGlave PB, Ramsay NKC, Blazar BR: Second infusion of bone marrow for treatment of graft failure after allogeneic bone marrow transplantation. Bone Marrow Transplant 14:73, 1994 26. Gherlinzoni F, Miggiano MC, Visani G, Ricci P, Mazza P, Zinzani PL, Motta MR, Rosti G, Bandini G, Lemoli RM, Tura S: Granulocyte colony-stimulating factor (G-CSF) accelerates granulocytic recovery faster than granulocyte-macrophage colony-stimulating factor (GM-CSF) in non-Hodgkin’s lymphoma (NHL) patients submitted to autologous bone marrow transplantation (ABMT). Blood 80:522a, 1992 (suppl) 27. Spitzer G , Adkins DR, Spencer V, Dunphy FR, Petruska PJ, Velasquez WS, Bowers CE. Kronmueller N, Niemeyer R, McIntyre W: Randomized study of growth factors post-peripheral-blood stemcell transplant: Neutrophil recovery is improved with modest clinical benefit. J Clin Oncol 12:66l, 1994 28. Miksits K, Beyer J, Siegert W: Serum concentrations of GCSF during high-dose chemotherapy with autologous stem cell rescue. Bone Marrow Transplant 11:375, 1993 29. Cairo MS, Gillan ER, Weinthal J, Yancik S, van de Ven C, Ho W, Shen V, Buzby JS, Suen Y: Decreased endogenous circulating steel factor (SLF) levels following allogeneic and autologous BMT: Lack of an inverse correlation with post-BMT myeloid engraftment. Bone Marrow Transplant 11 :l%, 1993 30. Haas R, Gericke G, Witt B, Cayeux S, Hunstein W: lncreased serum levels of granulocyte colony-stimulating factor after autologous bone marrow or blood stem cell transplantation. Exp Hematol 21:109, 1993 From www.bloodjournal.org by guest on February 6, 2015. For personal use only. 1995 85: 3452-3456 Hematopoietic growth factors for graft failure after bone marrow transplantation: a randomized trial of granulocyte-macrophage colony- stimulating factor (GM-CSF) versus sequential GM-CSF plus granulocyte- CSF DJ Weisdorf, CM Verfaillie, SM Davies, AH Filipovich, JE Jr Wagner, JS Miller, J Burroughs, NK Ramsay, JH Kersey and PB McGlave Updated information and services can be found at: http://www.bloodjournal.org/content/85/12/3452.full.html Articles on similar topics can be found in the following Blood collections Information about reproducing this article in parts or in its entirety may be found online at: http://www.bloodjournal.org/site/misc/rights.xhtml#repub_requests Information about ordering reprints may be found online at: http://www.bloodjournal.org/site/misc/rights.xhtml#reprints Information about subscriptions and ASH membership may be found online at: http://www.bloodjournal.org/site/subscriptions/index.xhtml Blood (print ISSN 0006-4971, online ISSN 1528-0020), is published weekly by the American Society of Hematology, 2021 L St, NW, Suite 900, Washington DC 20036. Copyright 2011 by The American Society of Hematology; all rights reserved.
© Copyright 2026