Induction of Anti-Recombinant Human Granulocyte
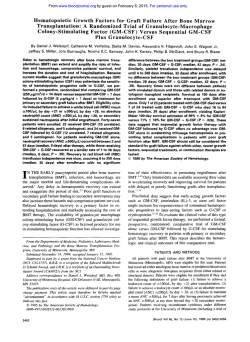
From www.bloodjournal.org by guest on February 6, 2015. For personal use only. Induction of Anti-Recombinant Human Granulocyte-Macrophage Colony-Stimulating Factor (Escherichia coli-Derived) Antibodies and Clinical Effects in Nonimmunocompromised Patients By Peter Ragnhammar, Heinz-Jurgen Friesen, Jan-Erik Frodin, Ann-Kari Lefvert, Moustapha Hassan, Anders Osterborg, and HAkan Mellstedt The pharmacokinetics of recombinant human granulocytemacrophage colony-stimulating factor (rhGM-CSF), induction of anti-GM-CSF antibodies, and clinical effects related t o the induction of the antibodies were analyzed in patients with metastatic colorectal carcinoma (CRC)who were not on chemotherapy (n = 20, nonimmunocompromisedpatients). rhGM-CSF (250 pg/m2/d; Escherichia coli-derived) was administered subcutaneously for 10 days every month for 4 months. Eight patients with multiple myeloma (MM) on intensive chemotherapy followed by rhGM-CSF treatment were also included (immunocompromisedpatients). After a single injection of GM-CSF at the first cycle in CRC patients, the maximum calculated concentration (Cmax)was 5.24 ? 0.56 ng/mL; the half life was 2.91 f 0.8 hours; and the area under the concentration curve (AUC) was 30.86 f 6.03 hours x ng/mL (mean f SE). No anti-GM-CSF antibodies were detected. During the subsequent cycles, 95% of the CRC patients developed anti-GM-CSF IgG antibodies, which significantly altered the pharmacokinetics of rhGM-CSF at the third and fourth cycles with decreased, C (2.87 f 0.57 ng/mL; P .05),(1.57 2 0.2 hours; P < .05), and AUC (14.90 f 4.10 hours x ng/mL; P < .005). The presence of anti-GM-CSF antibodies significantly reducedthe GM-CSFinduced enhancement of granulocytes, there and was a clear tendency for a decreased increment of monocytes. Antibodies diminished systemic sideeffects of rhGM-CSF. Only 1 of 8 MM patients showed a very low anti-GM-CSF antibody titer after GM-CSF therapy, as shown by enzyme-linked immunosorbent assay and Westernblot. Therefore, in nonimmunocompromised patients,exogenous nonglycosylated GM-CSF induced an anti-GM-CSF IgG antibody response in practically all patients, which seemed t o be of clinical significance. In immunocompromised patients, virtually no significant antibody response was shown. 0 1994 by The American Society of Hematology. C ~ytes.',',~The immunogenicity of tumor cells may be enhancedby GM-CSF through facilitating "tumor antigen" presentation.8 GM-CSF has also been shown to cooperate with other cytokines in the expansion of specific T cells? Transfection of the GM-CSF gene to tumor cells with the aim to increase the immunogenicity of the cells and to locally stimulate effector cells might also bean interesting approach." GM-CSF alone might induce tumor regression in humans, probably by activating specific and unspecific killer cells.",'* Therapeutic unconjugated monoclonal antibodies (MoAbs) may eradicate tumor cells in vivo by activating various immune f~ncti0ns.l~ Some of these mechanisms such as antibody-dependent cellular cytolysis and induction and amplification of an idiotypic network response may be augmented by GM-CSF.14"6Based on our therapeutic experience with the anticolon carcinoma MoAb 17-1A (mouse IgG2A) alone,I5 on in vitro results combining GM-CSF and MoAb 17-1A for killing of human carcinoma cell lines14 and on the above-mentioned effects of GM-CSF, a therapeutic trial in patients with metastatic colorectal carcinoma (CRC) was initiated combining GM-CSF and MoAb 17-1A. Long-lasting complete remissions were noted.17 The effects on the cytotoxic capability of peripheral blood mononuclear cells in vivo and on cell subsets involved in the cytotoxic reactions have recently been described." Detailed information on various aspects of exogenously administered GM-CSF should be of value to optimize the use of this cytokine as an antineoplastic and hematopoetic stimulatory agent. In this report, we describe the pharmacokinetics of GM-CSF and the induction of anti-GM-CSF antibodies as well as some clinical effects connected to the induction of these antibodies. The antibody response was also related to whether the patients were nonimmune-compromised (no concomitant chemotherapy) or immunocompromised (concomitant intensive chemotherapy). OLONY-STIMULATING FACTORS (CSFs) have pleiotropic effects, inducing maturation and functional activation of blood cells. Several hematopoetic growth factors (ie, interleukin-l [IL-l], IL-3, IL-6, IL-11, erythropoetin, stem cell factor, macrophage-CSF, granulocyte-CSF, and granulocyte-macrophage-CSF [GM-CSF]) have been identified' with the major clinical applications to support myelogeneration after myelosuppressive therapy. GM-CSF might also be a useful cytokine for biotherapy of malignant diseases. GM-CSF induces (1) differentiation of monocytes to large macrophage-like cells?3 ( 2 ) augmentation of major histocompatibility complex class 11 antigen expression on monocyte^?^ (3) enhancement in vitro of macrophage and granulocyte spontaneous cytotoxicity and antibody-dependent cellular cytolysis,6 and(4) increased expression of adhesion molecules on granulocytes and mono- From the Department of Oncology (Radiumhemmet) and the Immunological Research Laboratory, Karolinska Hospital, Stockholm, Sweden; Behringwerke AG, Marburg, Germany; and the Research Department, Karolinska Pharmacy, Stockholm, Sweden. Submitted August 23, I993; accepted August 25, 1994. Supported by grants from the Swedish Cancer Society, the Cancer Society in Stockholm, theKing Gustaf V Jubilee Fund,theElina Andersen Foundation, theEva and Jerzy Cederbaum Foundation, and the Karolinska Institute Foundations. The study was approved by the Ethics Committee of the Karolinska Institute. Address reprint requests to HikanMellstedt, MD, PhD, Associate Professor, Department of Oncology (Radiumhemmet), Karolinska Hospital, S - l 71 76 Stockholm, Sweden. The publication costs of this article were defrayed in part by page charge payment. This article must therefore be hereby marked "advertisement" in accordance with 18 U.S.C. section 1734 solely to indicate this fact. 0 1994 by The American Society of Hematology. 0006-497I/94/84I2-06$3.00/0 4078 Blood, Vol 84, No 12 (December 15). 1994 pp 4078-4087 F From www.bloodjournal.org by guest on February 6, 2015. For personal use only. 4079 ANTI-GM-CSFANTIBODIES-BIOLOGICEFFECTS Table 1. Characteristics of Patients With CRC Age (YrVSex Primary Tumor Site (Tumor Differentiation) MACC Previous Therapy PS-T of (MO) 1 2 3 53ff 63F 661F Colon (M) Rectum (M) Colon (M) c3 B2 D S S S 2 115 17 4 5 6 651M 671F 291M Rectum (M) Colon (M) Colon (P) D c3 Chemo S S S 14 1 3 7 14/F Colon (M) c3 S Chemo lrrad 9 8 9 10 11 12 13 14 15 16 17 18 19 20 70m 51m 69m 23m 66m 45m 38ff 69/M 78/M 661M 53lM 74F 29/F Colon (P) Rectum (M) Colon (M) Rectum (M) Rectum (M) Colon (“P) Colon (M) Colon (M) Rectum (M) Rectum (M) Colon (M) Rectum (M) Colon (M) B3 D D c3 B3 c2 c3 B3 B1 c3 c2 c3 D S S 3 3 3 9 48 2 2 6 59 2 22 29 S 4 Patient No. D S S S S S S S S S S No. of GM-CSF Treatment Cycles Total dose of GM-CSF (pg) Mesenteric nodes Left cervical nodes Lung 3 4 3 9,140 10,500 13,500 1.933 0.500 1.686 66 38 66 Liver Liver Liver, Lung, Abdominal mass Liver, lymph nodes 3 4 2 15,000 16,000 8,000 1.009 1.732 0.503 66 94 38 3 13,000 1.595 66 Retroperitoneal wall Liver Liver Omentum Abdominal wall Lymph nodes Lymph nodes Abdominal wall Liver Lymph nodes Liver, Abdominal wall Pulm Liver, Lymph nodes 4 3 4 4 4 4 4 4 2 4 4 4 4 17,400 13,200 19,000 18,800 19,000 19,000 16,000 2 1,600 9,200 19,600 18,300 17,600 16,200 2.069 1.282 1 .g70 1.739 2.085 0.430 1.966 0.350 0.600 <0.300 1.155 0.981 0.430 66 66 94 94 66 94 66 85 57 Site Metastases Maximum Anti-GM-CSF (IgG) Titer (OD) Day of Maximum Antibody Titer From Start of Therapy 94 94 85 Abbreviations: M, moderately differentiated; P, poorly differentiated; MACC, modified Astler Coller class; S, surgery; Chemo, chemotherapy; Irrad, irradiation; PS-T, time from primarysurgery to start of therapy. Treatment Schedule MATERIALS AND METHODS Patients CRC. Twenty patients (12 males and 8 females) entered a phase II trial (Table l). The median age was 65 years (range, 14 to 78 years). All patients had metastatic CRC and a Karnofsky index of 280%. One patient had received chemotherapy and irradiation 5 months earlier, and another had chemotherapy 2 months previously. All others were, except for primary surgery, untreated. Multiple myeloma (MM). Eight patients (2 menand 6 women) with MM clinical stage IIA or IIIA according to Durie and Salmon” were. included (Table 2). The diagnostic criteria for MM have been described previously.2”The median age was 69 years (range, 50 to 74 years). All patients were previously untreated and had a Karnofsky index of 280%. CRC patients. Recombinant human GM-CSF (rhGM-CSF) produced in Escherichia coli (specific activity, 5 X lo7 Ulmg protein; Behringwerke AG, Marburg, Germany) was administered at a dose of 250 ,ug/m2/d subcutaneously (SC) for 10 days. On day 3,400 mg of MoAb 17-1A (mouse IgG,; Centocor, Malvern, PA) was infused intravenously (IV) for 60 minutes. The treatment cycles were repeated every fourth week. Four cycles were administered.” If the disease progressed during the study period, the patients were withdrawn from the study and were offered chemotherapy. MM patients. The MM patients entered a phase I multicenter trial studying escalating doses of cyclophosphamide in combination with interferon-a (IFN-a) and betamethasone. The dose of cyclophosphamide (Cyclofosfamid; Orion, Espoo, Finland) ranged from Table 2. Characteristics of Patients Wkh MM Patient No. 1 2 3 4 5 6 7 8 Clinical Age (Yr)/Sex 3 72lM 2 4F 681F 4 71F 3 6 5 69lF 4 67lM Stage 111 <0.300 A II A <0.300 111 <0.300 A II A II A II A 111 A II0.312 A No. of GM-CSF Treatment Cycles 8,600 8,600 18,400 16,000 14,800 415,200 Total Dose of Cyclophosphamide (mg) 10,200 6,800 12,400 4,000 <0.300 14,400<0.300 12,400 9,270 7,600 Total Dose of GM-CSF ( p g ) Maximum Anti-GM-CSF (IgG) Titer (OD) 13,200 2 1,600 <0.300 ~0.300 From www.bloodjournal.org by guest on February 6, 2015. For personal use only. RAGNHAMMAR ET AL 4080 500 mg/m2 to 950 mg/m* IV. CY was administered on days 1 and 3 of a 4-day treatment cycle. IFN-(Y(WellferonR; Wellcome Ltd, Beckenham, London, UK) was administered daily SC on days 1 through 4. Betamethasone (30 mg daily; BetapredR; Glaxo, Middlesex, UK) was administered orally on days 1. through 4. The cycle was repeated every fourth week. All MM patients received 5 pg/ kgldof GM-CSF (molgramostim; E coli-derived; LeucomaxR; Schering-Plough Corp, Kenilworth, NJ) SC from day 5 of a cycle until the day when the granulocyte count exceeded 1.5 X IO’IL and the nadir platelet count was passed. The individual number of treatment cycles as well as the total dose of rhGM-CSF are shown in Table 2. In all MM patients, GM-CSF was administered for 7 to 12 consecutive days, with a median time of 9 days. Serum samples for anti-GM-CSF antibody analyses were drawn at least 10 days after a GM-CSF injection. Blood Cell Counts The total number of white blood cells (WBCs) were counted using a Zeiss standard RA microscope in ordinary light (magnification X 1,000). Two hundred cells were counted. The percentage of WBC subsets was determined by a differential count on smears of peripheral blood stained with May-Griinwald and Giemsa. The total number of blood cell populations was calculated from these figures. Serum Sampling Venous blood was collected in sterile tubes. The serum was separated and stored at -70°C until assayed. GM-CSF Assay The pharmacokinetics of GM-CSF were determined on the first day of a cycle. GM-CSF was assayed in enzyme-linked immunosorbent assay (ELISA), using flat-bottomed microtiter ELISA plates (96 wells; Costar, Cambridge, MA), coated with a mouse monoclonal antihuman GM-CSF antibody (IgG,; Genzyme, Cambridge, MA, USA) overnight at 4°C. After blocking with 8% boiled fat-free milk (Semper, Stockholm, Sweden) diluted in phosphate buffer (pH 9.7) for 2 hours at 37“C, the serum samples and the GM-CSF standard (in human normal AB serum [1:6]; Behringwerke AG) diluted in phosphate buffer (pH 7.2) were added in duplicates and incubated overnight at 4°C. The serum samples as well as the GM-CSF standard were passed through a Protein A Sephadex column (CL-4b; Pharmacia, Uppsala, Sweden) before adding to the ELISA plates to remove cross-reacting antibodies.21Then, a polyclonal rabbit antiGM-CSF antibody (Genzyme) in phosphate buffer, pH 7.4, (1:lOOO) containing 1% milk was added for 2 hours at 37°C. The plates were then reacted for 2 hours at 37°C with a goat antirabbit IgG alkaline phosphate conjugate (Sigma, St Louis, MO) in phosphate buffer, pH 7.4, with 1% milk (1:300). After enzyme reaction for 30 minutes at room temperature using p-nitrophenylphosphate (1 mg/mL; Sigma) in diethanolamine buffer, pH 9.8, the absorbance was read at 405 nm using an automatic ELISA reader (Multi-Scan plus; Laboratory Systems, Helsinki, Finland). Anti-GM-CSF Antibody Assay Antibodies to rhGM-CSF were detected by a solid-phase, indirect ELISA. Briefly, round-bottom microtiter plates (Behring Diagnostics, Marburg, Germany) were coated with 125 MLper well of rhGMCSF (1 .O pg/mL) in 50 mmoVL phosphate buffer, pH 7.2, at room temperature overnight. (The rhGM-CSFBehringwerke preparation used to coat the plates was shown by mock-ELISA to contain 2.8 ppm of E coli-derived contaminants.) Serum samples were diluted 1 :20 in a TRIS/HCL-buffer, pH 8.1, containing lactofemn, gelatine, bovine serum, and 0.5% Tween 20 (product no. OWBE; Behringwerke AG) for detection of IgG antibodies. To determine antiGM-CSF IgM antibodies, the sample was further diluted ( I : l [vol/ vol]) with rheumatic factor (RF) adsorbent (product no. OUCG 14: Behringwerke AG) and incubated at room temperature for 15 minutes. (The RF adsorbent binds RF, which might give false-positive results in an IgM antibody assay.) The serum sample was then mixed with an E coli lysate (2%; prepared from the E coli strain LE 392 K12 USS; Behringwerke AG) and incubated at room temperature for 1 hour. (This procedure was introduced to remove E cdi-directed antibodies.) A total of 100 pL of the serum samples was then added to microtiter wells in duplicate and incubated at room temperature for 2 hours. The wells were washed in phosphate-buffered saline containing 0.5% Tween 20. The plates were then incubated with 0. I mL per well of peroxidase conjugated antihuman IgM ( I :40; product no. OSDJ; Behringwerke AG) or antihuman IgG ( 1:40; product no. OSDH; Behringwerke AG), respectively, for 2 hours at room temperature. After washing 4 times, 0.1 mL of the substrate tetramethylbenzidine (product no. OUVOlO; Behring Diagnostica) was added to each well, and the plate was incubated for 30 minutes at room temperature. The enzyme reaction was stopped by adding 0.5 N sulfuric acid. The plate was read at 450 nm using a Behring ELISA Processor BEP I1 (Behring Diagnostica). Serum samples with an optical density (OD) value above the range of 300 normal blood donors were considered positive, were further quantitated by ELISA, and were applied to Western blot analysis as a confirmatory assay. The OD values were related to a synthetic standard composed of rabbit antihuman-GM-CSF Fab’ fragments chemically linked to human IgG or IgM molecules, respectively (patent no. EPA 291086 [Boehringer Mannheim] and DEOS 31 12334 [Behringwerke AG]). The synthetic standard has the property of binding to GM-CSF by the Fab’ fragment of rabbit Ig and to antihuman Ig antibodies through the human Ig part of the molecule. Western Blotting rhGM-CSF was separated on sodium dodecyl sulfate-polyacrylamide gel electrophoresis (SDS-PAGE; 16%) using the Laemmli buffer system.22The protein was electroblotted into nitrocellulose filters (Hybond C-Extra; Amersham, Braunschweig, Germany) according to the method of Towbin et aIz3using 25 mmol/L Tris to 192 mmol/L glycine/20% methanol buffer (pH 8.3; vol/vol). A voltage gradient of 6 V/cm was applied for I hour. Each blot was checked by AuroDye protein staining (Amersham). After blotting, the filter was immersed in blocking solution (TRIS/HCI buffer, pH 8.l), containing lactofemn, gelatine, bovine serum, and0.5% Tween 20 (product no. OWBE) and agitated for 1 hour at room temperature. The samples (diluted 150 in OWBE) were preincubated without or with E coli lysate (2%) for 1 hour at room temperature. The filter was then incubated with the samples at room temperature overnight under continuous agitation. After 5 washes in phosphate-buffered saline containing 0.5% Tween 20, the filter was incubated for 1 hour at room temperature with a goat antihuman IgG labeled with colloid gold (Amersham). The signal was amplified, according to the manufacturer’s instructions, using a silver enhancement kit (IntenSE; Amersham). In each test, a positive serum was included showing the same staining pattern as the synthetic standard. Serum Immune Complexes Immune complexes in serum were analyzed using the C l q binding technique as described in detail previo~sly.’~ Pharmacokinetics The pharmacokinetics parameters for subcutaneous administration were evaluated and fitted by a one-compartment model with the From www.bloodjournal.org by guest on February 6, 2015. For personal use only. ANTI-GM-CSF ANTIBODIES-BIOLOGIC EFFECTS 4081 5r Time (hour) Fig 1. Serum concentration (mean) of GM-CSF after a single SC injection (250 pg/m*) at treatment cycle I (0;n = 6; CRC patients no. 10, 11, 12, 14, 18, and 19) and treatment cycles 111 or IV (0;n = 5; CRC patients no. 11, 12, 14, 18, and 19). respectively. (All 5 patients analyzed at cycles 111 or IV had anti-GM-CSF lgG antibodies]. The difference in AUC was statistically significant ( P c .005). first order of absorption. Parameter estimation using nonlinear least squares analysis was performed using PCNONLIN (Statistical Consultants Lexington, KY). Statistical Analyses The differences between means were analyzed using Student's rtest or Wilcoxon signed rank test for paired and unpaired observations. The linear regression model was used to estimate correlation between independent observations. RESULTS Pharmacokinetics of GM-CSF GM-CSF wasnot detectable in serum before therapy. After an SC injection of 250 pg/m' of GM-CSF at cycle I, the maximum calculated concentration (C,,,=) was 5.24 -+ 0.56 ng/mL and was reached at 3.25 2 0.25 hours after the injection. The C, at cycles I11 and IV in the same patients was 2.87 -+ 0.57 ng/mL after 2.67 2 0.33 hours. The difference in serum C,, was statistically significant ( P < .05). The corresponding serum half-lives (TI,') were 2.91 -+ 0.8 hours and 1.59 -+ 0.2 hours, respectively ( P < .OS). There was also a statistically significant difference in the area under the concentration curve (AUC) comparing cycle I (30.86 2 6.03 hours X ng/mL) with cycles 111 and IV (14.90 2 4.10 hours X ng/mL; P < ,005; see Fig 1). The decrease in C,, and AUC by increasing number of treatment cycles was related to the induction of GM-CSF antibodies (see below). Induction of Anti-GM-CSF Antibodies results, the serum samples were preincubated with an E coli lysate to adsorb anti-E coli antibodies. Analyses of serum samples not preincubated with the E coli lysate gave higher OD values (data not shown). Therefore, our assay system has an improved specificity for anti-GM-CSF antibodies. An OD value of greater than 0.3 was used as cutoff for anti-GM-CSF IgG antibodies, and an OD value of greater than 0.15 was usedfor IgM antibodies. In the control population of 300 healthy blood donors, greater than 95% of the individuals had OD values below these levels. Of the 300 donors, 5 had antibodies against GM-CSF detected by ELISA, which wasconfirmed by a weak but specific staining in Western blot (data not shown). No CRC patients had antibodies against GM-CSF before therapy. Anti-GM-CSF IgM antibodies were not detected with the present sampling design. During GM-CSF therapy in the CRC patients, increasing titers of specific anti-GMCSF IgG antibodies were noted (Figs 2 and 3 and Table l). The GM-CSF antibody titers had disappeared at about 30 weeks after the last injection (Fig 2). At the end of cycles I1 and IV, 50% and 90%, respectively, of the tested patients had IgG antibodies (Fig 3). In total, 19 of the 20 CRC patients (95%) developed anti-GM-CSF IgG antibodies (Table l). Three groups of CRC patients could be distinguished with regard to the level of antibody titers induced: no antibody titer (n = 1; CRC patient no. 17); low antibody titers (n = 5; CRC patients no. 2, 6, 13, 15, and 20); andhigh antibody titers (n = 14; CRC patients no. 1, 3, 4, 5, 7, 8, 9, 10, 11, 12, 14, 16, 18, and 19). The presence of anti-GM-CSF IgG antibodies was confirmed by Western blot analyses in all patients, as shown in Fig 4. In addition to the GM-CSF bands (14.5 kD), several weak bands with a molecular weight (MW) corresponding to the MW of E coli proteins (ca 20 kD) could be observed after protein staining (Fig 4, lane A). Immunoblotting of sera preincubated with E coli lysate using an antihuman IgG antiserum showed no bands at the place of E coli proteins but showed only antibodies reacting with GM-CSF (Fig 4, lane B). Sera not preincubated with E coli lysate showed the ]A TI c c , , TI1 TV c, L) A high proportion of normal individuals has antibodies against E coli, usually of high affinit~.'~Such antibodies may interfere in the assay system because the rhGM-CSF preparation for coating of the plates might contain minute amounts (2.8 ppm) of E coli proteins. To avoid false-positive E 2P 13 ""- """""-""""""""" """ ao l2 28 Jx Time (weeks) Fig 2. Anti-GM-CSF IgG antibody titers (ELISA; mean) of patients In = 19) treated with SC injections of GM-CSF for 10 days every month for 4 months. Arrows show treatment cycles; (---l indicates cutoff level. From www.bloodjournal.org by guest on February 6, 2015. For personal use only. RAGNHAMMAR ET AL 4082 I 10 (n.20) IO I I II I (n.20) IO I I, 1 111 IV (nzls) (11.13) Fig 3. Frequency of patients with anti-GM-CSF lgG antibodies at day 1 and day 10 of each treatment cycle (Ithrough IV).Patients with no detectable anti-GM-CSF antibodies (m) and with anti-GM-CSF of patients antibodies (W). Figures with brackets indicate the number receiving therespective GM-CSF cycle. presence of antibodies against E coli as well as GM-CSF (Fig 4, lane C). Blotting of the synthetic antibody standards (IgG and IgM) showed a similar pattern to that of the induced antibodies (Fig 4, lanes D and E). In 2% of the 300 normal donors, anti-E coli IgG antibodies could be detected (Fig 4, lane F) that disappeared after preincubation with E coli lysate (Fig 4, lane G). From an immunologic point of view, the CRC patients might be regarded as having a noncompromised immune systems because they had not previously received chemotherapy (with the exception for 2 patients who had been adminis- A '1) 21) 41) 51) B C D E tered cytostatics 2 to 5 months earlier). All CRC patients had a good performance status. For comparison, a group ofMM patients who had been treated with an intensive chemotherapy regimen followed by GM-CSF administration to support bone marrow regeneration (immunocompromised patients) was included. The MMpatientsreceived rhGM-CSF in a similar scheduling as the CRC patients (see Materials and Methods). Thenumber of cyclesadministeredbeforetestingforantiGM-CSF antibodies in MM patients varied between 2 and 6 (median no., 4). Only 1 MM patient (MM patient no. 8) had detectable anti-GM-CSF antibodies after 4 GM-CSF treatment cycles. The antibody titer was very low. The OD value (0.312; see Table 2 and Fig 5 ) was just above the cutoff level(0.300), and a weak band was noted on Western blot (data not shown). In the remaining 7 patients, no anti-GM-CSF antibodies were detected by ELISA and Western blot (Fig 5). The difference in number of patients with regard to anti-GM-CSF antibody induction between the two groups was statistically, highly significant (x' = 5.23; P < .001). The two patient groups both received E coli-derived GMCSF. However, CRC patients were administered a recombinant protein produced by Behringwerke, and MM patients received rhGM-CSF from Schering-Plough. As can be observed in Fig 5, CRC patients treated with rhGM-CSFIBehringwerke developed antibodies reacting withrhGM-CSF/ Behringwerke as well as with rhGM-CSF/Schering-Plough. Clinical Effects of Anti-GM-CSF Antibodies Pharmcrcokinetics. The induction of anti-GM-CSF antibodies was associated with a significant reduction of C,,, TI,?.and AUC of exogenously administered GM-CSF (see above and Fig 1). F G Fig 4. Western blotting of anti-GM-CSF antibodies (CRC patient no. 9). Mobilities of the MW standards are indicated at the margin: left (1) bovine trypsin inhibitor, 6.2 kD; (2) lysozyme, 14.3 kD; (3) plactoglobulin, 18.4 kD; (4) carbonic anhydrase, 28.5 kD; and (5) ovalbumin, 43.8 kD. (Horizontal arrow indicates the localizationof the E coli bands.) Lane A shows AuroDye staining of blots. Note the GMCSF main bandwith an MW of 14.5 kD and the main € coli bands at ca. 20 kD. LaneB shows immunoblotting of a patient serum after preincubation with E coli lysate. Note only visible bands at the place of GM-CSF. LaneC is the same as for lane B but without preincubation with € coli lysate. Note also the presence of anti-€ coli antibodies. Lanes D and E show immunoblotting after adding the anti-GM-CSF IgM (D) and anti-GM-CSF IgG (E) synthetic standards. Lane F shows immunoblottingof a normal blooddonor serum without preincubation with€ coli lysate. Note the detectionof anti-€ coli antibodies. Lane G is thesame as for lane F but withpreincubation with E coli lysate. Note the disappearance of anti-€ coli antibodies. From www.bloodjournal.org by guest on February 6, 2015. For personal use only. 4083 ANTI-GM-CSFANTIBODIES-BIOLOGICEFFECTS 4- n 3- Fig 5. Anti-GM-CSF IgG antibody titers IEUSA) in 10 CRC patients ( s e e Table 1) and 8 MM patients (see Table 2) tested against plates coated with GMCSFIBehringwerke).( or GM-CSFISchering-Plough (0). titer and total number of WBCs ( r = -0.438; P < .005), neutrophils ( r = -0.467; P < .001), and eosinophils ( r = -0.334; P < .05) when comparing day 10 of all treatment cycles. By increasing anti-GM-CSF titers, the cell counts decreased. In patients with lowantibody titers, no such correIation could be noted. After each treatment cycle, WBC counts returned to baseline level within 5 days. There was no significant influence on the total number of WBCs during long-term follow-up (Fig 7). Side effects. The main side effects in all CRC patients at cycle I that were considered to depend on the GM-CSF treatment were myalgia (50%), local irritation (45%), fever (greater than38.5"C; 35%), bone painskternalgia (35%), rashlpruritus (35%), conjunctivitis (30%), headache (25%), nausea (15%), and chills (15%). Myalgia was easily controlled by dextropropoxiphene. However, in 1 patient (CRC pateint no. l), the GM-CSF dose had to be reduced because of severe myalgia. Myalgia appeared at days 2 to 3 and disappeared at days 8 to 9 of the cycle. Fever (greater than WBCs. At treatment cycle IV, in CRC patients, the maximum total numbers of WBCs, neutrophils, and eosinophils were significantly lower than the peak values at the previous cycles (P < .05). There was also a clear tendency by each treatment cycle for gradually decreased monocyte counts at day 10 ( P = .06). No tendency for a decreased increment of lymphocytes was noted (Table 3). Patients with low antiGM-CSF antibody titers showed significantly higher values of WBCs, eosinophils, and neutrophils at day 10 of cycle IV as compared with patients with high anti-GM-CSF antibody titers (Table 4). The individual WBC counts at day 10 of each cycle for those 13 patients completing 4 treatment courses are shown in Fig 6. The total number of WBCs was unchanged during the 4 treatment cycles in the patient (CRC17) not developing anti-GM-CSF antibodies, whereas there was a modest decrease in the low-titer patients and a marked decrease at treatment cycles 111 and/or IV in the high-titer group. Moreover, in the high-titer group, there was a statistically significant correlation between the anti-GM-CSF antibody Table 3. Total No. of Blood Cells (Mean f: SE; x lo-' L) at Days 1 and 10 of the 4 Treatment Cycles Cycle l (n = 20) Blood Cells WBC Neutrophils Eosinophils Basophils Monocytes Lymphocytes t 5 Cycle II (n = 20) Day 1 Day 10 6.66 2 0.35 4.42 t 0.35 0.27 2 0.05 0.02 2 0.01 0.42 2 0.05 1.53 2 0.10 26.24 2 1.78' 17.12 2 1.58t 4.47 2 0.57t 0.06 f 0.02 1.16 2 0.23t 2.72 f 0.24' Day 1 6.35 2 4.21 2 0.21 2 0.02 2 0.37 +1.54 +- 0.39 0.37 0.03 0.01 0.05 0.12 Cycle IV In = 13) Cycle 111 (n = 18) Day 10 30.41 2 19.24 2 6.38 2 0.04 2 0.96 2 3.27 2 1.97* 1.31t 0.79t 0.02 0.17t 0.32' P < .05 and " P < ,001 comparing day 1 and 10 of each cycle. P < .05 and * P < .01 comparing day 10 of cycle I and day 10 of cycle IV. Day 1 Day 10 Day 1 Day 10 6.54 ir 0.40 4.27 2 0.43 0.32 2 0.06 0.03 t 0.01 0.44 2 0.08 1.51 2 0.17 22.65 2 3.81" 13.97 t 2.53" 4.41 +- 1.05' 0.04 t 0.02 0.85 t 0.13t 2.80 -e 0.33" 7.34 2 0.56 5.15 +- 0.69 0.33 +- 0.13 0.04 ? 0.02 0.43 t 0.04 1.53 +- 0.18 15.83 2 2.48+* 9.65 +- 1.50tS 2.68 -c 0.69t5 0.02 5 0.01 0.80 0.11t 2.57 t 0.45t From www.bloodjournal.org by guest on February 6, 2015. For personal use only. RAGNHAMMAR ET AL 4084 Table 4. Total No. of Blood Cells (Mean 2 SE; x lo-’ L) in CRC Patients With Low (n = 4) and High (n = 8 ) Anti-GM-CSF Antibody Titers, Respectively, at Days l and 10 of Treatment Cycle IV Day 1 Low Anti-GM-CSF Blood Subsets WBC Neutrophils Eosinophils Basophils Monocytes Lymphocytes Antibody Titer 6.63 4.34 0.19 0.04 0.52 1.92 i- 0.84 2 1.07 i 0.09 t 0.01 2 0.14 i 0.36 Day l 0 High Anti-GM-CSF Antibody Titer 7.72 5.40 0.37 0.04 0.40 1.41 i 0.71 0.84 i 0.16 t 0.01 i 0.04 i 0.20 -t Low Anti-GM-CSF Antibody Titer High Anti-GM-CSF Antibody Titer 23.43 i 3.64 13.95 -t 1.38 4.65 i 1.46 0.02 -t 0.01 0.99 2 0.08 3.89 -t 1.12 : 2.34* 12.04 : 7.50 z 1.71* 1.70 2 0.49* 0.03 -t 0.01 0.70 ir 0.16 3.69 t 0.91 Only patients with low (CRC patients no. 2,13,15, 20) and high (CRC patients no. 5, 8, 10, 11, 12, 14, 18, 4 GM-CSF treatment cycles are depicted in this table. * P < .05 comparing the low- and high-titer groups at the same dayof the treatment cycle. 38.5”C) was noted 2 to 3 hours after the injection and lasted for 2 to 6 hours. There was a clear tendency towards reduced frequency of systemic adverse reactions such as myalgia, fever, rusWpruritus, conjunctivitis, headache, and nausea by treatment cycle IV. The side effects during each cycle in those 13 CRC patients completing 4 GM-CSF treatment courses are shown in Table 5. Furthermore, in the high antiGM-CSF antibody titer group, a total of 4 systemic adverse events were registered among 9 patients at treatment cycle IV, whereas 7 were recorded among the 4 low antibody titer patients. There were no clinical signs of immune complex-related adverse reactions. The kidneys are supposed to be the most sensitive organ to immune complexes. No patient had proteinuria or red blood cells in the urine, which are sensitive indicators of renal immune complexes depositions. Serum immune complexes were analyzed at each treatment cycle. No circulating immune complexes could be detected. DISCUSSION Nonimmunocompromised patients with metastatic CRC received 10 days of GM-CSF treatment repeated every month for 4 months with the aim being to activate cellular cytotoxic functions as well as antigen presenting cells and to amplify an idiotypic immune network response. The pharmacokinetics (C,,,, TI,>,and AUC) of GM-CSF during cycle I was similar to that described by other^.^^^^' However, after repeated cycles, pharmacokinetics analyses of GM-CSF showed significantly reduced C,,,,, andAUCthat correlated with the appearance of anti-GM-CSF antibodies. To acertain that our assay system detected true anti-GMCSF antibodies, particular attention waspaidto avoiding measuring anti-E coli antibodies, because minute amounts of E coli proteins might be present in the drug preparations administered to the patients aswell as in the rhGM-CSF preparations used to capture anti-GM-CSF antibodies. Morover, anti-E coli antibodies are common among normal individuals and increase with an individual’s age.25By preincubation of the sera with an E coli, lysate false-positive results could be avoided. These precautions should be taken in all immune assays using recombinant proteins producedin E 19) anti-GM-CSF titers completing coli. Furthermore, human antimouse antibodies (HAMAs) were induced in all CRC patients, but HAMAs did not seem to interact with anti-GM-CSF antibodies in the assay. The incubation medium contained whole bovine serum that effectively suppressed nonspecific binding to the solid phase. Nonbound HAMAs were washed away before adding the conjugate. Moreover, there was no correlation between the HAMA response and the anti-GM-CSF response. The induction of HAMAs was more rapid than that of anti-GMCSF antibodies. Most of the CRC patients had developed HAMAs at start of cycle 11, whereas no patient had antiGM-CSF antibodies at this time-point. At 30 weeks after completion of therapy, no patient had detectable anti-GMCSF titer, whereas all patients still had HAMAs (submitted for publication). The induction of anti-GM-CSF antibodies was probably a primary immune response even though no IgM antibodies were detected. The kinetics of the IgG antibodies were clearly that of a primary immunization. Reports on induction of anti-GM-CSF antibodies are scanty. Of 16 patients with advanced malignancies who were heavily pretreated or on intensive chemotherapy, 4 developed anti-GM-CSF IgG antibodies against rhGM-CSF.” Of 16 patients with myelodysplastic syndrome receiving GM-CSF after previous treatment with chemotherapy, 1 developed a low titer of antiGM-CSF antibodiesz9 In spite of an abundance of studies using rhGM-CSF to support myeloregeneration after myelosuppressive therapy, to our knowledge, these are the only studies that show anti-GM-CSF antibody induction. These two reports are in agreement with the results in the MM patients of the present study, where l of 8 patients on heavy chemotherapy had a low anti-GM-CSF antibody titer after 4 cycles of GM-CSF administration. The high frequency of anti-GM-CSF antibodies inthe CRC patients may have several explanations. All patients had a good performance status, and only 2 of them had previously received chemotherapy/irradiation.Therefore, the CRC patients should be regarded as nonimmunocompromised as compared with the MM patients who, like the patients of the other studies, were most likely immunocompromised as a consequence of intensive chemotherapy. From www.bloodjournal.org by guest on February 6, 2015. For personal use only. 4085 ANTI-GM-CSFANTIBODIES-BIOLOGICEFFECTS 40 30 20 10 20 30 40 50 Time (weeks) Fig 7. Total WBC counts (mean) during and after GM-CSF treatment. Arrows indicate treatment cycles. 10 0 I I I II 111 I IV Treatment cycle Fig 6. Total number of WBCs at day 10 of the 4 GM-CSF treatment cycles in those 13 patients completing 4 cycles (Table 1) is shown in relation to anti-GM-CSF antibody titers. (.I no anti-GM-CSF antibodies (CRC patient no. 171; (@) low anti-GM-CSF antibody titers (CRC patients no. 2, 13, 15, and 20); (A)high anti-GM-CSF antibody titers (CRC patients no. 5, 8, 10, 11, 12, 14, 18, and 19). Therefore, our results might support the assumption that chemotherapy prevented the development of antibodies to rhGM-CSF. Moreover, we administered GM-CSF SC, which is an excellent route for antigen presentation as compared with IV administration. Furthermore, GM-CSF was administered in repeated cycles that boostered the patients. Interestingly, antibodies developed against GM-CSF/ Behringwerke also reacted with GM-CSF/Schering-Plough. (Both GM-CSFs were produced in E coli.) The standards as well as most of the positive serum samples showed higher signals on GM-CSF/Schering-Plough-coated plates as compared with GM-CSFBehringwerke-coated plates (Fig 5). This might partly be because of the fact that, in this set-up of analyses, freshly coated GM-CSFISchering-Ploughplates were used, whereas the GM-CSFBehringwerke plates were precoated and stored with a drying agent in sealed bags at +4"C until use. However, there was no constant factor from sample to sample between plates coated with the different GM-CSFs. This is not surprising. The two GM-CSFs were prepared by different production procedures. The epitope pattern of the two different GM-CSFs would be expected to differ, and the antibody response may vary from patient to patient with regard to epitopes recognized. The presence of GM-CSF antibodies seemed to have biologic effects. The altered pharmacokinetics of GM-CSF with decreased C, and AUC as well as shorter T I n resulted probably in reduced amounts of bioavailable rhGM-CSF, which was also suggested by Gribben et al.'' In that study, the increase in neutrophils was not that expected in 1 of 4 patients developing anti-GM-CSF antibodies. In our patients, there was a clear relationship between the anti-GMCSF antibody titers and the increase in WBCs, neutrophils, and eosinophils (ie, the higher the antibody titer, the lower the cell increase). With repeated cycles, there was a clear tendency towards a lower increment in total number of monocytes, although the difference did not reach statistical significance. Lymphocyte counts seemed to be uneffected. The results are in agreement with the notion that GM-CSF mainly affects maturatiodproliferation of hematopoetic cells Table 5. Frequency of GM-CSF Side Effects in Those 13 Patients Completing 4 GM-CSF Treatment Cycles Treatment Cycle Side Effects Myalgia Local irritation Fever >38.5"C Bone pains/sternalgia Rashlpruritus Headache Conjunctivitis Nausea Chills Percentages are shown in parentheses. II From www.bloodjournal.org by guest on February 6, 2015. For personal use only. 4086 RAGNHAMMAR ET AL 4. Steis RG, VanderMolen LA, Longo DL, Clark JW, Smith JW, KoppWC,Ruscetti F W , CreekmoreSP,Elwood LJ. Hursey EJ. UrbaWJ:Recombinanthumangranulocyte-macrophagecolonystimulating factor in patients with advanced malignancy: A phase I b trial. J Natl Cancer Inst 82:697, 1990 S. Blanchard DK, Dieu JY:Differentialmodulation of surface antigens on human macrophages by 1FN-gamma and GM-CSF.Effect on susceptibility to LAK lysis. J Leukoc Biol 50:28, 1991 6. Grabstein KH, Urdal DL, Tushinski RJ, Mochizuki DY, Price VJ, CantrellMA,Gillis S, ConlonPJ:Induction of macrophage tumoricidal activity by granulocyte-macrophage colony stimulating factor. Science 232506, 1986 7. Arnaout MA, Wang EA, Clark SC, Sieff CA: Human recombinant granulocyte-macrophagecolony-stimulatingfactorincreases cell-to-cell adhesion and surface expression of adhesion-promoting surface glycoproteins on mature granulocytes. J Clin Invest 78:597, 1986 8. FischerHG,Frosch S, Reske K, Reske-KunzAB:GM-CSF activates macrophages derived from hone marrow cultures to syntheI1 molecules andto augmented antigen presentation sis of MHC class function. J Immunol141:3882,1988 9. Santoli D, ClarkSC,KreiderBL,Patricia AM, Maslin A, Rovera G: Amplification of IL-2 driven T-cell proliferation by recombinant human IL-3 and granulocyte-macrophage colony stimulating factor. J Immunol 141:519, 1988 10. Dranoff G, Jaffee E, Lazenby A, Golumbek P, Levitsky H, Brose K, Jackson V, Hamada H, Pardoll D, Mulligan R: Vaccination with irradiated tumor cells engineered to secret murine granulocytemacrophagecolony-stimulatingfactorstimulates potent. specific, andlong-lastinganti-tumorimmunity.Proc Natl AcadSci USA 903530, 1993 1 1 . Steward WP, Scarffe JH, Austin R, Bonnem E, Thatcher N, Morgenstern G, Crowther D: Recombinant human granulocyte macrophage colony stimulating factor (rhGM-CSF) given as daily short infusions-a phase I dose-toxicity study. Br J Cancer 59: 142, 1989 12. Boente P, SampaioC,Brandao M, Moreira E, BadaroR, Jones T: Local peri-lesional therapy with rhGM-CSF for Kaposi's sarcoma. Lancet 341:1154, 1993 13. Herlyn D, Herlyn M, Ross AH, Emst C,Atluns B, Koprowski H: Efficient selection of human tumor growth-inhibiting monoclonal antibodies. J Immunol Methods 73:157, 1984 14. Masucci G, Wersall P, Ragnhammar P, Mellstedt H: Granulocyte-monocyte-colony-stimulating factor augments the cytotoxic capacity of lymphocytes and monocytesin antibody dependent cellular cytotoxicity. Cancer lmmunol Immunother 29:288, 1989 ACKNOWLEDGMENT 15. Mellstedt H, Frodin J-E, Masucci G, Ragnhammar P, FagerDr Jiirgen Frisch is greatly acknowledged for stimulating discusJ, Wersall P, Osterborg A: The therapeutic berg J, Hjelm A-L, Shetye sions. We thank Birgitta Hagstrom, Annika Overmo, and Gun Ersuse of monoclonal antibodies in colorectal carcinoma. Semin Oncol mark for skillful technical assistance; Anita Ljungberg for providing 18:462, 199 I excellent nursing; and Lena Helgesson and Gunilla Bur& for skill16. Tao M-H, Levy R: Idiotype/granulocyte-macrophage colonyfull typing of the manuscript. stimulating factor fusion protein as a vaccine for B-cell lymphoma. Nature 362:755, 1993 REFERENCES 17. Ragnhammar P, Fagerberg J, Frodin J-E, Hjelm A-L, Lindemalm C, Magnusson I, Masucci G, Mellstedt H: Effect of themonoI . Williams ME, Quesenbeny PI: Hematopoetic Growth Factors. clonal antibody 17-1 A and GM-CSFin patients with advanced coloHematol Pathol 6:105, 1992 rectal carcinoma.-Long lasting complete remissions can be 2. Young DA, Lowe LD, Clark SC: Comparision of the effects of IL-3, granulocyte-macrophage colony-stimulating factor and mac- induced. Int J Cancer 53:751, 1993 18. Ragnhammar P, MasucciG, Frodin J-E, Hjelm A-L, Mellstedt rophage colony-stimulating factor in supporting monocyte differentiH: Cytotoxic functions of blood mononuclear cells in patients with ation in culture. J Immunol 145:607, 1990 3. Robin G, Markovich S, Athamna A, Keisary Y: Human recom- colorectal carcinoma treated with MAb17-IA and GM-CSF. Cancer Immunol Immunother 35:158, 1992 binant granulocyte-macrophage colony-stimulating factor augments 19. Durie BGM, Salmon SE: A clinical staging system for multiviability and cytotoxic activities of human monocyte-derived macple myeloma. Cancer 36:842, 1975 rophages in long-term cultures. Lymphokine Cytokine Res 10257, 20. Mellstedt H, Bjorkholm M, Holm G: Intermittent melphalan 1991 of the myeloid and monocytic lineages. An alternative explanation to the lower leucocyte counts at subsequent cycles may bea decreased capacityof bone marrow to bestimulated by GM-CSF. Moreover, at cycle IV, systemic side effects of GM-CSF(myalgia,fever, rash/pruritus,conjunctivitis, headache, and nausea) were markedly reduced as compared with the previous cycles, which may be related to the induction of anti-GM-CSF antibodies. Also in this respect, there seemed to bea difference between those patients developing high anti-GM-CSF titers and those withlow titers. This finding is similar to that of another study showing that the appearance of antibodies to rIFN-ol2, reduced the sideeffects of rIFN-a2,.'" The induction of anti-rhGM-CSF antibodies did not seem to haveanegative impact on thelevelsof WBCs during long-term follow-up. This might be because of the fact that antibodies induced against exogenous E coli-derived GMCSF recognized epitopes on the nativeproteinbackbone, normallyprotected by 0-linked glycosylationbut exposed on E coli-produced GM-CSF." Therefore, endogenous GMCSF may not be recognized by these antibodies becausethis molecule might not express the relevant immunotopes. AntiGM-CSF antibodies alsogradually disappeared after discontinuation of GM-CSF, probably as aresult of nofurther antigenic stimulation. Therefore, the effects on endogenous GM-CSF might not be hampered by antibodies against exogenous E coli-derived GM-CSF. In summary, this study showed that repeated SC administrationof E coli-derived GM-CSF in nonimmunocompromised patients induced a primary humoral immune response against exogenous GM-CSF in practically all patients. The pharmacokinetics and the variations in WBC counts during therapy indicated that the biologic effects of the exogenous GM-CSF werereduced by the induced antibodies. However, antibodyinductionin immunocompromisedpatientswas rare and of low titers. This has to betaken into consideration when designing therapeutic protocols using recombinant cytokines(probably not only GM-CSF) in patients prone to mount an immune response. From www.bloodjournal.org by guest on February 6, 2015. For personal use only. ANTI-GM-CSF ANTIBODIES-BIOLOGIC EFFECTS and prednisolone therapy in plasma cell myeloma. Acta Med Scand 2025, 1977 21. Kronwall G, Williams RC: Differences in anti-protein A activity among IgG subgroups. J Immunol 103:828, 1969 22. Laemmli U K Cleavage of structural proteins during the assembly of the head of bacteriophage T4. Nature 227:680, 1970 23. Towbin H,Staehelin T, Gordon J: Electrophoretic transfer of proteins from polyacrylamide gels to nitrocellulose sheets: Procedure and some applications. Roc Natl Acad Sci USA 76:4350, 1979 24. Fr6din J-E, Lefvert A-K, Mellstedt H: Pharmacokinetics of the mouse monoclonal antibody 17-LA in cancer patients receiving various treatment schedules. Cancer Res 504866, 1990 25. Webster ADB, Efter T, Asheron GL: Escherichia coli antibody: A screening test for immunodeficiency. Br Med J 3:16, 1974 26. Cebon J, Demsey P, Fox R, Kannourakis G, Bonnem E, Burges AW, Morstyn G: Pharmacokinetics of human granulocyte- 4087 macrophage colony-stimulating factor using a sensitive immunoassay. Blood 72:1340, 1988 27. Hovgaard D, Mortensen BT. Schifter S, Nissen N: Clinical pharmacokinetic studies of a human haemopoietic growth factor, GM-CSF. Eur J Clin Invest 22:45, 1992 28. Gribben JG, Devereux S, Thomas NSB, Keim M, Jones HM, Goldstone AH, Linch DC: Development of antibodies to unprotected glycosylation sites on recombinant human GM-CSF. Lancet 335:434,1990 29. Thompson JA, Lee DJ, Kidd P, Rubin E, Kaufman J, Bonnem EM, Fefer A: Subcutaneous granulocyte macrophage colony-stimulating factor in patients with myelodysplastic syndrome: Toxicity pharmacokinetics and hematological effects. J Clin Oncol 7:629. 1989 30. Inglada L, Pomes JC, La Banda F, Mora I, Carreno V: AntiIFN-a titres during interferon therapy. Lancet 2:1521, 1987 From www.bloodjournal.org by guest on February 6, 2015. For personal use only. 1994 84: 4078-4087 Induction of anti-recombinant human granulocyte-macrophage colony- stimulating factor (Escherichia coli-derived) antibodies and clinical effects in nonimmunocompromised patients P Ragnhammar, HJ Friesen, JE Frodin, AK Lefvert, M Hassan, A Osterborg and H Mellstedt Updated information and services can be found at: http://www.bloodjournal.org/content/84/12/4078.full.html Articles on similar topics can be found in the following Blood collections Information about reproducing this article in parts or in its entirety may be found online at: http://www.bloodjournal.org/site/misc/rights.xhtml#repub_requests Information about ordering reprints may be found online at: http://www.bloodjournal.org/site/misc/rights.xhtml#reprints Information about subscriptions and ASH membership may be found online at: http://www.bloodjournal.org/site/subscriptions/index.xhtml Blood (print ISSN 0006-4971, online ISSN 1528-0020), is published weekly by the American Society of Hematology, 2021 L St, NW, Suite 900, Washington DC 20036. Copyright 2011 by The American Society of Hematology; all rights reserved.
© Copyright 2026