Reduced Expression of Vascular Cell Adhesion Molecule-l
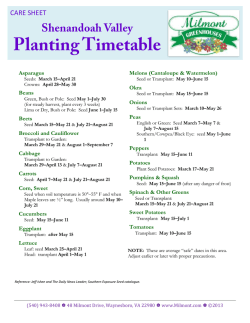
From www.bloodjournal.org by guest on February 6, 2015. For personal use only. Reduced Expression of Vascular Cell Adhesion Molecule-l on Bone Marrow Stromal Cells Isolated From Marrow Transplant Recipients Correlates With a Reduced Capacity to Support Human B Lymphopoiesis In Vitro By Bonnie N. Dittel and Tucker W. LeBien A common sequela t o allogeneic or autologous bone marrow transplantation (BMT) is a delay in the reconstitution of a functional B-cell immune response. Therefore,we examined whether the posttransplant BM microenvironment is deficient in supporting the proliferation and/or differentiation of B-cell precursors.BM stromal cell cultures were established from patients who received allogeneic orautologousBMT for acute lymphoblastic leukemia,Hodgkin‘s disease, or non-Hodgkin’s lymphoma. These cuttures were then compared with normal donor BM stromal cell cultures for expression of adhesion molecules and the capacity t o support the adhesion and interleukin-7 (IL7)-dependent growth of normal B-cell precursors. Analysisof BM stromal cell cultures established from 28 BMT recipients showed a significantly reduced expressionof cell surface vascular cell adhesion molecule-l (VCAM-l/CDlOG), comparedwith nor- mal donorBM stromal cells.TransplantBM stromal cell CD106 expression was responsiveto regulatory cytokines in a manner qualitatively comparable with normal donor BM stromal cells. Thelevel of B-cell precursor adhesion to transplant BM stromal cells correlated with the level of CD106 expression. Of 19 evaluable transplant BM stromal cell cultures, eight exhibited a reduced capacity to support the growth of CD19+/lightchain- normal B-cell precursors. The capacity of transplant BM stromal cells t o support B-cell precursor growth correlated with thelevel of CD106 expression, and the level of B-cell precursor adhesion. Our collective results may provide new mechanistic insight into why B-cell recoveryis delayed post-BMT and underscorethe importance of VCAM-1ICDlO6 in regulating B lymphopoiesis. 0 1995 by The American Society of Hematology. B was motivated by the well-known B-cell immune deficiency that is frequently present in recipients of allogeneic and autologous BMTt4 (and references therein). The kinetics of immune reconstitution post-BMT exhibit a general pattern: CD8’ cytotoxic T cells, monocytes, and neutrophils reach normal numbers in peripheral blood within 1 month, whereas CD4’ helper T cells and B cells are more delayed in appearance.I4B-cell dysfunction in the early (3 months) post-BMT period has been attributed to increased T-cell suppression, decreased T-cell help, or failure to recapitulate B-cell ontogeny because of chronic graft-versus-host d i ~ e a s e . Not~~-~~ withstanding the insight provided by these studies, the mechanism underlying the profound reduction in circulating B cells during the early post-BMT period has not been elucidated. The results in the current study define heretofore unidentified deficiencies in the capacity of BM stromal cells derived from BMT recipients to support the adhesion and growth of B-cell precursors. LYMPHOPOIESIS occurs exclusively in the bone marrow (BM) of adult mammals and requires the regulated processing of developmental signals from both cellular and extracellular matrix components in the BM microenvironment. BM stromal cells, a complex array of nonhematopoietic fixed tissue cells in the medullary cavity, play a crucial role in murine B-cell development.’” The development of a long-term murine BM culture that supports the growth of early B-lineage cells has facilitated analyses of stromal cell f ~ n c t i o n We . ~ have developed an in vitro BM stromal cell culture that supports the interleukin-7 (IL-7)-dependent growth of normal human B-cell precursor^.^ Recent studies have shown that CD19+/CD34+ pro-B cells are the 1L-7responsive cells in our BM stromal cell culture, whereas CD19+/CD34- pre-B cells are completely nonresponsive to IL-7.’ Our human BM culture, and similar cultures developed by all exhibit an absolute dependency Bof cell precursor growth on an intact BM stromal cell microenvironment. Several studies have found that the primary adhesive interaction between B-cell precursors and BM stromal cells is mediated byvery late antigen-4 (VLA-4, also designated CD49dKD29) and vascular cell adhesion molecule-l (VCAM-I, also designated CD106), re~pectively.~-” Miyake et a1’0.’2 reported that monoclonal antibody (MoAb) to CD106 and CD49dCD29 inhibit the outgrowth of murine lymphoid cells in long-term BM cultures. Mouse MoAb to the CD49d and CD29 subunits of human VLA-4 inhibit the growth of terminal transferase+ human lymphoid progenit o r ~ .However, ~ Kaisho et all3 reported that anti-CD106 failed to inhibit the growth of the murine pre-B cell line DW34 on human SV40 transformed BM stromal cell lines known to express CD106. Given the importance of an intact BM stromal cell microenvironment for sustaining normal murine B lymphopoiesis,*.*we were interested in developing a strategy to evaluate the role of BM stromal cells during human B-cell ontogeny. TO achieve this goal, we characterized the B-lymphopoietic supportive capabilities ofBM stromal cells isolated from patients undergoing BM transplantation (BMT). Our study Blood, Vol 86, No 7 (October 1). 1995:pp 2833-2841 MATERIALS AND METHODS Cells. BM from normal 18- to 21-week-old human fetuses, normal adult donors, and BMT recipients was obtained in accordance From the Department of Laboratory Medicine/Pathology and the Bone Marrow Transplant Program, University of Minnesota Medical School, Minneapolis. Submitted October 28, 1994; accepted May 26, 1995. Supported by Grants No. POI CA-21737 and R01 CA-31685from the National Institutes of Health and theMinnesota Medical Foundation. B.N.D. was the recipient of a predoctoralfellowship from National Institutes of Health Immunology Training Grant No. T32 AI07313. Address reprint requests to Tucker W. LeBien, PhD, Box 609 UMHC, Department of Laboratory MedicindPathology, University of Minnesota Medical School, Minneapolis, MN 55455. The publication costs of this article were defrayed in part by page charge payment. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C. section 1734 solety to indicate this fact. 0 1995 by The American Society of Hematology. 0006-4971/95/8607-0017$3.00/0 2833 From www.bloodjournal.org by guest on February 6, 2015. For personal use only. 2834 with the guidelines of the University of Minnesota Committee on the Use of Human Subjects in Research. CD10f/CD19'Aight chainB-cell precursors were isolated from human fetal BM using magnetic bead depletion, as previously described." Adult BM stromal cells were established from normal donors." Briefly, normal adult BM was centrifuged on Ficoll-Hypaque gradients (Sigma Chemical CO, St Louis, MO). Then, 10 to 40 x lo6 interface cells were cultured in individual T75 tissue culture flasks containing 10 mL of EX-CELL 320 (JRH Biosciences, Lenexa, KS) supplemented with 10% fetal calf serum (FCS), 100 units/mL penicillin, and 100 pglmL streptomycin. The adherent stromal cells reached confluence in 7 to 14 days and were passaged twice in EXCELL 320/10% FCS. At this point, we had typically generated four to nine T75 flasks of normal donor BM stromal cells in approximately 40 days. Normal donor BM stromal cells were used at second or third passage. Transplant BM stromal cell cultures were initiated from BM aspirates (2 to 10mL) obtained from individuals receiving autologous or allogeneic BMT for B-cell precursor-acute lymphoblastic leukemia (BCP-ALL), Hodgkin's disease (HD), or non-Hodgkin's lymphoma (NHL). The conditioning regimens and posttransplant therapies administered to these patients are described elsewhere.22.z3BM aspirates were obtained at 21 or 28 days post-BMT from all patients. Recent analysis of the cellularity of these day 2l/day 28 post-BMT marrows indicates that they contain from 1% to 100% of the nucleated cell concentration of normal donor BM. BM was washed twice inRPM1 1640/2% FCS (Hyclone, Ogden, UT), and the cellular components were plated into a T25 tissue culture flask containing EX-CELL 320/20% FCS. Nonadherent cells were washed off 1 to 3 days later. Adherent cells were maintained in EX-CELL 320/ 20% FCS and monitored for growth by light microscopy. Cultures exhibiting growth initially appeared as foci of adventitial reticular cells that underwent expansion tonear confluence within 7 to 14 days. The adherent cell contents of T25 flasks were then expanded into individual T75 flasks containing EX-CELL 320120% FCS. Once the stromal cells reached confluence (7 to 14 additional days), they were passaged twice using txypsiniEDTA. At this point, we had typically generated four to nine 'I75 flasks of transplant BM stromal cell cultures in approximately 54 days. Successfully established second or third passage transplant BM stromal cell cultures were maintained in EX-CELL 320/0% FCS without morphological changes or loss of viability, for greater than 6 months. Stromal cell cultures were successfully established from 27 BMT patients, referred to by unique patient numbers (UPN 1-27). Of the 27 cultures, 15 were from patients with BCP-ALL (UPN 1-15), 8 were from NHL (UPN 16-23), and 4 were from HD (UPN 24-27). Eleven BCP-ALL patients received allogeneic BMT and 4 received autologous BMT, all 8 NHL patients received autologous BMT, and 1 HD patient received allogeneic BMT and 3 received autologous BMT. All 27 BMT stromal cell cultures were evaluated for expression of VCAM-I/CD106. However, logistical problems precluded evaluation of all 27 for the capacity to support adhesion and growth of B-cell precursors. Anribodiesand cytokines. The adhesion molecules recognized by MoAb in the current study have several different designations. For purposes of continuity, we will use the CD nomenclature throughout. Therefore, PECAM-1 = CD31, H-CAM = CD44, JCAM-I = CD54, VCAM-1 = CD106, the a subunit of LFA-I = CDlla, the 8 2 subunit of LFA-I = CD18, the a1 subunit of VLA-1 = CD49a. the a 2 subunit of VLA-2 = CD49b, the a 3 subunit of VLA-3 = CD49c. the a 4 subunit of VLA-4 = CD49d, the a 5 subunit of VLA-5 = CD49e, the a 6 subunit of VLA-6 = CD49f, the @ lsubunit of VLA1-6 = CD29 and the a subunit of the vitronectin receptor = CD51. The VLA-4, VLA-S, and LFA-I heterodimers will be referred to as CD49dCD29, CD49e/CD29, and CD1 laICD18, respectively. 4B9/anti-CD10624and LB2/anti-CD54" were gifts from Drs John DITTELANDLEBIEN Harlan and Ed Clark (both from the University of Washington, Seattle). PSDZ/anti-CD29, P2G12/anti-CD31, P3H9-3- llanti-CD44, TS217/anti-CD49a, PlHS/anti-CD49b, PlBS/anti-CD49c, P4C2/ anti-CD49d. PlD6/anti-CD49e, GOH3/anti-CD49f, P3G8/anti-CD5I were gifts from Dr Elizabeth Wayner (Fred Hutchinson Cancer ReP8B1-2/anti-CD106 and P4G11-2/ search Center, Seattle, WA).26-Z* anti-CD54 were produced by immunizing mice with IL-18-induced adult BM stromal cells. The specificity of the latter two MoAbs was confirmed by immunoprecipitation. GH12 and ED11 are CD106 specific MoAb were kindly provided by Dr Laurelee Osbom (Biogen, Cambridge, MA)?9 Hybridoma cells secreting W6/32/antiHLA-A, B, C, and L243/anti/MHC class I1 were obtained from the American Type Culture Collection (Rockville, MD). JS/anti-CDlO was purchased from Coulter Immunology (Hialeah, FL). Hybridoma cells secreting 25Cllanti-CD19 were kindly provided by Dr Stephen Peiper (University of Louisville School of Medicine, Louisville, KY). 25C1 was conjugated to phycoerythrin (PE) using standard methods.3"HPCA-Uanti-CD34 and Leu-IZ-PE/anti-CD19 were purchased from Becton Dickinson Immunocytometry Systems (San Jose, CA). IgG1, IgG2a, and IgG2b control mouse myeloma proteins were purchased from Organon Teknika-Cappel (Durham, NC). F(ab'), goat antimouse Ig-FITC was purchased from Tago, Inc (Burlingame, CA). Recombinant human IL-18, recombinant human IL-4, and porcine transforming growth factor-8 (TGF-8) were obtained from R & D Systems (Minneapolis, MN). Recombinant human IL-7 was obtained from PeproTech Inc (Rocky Hill, NJ). Flow cytometry. Expression of cell surface molecules onBM stromal cells was analyzed by indirect immunofluorescent staining andflow cytometry, as previously described." BM stromal cells from normal donors and transplant recipients were dissociated from tissue culture flasks using Cell Dissociation Solution (Sigma Chemical CO).This nonenzymatic solution does not disrupt epitopes recognized by the MoAb used to characterize the stromal cells. Stromal cells were stained for the expression of CD10, CD29, CD31, CD34, CD44, CD49a-f, CD5 1, CD54, CD106, Class I major histocompatibility complex (MHC) and class 11 MHC using saturating concentrations of MoAb, counterstained with F(ab'), goat antimouse IgG-FITC, and fixed in 1% paraformaldehyde before analysis on a FACScan (Becton Dickinson, San Jose, CA) using CONSORT 30 software. Negative controls included mouse IgG,, IgGZ., or IgGZh myeloma proteins, Data are reported as percent positive cells or mean channel fluorescence (MCF) of 5,000 cells analyzed on a log scale. The influence of cytokines on BM stromal cell CD106 and CD54 expression was conducted as previously described." Adhesion assay. Adhesion of CDlO'ilight chain- B-cell precursors to normal and transplant BM stromal cells was performed as previously described." Briefly, 50,000 Naz "CrO, radiolabeled CDlO'Aight chain- cells were incubated with normal or transplant BM stromal cells in the presence or absence of blocking MoAb for 2 hours at 37°C. After two washes to remove nonadherent cells, the stromal cell adherent B-cell precursors were quantitated on a y counter. Each experimental variable was tested in replicates of eight. Percent B-cell precursor adherence was calculated as follows: % Adherence = Mean Adherent cpm x 100 Total Input cpm B-cell precursor growth assay. B-cell precursors were cultured in vitro as previously described: with the following modifications. Normal or transplant BM stromal cells were seeded onto 96-well flat-bottom microtiter plates at 3,000 cells per wellin EX-CELL 320/10% FCS. After 3 days, the medium was switched to X-VIVO 1010% FCS and maintained until further use ( 2 to 4 days). Normal B-cell precursors were seeded onto normal or transplant BM stromal cells at approximately 20,000 to 40,000 cells per well in X-VIVO 10/0% FCS containing 10 ng/mL IL-7. The cultures were fed every From www.bloodjournal.org by guest on February 6, 2015. For personal use only. 2835 BONE MARROW STROMAL CELL VCAM-1 5 days with fresh X-VIVO 10/0% FCS containing 10 ndmL IL-7. CD19+ B-cell precursors were quantitated on days 0, 7, 14, and 21 by harvesting the cellular contents of the microtiter wells with Cell Dissociation Solution (Sigma) and stained for expression of CD19 using Leu-12-PE or 25C1-PE. For each condition, the cellular contents from 12 microtiter wells were pooled in groups of three wells, to provide four replicate data points. Polystyrene6.0 micron microspheres (Polysciences, Inc. Warrington, PA) were used to quantify cell numbers using the F A C S C ~ ~ ? . ~ ' Statistics. Statisticalsignificancewasdetermined bytheunpaired Student's t-test using Statworks (Cricket Software, Philadelphia, PA). Linear regression analysis and Pearson's correlation coefficient were determined using Cricket Graph (Cricket Software). RESULTS Transplant BM stromal cells express lower levels of CD104 compared with normal BM stromal cells. B-cell Stroma precursor/BM stromal cell adhesive interactions mediated by 30 CD49dCD29 and CD106 regulate the in vitro adhesion and B growth of normal B-cell precursors in human^'^^^" and g 25~ c e . ~ n . Therefore, ~ 2 we reasoned that an alteration in the BMT Recipient Normal Stroma U 'C v) expression and/or function of CD106 on BM stromal cells v) Q) 20after BMT may help explain the delayed appearance of peL n 0 A ripheral blood B cells so frequently observed posttransG 15BM aspirates from 73 BMT recipients were colt lected on day +21 or +28 posttransplant, and cultured as v) n described in Materials and Methods. Stromal cell cultures u were successfully established from 27 patients (see Materials e Q and Methods). No correlation was observed between the Q) success or failure in establishing transplant BM stromal cell I: cultures relative to the hematopoietic disorder, type of transplant (allogeneic or autologous), age of the recipient, or BMT Recipient Normal number of remissions patients had experienced at the time Stroma Stroma their marrows were cultured. We compared the CD106 fluorescence intensity on BM Fig 1. Expression of CD106 and CD54 on normal and transplant stromal cells established from 12 normal donors and 27BMT stromal cells. BM stromal cells from 27 transplant recipients IO) and recipients. As shown in Fig lA, the mean CD106 MCF on 12 normal donors (A) were analyzed for the expression of CD106 (A) and CD54(B1 by indirect immunofluorescence on a FACScan. The normalBM stromal cells was 23.4 9.8 (range, 5 to 36), individual data points represent the CD106 or CD54 M W minus the whereas the mean CD106 MCF on transplant BM stromal MCF of the isotype control. If an individualtransplant or normal strocells was 14.8 5 8.7 (range, 2 to 38). This difference was mal cell culture was analyzed more thanonce, the value represented significant (P < .Ol). In contrast, Fig 1B shows that the in (A) and (B) is the mean of all observations. CD54 MCF on normal BM stromal cells was6.7 2 4.7 (range, 2 to 18), whereas the CD54 MCF on transplant BM stromal cells was 6.8 t 5.7 (range, 0 to 26). Even though stained with MoAb specific for CD106 domain 1 (MoAb the transplant BM stromal cells analyzed had a statistically 4B9), the domain 1-2 interface (P8B1-2), and domain 4 significant reduction in the intensity of CD106 expression, (GH12). The results in Fig 2 clearly demonstrate thatall their expression of CD10, CD29, CD44, CD49a, CD49b, three anti-CD106 MoAb stain both normal and transplant CD49c, CD49e, CD51, and class I MHC was indistinguishBM stromal cells. Furthermore, normal and transplant BM stromal cells express the 7 Ig form of CD106, as indicated by able from normal BM stromal cells (data not shown). CD106 cell surface expression on normalBM stromal positive staining with the CD106 domain 4-specific MoAb cells exhibited minor fluctuation as a function of time in GH12. A second MoAb specific for CD106 domain 4 (ED1 1) culture, but expression was essentially unchanged for periods stained normal and transplant BM stromal cells in an identiup to 4 months in serum-free medium (data not shown). cal manner to MoAb GH12 (data not shown). The low-level CD106 staining in Fig 2 (similar to our previous study") Expression of the 7 Ig form of CD104 on normal and transplant BM stromal cells. Because the 4th Ig domain does not preclude the possibility that CD106 negative stroin the 7 Ig domain form of CD106 can be alternatively mal cells exist. However, they would be present in normal spliced to yield a 6 Ig domain form of CD106,32.33 we examand transplant BM stromal cell cultures. ined BM stromal cells obtained from both normal donors Cytokine regulation of CD104 on normal and transplant and transplant recipients for the expression of these two BM stromal cells. In previous studies we showed that cell CD106 isoforms. BM stromal cells cultured from one normal surface expression of CD106 on normal BM stromal cells donor and from transplant recipients UPN 25 and 26 were is upregulated by the cytokines L-lg and IL-4, and down- From www.bloodjournal.org by guest on February 6, 2015. For personal use only. DIlTEL AND LEBIEN 2836 1 NormalStroma MCF=55 UPN 26 UPN 25 1 MCF=161 Domain 1 1 MCF=43 MCF=14 Domain Domain4 FluorescenceIntensity Fig 2. Expression of the 7-19 isoform of CD106 on BM stromal cells from a normal donor and Hodgkin's disease transplant recipients UPN 25 and 26. B M stromal cells were stained by indirect immunofluorescence with anti-CD106 MoAb 489. P8B1-2, and GH12 at 10 pg/mL to detect CD106 "19-like" domains 1,1/2 interface, and domain 4, respectively, and analyzed on a FACScan. Expression of CD106 isrepresented by solid lines and the isotype control is represented by the dotted lines in the top panel of histograms. The CD106 MCF is indicated in the upper righthand corner of each individual histogram. regulated by TGF-D." The cytokine regulated increase or decrease in CD106 led to a corresponding increase or decrease in the adhesion ofB-cell precursors.'' The data in Table I show that treatment of normal and transplant BM stromal cells with IL-ID and IL-4 leads to an increase in CD106 expression, and an increase in B-cell precursor adhesion. Conversely. incubation of normal BM stromal cells with TGF-/3 leads to a reduction in CD106 expression and a corresponding decrease in B-cell precursor adhesion. Evaluation of the effect of TGF-Don transplant BM stromal cells was compromised by the decreased CD106 expression present on the majorityof transplant BM stromal cells (Table 1 and Fig 1 ). Using MoAb toa panel of adhesion molecules, we showed that B-cell precursor adhesion to transplant BM stromal cells was mediated by CD49d/CD29 and CD106 (data not shown), comparable to our earlier studies with normal BM stromal cells." Trurlsplant BM s t r o n d cells from n subset of patients .show CI reduced cnpacih t o support tire in vitro proliferation of B-cell precursors. We usedanIL-7/BM stromal cell culture to examine the capacity of transplant BM stromal cells to support the in vitro growth of normal B-cell precur- sors. As shown in Table 2,8 of the 19 transplant BM stromal cell cultures examined exhibited a reduced capacity to supportB-cell precursor proliferation (<90% of control BM stromal cells at all three timepoints, and a mean < 80%). The remaining 1 1 transplant BM stromal cell cultures supportedthe in vitro growth of B-cell precursors similar to normal stromal cells (>90% of control stroma for at least one time point, and a mean > 80%). Statistical comparison of the 8 cultures with reduced supportive capacity (mean ? SD = 66.2% ? 6.8%) to the 1 1 cultures with normal supportive capacity (mean ? SD = 89.6% ? 5.9%) showed a P value of < .OOl (unpaired t-test). The reduced support of Bcell precursor growth observed with some transplant BM stromal cells could notbe explained by simple differences in plating densities of the BM stromal cells. When normal BM stromal cells were seeded at densities of 6,000, 3,000, 1,500, or 750 cells/well, similar numbers of CD19' cells were recovered fromeach culture 14 days later (data not shown). Adhesion of B-cell precur.sors is correlated to the expression of CDl06, but not CD54, on transplant BM stromal cells. We have previously reported" and demonstrated in Table l , that B-cell precursor adhesion to normal and trans- ROMAL From www.bloodjournal.org by guest on February 6, 2015. For personal use only. BONE MARROW CELL VCAM-1 2837 Table 1. Adhesion of B-Cell Precursorsto Normal and BMT Stromal Cells CorrelatesWith the Expression of CD106 Normal Stroma UPN 9 CD106' Medium alone IL-lp (100 pg/mL) IL-4 (10 ng/mL) TGF-8 (1 ng/mL) CD106 CD106 Fluorescence Condition UPN 21 Fluorescence % Adhesion* 23 -c 1.2 31 I 1.0 39 2 1.1 19 2 1.0 26 36 34 11 19 40 18 33 34 14 % Adhesion 14 -t 0.8 33 2 0.8 2 1.8 19 2 0.7 28 Fluorescence % Adhesion 8 16 15 2 0.5 21 2 0.6 2 1.2 11 i 0.6 6 ~ Numbers represent the CD106 MCF value of a single stromal cell culture measured on a FACScan. t Values represent the mean t SE of eight replicates. plant BM stromal cells parallels the cytokine regulated expression of CD106. Linear regression analysis comparing the level of cell surface CD106 expression by transplant BM stromal cells with the ability of the same stromal cells to support the adhesion of B-cell precursors showed a linear relationship (Fig 3A, R = .638, P = .006). In contrast, no linear relationship was observed between B-cell precursor adhesion and CD54 expression (Fig 3B, R = .152, P = S73). Expression of CD106 on transplant BM stromal cells is correlated to the level of IL-7-induced B-cell precursor Table 2. A Subset of BMT Recipient Stromal Cells Exhibits a Reduced Capacityto Support the In Vitro Growthof Normal B-Cell Precursors B-Cell Precursor Growth* UPN Diseasenransplanr Day7 Day 14 Day21 Mean 6 7 8 9 10 11 12 14 16 17 18 19 20 21 22 23 25 26 27 ALL-ALL0 71t 56t 95 86 81t 80t 102 84 69t 92 102 58 66t 82t 84t 92 72 48 98 68t 59t 95 92 69t 60 82 78 52t 100 93 100 80t 82t 49 t 123 98 98 106 56t 57t 93 68 53t 55t 64 102 63t 65t 57t 94 82 68t 65t 83 88 61t 97 99 88 72t 79t 63t 94 84 84 93 ALL-AUTO NHL-AUTO HD-AUTO 100 101 106 71t 73t 56t 68 83 105 75 Abbreviations: ALL-acute lymphoblastic leukemia; NHL, non-Hodgkin's lymphoma; HD, Hodgkin's disease; ALLO-allogeneic, AUTO-autologous. Values represent the percentage of CD19' B-lineage cells recovered from transplant BM stromalcells compared with the number of CD19' B-lineage cells recovered from normal BM stromal cells. The percentage was derived by dividing theabsolute CD19' cell number recovered on transplant stromal cells bythe absolute CD19'cell number recovered on normal stromalcells. The mean value is theaverage of the three time points. t Values defined as having a reduced capacity to support the in CD19' B-cell precursors (<go% of control stromal cells vitro growth of at all three timepoints and a mean of <EO%). proliferation. Because the in vitro proliferation of normal human B-cell precursors is absolutely dependent on BM stromal cells: linear regression analysis was used to compare transplant BM stromal cell CD106 expression with the ability to support B-cell precursor proliferation. As shown in Fig 4A, the expression of CD106 was linearly related to the recovery of CD19+ cells on day 7 ( R = .459, P = .07). However, this relationship was lost by day 14 (Fig 4B, R = .l18, P = .66). Likewise, no linear relationship existed on day 21 ( R = .145, P = .58)(data not shown). When CD54 expression by transplant BM stromal cells was compared with the recovery of CD19' B-cell precursors on days 7 (Fig 4C) and 14 (Fig 4D), no linear relationship was observed. Adhesion of B-cell precursors to transplant BM stromal cells is correlated to the proliferation of B-cell precursors. Because CD106 expression was correlated to B-cell precursor adhesion (Fig 3A) and proliferation (Fig 4A), we analyzed the relationship between the ability of transplant BM stromal cells to support the adhesion and proliferation of Bcell precursors. The data in Fig 5 show a linear relationship between adhesion of B-cell precursors and the maximum recovery of CD19+ cells on either day 7, 14, or 21 ( R = S38, P = .03).Weaker correlations between adhesion and proliferation of B-cell precursors were observed on days 7 ( R = .263, P = .14), 14 ( R = .377, P = .12), and 21 ( R = ,322, P = .16). DISCUSSION Studies of human B-cell ontogeny have been facilitated by the development of BM stromal cell-dependent cultures that support the in vitro growth of normal B-cell precursors?6'8 Adhesion of normal B-cell precursors to BM stromal cells is primarily mediated by CD49dCD29 and CD106.9-LL MoAb to murine CD49dCD29" and CD106" block B lymphopoiesis in Whitlock-Witte cultures, and MoAb to the CD49d and CD29 subunits of human VLA-4 inhibit the growth of TdT+ lymphoid progenitors? However, evidence implicating CD106 in functional events beyond the initial adhesion of human B-cell precursors to BM stromal cells has not been reported. The delay in B-cell reconstitution after BMT has been known for some time.I4 Given the lack of a unifying mechanistic model to explain this delay, we hypothesized that an abnormality in BM stromal celVB-cell precursor interactions may be involved. The rationale underlying this hypothesis rests partially on the large body of evidence identifying the toxic effects of infectious agents, chemical agents, and ionizing irradiation on the BM micro- 0 From www.bloodjournal.org by guest on February 6, 2015. For personal use only. 2838 DllTEL AND LEBEN A C .-0 150 v) v) P) L. n x W 100 (D 0 F 50 P V 1 l L o ! 75 50 B -= . , . II m , . , . , . I 25 B Cell PrecursorAdhesion B A 400 C .-0 v) v) 300 4 x W d v) P V A A ' 25 50 75 A 100 125 150 B Cell PrecursorAdhesion Fig 3. Relationship between CD106 expression and CD54 expression on transplant BM stromal cells and their capacity to support the adhesion of B-cell precursors. B-cell precursor adhesion on the horizontal axis is represented as the adherent cpm of B-cell precursors to transplant BM stromal cells, divided by the adherent cpm of B-cellprecursors to normal BM stromal cells, multiplied by 100. CD106 (A) or CD54 (B) expression onthe vertical axis is represented as the CD106 or CD54 MCF (minus the isotype control MCF) of transplant BM stromal cells, divided by the CD106 or CD54 MCF (minus the isotype control MCF) of normal BM stromal cells, multiplied by 100. Eachindividualdata point represents CD106 expression (A) plotted against B-cell precursor adhesion forUPN 6-12, 14, 16, 17,20-23, and 25-27, or CD54 expression (B) plotted against B-cell precursor adhesion for UPN 6-12, 14, 16, 17, 20-22, and 25-27. If an individual transplant BM stromal cell culture was analyzed more than once, the value represented is the mean of all observations. Analysis of transplant and normal BM stromal cells for CD106and CD54 expression and adhesion of B-cell precursorswas conducted on the same day for each individual data point. e n v i r ~ n m e n tTherefore, .~~ we reasoned that one consequence of this BM damage might be an alteration in the capacity of BM stromal cells to support the adhesion and growth of Bcell precursors. This could, in turn, delay the appearance of normal B-cell numbers in peripheral blood. Although normal human B-cell precursors can be grown on BM stromal the technology has not developed to the point where limiting numbers (ie, the number of Bcell precursors that would be present in BM aspirates at day 28 (post-BMT) can be routinely grown. We therefore compared the functional integrity of BM stromal cells established from BMT recipients and normal donors for their adhesion molecule expression and the capacity to support the adhesion and growth of normal B-cell precursors. The strategy we employed was to establish BM stromal cell CUItures from patients who had received allogeneic or autologous BM transplants for BCP-ALL, NHL, or HD. We SUCcessfully established BM stromal cells from 27 of 73 patients, but observed no relationship between successful establishment and type of transplant, underlying disease, or recipient age. One explanation for the failure to establish confluent BM stromal cell cultures may have been damage from irradiation andor chemotherapy, resulting in extreme hypocellularity in the BM aspirates used to initiate the cultures (see below). Although the hypocellularity of recipient marrowat 21 to 28 days post-BMT resulted in a consistent delay in the establishment of transplant BM stromal cell cultures compared withnormal donor BM, the cell surface phenotype was indistinguishable, with the exception of CD106. The level of CD106 was significantly lower on BMT recipient stromal cell cultures compared with normal donors (Fig 1 ), buttherewasno apparent abnormality in CD106 isoform expression (Fig 2 ) or regulated response to cytokine stimulation (Table 1). The reduced CD106 expression has several possible explanations including: outgrowth of a subpopulation of BM stromal cells expressing low CD106, senescence of transplant BM stromal cells, or inheritable changes in BM stromal cell gene expression secondary to DNA damage caused by irradiation or chemotherapy. The former possibility seems unlikely for several reasons. First, 16 distinct cell surface antigens identified by MoAb were identical in expression on normal and transplant BM stromal cells, with the exception of CD106. In addition, cytokine responsiveness based onregulated expression of CD106 was essentially the same (Table l), andbothnormaland transplant BMstromal cells expressed the 7 Igdomain isoform of CD106 (Fig 2). Thus, by the criteria of constitutive expression of many distinct gene products, and cytokine-regulated expression of CD106, the predominant cellular component of normal and transplant BM stromal cell cultures was the same. We cannot rule out the possibility that small numbers of macrophages were presentin some of the stromal cell cultures, and macrophage-derived cytokines (eg, IL- 1) can regulate CD106 expression. Although we didnot monitor macrophage content in all the BM stromal cell cultures used in the current study, our previous studies have shown that CD 1 1b+/HLA-DR+macrophages are very low in number or undetectable in second passage BM stromal cells." Transplant BM stromal cells deficient in the capacity to support the adhesion and growth of B-cell precursors may have been senescent, due to a potentially increased number of doublings required to generate confluent monolayers. We tried to control for this possibility by classifying our BM stromal cell cultures using criteria previously used to categorize aging fibroblasts in vitro.?' We only used normal and transplant BM stromal cell cultures that displayed morphologic characteristics of mitotic and postmitotic fibroblasts; that is, fibroblasts able to adhere, spread, and form confluent monolayers? Transplant and normal BM stromal cell cul- From www.bloodjournal.org by guest on February 6, 2015. For personal use only. 2839 BONE MARROWSTROMALCELLVCAM-1 200 A W - (11 B n 100 nl 75 50 25 100 . .D . , D . , . , . 125 B CellPrecursorGrowth B CellPrecursorGrowth A 4000 m P W" P . A AA 200200 v) n P A A 100100 A O 25 . . A . 50 A A . . 75 . U ' 100 P A " A A n 125 B CellPrecursorGrowth B CellPrecursorGrowth Fig 4. Relationship between CD106 expression andCD54 expression on transplant BM stromal cells and their cqpacity to support the IL7-induced proliieration of Bsell precursors. B-cell precursorproliieration on the horizontal axis is represented as absolute numbersof CD19+ cells recoveredfrom transplant BM stromal cells, divided by the absolute numbers of CD19+ cells recoveredfrom normal BM stromal cells, multiplied by 100. CD106 (A, B) or CD54 IC, D) expression on the vertical axis is representedas the CD106 or CD54 MCF (minus the irotype control MCF) of transplant stromal cells divided by the CD106 or CD54 MCF(minusthe isatype control MCFI of normal stromal cells, multiplied by 100. Individual data points represent CD106 expression plotted against B a l l precursor proliieretion on day 7 (AI and day 14 (B) for UPN 6-12,14,16,17,20-23, and 25-27, or CD54 expression plotted against B e l l precursor proliferation on day 7 (C) and day 14 (D) for UPN 6-12, 14, 16, 17,20-22, and 25-27. If an individual tranrplant BM stromal cell was analyzed morethan once, the value representedis the mean of a11 observations. Analysis of transplant and normal BM stromal cells for CD106 and CD54 expression was conducted the same day the Bsell precursor proliferation assay was initiated. tures were both used at second or third passage and displayed indistinguishable morphological characteristics and growth kinetics. The optimal approach for initiation and establishment of stromal cell cultures would employ positive selection (perhaps using anti-CD106 MoAb) of BM stromal cell precursors (ie, the adventitial reticular cells that adhere to tissue culture flasks and undergo expansion), and subsequent plating of equal numbers in culture on day 0. Transplant BM stromal cell cultures expressing reduced levels of CD106 may have acquired genetic changes induced by irradiation or chemotherapy. The reduced expression of cell surface CD106 (Fig 1) could reflect alterations in transcription, translation, or protein stability. CD106 expression is regulated differently in individual cell types. For example, CD106 is only expressed on endothelial cells following cytokine ~timulation.~~*~' Alternatively, BM stromal cellsg"' and follicular dendritic cells3' constitutively express CD106, which can be increased by specific cytokines. Although transcriptional regulation ofBM stromal cell CD106 has not been characterized, transcription of CD106 in endothelial cells is known to be regulated by two NF-kB sites within the CD106 promoter.3941Independent of the mechanism by which CD106 expression is regulated following cytokine stimulation of BM stromal cells, this process does not appear to be grossly altered in stromal cells established from transplant recipients (Table 2). Thus, the mechanism by which constitutive CD106 expression is reduced in BMT recipient stromal cells remains to be determined. Although not investigated in the current study, alterations in cytokine production could also be involved. TGF-P downregulates CD106 expression in normal BM stromal cells," and CD106 is constitutively expressed by BM stromal cells established under Dexter culture conditi0ns.4~~~ Thus, overexpression of stromal cell TGF-P could lead to reduced levels of CD106 expression, in addition to exerting a general antiproliferative effect on a variety of lymphohematopoietic cells. It is noteworthy that increased levels of TGF-P production by BM stromal cells from patients with chronic lymphocytic leukemia have been reported.& Our inability to establish transplant BM stromal cell cultures from -60% of BM aspirates may reflect the intrinsic hypocellularity of recipient BM in the first several weeks posttransplant. Indeed, some BM aspirates gave rise to adherent cells with only a limited capacity to grow, thereby yielding partially confluent cultures that could not be expanded for functional studies. The toxic effects of ionizing From www.bloodjournal.org by guest on February 6, 2015. For personal use only. 2840 DITTEL AND LEBIEN 150 to support B-cell precursor adhesion and growth. The reduced CD106 expression could result in a lower threshold of cell signaling events delivered to B-cell precursors through CD49dCD29, leading to a decrease in B-cell precursor proliferation. However, given the array of toxic effects exerted by irradiation and chemotherapy on the BM microenviron~ n e n tit, ~ is ~almost certain that additional abnormalities exist that compromise the B lymphopoietic supportive capacity of BM stromal cells. c .-0 v) Q c 125 2 100 75 ACKNOWLEDGMENT 50 m 1 50 75 100 125 150 B Cell Precursor Growth Fig 5. Relationship between the capacity of transplant BM stromal cells to support B-cell precursor adhesion and 117-induced proliferation of Bsell precursors. B-cell precursor proliferation on the horizontalaxis is represented asthe absolute number ofCDl9+ cells recovered from transplant BM stromal cells, dividedby the absolute number of CD19+cellsrecovered from normal BM stromal cells, multiplied by 100. B-cell precursor adhesion on the vertical axis is represented as the adherent cpm of Bsell precursors to transplant BM stromal cells, divided by the adherent cpm of B-cell precursors to normal BM stromal cells, multiplied by 100. Each individual data point represents the maximum recovery of CD19* cells on day 7,14, or 21 plotted against B a l l precursor adhesion forUPN 6-12, 14, 16, 17,ZO-23, and 25-27. If an individual transplantBM stromal cell was analyzed more than once, the value represented is the mean of all observations. Analysis oftransplant and normal BM stromel cells for edhesion of &cell precursorswas conducted the same day the B-cell precursor proliferation assay was initiated. irradiation on the BM microenvironment are l e g i ~ n . ~Ex~.~' periments in the mouse have noted damage to BM stromal cells after irradiation or chemotherapy, manifested as morphologically altered cytoplasmic organelles andplasma membranes, cytoplasmic vacuoles, and nuclear damage.34 Our difficulty in establishing confluent monolayers might find explanation in earlier murine studies. Whereas highdose-irradiated marrow sites showed no evidence of structural damage in situ, significant cell kill was observed after one to two traversals of the cell cycle in High-doseirradiated sites left undisturbed for 6 months showed significant repair of potentially lethal irradiation da1nage.4~Extrapolating these findings to our study, it is conceivable that some of our transplant BM stromal cell culture failures could reflect an inability to repair irradiation damage that culminated in premature stromal cell death in vitro. Other studies have noted heterogeneity in the radiosensitivity of human BM stromal cell lines (established from a single donor) to low-dose-rate irradiation." Therefore, it would seem highly possible, and even probable, that radiobiologic differences would exist in radiosensitivity and repair capacity of BM stromal cells from different transplant recipients. In conclusion, our results further illuminate the functional importance of CD106 expression on human BM stromal cells that support the IL-7-dependent growth of human B-cell precursors. We have shown that BM stromal cells isolated from transplant recipients have a reduced expression of CD 106, and this reduction correlates with a reduced capacity We thank Joanne Howard and the bone marrow transplant physicians for their generous assistance in providing bone marrow aspirates and Dr Michael Steinbuch for providing information on the clinical characteristics of the patients. Drs John Kersey and Daniel Weisdorf provided helpful comments on the manuscript. We thank Karen Nelson for assistance with word processing. Dr Laurelee Osborn (Biogen Corp. Cambridge, MA) kindly provided the GH12 and ED11 anti-CD106 Ab. We particularly thank Dr Steve Rich for his advice on statistical analyses. REFERENCES 1. Kincade PW, Lee G, Watanabe T, Sun L, Scheid MP: Cells and molecules that regulate B lymphopoiesis in bone marrow. Annu Rev Immunol 7:111, 1989 2. Dorshkind K: Regulation of hemopoiesis by bone marrow stromal cells and their products. Annu Rev Immunol 8:1l l , 1990 3. Whitlock CA, Witte ON: Long-term culture of B lymphocytes and their precursors from murine bone marrow. Roc Natl Acad Sci USA 79:3608, 1982 4. Wolf ML, Buckley JA, Goldfarb A, Law C-L, LeBien TW: Development of a bone marrow culture for maintenance and growth of normal human B cell precursors. J Immunol 147:3324, 1991 5. Dittel BN, LeBien TW: The growth response to IL-7 during normal human B cell ontogeny is restricted to B-lineage cells expressing CD34. J Immunol 154:58, 1995 6. McGinnes K, Quesniaux V, Hitzler J, and Paige CJ: Human B-lymphopoiesis is supported by bone marrow-derived stromal cells. Exp Hematol 19:294, 1991 7. Ryan DH, Nuccie BL, Abboud CN: Inhibition of human bone marrow lymphoid progenitor colonies by antibodies to VLA integrins. J Immunol 149:3759, 1992 8. Moreau I, Duvert V, Banchereau J, Saeland S : Culture of human fetal B-cell precursors on bone marrow stroma maintains highly proliferative CD20"" cells. Blood 81:1170, 1993 9. Ryan DH, Nuccie BL, Abboud CN, Winslow JM: Vascular cell adhesion molecule-l and the integrin VLA-4 mediate adhesion of human B cell precursors to cultured bone marrow adherent cells. J Clin Invest 88:995, 1991 IO. Miyake K, Medina K, Ishihara K, Kimoto M, Auerbach R, Kincade PW: A VCAM-like adhesion molecule on murine bone marrow stromal cells mediates binding of lymphocyte precursors in culture. J Cell Biol 114:557, 1991 11. Dittel BN, McCarthy JB, Wayner EA, LeBien TW: Regulation of human B-cell precursor adhesion to bone marrow stromal cells by cytokines that exert opposing effects on the expression of vascular cell adhesion molecule-l (VCAM-1). Blood 81:2272, 1993 12. Miyake K, Weissman L,Greenberger JS, Kincade PW: Evidence for a role of the integrin VLA-4 in lympho-hemopoiesis. J Exp Med 173:599, 1991 13. Kaisho T, Oritani K, Ishikawa J, Tanabe M, Muraoka 0, Ochi T, Hirano T: Human bone marrow stromal cell lines from myeloma and rheumatoid arthritis that can support murine pre-B cell growth. J Immunol 149:4088, 1992 14. Lum LG: The kinetics of immune reconstitution after human marrow transplantation. Blood 69:369, 1987 From www.bloodjournal.org by guest on February 6, 2015. For personal use only. BONE MARROW STROMAL CELL VCAM-1 15. Wimperis JZ, Brenner MK, Prentice HG, Thompson EJ, Hoffbrand AV: B cell development and regulation after T cell-depleted marrow transplantation. J Immunol 138:2445, 1987 16. Kiesel S, Pezzutto A, Moldenhauer G, Rainer R, Korbling M, Hunstein W, Dorken B: B-cell proliferative and differentiative responses after autologous peripheral blood stem cell or bone marrow transplantation. Blood 72:672, 1988 17. Bengtsson M, Smedmyr B, Festin R, Oberg G, Simonsson B, Tottennan TH: B lymphocyte regeneration in marrow and blood after autologous bone marrow transplantation: Increased numbers of B cells carrying activation and progression markers. Leuk Res 13:791, 1989 18. Kagan JM, Champlin RE, Saxon A: B-cell dysfunction following human bone marrow transplantation: Functional-phenotypic dissociation in the early posttransplant period. Blood 74777, 1989 19. Small T N , Keever CA, Weiner-Fedus S, Heller G, O’Reilly RJ, Flomenberg N: B-cell differentiation following autologous, conventional, or T-cell depleted bone marrow transplantation: A recapitulation of normal B-cell ontogeny. Blood 76:1647, 1990 20. Storek J, Ferrara S , Ku N, Giorgi JV, Champlin RE, Saxon A: B cell reconstitution after human bone marrow transplantation: Recapitulation of ontogeny? Bone Marrow Transplant 12:387, 1993 21. Villablanca JG, Anderson JM, Moseley M, Law C-L, Elstrom RL, LeBien T W : Differentiation of normal human pre-B cells in vitro. J Exp Med 172:325, 1990 22. Weisdorf DJ, Woods WC, Nesbit ME, Uckun F, Dusenbery K, Kim T, Haake R, Thomas W, Kersey JH, Ramsay NKC: Allogeneic bone marrow transplantation for acute lymphoblastic leukaemia: Risk factors and clinical outcome. Br J Haematol 86:62, 1993 23. Weisdorf D, Katsanis E, Verfaillie C, Ramsay NKC, Haake R, Garrison L, Blazar BR IL-laadministered after autologous transplantation: A phase I/II clinical trial. Blood 84:2044, 1994 24. Carlos TM, Schwartz BR, Kovach NL, Yee E, Rosso M, Osbom L, Chi-Ross0 G, Newman B, Lobb R, Harlan JM: Vascular cell adhesion molecule-l mediates lymphocyte adherence to cytokine-activated cultured human endothelial cells. Blood 76:965, 1990 25. Clark EA, Yokochi Y: Human B cell and B cell blast-associated surface molecules defined with monoclonal antibodies, In Bernard, A, Bournsell L, Dausset J, Milstein C, Scholossman SF (eds): Leukocyte Typing I. Human Leukocyte Differentiation Antigens. Berlin, Germany, Springer, 1984, p 339 26. Wayner EA, Garcia-Pardo A, Humphries MJ, McDonald JA, Carter WC: Identification and characterization of the T lymphocyte adhesion receptor for an alternative cell attachment domain (CS-l) in plasma fibronectin. J Cell Biol 109:1321, 1989 27. Wayner EA, Carter WC: Identification of multiple cell adhesion receptors for collagen and fibronectin in human fibrosarcoma cells possessing unique a and common p subunits. J Cell Biol 105:1873, 1987 28. Wayner EA, Carter WC, Piotrowicz RS, Kunicki TJ: The function of multiple extracellular matrix receptors in mediating cell adhesion to extracellular matrix: Preparation of monoclonal antibodies to the fibronectin receptor that specifically inhibit cell adhesion to fibronectin and react with platelet glycoproteins Ic-IIa. J Cell Biol 107:1881, 1988 29. Osbom L, Vassallo C, Benjamin CD: Activated endothelium binds lymphocytes though a novel bmding site in the alternately spliced domain of vascular cell adhesion molecule-l. J Exp Med 17699,1992 30. Coligm E,Kruisbeek AM, Margulies DH, ShevachEM, Stmber W: Current Protocols in Immunology. Greene Publishing Associates and Wiley-IntersEience, New York, N Y , 5.3.5 Supplement 3, 1992 31. Larson AW, LeBien Tw: Cross-linking CD40 on human B cell precursors inhibitsor enhancesgrowthdepending on the stage of development and the interleukin CO-stimulus. J Immunol 153:584, 1 9 9 4 32. Cybulsky MI, Fries JWU, Williams AJ, Sultan P, Davis VM, Gimbrone MA Jr, Collins T Alternative splicing of human VCAM1 in activated vascular endothelium. Am J Pathol 138:815, 1991 2841 33. Hession C, Tizard R, Vassallo C, Schiffer SB, Goff D, Moy P, Chi-Rosso G, Luhowskyj S, Lobb R, Osbom L: Cloning of an alternate form of vascular cell adhesion molecule-l (VCAM-l). J Biol Chem 266:6682, 1991 34. Greenberger JS: Toxic effects on the hematopoietic microenvironment. Exp Hematol 19:1101, 1991 35. Bayreuther K, Rodemann HP, Hommel R, Dittmann K, AIbiez M, Francz PI: Human skin fibroblasts in vitro differentiate along a terminal cell lineage. Proc Natl Acad Sci USA 8551 12, 1988 36. Rice GR, Munro JM, Bevilacqua M P Inducible cell adhesion molecule 110 (INCAM-110) is an endothelial receptor for lymphocytes. A CD1 IKD18-independent adhesion mechanism. J Exp Med 171:1369,1990 37. Osborn L, Hession C, Tizard R, Vassallo C, Luhowskyj S , Chi-Rosso G, Lobb R: Direct expression cloning of vascular cell adhesion molecule I, a cytokine-induced endothelial protein that binds to lymphocytes. Cell 59:1203, 1989 38. Clark EA, Grabstein KH, Shu CL: Cultured human follicular dendritic cells. Growth characteristics and interactions with B lymphocytes. J Immunol 148:3327, 1992 39. Iademarco MR, McQuillan JJ, Rosen CD, Dean DC: Characterization of the promoter for vascular cell adhesion molecule-l (VCAM-1). J Biol Chem 267:16323, 1992 40. Iademarco M F , McQuillan JJ, Dean DC: Vascular cell adhesion molecule 1: Contrasting transcriptional control mechanisms in muscle and endothelium. Proc Natl Acad Sci USA 90:3943, 1993 41. Shu H B , Agranoff AB, Nabel EG, Leung K, Duckett CS, Neish AS, Collins T, Nabel GJ: Differential regulation of vascular cell adhesion molecule 1 gene expression by specific NF-KBsubunits in endothelial and epithelial cells. Mol Cell Biol 13:6283, 1993 42. Eaves C J , Cashman JD, Kay RI, Dougherty T, Otsuka T, Gaboury LA, Hogge DE, Lansdorp PM, Eaves AC, Humphries RK: Mechanisms that regulate the cell cycle status of very primitive hematopoietic cells in long-term human marrow cultures. 11. Analysis of positive and negative regulators produced by stromal cells within the adherent layer. Blood 78:110, 1991 43. Teixido J, Hemler M E , Greenberger JS, Anklesaria P: Role of B, and B2 integrins in the adhesion of human CD34histem cells to bone marrow stroma. J Clin Invest 90:358, 1992 44. Simmons PJ, Masinovsky B, Longenecker BM, Berenson R, Torok-Storb B, Gallatin WM: Vascular cell adhesion molecule-l expressed by bone marrow stromal cells mediates the binding of hematopoietic progenitor cells. Blood 80:388, 1992 45. Liesveld JL, Abboud CN: Marrow stromal cell exposure to hematopoietic progenitors results in increased production of TGFp. Exp Hematol 22:769, 1994 (abstr) 46. Lagneaux L, Delforge A, Dorval C, Bron D, Stryckmans P: Excessive production of transforming growth factor-p by bone marrow stromal cells in B-cell chronic lymphocytic leukemia inhibits growth of hematopoietic precursors and interleukin-6 production. Blood 82:2379, 1993 47. Bierkens JG, Hendry JH, Testa NG: The radiation response and recovery of bone marrow stroma with particular reference to long-term bone marrow cultures. Eur J Haematol 43:95, 1989 48. Greenberger JS, Otten JA, Eckner RJ, Tennant RW: In vitro quantitation of lethal and leukemogenic effects of gamma irradiation on stromal and hematopoietic stem cells in continuous mouse bone marrow culture. Int J Radiat Oncol Biol Phys 8:1155, 1982 49. Gallini R, Hendry JH, Molineux G, Testa NG: The effect of low dose rate on recovery of hemopoietic and stromal progenitor cells in a-irradiated mouse bone marrow. Radiat Res 115:481, 1988 50. Fitzgerald TJ, Santucci MA, Harigaya K, Woda B, McKenna M, Sakakenny MA, Pierce JH, Kase K, Holland CA, Greenberger JS: Radiosensitivity of permanent human bone marrow stromal cell lines: effect of dose rate. Int J Radiat Oncol Biol Phys 15:1153, 1988 From www.bloodjournal.org by guest on February 6, 2015. For personal use only. 1995 86: 2833-2841 Reduced expression of vascular cell adhesion molecule-1 on bone marrow stromal cells isolated from marrow transplant recipients correlates with a reduced capacity to support human B lymphopoiesis in vitro BN Dittel and TW LeBien Updated information and services can be found at: http://www.bloodjournal.org/content/86/7/2833.full.html Articles on similar topics can be found in the following Blood collections Information about reproducing this article in parts or in its entirety may be found online at: http://www.bloodjournal.org/site/misc/rights.xhtml#repub_requests Information about ordering reprints may be found online at: http://www.bloodjournal.org/site/misc/rights.xhtml#reprints Information about subscriptions and ASH membership may be found online at: http://www.bloodjournal.org/site/subscriptions/index.xhtml Blood (print ISSN 0006-4971, online ISSN 1528-0020), is published weekly by the American Society of Hematology, 2021 L St, NW, Suite 900, Washington DC 20036. Copyright 2011 by The American Society of Hematology; all rights reserved.
© Copyright 2026