Mesenchymal Stem Cells Regulate Angiogenesis
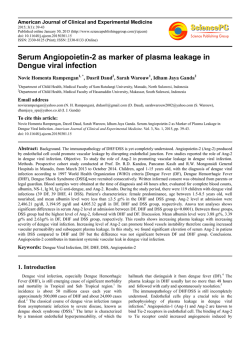
TISSUE-SPECIFIC STEM CELLS Mesenchymal Stem Cells Regulate Angiogenesis According to Their Mechanical Environment GRIT KASPER,a,b NIELS DANKERT,a JENS TUISCHER,a MORITZ HOEFT,a TIMO GABER,c JULIANE D. GLAESER,a,d DESIREE ZANDER,a MIRIAM TSCHIRSCHMANN,e MARK THOMPSON,a GEORG MATZIOLIS,a GEORG N. DUDAa,b a Musculoskeletal Research Center Berlin, bBerlin-Brandenburg Center for Regenerative Therapies, and cDepartment of Rheumatology and Clinical Immunology, Charite´–Universita¨tsmedizin, Berlin, Germany; dDepartment of Biology, Chemistry, and Pharmacy, Free University Berlin, Berlin, Germany; eMedical Biotechnology Department, University for Technologies, Berlin, Germany Key Words. Angiogenesis • Endothelial cells • Mesenchymal stem cells • Mechanical loading • Regeneration • Vascularization ABSTRACT In fracture and bone defect healing, MSCs largely drive tissue regeneration. MSCs have been shown to promote angiogenesis both in vivo and in vitro. Angiogenesis is a prerequisite to large tissue reconstitution. The present study investigated how mechanical loading of MSCs influences their proangiogenic capacity. The results show a significant enhancement of angiogenesis by conditioned media from mechanically stimulated compared with unstimulated MSCs in two-dimensional tube formation and three-dimensional spheroid sprouting assays. In particular, proliferation but not migration or adhesion of endothelial cells was elevated. Promotion of angiogenesis was dependent upon fibroblast growth factor receptor 1 (FGFR1) signaling. Moreover, stimulation of tube forma- tion was inhibited by vascular endothelial growth factor receptor (VEGFR) tyrosine kinase blocking. Screening for the expression levels of different soluble regulators of angiogenesis revealed an enrichment of matrix metalloprotease 2, transforming growth factor 1, and basic fibroblast growth factor but not of vascular endothelial growth factor in response to mechanical stimulation. In conclusion, mechanical loading of MSCs seems to result in a paracrine stimulation of angiogenesis, most likely by the regulation of a network of several angiogenic molecules. The underlying mechanism appears to be dependent on the FGFR and VEGFR signaling cascades and might be mediated by an additional cross-talk with other pathways. STEM CELLS 2007;25:903–910 Disclosure of potential conflicts of interest is found at the end of this article. INTRODUCTION At present, the prevention of tissue-engineered implant failure due to the lack of blood vessels and resulting hypoxia is still a fundamental challenge in regenerative medicine. To address these problems, approaches based on cell delivery systems harboring proangiogenic properties seem to be preferable to pharmacological stimulation, since the agents delivered, such as recombinant vascular endothelial growth factor (VEGF) or basic fibroblast growth factor (bFGF), are rapidly cleared from the target site and may lead to unwanted side effects, such as vascular leakage and hypotension [1, 2]. MSCs have proangiogenic properties, are relatively easy to harvest, and harbor a great expansion potential [3]. These cells are able to differentiate not only into mesenchymal cells, such as osteoblasts and chondrocytes, but also into nonmesenchymal cells, such as endothelial cells (ECs) and neural cells [3–5]. These properties make MSCs an attractive cell source for a wide variety of tissue engineering strategies. Indeed, these cells are used in clinical applications as single cell-type constructs and show promise in combination with ECs in multicell-type in vitro prevascularized constructs for bone regeneration [6, 7]. It is well established that MSCs are able to influence EC behavior and vice versa. For example, the presence of ECs appears to promote osteogenic differentiation of MSCs [8 –10]. In addition, MSCs are capable of neoangiogenesis [11] induction in an in vivo model [12]. A recent study consolidates these observations in vitro by demonstrating that MSCs promote EC migration and tube formation [13]. Furthermore, MSCs seeded on three-dimensional (3D) constructs seem to support endothelial cell growth [14]. VEGF is one factor that could potentially mediate the cross-talk between MSCs and ECs. MSCs were shown to secrete VEGF, the expression of which was elevated during osteogenesis [15]. In addition, MSCs have been shown to generate sufficient VEGF to support the survival and differentiation of ECs [16]. Apart from VEGF, other molecules expressed by MSCs, including transforming growth factor- (TGF-) and matrix metalloproteases (MMPs) (e.g., MMP-2 and MMP-14), could contribute to the complex interaction of MSCs and ECs [17, 18]. In addition, mechanical boundary conditions are known to alter the gene expression pattern and consequently the functional behavior of MSCs. For example, osteogenic differentiation and proliferation of MSCs appear to be stimulated by mechanical loading [19 –22]. In conclusion, there is clear evidence for a complex interplay between MSCs and ECs, and thereby MSCs seem to be Correspondence: Grit Kasper, Ph.D., Musculoskeletal Research Center Berlin, Charite´–Universita¨tsmedizin Berlin, Augustenburger Platz, 113353 Berlin, Germany. Telephone: 49-30-450615116; Fax: 49-30-450559969; e-mail: [email protected] Received July 14, 2006; accepted for publication December 28, 2006; first published online in STEM CELLS EXPRESS January 11, 2007. ©AlphaMed Press 1066-5099/2007/$30.00/0 doi: 10.1634/stemcells.2006-0432 STEM CELLS 2007;25:903–910 www.StemCells.com MSCs Regulate Angiogenesis 904 able to promote angiogenesis. However, the influence of mechanical loading on this interaction remains unknown. In the present study, we report data demonstrating that mechanical stimulation of MSCs increases their paracrine proangiogenic properties by the induction of molecules other than VEGF. The results presented are relevant for the generation of in vitrovascularized tissue-engineered constructs, as well as for the stimulation of physiological regeneration processes. MATERIALS AND METHODS Cell Culture and Characterization of MSCs Bone marrow was obtained from patients undergoing hip surgery. All donors gave informed consent. The median age of male and female donors was 50 years (range, 33– 84 years). MSCs were isolated within 4 hours by centrifugation with Histopaque-1077 (Sigma-Aldrich, Steinheim, Germany, http://www.sigmaaldrich. com) density separation and subsequent adherence to tissue culture plastic. MSCs were cultured in Dulbecco’s modified Eagle’s medium (DMEM) (Invitrogen, Karlsruhe, Germany, http://www. invitrogen.com) supplemented with 10% fetal calf serum (FCS) (Biochrom AG, Berlin, http://www.biochrom.de) and 100 U/ml penicillin ⫹ 100 g/ml streptomycin. Cells were passaged at 70%– 80% confluence and seeded at a density of 2.5 ⫻ 103 cells per cm2. Only cells from passages 3–7 were used for experiments. For flow cytometry, 1 ⫻ 105 cells were trypsinized and washed with phosphate-buffered saline/bovine serum albumin before a 15-minute incubation with fluorescence-conjugated antibodies on ice. After washing, propidium iodide was added, and cells were analyzed using FACSCalibur (BD Biosciences, Heidelberg, Germany, http:// www.bdbiosciences.com). Twenty thousand events were acquired and analyzed using the FCSExpress 2 software (De Novo Software, Thornhill, ON, Canada, http://www.denovosoftware.com). Antibodies used were as follows: mouse (␣-human CD73): phycoerythrin (PE) (BD Biosciences), mouse (␣-human CD44): fluorescein isothiocyanate (FITC) (BD Pharmingen, Heidelberg, Germany, http://www.bdbiosciences.com/pharmingen),mouse(␣-humanCD105): FITC (Serotec, Du¨sseldorf, Germany, http://www.serotec.com), mouse (␣-human CD106):PE (Pharmingen), mouse (␣-human CD34):PE (BD Biosciences), mouse (␣-human CD45):FITC (BD Biosciences), and mouse (␣-human CD90):FITC (BD Biosciences). As negative controls, cells were stained with nonspecific molecules of the same isotype as the antibodies used. In addition, MSC capacity to differentiate into the osteogenic and adipogenic lineage by addition of the appropriate media [3] was confirmed. SV40immortalized human dermal microvascular endothelial cells (HMEC-1) were used [23]. This cell line was kindly provided by Prof. G. Scho¨nfelder (Charite´, Universita¨tsmedizin, Berlin) and was cultured in MCB-131 (Invitrogen) supplemented with 1 g/ml hydrocortisone, 2 mM L-glutamine, 5% FCS (Biochrom), and 100 U/ml penicillin ⫹ 100 g/ml streptomycin. Generation of Conditioned Media and Characterization of the Bioreactor The bioreactor system used has been described previously [24]. Briefly, MSCs were trypsinized, and 2 ⫻ 106 cells in 350 l of culture medium were mixed with 300 l of fibrinogen per medium (1:2) mixture and 50 l of thrombin S/medium mixture (1:2) (Tissucol; Baxter, Munich, Germany, http://www.baxter.com). The construct mixture was placed between two spongiosa chips (4 mm in height and 15 mm in diameter) and allowed to solidify for 30 minutes at 37°C. The solid sandwich was placed into the bioreactor, and 25 ml of MSC culture medium was added containing 0.6 ml of Trasylol (Bayer, Leverkusen, Germany, http://www.bayer.com) and, if indicated, 6.7 M MMP-2 inhibitor (Calbiochem, Darmstadt, Germany, http://www.merckbiosciences.com). Oxygen partial pressure was measured by Licox MCB Revooxide Oxygen Probe (Integra Neuroscience, Ratingen, Germany, http://www.integra-ls. com). Cell viability in the constructs was determined by CellTiter 96 AQueous test (Promega, Mannheim, Germany, http://www. promega.com). Levels of cell proliferation were determined based on 5-bromo-2⬘-deoxyuridine incorporation using the cell proliferation enzyme-linked immunosorbent assay (ELISA) kit (Roche, Manheim, Germany, http://www.roche.com). Results showed that in contrast to positive controls (MSCs on cell culture plastic), MSCs within the construct do not proliferate either with or without mechanical loading. This was confirmed visually by hematoxylin staining that revealed single cells in the construct. Mechanical loading was carried out for 72 hours at 1 Hz and 10 kPa (approximately 30% strain). Afterward, conditioned medium (CM) was harvested and centrifuged at 500g. The supernatant was stored in working aliquots at ⫺20°C and analyzed within 3 weeks. All measurements were made in three independent experiments. RNA Isolation, cDNA Synthesis, and Quantitative Reverse Transcription-Polymerase Chain Reaction Total RNA was extracted using RNeasy Mini Kit (Qiagen, Hilden, Germany, http://www1.qiagen.com) according to the manufacturer’s instructions. RNA quality was assessed by determination of the 18S/28S rRNA ratio using the Agilent Bioanalyzer (Agilent Technologies, Waldbronn, Germany, http://www.agilent.com). Subsequently, cDNA was obtained by reverse transcription of total RNA using the TaqMan reverse transcription reagents (Applied BioSystems, Foster City, NJ, http://www.appliedbiosystems.com) according to the manufacturer’s instructions. The quantification of HIF1␣, VEGF, and -actin transcripts were assessed by quantitative reverse transcription-polymerase chain reaction (qRT-PCR) using the LightCycler FastStart DNA Master SYBR Green I Kit and the Roche LightCycler instrument and software (Roche, Mannheim, Germany). VEGF and HIF-1␣ transcript expression were normalized versus the housekeeping gene -actin. The following primers used in the real-time PCR assay were purchased from TIB Molbiol (Berlin, http://www.tib-molbiol.com): -actin forward primer, 5⬘gAC Agg ATg CAg AAg gAg ATC ACT-3⬘; -actin reverse primer, 5⬘-TgA TCC ACA TCT gCT ggA Agg T-3⬘; HIF-1␣ forward primer, 5⬘-CCA TTA gAA AgC AgT TCC gC-3⬘; HIF-1␣ reverse primer, 5⬘-Tgg gTA ggA gAT ggA gAT gC-3⬘; VEGF forward primer, 5⬘-TCC ATg gAT gTC TAT CAg Cg-3⬘; VEGF reverse primer, 5⬘-gCT CAT CTC TCC TAT gTg CT-3⬘. The accuracy of the qRT-PCR assay as determined by the amplification efficiency (E) was assessed by measurement of dilution series of a randomized cDNA mix (-actin, E ⫽ 1.95 ⫾ 0.05; HIF-1␣, E ⫽ 1.98 ⫾ 0.03; VEGF, E ⫽ 1.94 ⫾ 0.04). Transcripts from four MSC donors were analyzed. Angiogenesis Assays For tube formation assays, 24-well plates were coated with 50 l of Matrigel (10 mg/ml; Invitrogen) and allowed to solidify for 30 minutes at 37°C. Afterward, 4 ⫻ 104 HMEC-1 cells were seeded in 100 l of endothelial cell medium per well, and 500 l of CM was added. Sprouting assays were conducted according to Korff et al. [25]. Briefly, spheroid formation was performed by suspending 1 ⫻ 103 HMEC-1 cells in culture medium containing 0.25% (wt/vol) methylcellulose and seeded into nonadherent round-bottom 96-well plates. After cultivation for 24 hours, spheroids were embedded into collagen gels (Vitrogen; Nutacon BV, Leimuiden, The Netherlands, http://www.nutacon.nl), where three parts collagen were mixed with one part medium containing the spheroids. The gel was allowed to polymerize (30 minutes at 37°C) and overlaid with 100 l of CM. Both assays were incubated for 17 hours before results were visualized by light microscopy. Images were digitalized at a magnification of ⫻10 and a resolution of 1,600 ⫻ 1,200 pixels. Quantification was performed by means of NIH ImageJ software package (http://rsb.info.nih.gov/nih-image/). The length of the two-dimensional (2D) capillary network was analyzed in five independent fields per well. Cumulative sprout length was summed from sprouts over the threshold length of 55 pixels. Four spheroids per sample were evaluated. Experiments were repeated at least three times with duplicates. Equal cell numbers were confirmed by a CellTiter 96 AQueous test (Promega) at the end of the assays. Inhibitors used in the assays were as follows: a monoclonal ␣-human VEGF antibody (25 g/ml; R&D Systems, Wiesbaden, Germany, http://www. rndsystems.com), a vascular endothelial growth factor receptor Kasper, Dankert, Tuischer et al. 905 (VEGFR) tyrosine kinase inhibitor (20 M; Calbiochem), a MMP-2 inhibitor (6.7 M; Calbiochem), a monoclonal ␣-human TGF-1 antibody (1 g/ml; Calbiochem), and the fibroblast growth factor (FGF) receptor tyrosine kinase inhibitor SU5402 (80 M; Calbiochem). Proliferation Assay HMEC-1 cells (4 ⫻ 103) were seeded in HMEC-1 culture medium into 96-well plates. The following day, cells were washed twice with DMEM without FCS, and CM was added. After 3 days of incubation, a CellTiter 96 AQueous test (MTS test; Promega) was performed according to the manufacturer’s instructions. Six independent experiments using different MSC donors were conducted using five wells per experiment. Transwell Migration Assay Migration was measured by a modified Boyden chamber assay [26] using polycarbonate filters (8-m pore size; Nunc, Wiesbaden, Germany, http://www.nuncbrand.com) coated with Matrigel (1 mg/ ml; Invitrogen). CM (500 l) from stimulated or unstimulated MSCs was placed in the lower chamber. HMEC-1 cells (2 ⫻ 104) were seeded onto the filters in 500 l of CM from unloaded samples. After 1 hour of incubation at 37°C, cells were fixed by paraformaldehyde. Nonmigrated cells were removed by scraping, and remaining migrated cells were stained by Hoechst. Cell numbers of five microscopic fields per filter were analyzed using the NIH ImageJ software package (http://rsb.info.nih.gov/nih-image/). Six independent experiments using different MSC donors with duplicates in each were conducted. Adhesion Assay After trypsinization, 2 ⫻ 104 HMEC-1 cells were resuspended in 100 l of CM of MSC and seeded into 96-well plates. After 20 minutes of incubation, nonadherent cells were removed by inverting the plates. Remaining adherent cells were quantified by CellTiter 96 AQueous test (MTS test; Promega) according to the manufacturer’s instructions. Five independent experiments using different MSC donors were conducted using five wells per experiment. Zymogram and ELISA Gelatin zymography was performed by the Novex system (Invitrogen) according to the manufacturer’s protocol. To detect MMP-2, CM from six MSC donors was tested at a dilution of 1:30. All ELISAs were obtained from R&D Systems and performed in triplicate according to the manufacturer’s instructions. In VEGF and TGF-1 ELISAs, original CM was used. For bFGF ELISA, the CM was concentrated 30 times. CM with and without MMP-2 inhibitor application via conditioning was tested from three MSC donors. Statistical Analysis The SPSS 12.0 software package (SPSS, Inc., Chicago, http://www. spss.com) was used for statistical evaluation. Data from functional assays were analyzed by nonparametric testing and are displayed in box plots showing medians as bars and interquartile ranges as boxes. Effects of CM from mechanically loaded versus unloaded MSCs from the same donors were analyzed by means of the Wilcoxon test. For analysis of the effect of inhibitor supplementation on the ratio of angiogenesis stimulation by CM from loaded to unloaded MSCs versus this ratio in control samples without inhibitors, the Mann-Whitney U test was used. Results from expression analyses were analyzed by Student’s t tests. All tests were two-sided and at a significance level of p ⬍ .05. In Figs. 3– 6, statistical significance is indicated by asterisks. RESULTS Characterization of the Bioreactor System for Mechanical Stimulation The MSCs used were characterized by their marker protein expression, as well as their potential to differentiate (Fig. 1; data www.StemCells.com Figure 1. Flow cytometry analysis of cell surface markers in MSCs. The cells were negative for CD34 and CD45 and stained positive for CD13, CD44, CD73, CD90, CD105, and CD106. Shown are cell counts (y-axis) and relative fluorescence intensities (x-axis). Isotype controls are displayed in gray, and samples incubated with specific antibodies are indicated in black. Abbreviations: FITC, fluorescein isothiocyanate; PE, phycoerythrin. not shown). The bioreactor system presented [24] was used for the generation of CM from mechanical loaded MSCs. For a characterization of the system, oxygen partial pressure was measured throughout the construct (Fig. 2B). The partial pressure for the setting used was not lower than 75% of that of saturated cell culture media, which corresponds to approximately 15 kPa. Thus, compared with physiological oxygen pressure, the conditions in the bioreactor can be considered as nonhypoxic. Furthermore, it was demonstrated that the viability of MSCs could be maintained over the time of conditioning of media and that cell numbers were similar in mechanically stimulated and unstimulated cell constructs (data not shown). Influence of CM from Mechanically Stimulated MSCs on Angiogenesis To address the question of how mechanical stimulation of MSCs might influence their angiogenesis-promoting capacity, the CM was tested in in vitro angiogenesis assays. Beforehand, expression levels of hypoxia-induced HIF-1␣ and VEGF were determined and found to be unchanged in response to mechanical stimulation of MSCs (Fig. 2C). CM of unstimulated MSCs 906 MSCs Regulate Angiogenesis loaded MSCs, inhibitory agents were used (Fig. 4). In 2D tube formation assays, the inhibitor of the VEGFR tyrosine kinase, as well as the inhibitor of the fibroblast growth factor receptor (FGFR), led to a significantly reduced enhancement of angiogenesis by CM from mechanically loaded versus unloaded MSCs (mediancontrol ⫽ 263%, medianVEGFR inhibitor ⫽ 94%, medianFGFR inhibitor ⫽ 123%; pVEGFR inhibitor ⫽ 0.011, pFGFR inhibitor ⫽ 0.020). The supplementation of an inhibitory antibody against TGF-1 resulted in a trend of suppression of angiogenesis stimulation, which was not statistically significant (median␣-TGF-1 ⫽ 149%; p ⫽ .088). In agreement with the 2D results, the application of FGFR inhibitor in 3D sprouting assays resulted in a diminished angiogenesis promotion (mediancontrol ⫽ 174%, medianFGFR inhibitor ⫽ 93%; p ⫽ .045). Furthermore, the supplementation of CM with a MMP-2 inhibitor showed a tendency to inhibit the described effect without reaching significance (medianMMP-2 inhibitor ⫽ 121%; p ⫽ .055). Since the level of induction of angiogenesis varied between donors (Fig. 3), results for MMP-2 and TGF-1 inhibition might reach statistical significance in a larger donor cohort. Influence of CM from Mechanically Stimulated MSCs on EC Function Figure 2. Characterization of oxygen supply in the bioreactor system. (A): The bioreactor consists of a closed cylindrical polyethylene chamber communicating via four sterile filters with the surrounding gas. Mechanical stimulation of cell loaded constructs is mediated by a pneumatically driven displacement of the upper silicone membrane. The lower membrane is connected to a pressure transducer, enabling pressure regulation. (B): Construct used for mechanical loading. Oxygen saturation within constructs is displayed relative to saturated cell culture media. (C): mRNA levels of HIF-1␣ and VEGF as determined by quantitative reverse transcription-polymerase chain reaction from MSCs relative to -actin. The ratio of expression levels in mechanically loaded relative to unloaded controls is presented. Abbreviation: VEGF, vascular endothelial growth factor. showed no significant effect on angiogenesis in the 2D or 3D assays in comparison to control media from constructs without cells (Fig. 3). In contrast, CM from mechanically stimulated MSCs enhanced angiogenesis compared with CM from unstimulated cells in both assays (2D: medianstimulated ⫽ 142 ⫻ 105 pixels, medianunstimulated ⫽ 49 ⫻ 105 pixels; p ⫽ .028; 3D: medianstimulated ⫽ 96 ⫻ 104 pixels, medianunstimulated ⫽ 40 ⫻ 104 pixels; p ⫽ .028). This effect was not detectable in assays using CM from mechanically loaded control constructs without cells. Absolute levels of sprouting and tube formation were rather diverse between CM from different MSC donors. However, due to the small sample size, no correlation to donor characteristics, such as sex or age, could be made. Involvement of bFGF and VEGFR Signaling Cascade To investigate the relevance of different signaling cascades for the paracrine stimulation of angiogenesis by mechanically Since angiogenesis involves several functional activities of ECs, the proliferation, migration, and adhesion of HMEC-1 cells was investigated in appropriate in vitro models. CM from untreated MSCs showed a stimulatory effect on HMEC-1 migration compared with media from constructs without cells (medianMSCs ⫽ 32 cells per field, medianno cells ⫽ 17 cells per field; p ⫽ .043; Fig. 5). Proliferation and adhesion of HMEC-1 cells were similar in CM from MSCs and from control constructs without cells. However, mechanical loading of MSCs led to a significant enhancement of proliferation of HMEC-1 cells (medianstimulated ⫽ 0.754 optical density [OD]490 nm, medianunstimulated ⫽ 0.439 [OD]490 nm, p ⫽ .028; Fig. 5A), whereas CM from mechanically loaded control constructs without cells showed no effect (p ⫽ .917). Migration and adhesion of HMEC-1 cells was not affected by CM from mechanically stimulated MSCs (pmigration ⫽ 0.528, padhesion ⫽ 0.500; Fig. 5B, 5C). Levels of Angiogenic Factors in CM of MSCs To reveal factors that are potentially involved in the enhancement of angiogenesis by mechanically stimulated MSCs, levels of the angiogenesis regulators MMP-2, VEGF, TGF-1, and bFGF were investigated in CM of stimulated and unstimulated MSCs. MMP-2 was upregulated by mechanical loading, as shown by zymography (Fig. 6A; G. Kasper, J.D. Glaeser, S. Giessler, A. Ode, J. Tuischer, G. Matziolis, C. Perka, G.N. Duda, manuscript in preparation). The presence of MSCs led to a significant accumulation of VEGF in CM compared with CM from control constructs without cells (meanno cells ⫽ 2 ng/ml, meanMSCs ⫽ 158 ng/ml; p ⬍ .001). However, no consistent change of VEGF levels in response to mechanical loading was observed (Fig. 6B). TGF-1 was not enriched in cell culture supernatant from untreated MSCs (meanno cells ⫽ 120 pg/ml, meanMSCs ⫽ 121 pg/ml). However, after mechanical stimulation, TGF-1 levels were significantly increased (Fig. 6C). When investigating bFGF concentrations in CM of MSCs, a wide variation in absolute expression levels of this growth factor was observed between MSC donors (Fig. 6D). bFGF showed a trend of accumulation in the CM of untreated MSCs that did not reach statistical significance (meanno cells ⫽ 0.01 pg/ml, meanMSCs ⫽ 1.04 pg/ml). However, protein levels were increased by mechanical loading of MSCs. Since MMPs are able to release growth factors [27], the elevated levels of TGF-1 and bFGF could be due to the observed enhanced MMP-2 Kasper, Dankert, Tuischer et al. 907 Figure 3. Conditioned medium of mechanically stimulated MSCs enhanced in vitro angiogenesis. Representative photographs and analysis of the cumulative length of the tubular network from two-dimensional tube formation (A) and sprouts per spheroid from three-dimensional sprouting (B). Shown are six MSC donors, as well as the average of these donors and of the corresponding negative controls (constructs without cells). Original magnification of photographs, ⫻10. Slashed circles define extreme values. Abbreviation: w/o, without. Figure 4. Potential involvement of fibroblast growth factor receptor and the VEGFR signaling cascades in angiogenesis stimulation. Displayed are ratios of the cumulative length resulting from conditioned medium of loaded to unloaded MSCs from tubular structures in two-dimensional tube formation assays (A) and sprouts per spheroid in threedimensional sprouting assays (B). Abbreviations: MMP, matrix metalloprotease; ␣TGF-, transforming growth factor- blocking antibody; ␣-VEGF, vascular endothelial growth factor blocking antibody; VEGFR, vascular endothelial growth factor receptor. activity. However, the application of an MMP-2 inhibitor showed no effect on the increased TGF-1 or bFGF levels, indicating that this protease is not involved in an increased release of these growth factors (Fig. 6C, 6D). The effects described were not seen in CM from control constructs without cells. Thus, mechanical loading leads to a specific accumulation of MMP-2, TGF-1, and bFGF in the microenvironment of MSCs. www.StemCells.com DISCUSSION In the present study, the influence of mechanical loading on the paracrine stimulation of angiogenesis by MSCs was investigated. CM from untreated MSCs was not capable of stimulating angiogenesis. However, enhanced tube formation in endothelial cells cultivated with CM from unstimulated MSCs has recently 908 MSCs Regulate Angiogenesis Figure 5. Proliferation of endothelial cells was influenced by conditioned medium (CM) from mechanically stimulated MSCs. Shown are OD490 nm values corresponding to HMEC-1 cell numbers (A), migrated HMEC-1 cells per microscopic field (B), and OD490 nm values corresponding to numbers of adhered HMEC-1 cells (C). All assays were conducted with CM from mechanically stimulated and unstimulated MSCs and negative control constructs. Abbreviation: OD, optical density. Figure 6. MMP-2, TGF-1, and bFGF were enriched by mechanical loading. (A): A representative zymogram using MSCs from one donor is displayed. Shown are VEGF (B), TGF-1 (C), and bFGF (D) concentrations as determined by enzyme-linked immunosorbent assay in conditioned medium of mechanically loaded and unloaded MSCs from three different donors in the presence and absence of an MMP-2 inhibitor. Abbreviations: bFGF, basic fibroblast growth factor; MMP, matrix metalloprotease; TGF, transforming growth factor; VEGF, vascular endothelial growth factor. been reported [13]. This discrepancy might be due to the different experimental settings used (e.g., a 3D system in fibrin to approach physiological conditions versus a 2D cultivation of MSCs on tissue culture plastic). The data from the present study suggest that unstimulated MSCs lack the ability to promote angiogenesis. Instead, the cells seem to gain this capability in response to changes in their mechanical boundary conditions. This regulatory mechanism might be of high physiological relevance, since angiogenesis is an essential process for tissue regeneration [28] but on the other hand needs to be tightly controlled spatially and temporally to prevent tumor formation [29]. It has been shown that ECs and osteoprogenitor cells interact by gap junctions [9]. The results presented here demonstrate that paracrine mechanisms for a cross-talk between MSCs and ECs, independent of direct cell-cell contacts, appear to exist in response to mechanical loading of MSCs. The transcription factor HIF-1␣ and its downstream target VEGF could represent Kasper, Dankert, Tuischer et al. candidate mediators for the translation of mechanical signals into a proangiogenic response, since these angiogenesis regulators were shown to be upregulated because of mechanical stress [30, 31]. However, under the conditions in this study, neither HIF-1␣ nor VEGF expression was enhanced after mechanical stimulation of MSCs. Since these factors are also induced by hypoxia [30 –32], it is important to note that the mechanical loading setting described was demonstrated to run under nonhypoxic conditions by direct oxygen measurement. Furthermore, the upregulation of MMP-2 indicates a nonhypoxic environment, since a report of Annabi et al. [33] showed that hypoxia downregulates MMP-2 expression in MSCs. The hypothesis that VEGF is not the mediating factor of the stimulatory effect of mechanical loading on angiogenesis shown in this study is further supported by the inability of a VEGF inhibitory antibody to repress the proangiogenic response. However, our data indicate that although the promotion of tube formation occurs independently of VEGF, there is still a dependence on the activity of the VEGFR pathway. This suggests that the effect might be mediated by cross-talk to another pathway. Additional candidates for soluble factors mediating the observed effect are the angiogenesis regulators MMP-2, TGF-1, and bFGF, which were shown to be upregulated in response to mechanical loading. Since the proproliferative molecule VEGF [34, 35] was not enhanced in response to mechanical stimulation, the reported effect of angiogenesis promotion by mechanically loaded MSCs is not a likely result of this factor. However, microvascular cells have the potential to respond not only to VEGF but also to TGF-1 and bFGF, since they were shown to express the corresponding cell surface receptors [36, 37]. Indeed, we could demonstrate that FGFR signaling, which is known to have the potential to stimulate survival, proliferation, migration, and differentiation of endothelial cells [34, 35, 38], is involved in angiogenesis stimulation by CM from mechanically loaded MSCs. MMP-2 is postulated to be essential for the initiation of angiogenesis [39]. Our results suggest that MMP-2 is not involved in the enrichment of CM by TGF-1 or bFGF but might contribute to angiogenesis by other mechanisms, such as the removal of mechanical barriers by extracellular matrix degradation or the generation of regulatory breakdown products from the extracellular matrix [40]. In fact, 3D sprouting assays hint at a potential involvement of MMP-2 in mediating the observed effect. TGF-1 seems to play a dual role in angiogenesis. Low concentrations (ⱕ0.5 ng/ml) stimulate tube formation, whereas higher concentrations (1–5 ng/ml) are inhibitory [41– 43]. Similar effects are seen for EC proliferation [44]. ELISA results from this study point to TGF-1 concentrations lower than 0.2 ng/ml in CM from mechanically stimulated MSCs. Therefore, the proproliferative and tube formation-enhancing effect on ECs observed in this study could be mediated by TGF-1. Indeed, inhibition of TGF-1 showed a tendency to repress the enhance- REFERENCES 1 2 3 4 5 Hariawala MD, Horowitz JR, Esakof D et al. VEGF improves myocardial blood flow but produces EDRF-mediated hypotension in porcine hearts. J Surg Res 1996;63:77– 82. Lazarous DF, Shou M, Stiber JA et al. Pharmacodynamics of basic fibroblast growth factor: Route of administration determines myocardial and systemic distribution. Cardiovasc Res 1997;36:78 – 85. Pittenger MF, Mackay AM, Beck SC et al. Multilineage potential of adult human mesenchymal stem cells. Science 1999;284: 143–147. Oswald J, Boxberger S, Jorgensen B et al. Mesenchymal stem cells can be differentiated into endothelial cells in vitro. STEM CELLS 2004;22: 377–384. Kopen GC, Prockop DJ, Phinney DG. Marrow stromal cells migrate www.StemCells.com 909 ment of tube formation. In addition to their paracrine implications, the mechanically stimulated factors that we report here may also act directly on MSCs, since they express the appropriate cell surface receptors, such as FGFR, TGF-1R, and TGF-2R, and MSC function is known to be influenced by MMPs [45]. Such paracrine and autocrine mechanisms are likely to act together to determine the consequences of mechanical loading on the signaling between MSCs and ECs. CONCLUSION At present, the generation of viable tissue-engineered constructs larger than a few millimeters in size using mesenchymal or other stem cells is limited due to the lack of functional vasculature within the constructs. Data from the present study indicate that mechanically stimulated MSCs create an angiogenesis-promoting environment. The underlying mechanisms of the paracrine stimulation of angiogenesis by mechanically loaded MSCs seem not to be mediated by an upregulation of VEGF but might at least partially involve the VEGFR signaling cascade. Furthermore, the FGFR pathway seems to be involved in angiogenesis stimulation. Although the interplay between MSCs and ECs is likely to be even more complex in vivo, further insight into these interactions and the influence of mechanical boundary conditions is vital for an understanding of the physiological coordination of angiogenesis, progenitor cell differentiation, and regenerated tissue formation. This understanding is in turn the foundation for a rational approach to the design and optimization of prevascularized tissue-engineered constructs and essential for predicting optimal mechanical stabilization conditions for successful tissue regeneration. ACKNOWLEDGMENTS This study was partially supported by the Bundesministerium fuer Bildung und Forschung excellence cluster Berlin-Brandenburg Center for Regenerative Therapies and the AO Foundation, Switzerland. We are grateful to Prof. U. Dirnagl (Neurology, Charite´, Universita¨tsmedizin, Berlin, Germany) for the use of the oxygen probe. We thank Dr. A. Rump (Molecular Genetics, TU-Dresden) for critical reading of the manuscript and M. Princ for excellent technical assistance. DISCLOSURE OF POTENTIAL OF INTEREST CONFLICTS The authors indicate no potential conflicts of interest. throughout forebrain and cerebellum, and they differentiate into astrocytes after injection into neonatal mouse brains. Proc Natl Acad Sci U S A 1999;96:10711–10716. 6 Quarto R, Mastrogiacomo M, Cancedda R et al. Repair of large bone defects with the use of autologous bone marrow stromal cells. N Engl J Med 2001;344:385–386. 7 Katritsis DG, Sotiropoulou PA, Karvouni E et al. Transcoronary transplantation of autologous mesenchymal stem cells and endothelial progenitors into infarcted human myocardium. Catheter Cardiovasc Interv 2005;65:321–329. 8 Meury T, Verrier S, Alini M. Human endothelial cells inhibit BMSC differentiation into mature osteoblasts in vitro by interfering with osterix expression. J Cell Biochem 2006;98:992–1006. 9 Villars F, Guillotin B, Amedee T et al. Effect of HUVEC on human osteoprogenitor cell differentiation needs heterotypic gap junction communication. Am J Physiol Cell Physiol 2002;282:C775–C785. 10 Choong CS, Hutmacher DW, Triffitt JT. Co-culture of bone marrow MSCs Regulate Angiogenesis 910 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 fibroblasts and endothelial cells on modified polycaprolactone substrates for enhanced potentials in bone tissue engineering. Tissue Eng 2006;12: 2521–2531. Asahara T, Bauters C, Zheng LP et al. Synergistic effect of vascular endothelial growth factor and basic fibroblast growth factor on angiogenesis in vivo. Circulation 1995;92(Suppl 9):II365–II371. Al-Khaldi A, Eliopoulos N, Martineau D et al. Postnatal bone marrow stromal cells elicit a potent VEGF-dependent neoangiogenic response in vivo. Gene Ther 2003;10:621– 629. Gruber R, Kandler B, Holzmann P et al. Bone marrow stromal cells can provide a local environment that favors migration and formation of tubular structures of endothelial cells. Tissue Eng 2005;11:896 –903. Markowicz M, Koellensperger E, Neuss S et al. Enhancing the vascularization of three-dimensional scaffolds: New strategies in tissue regeneration and tissue engineering. In: Ashammakhi N, Reis RL, eds. Topics in Tissue Engineering. Vol 2. 2005:1–16. Available at http://www.oulu. fi/spareparts/ebook_topics_in_t_e_vol2/abstracts/markowicz1_0102.pdf. Accessed February 26, 2007. Mayer H, Bertram H, Lindenmaier W et al. Vascular endothelial growth factor (VEGF-A) expression in human mesenchymal stem cells: Autocrine and paracrine role on osteoblastic and endothelial differentiation. J Cell Biochem 2005;95:827– 839. Kaigler D, Krebsbach PH, Polverini PJ et al. Role of vascular endothelial growth factor in bone marrow stromal cell modulation of endothelial cells. Tissue Eng 2003;9:95–103. Beyth S, Borovsky Z, Mevorach D et al. Human mesenchymal stem cells alter antigen-presenting cell maturation and induce T-cell unresponsiveness. Blood 2005;105:2214 –2219. Ahlborg HG, Johnell O, Turner CH et al. Bone loss and bone size after menopause. N Engl J Med 2003;349:327–334. Koike M, Shimokawa H, Kanno Z et al. Effects of mechanical strain on proliferation and differentiation of bone marrow stromal cell line ST2. J Bone Miner Metab 2005;23:219 –225. Mauney JR, Sjostorm S, Blumberg J et al. Mechanical stimulation promotes osteogenic differentiation of human bone marrow stromal cells on 3-D partially demineralized bone scaffolds in vitro. Calcif Tissue Int 2004;74:458 – 468. Yoshikawa T, Peel SA, Gladstone JR et al. Biochemical analysis of the response in rat bone marrow cell cultures to mechanical stimulation. Biomed Mater Eng 1997;7:369 –377. Jagodzinski M, Drescher M, Zeichen J et al. Effects of cyclic longitudinal mechanical strain and dexamethasone on osteogenic differentiation of human bone marrow stromal cells. Eur Cell Mater 2004;7:35– 41; discussion 41. Ades EW, Candal FJ, Swerlick RA et al. HMEC-1: Establishment of an immortalized human microvascular endothelial cell line. J Invest Dermatol 1992;99:683– 690. Matziolis G, Tuischer J, Kasper G et al. Simulation of cell differentiation in fracture healing: Mechanically loaded composite scaffolds in a novel bioreactor system. Tissue Eng 2006;12:201–208. Korff T, Kimmina S, Martiny-Baron G et al. Blood vessel maturation in a 3-dimensional spheroidal coculture model: Direct contact with smooth muscle cells regulates endothelial cell quiescence and abrogates VEGF responsiveness. FASEB J 2001;15:447– 457. Falk W, Goodwin RH Jr, Leonard EJ. A 48-well micro chemotaxis 27 28 29 30 31 32 33 34 35 36 37 38 39 40 41 42 43 44 45 assembly for rapid and accurate measurement of leukocyte migration. J Immunol Methods 1980;33:239 –247. Mott JD, Werb Z. Regulation of matrix biology by matrix metalloproteinases. Curr Opin Cell Biol 2004;16:558 –564. Hausman MR, Schaffler MB, Majeska RJ. Prevention of fracture healing in rats by an inhibitor of angiogenesis. Bone 2001;29:560 –564. Gupta MK, Qin RY. Mechanism and its regulation of tumor-induced angiogenesis. World J Gastroenterol 2003;9:1144 –1155. Petersen W, Varoga D, Zantop T et al. Cyclic strain influences the expression of the vascular endothelial growth factor (VEGF) and the hypoxia inducible factor 1 alpha (HIF-1alpha) in tendon fibroblasts. J Orthop Res 2004;22:847– 853. Pufe T, Lemke A, Kurz B et al. Mechanical overload induces VEGF in cartilage discs via hypoxia-inducible factor. Am J Pathol 2004;164:185–192. Robins JC, Akeno N, Mukherjee A et al. Hypoxia induces chondrocytespecific gene expression in mesenchymal cells in association with transcriptional activation of Sox9. Bone 2005;37:313–322. Annabi B, Lee YT, Turcotte S et al. Hypoxia promotes murine bonemarrow-derived stromal cell migration and tube formation. STEM CELLS 2003;21:337–347. Grgic I, Eichler I, Heinau P et al. Selective blockade of the intermediateconductance Ca2⫹-activated K⫹ channel suppresses proliferation of microvascular and macrovascular endothelial cells and angiogenesis in vivo. Arterioscler Thromb Vasc Biol 2005;25:704 –709. Vasse M, Pourtau J, Trochon V et al. Oncostatin M induces angiogenesis in vitro and in vivo. Arterioscler Thromb Vasc Biol 1999;19:1835–1842. Sankar S, Mahooti-Brooks N, Bensen L et al. Modulation of transforming growth factor beta receptor levels on microvascular endothelial cells during in vitro angiogenesis. J Clin Invest 1996;97:1436 –1446. MacKenzie F, Duriez P, Larrivee B et al. Notch4-induced inhibition of endothelial sprouting requires the ankyrin repeats and involves signaling through RBP-Jkappa. Blood 2004;104:1760 –1768. Cross MJ, Claesson-Welsh L. FGF and VEGF function in angiogenesis: Signalling pathways, biological responses and therapeutic inhibition. Trends Pharmacol Sci 2001;22:201–207. Fang J, Shing Y, Wiederschain D et al. Matrix metalloproteinase-2 is required for the switch to the angiogenic phenotype in a tumor model. Proc Natl Acad Sci U S A 2000;97:3884 –3889. Sternlicht MD, Werb Z. How matrix metalloproteinases regulate cell behavior. Annu Rev Cell Dev Biol 2001;17:463–516. Merwin JR, Newman W, Beall LD et al. Vascular cells respond differentially to transforming growth factors beta 1 and beta 2 in vitro. Am J Pathol 1991;138:37–51. Mu¨ller G, Behrens J, Nussbaumer U et al. Inhibitory action of transforming growth factor beta on endothelial cells. Proc Natl Acad Sci U S A 1987;84:5600 –5604. Maher PA. Stimulation of endothelial cell proliferation by vanadate is specific for microvascular endothelial cells. J Cell Physiol 1992;151: 549 –554. Myoken Y, Kan M, Sato GH et al. Bifunctional effects of transforming growth factor-beta (TGF-beta) on endothelial cell growth correlate with phenotypes of TGF-beta binding sites. Exp Cell Res 1990;191:299 –304. Minguell JJ, Erices A, Conget P. Mesenchymal stem cells. Exp Biol Med (Maywood) 2001;226:507–520.
© Copyright 2026