CD3+, CD56+ Aggressive Variant of Large Granular
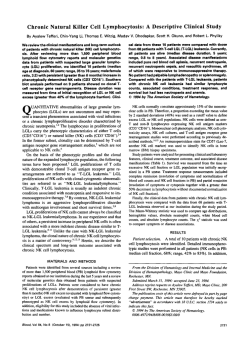
From www.bloodjournal.org by guest on February 6, 2015. For personal use only. CD3+, CD56+ Aggressive Variant of Large Granular Lymphocyte Leukemia By Teresa C. Gentile, Aysegul H. Uner, Robert E. Hutchison, Jonathan Wright, Jonathan Ben-Ezra, E. Clifton Russell, and Thomas P. Loughran, Jr Clonal expansions of CD3+ large granular lymphocytes (LGL) have been classified as T-LGL leukemia. The majority ofpatients with T-LGL leukemia have a chronic disease (years) manifested often bysevere neutropenia, rheumatoid arthritis, and mild-to-moderate splenomegaly. The characteristic phenotype of theleukemic LGL is CD3'. CD8+, CD16'. CD57+, and CD56-. In this report wedescribe an aggressive variant of T-LGL leukemia in which leukemic LGL also expressed CD56, as identified by two-color flow-cytometry analysis. In contrast to the chronic nature typical of T-LGL leukemia, these patients presented with a severesystemic illness that was rapidlyprogressive and resistant t o treatment. Atypical clinical features included rapidly increasing spleen size t o massive proportions, extensive lymphadenopathy, and the presence of B symptoms (fever, nightsweats, weight loss). Hematologic and pathologic features were also unusual for T-LGL leukemia. These patients had very high LGL counts at diagnosis (range 11,692 t o 26,312 pL), which increased rapidly despite treatment. Histopathologic examination of splenic sections showed extensive infiltration of red pulp cords and sinuses by leukemic cells with atrophy of the white pulp, These clinicopathologic features are similar t o those described for patients with natural killercell (NKI-LGL leukemia, whose cells are also CD56+. However, unlike NKLGL leukemia, we could not show a direct pathogenic role for Epstein-Barr virus (EBV), asSouthern-blot analyses using an EBV-joinedtermini probe were negative in these patients. Our findings suggest that CD3+, CD56+ LGL leukemia is a distinctclinicopathologic entity separate from the usual CD3+, CD56- T-LGL leukemia. The expression on leukemic LGL of CD56, an adhesion molecule, may determine the aggressive biologic nature of this newly described disease. 0 1994 by The American Society of Hematology. C clinicopathologic features of these patients were similar to those of NK-LGL leukemia. LONAL DISORDERS of large granular lymphocytes (LGL) may have either a CD3+ or a CD3- phenotype,"3 and have been designated as T-cell (T)-LGL leukemia or natural killer cell (NK)-LGL leukemia respectively: T-LGL leukemic cells have a characteristic phenotype, CD3+, CD8+, CD16+, CD57', and show clonal T-cell receptor (TCR) gene rearrangement. NK-LGL leukemic cells are indistinguishable by light microscopy from T-LGL leukemic cells and show the following phenotype: CD3-, CD4-, CD8-, CD16+, CD56+,CD57-. It is more difficult to prove clonality in CD3- LGL because these cells do not rearrange TCR genes. However, clonal cytogenetic abnormalities have been shown in a number of patients and support the diagnosis of NK-LGL leukemia?-8 The clinical presentation of T-LGL leukemia is quite different from that of NK-LGL leukemia. The majority of patients with T-LGL leukemia have a chronic disease with symptoms primarily resulting from the consequences of neutropenia, which can often be severe. Recurrent bacterial infections are a hallmark of the disease and often the primary indication for therapy. Rheumatoid arthritis also occurs frequently in patients with T-LGL leukemia, 9-11 as well as numerous serologic abnormalities including polyclonal hypergammaglobulinemia, circulating immune complexes, and positive tests for rheumatoid factor, antinuclear antibodies, antineutrophil antibodies, and antiplatelet antibodies4 In contrast, manifestations of systemic disease are often the initial clinical finding in NK-LGL l e ~ k e m i a l ~ fever " ~ ; without signs of infection, night sweats, and weight loss are common. Most patients with NK-LGL leukemia die of disseminated disease within a few months of presentation, despite therapy. Rheumatoid arthritis has not been observed in any patient with NK-LGL leukemia, and other serologic abnormalities have for the most part not been evaluated. In this report we describe three patients with clonal CD3' LGL leukemia whose leukemic cells also co-expressed CD56, a marker usually found in CD3- LGL leukemia. Despite expressing CD3 and showing clonal TCR gene rearrangements typical of patients with T-LGL leukemia, the Blood, Vol 84, No 7 (October l), 1994: pp 2315-2321 CASE REPORTS Patient no. 1. A 14-year-old girl, originally from Jordan, presented in May 1992 with massive splenomegaly, adenopathy (most notably in the cervical and axillary areas), and fever. Workup for infection was unrevealing and she subsequently underwent excisional biopsy of a lymph node for diagnosis and elective splenectomy for severe abdominal pain. The lymph node showed mostly matureappearing lymphocytes and a provisional diagnosis of lymphoma was made. DNA flow cytometry of the spleen showed a diploid cell population, and cell cycle analysis showed 15% S phase. Bone marrow examination at that time showed about 50% lymphocytes similar to those seen in the lymph node. Unstimulated cultures of bone marrow showed a normal karyotype. Approximately 3 weeks after splenectomy, she developed rapidly enlarging cervical lymph nodes, a peripheral white blood cell ( W C ) count of 64,300 with 79% lymphocytes, and worsening anemia and thrombocytopenia. Repeat bone marrow showed 65% small, mature-appearing lymphocytes. Immunophenotyping and TCR gene rearrangement studies were subsequently performed on her peripheral blood mononuclear cells and led to the diagnosis of LGL leukemia. Rheumatoid factor (RF) and antinuclear antibody (ANA) were negative. Quantitative immuno- From the Departments of Medicine, Microbiology and Immunology, and Pathology, Health Science Center, State University of New York at Syracuse; Department of Veterans Affairs Medical Center, Syracuse, NY; and the Departments of Pediatrics and Pathology, Medical College of Virginia, Richmond. Submitted March ii, 1994; accepted June 9, 1994. Supported by Grants No. CA46903 and CA54552 awarded by the National Cancer institute, National Institutes of Health. Address reprint requests to Teresa C. Gentile, MD, PhD, Veterans Affairs Medical Center, 800 Irving Ave, Syracuse, NY 13210. The publication costs of this article were defrayed in part by page charge payment. This article must therefore be hereby marked "advertisement" in accordance with 18 U.S.C. section 1734 solely to indicate this fact. 0 1994 by The American Society of Hematology. 0006-497i/94/8407-0032$3.00/0 2315 From www.bloodjournal.org by guest on February 6, 2015. For personal use only. 2316 GENTILE ET AL globulins showed normal IgG, IgM, and IgA concentrations. Serum protein electrophoresis (SPEP) was normal. Over the next 7 to 8 months she was treated with varying doses of prednisone, vincristine, methotrexate, and 6-mercaptopurine, with temporary disease control. In January 1993 she again had rapid progression of her disease as evidenced by dramatic increases in the size of axillary and cervical lymph nodes. She was treated with induction chemotherapy similar tothat administered for childhood acute lymphoblastic leukemia (vincristine, prednisone, adriamycin, L-asparaginase) followed by five cycles of consolidation therapy with intermediate-dose methotrexate and cytosine arabinoside. Her disease control was again temporary and she has recently had increasing adenopathy. She is currently undergoing conditioning for allogeneic bone marrow transplantation. Patient no. 2. A 52-year-old whiteman presented to his physician in July 1993 complaining of a cough and postnasal drip. Examinationat that time showed an enlarged spleen (palpated 1I to12 cm below the left costal margin) and an elevated WBC count. On further questioning the patient reported a 20-pound weight loss over the prior 2 months and some mild sweating episodes. Bone marrow examination showed a hypercellular marrow (70% to 80%) with markedly increased numbers of lymphoid cells. Unstimulated cultures of bone marrow showed a normal karyotype. Immunophenotyping and T-cell gene rearrangement studies led to the diagnosis of LGL leukemia. RF and ANA tests were negative. Serum immunoglobulin levels were mildly decreased (IgG: 551 mg/dL, normal 591 to 1965 mg/dL; IgM: 60 mg/dL, normal 77 to 400 mg/dL; IgA: 44 mg/dL, normal 50 to 31 I mg/dL). SPEP showed an increased alpha 1 fraction at 6.0% (normal 1.9% to 4.5%). Over the next month the patient continued to lose weight and complained of progressively increasing severe left upper quadrant and left shoulder pain. Because of his worsening symptoms, therapy was instituted and he subsequently received 3 courses of cytoxan 1,400 mg, adriamycin 95 mg, vincristine 2 mg, and prednisone 100 mg (CHOP) every day for 5 days, resulting in a decrease in his peripheral WBC count hutno significant improvement in his splenomegaly. In November 1993 he underwent elective splenectomy. Cell-cycle analysis showed an S phase of 5.5%. Markedly increased numbers of LGL (in the range of 70,000 to 100,OOO/pL) with unusually prominent nucleoli, were noted postsplenectomy. Thrombocytopenia did not improve. Highdose cytoxan (4.5 gm/m2) was administered, and he is being evaluated for HLA-identical allogeneic bone marrow transplantation. Patientno. 3. A 41-year-old Brazilian man was noted to have an enlarged spleen (palpated 15 cm below the left costal margin) during a routine physical exam in September 1992. Subsequent laboratory evaluation showed an elevated WBC count with 80% lymphocytes, the majority of which had the morphology of LGL. Irnmunophenotyping of peripheral blood and TCR gene rearrangement studies confirmed the diagnosis of LGL leukemia. The RF test was positive at a titer of 1:320, andANAwas negative. Quantitative immunoglobulins and SPEP were within normal limits. Over the next 3 months he developed systemic symptoms of low-grade fever and night sweats as well as increasing abdominal painfrom an enlarging spleen and splenic infarctions. In January he was treated with daily oral cytoxan which decreased his peripheral WBC count (from 32,000 to 18,000/pL) but did not much improve his splenomegaly. Subsequently he was treated with chlorodeoxyadenosine (2CdA), again with little improvement in the symptomatology caused by enlarging spleen. In March 1993 he underwent splenectomy, which was complicated by sepsis, and led to his eventual death. MATERIALS AND METHODS Cell phenotyping and separation. Peripheral blood mononuclear cells (PBMCs) were first isolated from whole blood using FicollHypaque density gradient centrifugation (Pharmacia, Piscataway, NJ). These cells were subsequently analyzed for the presence of cell surface antigens using FACScan (Becton-Diclunson, Mountainview, CA) and a panel of monoclonal antibodies (MoAbs) directly conjugated with either fluorescein isothiocyanate or phycoerythrin. These MoAbs included PE-leu 4 (CD3 specific; Becton-Dickinson), FITCT3 (CD3 specific; Olympus, Lake Success, NY), FITC-leu 3 (CD4 specific; Becton-Dickinson), FITC-leu 2 (CD8 specific; BectonDickinson), FITC-leu 1l (CD16 specific; Becton-Dickinson), FITCleu 7 (CD57 specific; Becton-Dickinson) and PE-leu 19 (CD56 specific; Becton-Dickinson). Data were collected and analyzed using Consort 30 software (Becton-Dickinson), gating on leukocytes using Leukogate (Becton-Dickinson). Results are reported as percentage positive based on threshold values of fluorescence determined using suitable isotype-specific control antibodies (Becton-Dickinson or Olympus). HistopathologyandImmunopathology. Four micron sections were cut andmounted on Probe-on Plus (Fisher Scientific, Pittsburg, PA) slides for immunohistochemical staining. One slide was stained with hematoxylin and eosin for histopathology. The antibody panel used was a modification of a panel shown to identify lymphocyte lineage with approximately 95%accuracy.14 Antibodies included leukocyte common antigen (LCA, CD45; DAKO, Carpenteria,CA), L26 (CD20; DAKO), 4KB5 (CD45Ra; DAKO), MB2 (Biotest, Swedesboro, NJ), UCHL-I (CD45Ro; DAKO), CD3 (DAKO)," MTI (CD43; Biotest), Ber-H2 (CD30; Biotest)," Leu-MI (CD15; Becton-Dickinson), and KP-1 (CD68; DAKO)." Additional antibodies including CD5 (Becton-Dickinson), CD8 (Becton-Dickinson), CD4 (Becton-Dickinson), CD2 (Coulter, Marietta, Ga), CD7 (Becton-Dickinson), CD1 (Becton-Dickinson), and CD22 (DAKO) were applied to frozen sections. Each antibody was applied at optimal dilutions followed by application of a biotinylated secondary antibody. Alkaline phosphatase-conjugated streptavidin wasthen reacted withthe biotinylated secondary antibody andthe complex detected using fast red TR. Counterstaining was with hematoxylin followed by a polymeric covering. Each reagent was applied in uniform volume by capillary action to paired slides on a code-on immunostainer (Fisher Scientific, Rochester, NY). Appropriate blocking agents, washes, and enzyme treatments were integrated. Reactions were scored by light microscopy. Clonalanalyses. High molecular weightDNAwas isolated by subjecting cells to lysis and digestion in I % sodium dodecyl sulfate and 200 ug/mL of Proteinase K (BRL Life Technologies, Gaithersburg, MD) and incubating overnight at37°C.DNAwas extracted with Tris-saturated phenol (0.5 molL Tris, pH 7.5) followed by chloroform-isoamyl alcohol (24: 1) and then precipitated in 0.3 mol/ L sodium acetate and 2 v01 of 95% ethanol. DNA was next digested withthe restriction enzymes BamHI (Oncor, Gaithersburg, MD), Table 1. Clinical Features of Patients With CD3'. CD56' LGL Leukemia Patient No. Age at diagnosis (yrs) 52 Sex Disease duration (mos) Recurrent infections Rheumatoid arthritis Systemic B symptoms Massive splenomegaly (g)* Lymphadenopathy 1 2 3 14 F 19 M 41 M 5 8* + + + +(2,926) +(1,700) +(2.900) * Deceased. t Normal spleen weight <250 g. + + + From www.bloodjournal.org by guest on February 6, 2015. For personal use only. 2317 CD3+, CD56+ LGL LEUKEMIA Table 2. Hematologic Features of Patients With CD+, CD%' LGL Leukemia Patient No. 3 1 2 14,800 11,692 2,368 30.8 97 29,900 26,312 2,691 47.8 101 19.000 64,300 50,797 99,400 90,454 62,800 55,264 At presentation: Leukocytes/pL LGUpL NeutrophiWpL Hematocrit % Platelets (1 X 103/pL) Within 3 mos of presentation: Leukocytes/pL LGUpL 15,200 3,800 35.1 208 EcoRI (Oncor) and Hind111 (Oncor) followed by Southern blot analysis using a 32P-labeled TCR p probe (Oncor). Epstein-Barr virus ( E N ) analyses. Genomic DNA was tested for an EBV-specific clonal marker using NJ6 E clone as probe (provided by Dr E. Kieff, Department of Medicine, Harvard University) in Southern blot analysis, as de~cribed.".'~This clone contains the 5.2-kb BamHI-EcoRI fragment that includes the 500-base pair terminal fragment of EBV.I8.l9 PCR amplification of EBV genome was performed as described19using oligonucleotide primers TC 70 and TC 72 (Research Genetics, Huntsville, AL). These primers are designed to amplify a 265-bp fragment of BMLF1, a single-copy gene of the EBV genome. Positive control DNA for both Southern blot and polymerase chain reaction (PCR) assays was DNA extracted from Raji cell line. The sensitivity of the PCR assay in these experiments enables the detection of as few as 10 EBV-infected Raji cells. Strict precautions were taken to guard against false-positive results cased by PCR contamination, as described." RESULTS Table 1 summarizes the clinical features of the patients. The acute, aggressive nature of the disease is evidenced by the presentation with systemic B symptoms, massive splenomegaly, extensive lymphadenopathy, and resistance to therapy. Features also atypical for T-LGL leukemia include absence of recurrent infections or rheumatoid arthritis. The hematologic profiles of the patients are outlined in Table 2. An absolute lymphocytosis was present in all pa- tients at presentation, with relatively high numbers of LGL compared with values typically observed in patients with TLGL leukemia (median 4 2 0 0 / ~ L )Of . ~ note, there were rapid increases (within 3 months) in circulating LGL to high levels in all patients. Such a finding is not observed in T-LGL leukemia but is typical for NK-LGL leukemia. None of the patients was neutropenic. All patients had moderate degrees of thrombocytopenia, either at presentation or with disease progression. Leukemic cells in all three patients coexpressed CD3 and CD56 (Table 3). In patient no. 1, the percentage of doublelabeled CD3+CD56+cells was lower; however, this analysis was not done on presentation but after extensive treatment with multiple chemotherapeutic agents. It is reasonable to assume that this value may have been higher at presentation because decreases in circulating LGL were seen, at least transiently, as a consequence of treatment. Leukemic cells were also CD8+. Variable expression of CD16 and CD57 were noted on leukemic LGL. Characteristic histopathologic features of CD3+, CD56+ T-LGL leukemia are shown in Fig 1. Massive splenomegaly was aprominent feature of the disease in each patient. Spleen weights ranged from 1,700 to 2,900 g, with normal being less than 250 to 300 g. Histologically, each spleen specimen showed extensive, diffuse infiltration of the splenic red pulp cords and sinuses by lymphoid cells (Fig IC and d). These findings are similar to those seen in typical T-LGL leukemia." Variable degrees of atrophy of the white pulp were also noted in these patients, in contrast to follicular hyperplasia usually noted in T-LGL leukemia." Immunoperoxidase staining of frozen section from each spleen confirmed that infiltrating lymphoid cells had the same phenotype as circulating LGL (not shown). DNA hybridization studies showed clonal rearrangement of TCR p gene in each patient (Fig 2). There was no hybridization with the NJSE probe (not shown), indicating that the clonal expansion of LGL was not related to Epstein-Barr virus (EBV) infection. Using PCR analysis we were able to detect EBV sequences in PBMC from only one of these patients, at a low copy number. Subsequent testing byin situ hybridization showed only occasional positive cells consistent with a background of previous EBV infection. Table 3. One- and Two-Color Flow Cytometry Analysis of PBMC % Positive Absolute No./pL Patient No. 1 2 3 Normals Antigens CD3 CD4 CD8 CD16 CD57 CD3TDI6' CD3+CD56+ CD3TD57' 94 8 77 3 6 ND 45' ND 95 1 93 66 0 66 94 0 99 0 85 88 40 89 95 41 74 + 6 47 + 4 25 + 5 9+4 13 + 6 + Normals values are mean SD of 10 normal subjects. Abbreviation: ND, not done. Value obtained after treatment. I f 1 2+1 10 4 +- 1 2 3 10,990 935 9,003 351 701 ND 1,439' ND 24,996 263 24,970 13,638 0 13,638 19,521 0 10,169 0 8.731 5,650 4,109 9,142 9,758 4,212 Normals 1.448 910 485 174 263 25 32 204 + 325 + 188 + 149 + 94 + 131 + + + 28 16 99 From www.bloodjournal.org by guest on February 6, 2015. For personal use only. GENTILE 2318 AL Fig 1. Characteristic histopathologic features of CD3'. CD56' T-LGL leukemia. (A) Peripheral blood showing typical LGL (hematoxylin-eosin stain, original magnificationx 250). (B) Anormal lymphoidcells admixed diffusely among normalhematopoietic elements inbone marrow (hematoxylin-eosin stain, original magnification x 2501. Serologic reactivity to human T-cell leukemia virus VI1 antigens was tested in all three patients. Serum from each patient was enzyme-linked immunosorbent assay negative and Western-blot indeterminant, similiar to previously published observations in patients with T-LGL leukemia?' DISCUSSION We describe a new disease, CD3+, CD56' LGL leukemia. which is anaggressive variant of T-LGL leukemia. The characteristic features of this disorder include clonally expanded CD3+,CD56+ LGLthat increase rapidly after diagnosis, systemic B symptoms (fever, nightsweats, weight loss), and massive splenomegaly. Moderate thrombocytopenia and lymphadenopathy are also observed. Common features of TLGL leukemia such as neutropenia, recurrent bacterial infections, and rheumatoid arthritis did not occur in the CD3+, CD56+ variant. Indeed, the clinical presentation of this disease is unlike the usual clinical course of T-LGL leukemia, but remarkably similar to features of NK-LGL leukemia. The cellular origin of the malignant LGL clone in our From www.bloodjournal.org by guest on February 6, 2015. For personal use only. CD3'.CD56' LGLLEUKEMIA 2319 Fig 1. ICont'd) (C) Infiltration of splenic red pulp cords and sinuses by LGL (hematoxylin-eosinstain, original magnification x 251. ID) Infiltration ofsplenic red pulp cords and sinuses by LGL fhematoxylin-eosin stain, original magnification x 250). patients is not known. CD56 is expressed on approximately 15% of normal PBMC, which have LGL morphology and mediate non-major histocompatibility complex-restricted cytotoxicity. The majority of these cells are NK cells, i.e. CD3-, CD56+. However, a small percentage ofnormal PBMC coexpress CD3 and CD56.22Itis likely that these LGL represent the normal counterparts of the leukemic LGL. Alternatively, it isconceivable that leukemic cells arose from normal T cells (CD3', CD56-), with upregulation of CD56 after activation. Supporting this hypothesis, marked expansion of CD3', CD56' cells can be generated in vitro from normal CD3+,CD56- T-cell precursors after activation with interleukin (1L)-l, IL-2, and interferon Our data suggest that expression of CD56 is an important biological marker in LGL leukemia. LGL leukemias expressing CD56, whether of NK (CD3-) or T-cell (CD3+) origin, have similar aggressive clinical features. In contrast, T-LGL leukemias not expressing CD56 have different manifestations and a chronic clinical course. A relationship between NK immunophenotype and biological behavior has been previously reported. Sheibani et a124observed that lymphoblastic lymphomas expressing NK-associated antigens showed From www.bloodjournal.org by guest on February 6, 2015. For personal use only. 2320 GENTILE ET AL mw 24 - episomes have a uniform configuration.'" These data support a clonal process that implicates EBV directly in the pathogenesis of both these diseases. In contrast, such analyses were negative in our patients. Furthermore, after PCR amplification we detected EBV sequences in only one patient, at a low copy number. These results do not support a role for EBV infection in CD3', CD56' LGL leukemia. Further studies are needed to elucidate the pathogenesis of this newly delineated disease. I -: REFERENCES I . Loughran TP Jr, Starkebaum G: Large granular lymphocyte leukemia: Report of 38 cases and review of the literature. Medicine - 7.7 66397, 1987 2. Chan WC, Link S, Mawle A, Check I, Brynes RK, Winton E F Heterogeneity of large granular lymphocyte proliferations: Delineation of two major subtypes. Blood 68:1142, 1986 3. Semenzato G, Pandolfi F, Chisesi T, DeRossi G , Pizzolo G, Zambello R, Trentin L, Agostini C, Dini E, Vespignani M, Cafaro A, Pasqualetti D, Giubellino MC, Migone N. Foa R: The lymphoproliferative disease of granular lymphocytes. A heterogeneous disorder ranging from indolent to aggressive conditions. Cancer 60297 1, 1987 4. Loughran TP Jr: Clonal diseases of large granular lymphocytes. Blood 82: I , 1993 5. Taniwaki M, Tagawa S, Nishigaki H. Horiike S, Misawa S, - 3.7 I 2 3 4 Fig2.Southern-blotanalysisusing32-P-labeled TCR /3 probe. Lane 1: placental DNA digested with B a d 1 restriction enzyme. Lane 2 DNA from patient no. 2 digested with B a d 1 restriction enzyme. Lane 3 placental DNA digested with Hindll restriction enzyme. Lane 4 DNA from patient no. 2 digested with Hindll restriction enzyme. Similiar results were obtained for patients no.1 and 3 (not shown). a more aggressive clinical course. However, CD56 was not included in their panel of NK-associated antigens. CD56 (leu-19, NKH-1) is a 220,000-d glycoprotein corresponding to neural cell adhesion molecule (NCAM). NCAM isa member of the immunoglobulin superfamily of cell adhesion molecules, and is found on cells in a variety of tissues including brain, nerve, muscle, gastrointestinal, and nasopharynx.2s''" NCAM mediates cell adhesion by exhibiting homophilic (like to like) binding, and as such may lead to cell targeting to tissues which also express NCAM. For example, nonHodgkin's lymphomas of T-cell lineage and coexpressing CD56 characteristically involve the nasopharynx and other tissues that normally express NCAM.3"O'3' Such CD56' lymphomas are part of a clinical spectrum of angiocentric immunoproliferative lesions (AIL), including lethal midline granuloma and lymphomatoid granulomatosis, as reviewed by Peiper.32 Molecular analyses of EBV-fused termini in CD56 expressing NK-LGL leukemias and AIL have shown that viral Shimazaki C, Maekawa T, Fujii H, Kitani T, Abe T Chromosomal abnormalities define clonal proliferation in CD3- large granular lymphocyte leukemia. Am J Hematol 33:32, 1990 6. Koizumi S, Seki H, Tachinami T, Taniguchi M, Matsuda A, Taga K, Nakarai T, Kat0 E, Taniguchi N. Nakamura H: Malignant clonal expansion of large granular lymphocytes with a Leu I I +, Leu 7-surface phenotype: In vitro responsiveness of malignant cells to recombinant human interleukin 2. Blood 68:1065. 1986 7. Ohno T, Kanoh T, Anta Y,Fujii H, Kuribayashi K. Masuda T, Horiguchi Y,Taniwaki M, Nosaka T, Hatanaka M, Uchino H: Fulmanent clonal expansion of large granular lymphocytes. Characterization of their morphology, phenotype, genotype, and function. Cancer 64:1918, 1988 8. Ohno Y,Amakawa R, Fukuhara S, Huang C-R, Kamesaki H, Amano H, Imanaka T, Takahashi Y,Anta Y,Uchiyama T, Kita K, Miwa H: Acute transformation of chronic large granular lymphocyte leukemia associated with additional chromosome abnormalities. Cancer 64:63, 1989 9. Wallis WJ. Loughran TP Jr. Kadin ME, Clark EA, Starkebaum GA: Polyarthritis and neutrapenia associated with circulating large granular lymphycytes. Ann Intern Med 103:357,1985 IO. Loughran TP Jr. Starkebaum GA, Kidd P, Neiman P Clonal proliferation of large granular lymphocytes in rheumatoid arthritis. Arthritis Rheum 31:31, 1988 1 I . Gonzales-Chambers R, Przepiorka D, Winkelstein A, Agarwal A, S t a n T W , Kline WE, Hawk H: Lymphocyte subsets associated with T cell receptor beta chain rearrangement in patients with rheumatiod arthritis and neutropenia. Arthritis Rheum 35:516, 1992 12. Fernandez LA, Pope B, Lee C, Zayed E Aggressive natural killer cell leukemia in an adult with establishment of an NK cell Line. Blood 67:925, 1986 13. Sheridan W, Winton EF, Chan WC, Gordon DS, Vogler WR, Phillips C, Boniovanni KF, Waldman T A Leukemia of non-T lineage natural killer cells. Blood 72:1701. 1988 14. Elghetany MT. Kurec AS, Schueler K. Forbes BA, Duggan DB, Davey FR: lmmunophenotyping of non-Hodgkin's lymphomas in paraffin-embedded tissue sections. A comparison with genotypic analysis. Am J Clin Path01 95:517, 1991 From www.bloodjournal.org by guest on February 6, 2015. For personal use only. CD3+, CD56+ LGL LEUKEMIA 15. Mason DY, Cordell J, Brown M, Pallesen G, Ralfkiaser E, Rothbard J, Crumpton M, Gatter KC: Detection of T-cells in paraffin wax embedded tissue using antibodies against a peptide sequence from the CD3 antigen. J Clin Pathol 42:1194, 1989 16. Schwarting R, Gerdes J, Durkopp H, Falini B, Pileri S, Stein H: BER-H2: A new anti-Ki-l (CD30) monoclonal antibody directed at a formol resistant epitope. Blood 74:1678, 1989 17. Pulford KA, Rigney EM, Micklem KJ, Jones M, Stross WP, Gatter WP, Mason DY: KP1: A new monoclonal antibody that detects a monocytelmacrophage associated antigen in routinely processed tissue sections. J Clin Path01 42:414, 1989 18. Loughran TP Jr, Zambello R, Ashley R, Guderian J, Pellenz M, Semenzato G, Starkebaum G: Failure to detect Epstein-Barr virus DNA in peripheral blood mononuclear cells of most patients with large granular lymphocyte leukemia. Blood 81:2723, 1993 19. Raab-Traub N, Flynn K: The structure of the termini of the Epstein-Barr virus as a marker of cellular clonal proliferation. Cell 47:883, 1986 20. Agnarsson BA, Loughran TP Jr, Starkebaum G, Kadin ME: The pathology of large granular lymphocyte leukemia. Hum Pathol 20:643, 1989 21. Starkebaum G, Loughran TP,Jr, Kalyanaraman VS, Kadin ME, Kidd PG, Singer JW, Ruscetti F W : Antibodies to human T cell leukemidymphoma virus type I in sera of patients with leukemia of large granular lymphocytes. Lancet 1:596, 1987 22. Lanier L, Le AM, Civin C, Loken M, Phillips J: The Relationship of CD16 (Leu-11) and Leu-l9 (NKH-1) antigen expression on human peripheral blood NK cells and cytotoxic T lymphocytes. J Immunol 136:4480, 1986 23. Schmidt-Wolf IGH, Lefterova P, Mehta BA, Fernandez LP, Huhn D,, Blume KG, Weissman IL, Negrin RS: Phenotypic characterization and identification of effector cells involved in tumor cell recognition of cytokine induced killer cells. Exp Hematol 21: 1673, 1993 2321 24. Sheibani K, Nathwani BN, Winberg CD, Burke JS, Swartz WG, Blayney D, Van De Veld S, Hill LR, Rappaport H: Antigenically defined subgroups of lymphoblastic lymphoma. Relationship to clinical presentation and biologic behavior. Cancer 60: 183, 1987 25. Lanier L, Testi R, Bind1 J, Phillips J: Identity of Leu-l9 (CD56) leukocyte differentiation antigen and neural cell adhesion molecule. J Exp Med 169:2233, 1989 26. Lanier L, Chang C, Azuma M, Ruitenberg J, Hemperly J, Phillips J: Molecular and functional analysis of human natural killer cell associated neural cell adhesion molecule (N-CAWCD56). J Immunol 146:4421, 1991 27. McClain D, Edelman G: A neural cell adhesion molecule from human brain. Proc Natl Acad Sci USA 79:6380, 1982 28. Cunningham B, Hemperly J, Murray B, Prediger E, Brackenbury R, Edelman G: Neural cell adhesion molecule: Structure, immunoglobulin like domains, cell surface modulation and alternative RNA splicing. Science 236:799, 1987 29. Thomas P, Pietrangeli C, Hayashi S-I, Schachner M, Goridis C, Low M, Kincade P: Demonstration of neural cell adhesion molecules on stromal cells that support lymphopoeisis. Leukemia 2: 171, 1988 30. Kern W, Spier E, Hanneman T, Miller M, Matzner M, Grogan T: Neural cell adhesion molecule positive peripheral T-cell lymphoma: A rare varient with a propensity for unusual sites of involvement. Blood 79:2432, 1992 31. Ng CS, Chan JKC, Lo STH: Expression of natural killer cell markers in non-Hodgkin's lymphomas. Hum Pathol 18: 1257, 1987 32. Peiper SC: Angiocentric lymphoproliferative disorders of the respiratory system: Incrimination of Epstein-Barr virus inpathogenesis. Blood 82:687, 1993 33. Ho FCS, Srivastava G, Loke SL, Fu KH, Leung BPY, Liang R, Choy D:Presence of Epstein-Barr virus DNA innasal lymphomas of B and T cell type. Hematol Oncol 8:271, 1990. From www.bloodjournal.org by guest on February 6, 2015. For personal use only. 1994 84: 2315-2321 CD3+, CD56+ aggressive variant of large granular lymphocyte leukemia [see comments] TC Gentile, AH Uner, RE Hutchison, J Wright, J Ben-Ezra, EC Russell and TP Jr Loughran Updated information and services can be found at: http://www.bloodjournal.org/content/84/7/2315.full.html Articles on similar topics can be found in the following Blood collections Information about reproducing this article in parts or in its entirety may be found online at: http://www.bloodjournal.org/site/misc/rights.xhtml#repub_requests Information about ordering reprints may be found online at: http://www.bloodjournal.org/site/misc/rights.xhtml#reprints Information about subscriptions and ASH membership may be found online at: http://www.bloodjournal.org/site/subscriptions/index.xhtml Blood (print ISSN 0006-4971, online ISSN 1528-0020), is published weekly by the American Society of Hematology, 2021 L St, NW, Suite 900, Washington DC 20036. Copyright 2011 by The American Society of Hematology; all rights reserved.
© Copyright 2026