of fluid and electrolyte balance, the haemodynamics of shock and
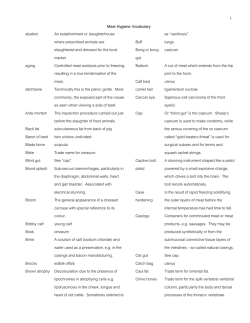
METABOLIC AND BLOOD COAGULATION CHANGES DURING INTRAVENOUS FAT INFUSIONS Arris and Gale Lecture delivered at the Royal College of Surgeons of England on 12th July 1967 by D. J. Reid, D.M., M.Ch., F.R.C.S. Consultant Surgeon, Brighton, Lewes and Mid-Sussex Hospitals IN SURGERY TO-DAY, emphasis has moved from speed in operative surgery to the overall care of the patient during the whole period of treatment. Much attention has been paid to problems such as anaesthesia, restoration of fluid and electrolyte balance, the haemodynamics of shock and the protection of blood flow to the kidneys. Of equal importance, however, and often neglected, is the nutrition of the patient; and although periods of relative starvation are well tolerated by the majority of patients undergoing routine surgical procedures, there are cases where adequate attention to this aspect of treatment may prove crucial to the survival of the patient. During all the stages of treatment in surgical patients there is an increase in demand for calories, which is often far greater than realized. Three to four times the number of calories required for a normal patient at rest may be required for the same patient in this early post-operative phase. Fever increases metabolic rate. Destruction of body tissues has to be made good by protein synthesis which requires energy. Wound healing requires protein and energy. At these times oral intake of food is often impossible, especially in operations on the gastro-intestinal tract. The deficiency is therefore more acute as demand increases and supplies are withheld. The body withstands starvation by drawing on reserves. At first glycogen stores in muscle and liver are utilized, but these are soon exhausted. The supplies of liver glycogen, which amount to only an average of 400 Gm., are rather less than the average daily intake of carbohydrate. Energy requirements are then met by the catabolism of fat and body protein. The length of time which any individual can survive a period of total starvation naturally depends on the extent of available body stores of fat and protein. Women's greater resistance to starvation was observed at Stalingrad in 1942 and in Holland in 1945. This is presumably due to the greater body stores of fat in women. For the well nourished with large stores of body fat, it is possible to remain in positive nitrogen balance for a considerable time on severely deficient calorie diets, provided a small quantity of protein is available in the diet. For the poorly nourished, this period is greatly reduced and 322 METABOLIC AND BLOOD COAGULATION CHANGES both the hazards of a surgical operation and the period of convalescence will be increased. If a patient is maintained for a long period in a state of malnutrition, hepatic dysfunction and hypoproteinaemia will follow. Wound healing is delayed, decreased tolerance to shock producing circumstances occurs, patients may exhibit an instability of blood pressure disproportionate to any actual haemorrhage and may respond unsatisfactorily to transfusion of blood and plasma. The gastro-intestinal tract is undoubtedly the best route to administer nourishment, but often this is impossible at the time when it would be most beneficial, so the intravenous route becomes necessary as a method of patient feeding. To provide 3,000 Cal. intravenously in the form of 5 per cent dextrose would require the administration of 15 litres. Fat when completely metabolized can yield 9 Cal./Gm. Intralipid 20 per cent, a new form of intravenous fat emulsion containing glycerol, provides 2,000 calories per litre. A form of intravenous fat which is safe has long eluded the researcher. The reason for this is that, in the normal human, fat exists in the circulation in a highly dispersed state, 1 micron or less in diameter, the droplets exhibiting Brownian movement. For a fat emulsion to be tolerated in the body, it must exist in this form. In order to achieve this state of dispersion, it is necessary to lower the surface charge on the fat droplets by utilization of an emulsifying agent. It is the toxicity of the emulsifying agents, which appear to be toxic in direct relationship to their value as emulsifying agents, that has limited the development of fat emulsions. A number of emulsions are now available which appear to be well tolerated, although it would be unwise to accept their complete safety yet. The material to be presented was carried out first to confirm that fat administered intravenously has an effect on body metabolism and secondly that its administration does not adversely affect the process of blood coagulation. The emulsion Intralipid, manufactured by the Vitrium Company of Sweden, has been used throughout this work. Intralipid is a soya bean oil in water emulsion with egg yolk phosphatide 1.2 per cent as the emulsifying agent. Glycerol 2.5 per cent is added to maintain isotonicity. 150 ml. N. sodium hydroxide is added to 500 litres of the emulsion to counteract the effect of free fatty acids liberated from the emulsion during storage. The particle size is approximately 1 micron in diameter. The emulsion has a shelf life of approximately one year. When exposed to high temperatures free fatty acids are liberated spontaneously from the emulsion and it is therefore necessary to store the material at 4° C. There is, however, no free fatty acid present in the emulsion when it is adequately stored. Fractionation of the phospholipid fraction present in the egg yolk phosphatide shows that 30 per cent is present in the form of phosphatidyl ethanolamine and the remainder is lecithin. 323 D. J. REID The metabolic action of Intralipid has been studied in two ways. First, nitrogen balance studies have been carried out and, secondly, changes in oxygen consumption and respiratory quotient have been measured in patients receiving the emulsion. In interpreting the results of nitrogen balance studies there are various points which must be borne in mind. 1. A period of adjustment is required before a balance experiment can be started, to ensure that the subject is in a stable metabolic state and has come into equilibrium on a stabilized diet. 2. Estimations of intake calculated on the weight of various items constituting the diet are not satisfactory. A stable oral intake cannot be relied upon as the protein content of various foods may vary considerably. Intake must be estimated by the technique of sampling and measured directly for its nitrogen content. 3. There may be spontaneous variations in nitrogen output which make measurements over a short period unreliable. 4. Adequate controls are necessary for interpretation of results. This makes experiments during the operative phase extremely difficult to plan and assess as there is no way of comparing two identical patients in the same situation. A surgical operation in the middle of a balance period introduces so many unknown quantities, such as increased energy demand and degrees of surgical trauma, that it is difficult to interpret results which include this phase. 5. Experiments are often carried out on the assumption that faecal excretion of nitrogen remains constant. This cannot be accepted where finer differences in nitrogen balance are expected. 6. Frequently in experimental work published on this subject, it is stated that nitrogen requirements were supplied intravenously in the form of plasma, albumen or protein hydrolysates. These substances may remain in the body tissue fluids for some time before being excreted or metabolized. They may therefore give a false impression of positive nitrogen balance over short periods, especially when compared with groups who were not supplied in this way. In a recent critical analysis of metabolic balance studies by Isaksson and Sjogren (1964), attention was drawn to nitrogen excretion in the sweat as a cause of false balance studies. Loss of nitrogen in the sweat might amount to anything between 20 and 130 mg. per 100 ml. sweat. Mitchell and Hamilton (1949) observed that, with a daily intake of 98 Gm. protein, the nitrogen excretion in sweat of men profusely sweating averaged 152 mg. per hour or 22.5 per cent of the total daily output. During conditions of minimal or normal sweating 15 mg. per hour occurred or 2.7 per cent of the total daily output. The changes are important in assessing where equilibrium lies and investigations must be carried out in air-conditioned surroundings at a constant temperature and humidity. 324 METABOLIC AND BLOOD COAGULATION CHANGES With these points in mind the following investigation has been carried out. Six patients understanding the experimental nature of these investigations were admitted to the Metabolic Ward of St. Thomas's Hospital. It was necessary to choose patients first who would benefit from intravenous feeding and secondly who were in stable states of metabolism and not suffering from any form of gastro-intestinal disturbance that might produce diarrhoea or vomiting. TABLE I THE COMPOSITION OF THE ORAL DIET THROUGHOUT THE EXPERIMENTAL PERIOD IN THE SIX PATIENTS STUDIED Case No. Oral Diet throughout Experiment (g. per day) Protein Fat Carbohydrate Protein Total Calorie Intake during Calorie Periods of Value Intravenous Feeding (calories per day) (calories per day) 1983 983 39 47 106 2604 2 57 1604 Fat 63 Carbohydrate 189 39 1901 3 Protein 901 Fat 10 Carbohydrate 163 2700 4 Protein 46 1200 37 Fat Carbohydrate 165 37 1495 2495 5 Protein 70 Fat Carbohydrate 167 39 1905 6 Protein 905 11 Fat Carbohydrate 162 During periods 7 and 8 in Case 6 the otal intake was increased to: protein 40 g. fat 76 g., and carbohydrate 245 g., yielding 1,824 calories per day. 1 Each patient was stabilized for five days on the diet of known composition before any measurements were made. Each patient was studied in five-day periods, over a total period of 30 days in Cases 1-5, and 40 days in Case 6. The patients received oral diet as shown in Table I. The first two five-day periods were control periods during which the patients received the oral diet only. Water was allowed freely throughout the periods of study. During the second two five-day periods the oral diet continued unchanged but the patients received additional calories in the form of intravenous fat bringing the total calories administered to the levels indicated in the right-hand column. In the sixth case there were an additional two five-day periods of study during which the additional calories supplied intravenously in periods 3 and 4 were supplied orally in periods 7 and 8. Daily urine collections were made from 10 a.m. to 325 D. J. REID 10 a.m. The patients started each 24 hour urine save at 10 a.m. with an empty bladder. At the end of each 24-hour period, the volume of urine passed in that period was measured and a sample set aside for nitrogen estimation. The Kjeldahl technique was used for nitrogen estimation. Faecal saves were collected in five-day periods, using a carmine-dye marker to indicate the end of one period and the beginning of another. CAR 1. A.c OaOr DUCENAL 2mwth w CAn oT 'ADA * N Ca wAm CAK a fwS d~so am ?C .'M~ ~ ~ ~ ~ ?f C^#4TOCOCOFSMI4CHSl NJO CCi_ bE*.C IICE (b) (a) G%e ~ 016 16 (d) ~ (c) ~ ~~. 9 "F ( b) II =l (c) Fig. 1. Charts I to 6 demonstrate urinary nitrogen excretion (Gm./day), nitrogen balance and fat balance in six patients. Intravenous fat was administered between days 10 and 20 in each patient. In the sixth patient, additional oral calories were administered between days 30 and 40. The charts in Figure I demonstrate the results obtained. The top row of results show the daily urinary nitrogen excretion measured in Gm. nitrogen per day. From the 10th to the 20th day (periods 3 and 4) daily intravenous infusions of fat were administered as shown on the charts. The emulsion was administered over a period of approximately 7 hours. The middle row of results show the overall nitrogen balance in five-day periods. Nitrogen intake is measured from the zero line downwards and nitrogen excretion is measured from the intake line upwards. Hence the 326 MM METABOLIC AND BLOOD COAGULATION CHANGES patient is in positive balance when the total nitrogen excretion is less than the total intake. In this case the nitrogen excretion line will fall below the zero line. When the patient is in negative nitrogen balance the nitrogen excretion line will fall above the zero line. The lowest row of results demonstrates fat balance. Intake is measured from the zero line upwards and output from the zero line downwards. This part of the investigation was carried out to investigate whether faecal fat excretion changed significantly during the periods of intravenous fat feeding. In Figure 1, Chart 1 demonstrates a patient in borderline balance but slightly in negative balance in the two control periods. In the periods during which fat was administered intravenously definite positive balance has been achieved. In the final two control periods the patient is again in borderline balance. No significant change in faecal fat excretion occurs during periods 3 and 4. Chart 2 demonstrates a patient in positive balance throughout the study, though in borderline balance in periods 1 and 6. During periods 3 and 4 there is a slight improvement in the degree of positive balance. Again no change occurs in faecal fat excretion during the periods of intravenous fat feeding. In Chart 3 the patient is in strong negative balance in the control periods before and after intravenous fat feeding but is in positive balance during the period of intravenous feeding. No change occurs in faecal fat excretion during periods 3 and 4. The patient shown in Chart 4 is in strong positive balance throughout the study. No real change has occurred during the period of intravenous feeding and again no change in faecal fat excretion occurred in periods 3 and 4. This patient received 150 Gm. fat daily as against 100 Gm. daily in the other patients. Chart 5 demonstrates another patient who is in positive nitrogen balance throughout and in whom no real change occurs either in nitrogen balance or in faecal fat excretion during the period of intravenous fat feeding. In the sixth patient it is seen that a strong negative balance exists in the first control period while the patient is receiving 900 Cal. daily by mouth. When the patient receives additional calories intravenously to bring the total intake to 1,900 Cal. he comes into strong positive balance but returns to a negative balance in the second control period. In periods 7 and 8 the same additional calories as were administered intravenously in periods 3 and 4 are administered orally and a similar positive nitrogen balance is achieved. These studies show that the patients who are in strong negative balance in the control periods (3 and 6) come into strong positive balance when given intravenous fat. Cases 1 and 2 are on the borderline between positive and negative balance in the control periods and some slight in327 D. J. REID crease in nitrogen retention occurs during the periods of intravenous feeding. Cases 4 and 5 were in positive balance throughout the study and no further improvement in nitrogen excretion occurred during the periods of intravenous feeding. No fever was recorded in any patient throughout the studies and no toxic symptoms were observed. TABLE II Table II shows the Respiratory Quotient (R.Q.), Oxygen Consumption (O.C.) in ml./min., and Metabolic Rate (M.R.) expressed in percentage change from the preinfusion level. The pre-infusion results are the mean of three separate measurements. Patients 1 to 5 received 1.5 Gm. fat per kg. of body weight in one hour. Patients 6 to 8 received 2 Gm. fat per kg. of body weight in one hour, and patients 9 and 10 received 3 Gm. fat per kg. body weight in one hour. Case 1 2 3 4 5 6 7 8 9 10 Pre-infusion R.Q. O.C. M.R. R.Q. O.C. M.R. R.Q. O.C. M.R. R.Q. O.C. M.R. R.Q. O.C. M.R. R.Q. O.C. M.R. R.Q. O.C. M.R. R.Q. O.C. M.R. R.Q. O.C. M.R. R.Q. O.C. M.R. 0.88 220 0 1.11 157 0 0.85 166 0 0.81 206 0 0.92 225 0 0.72 156 0 0.80 206 0 0.79 201 0 0.82 242 0 0.75 171 0 1 0.86 226 +2.5 1.12 178 +16.7 0.83 200 +20.3 0.74 212 +2.4 0.79 256 +13.4 0.70 184 +18.1 0.74 232 +12.8 0.7.8 208 +3.1 0.75 260 +8.7 0.73 186 +7.6 Hours after Start of Infusion 2 3 4 5 0.95 0.80 0.81 0.88 262 263 268 232 +21.3 +18.0 +19.2 +5.6 0.94 1.14 0.97 1.02 188 178 183 173 +23.1 +16.7 +20.6 +14.1 0.88 0.82 0.82 0.88 208 168 183 187 +26.1 +1.2 +10.7 +13.2 0.82 0.94 0.78 0.97 208 246 219 198 +1.2 +20.1 -3.5 +7.1 0.83 0.78 0.85 0.82 281 271 292 268 +23.2 +18.3 +28.1 +19.6 0.93 0.74 0.76 0.84 184 194 177 193 +16.6 +25.6 +21.5 +12.8 0.80 0.89 0.77 0.84 209 245 230 230 +1.5 +18.1 +11.6 +11.6 0.84 0.82 0.92 0.84 207 226 201 217 +3.1 12.4 0 +7.3 0.78 0.77 0.77 0.74 287 276 285 263 +19.5 +9.8 +12.0 +18.4 0.74 0.75 0.75 0.76 189 195 191 191 +8.7 +11.5 +11.5 +13.0 6 - - 0.90 221 +7.1 0.96 265 +15.8 - - 0.73 267 +28.4 - - 0.78 262 +7.6 - - Further proof of utilization of Intralipid comes from a study of oxygen consumption and respiratory quotient in patients receiving the fat emulsion. Ten patients who received the emulsion were studied throughout the period of infusion and for several hours afterwards (Table IL). Patients 1-5 received 1.5 Gm. fat/Kg. body weight over 1 hour. Patients 6-8 received 2 Gm. fat/Kg. body weight and patients 9 and 10 received 3 Gm. fat/Kg. body weight over a period of 1 hour. The pre-infusion values shown are the mean of three separate estimations. Patients have been studied at hourly intervals after start of the infusions. A fall in respiratory quotient towards 0.7 would indicate the metabolism of fat. The respiratory quotient results all show some fall during or after the infusion compared with the average figure before the start of the infusion. 328 METABOLIC AND BLOOD COAGULATION CHANGES Some patients had a low resting respiratory quotient. This was noted particularly in debilitated patients who were suffering from carcinomatosis (cases 6 and 10). A low respiratory quotient in these patients might be expected as they are probably burning endogenous fat. In these patients a further drop in respiratory quotient has occurred although the fall is small (0.72 to 0.70 and 0.75 to 0.73 respectively). The fall in respiratory quotient does not persist throughout the experiments and, although the oxygen consumption usually remains elevated throughout the period of study, the respiratory quotient often rises later in the experiment, in some cases above the resting level. In one patient a respiratory quotient above 1 was recorded which must be due to persistent overbreathing. TABLE III RESPIRATORY QUOTIENT, OXYGEN CONSUMPTION, AND PERCENTAGE CHANGE IN METABOLIC RATE OF PATIENT GIVEN INTRAVENOUS SALINE AND INTRALIPID ON Two SEPARATE DAYS Saline Infusion (510 ml. over 90 min.) Respiratory quotient .. Oxygen consumption (ml. per min.) Percentage change in metabolic rate .. Pre-infusion (average of 3 Hours after Start of Infusion 1 2 3 4 readings) 0.75 0.79 0.76 0.77 0.75 268 245 243 264 272 0 -8 -8 -2 +2 5 0.78 261 -3 Intralipid Infusion (1.5 g. per kg. over 90 min.) Pre-infusion (average of 3 Hours after Start of Infugion 1 2 3 5 4 readings) 0.77 0.74 0.72 0.72 0.72 0.74 Respiratory quotienit .. 277 257 245 275 275 235 Oxygen consumpticin .. (ml. per min.) Percentage changeIin 0 +8 +17 +18 +17 metabolic rate .. +4 Oxygen consumption increases in all patients studied. Metabolic rate increases by an average of 21 per cent in the 10 patients, indicating a specific dynamic action of fat. The emulsion is acting as a metabolic stimulus. When a single patient was studied with a saline infusion and an Intralipid infusion it was found that metabolic rate was increased only in the patient receiving the fat emulsion (Table III). It has been shown that the oral ingestion of fat causes changes in certain blood coagulation tests in the direction of increased coagulability. Chylomicrons, blood platelets, certain phospholipids and some fatty acids all increase the coagulability of blood. Certain phospholipids, notably phosphatidyl serine and phosphatidyl ethanolamine, are highly thromboplastic. Platelets contain these phospholipids and one of them, phosphatidyl ethanolamine, is present in Intralipid. There is a theory that the process of fibrin formation and fibrinolysis is not only a process which occurs following damage to a blood vessel wall, but that it is a continual process throughout the circulation. 329 D. J. REID This theory is not supported, however, by any real evidence. There is conflicting. evidence about the effect of lipoproteins on the process of fibrinolysis. Cholesterol appears to be inhibitory in fibrinolysis whereas neutral fat is not. The effect of Intralipid on various blood coagulation tests, including the process of fibrinolysis, has been studied. When the test is carried out on blood drawn from a patient who has received the emulsion intravenously the test is referred to as an in vivo test; when the emulsion is added to blood or plasma in a test tube the test is referred to as an in vitro test. The tests used in this study are the Partial Thromboplastin Time test (Langdell et al., 1953; Matchett and Ingram, 1965), the Thrombin Generation test (Macfarlane and Biggs, 1953), the Dilute Plasma Clot Lysis test (Mitchell and Briers, 1959) and a test of clot retraction measured by the wire spiral method (Macfarlane, 1939). In the Partial Thromboplastin Time (P.T.T.) test the coagulation mixture consists of platelet poor plasma (P.P.P.), Inosithin (1 mg./ml.), a buffer solution amino tris hydroxymethyl methane and calcium chloride solution. The effect of Intralipid on this coagulation test has been studied TABLE IV INTRALIPID AS A SOURCE OF PHOSPHOLIPID IN THE PARTIAL THROMBOPLASTIN TIME TEST Clotting Times Source of Phospholipid (sec.) (reagent concentrations) 62 .. .. .. .. None (buffer substituted) .. .. .. .. .. 32 .. Inosithin 1 mg./ml .. .. .. .. 58-61 Intralipid 2 per cent-20 per cent .. 28-29 Inosithin and Intralipid together in above concentrations by varying the phospholipid present in this mixture and recording the clotting time in seconds. These studies represent the mean values of 10 separate tests. When no phospholipid is present in the mixture the mean coagulation time is 62 sec. When Inosithin is present it is 32 sec. When Intralipid in concentration of 2 per cent to 20 per cent is added it does not significantly shorten the coagulation time compared to the times recorded in the tubes containing no phospholipid. When both Inosithin and Intralipid are present, the clotting time is similar to that when Inosithin alone is present (Table IV). It would appear, therefore, that Intralipid, even in concentrations exceeding those that would be obtained in patients receiving the emulsion, does not shorten the coagulation time in the Partial Thromboplastin Time test. When the two-stage Thrombin Generation test is employed a change is seen when Intralipid is introduced into the mixture. In the first stage of this test 1 ml. citrated whole blood or 0.5 ml. Platelet Poor Plasma or 0.5 ml. Platelet Rich Plasma are mixed with 0.5 ml. CaCl2 solut on (0.025 M.). At 1 minute intervals after this mixture is made 0.1 ml. are subsampled into tubes containing 0.4 ml. fibrinogen solution 330 METABOLIC AND BLOOD COAGULATION CHANGES (0.2 G./lOO ml.) and the clotting time is recorded. The results of thrombin 600 generation tests are plotted as against the sampling clotting time in sec. time in minutes. The reciprocal of the clotting time is more or less proportional to thrombin concentration. It has been shown previously (Amris et al., 1964) that both the rate and quantity of thrombin generation is increased by the addition of Intralipid to whole blood, platelet rich or platelet poor plasma and these findings are confirmed. The fat emulsion appears to replace the action of platelets. Fat might be producing this platelet replacement action by activating the contact mechanism of blood coagulation. In order to test this hypothesis the Thrombin Generation Test was carried out using blood samples drawn before and after an infusion of Intralipid. Citrated blood samples were taken in one case using glass equipment and in the other using siliconized oo THROMBIN GENERATION TEST BEFORE AND AFTER INTRALIPID INFUSION 20 20 ,ao / I0 1 2 3 4 S l7 S 9 o It. 12 TIME IN MINUTES Fig. 2. Lines 1 and 2 represent the thrombin generation test carried out on blood withdrawn with normal needles and glassware before and after infusion of Intralipid respectively. Lines 3 and 4 represent the test carried out on blood withdrawn with siliconized equipment before and after Intralipid infusion respectively. needles, syringes, pipettes and glassware. Hence in the samples taken into ordinary glass, the contact system was activated, and in those taken in siliconized equipment the contact system was not activated (Fig. 2). Lines 1 and 2 represent the thrombin generation curves using blood taken with ordinary glassware before and after Intralipid infusion respectively. Lines 3 and 4 represent the thrombin generation curves before and after the addition of Intralipid in blood withdrawn using siliconized equipment. If Intralipid was producing a thromboplastic action by activating the contact system, line 4 would approach line 1 on the graph. In fact very little change is noted in the curves with the addition of fat and the curves which result from non-contact blood (3 and 4) are closely comparable to those which result from contacted blood (1 and 2). Intralipid does not produce an increased rate of thrombin generation, therefore, by activating the contact system of blood coagulation. 331 D. J. REID THROMBIN GENERATION TEST PLATELET POOR PLASMA WITH INCREASING CONCENTRATION OF FAT EMULSION INTRALIPID TIME IN MINUTES Fig. 3. The thrombin generation test carried out on platelet-poor plasma. Lines 1 to 6 represent concentrations of Intralipid 0 per cent, 2 per cent, 4 per cent,18 per cent, 12 per cent and 16 per cent respectively. Using platelet poor plasma in the Thrombin Generation Test it is seen that the effect of Intralipid on thrombin generation increases as the concentration of Intralipid in the mixture increases (Fig. 3). Lines 1 to 6 represent concentrations of Intralipid of 0, 2, 4, 8, 12 and 16 per cent. There is little further effect, however, after 12 per cent. When the effect of Intralipid is compared to that of a number of other intravenous solutions commonly in use it is seen that Intralipid exerts a'far ALL TUBES CONTAIN 80 70 ML.PLATELET POOR PLASMA I.ML.CALCIUM OILORIDE M/40 THROMBIN GENERATION TEST 60 600/C.T. 50 40 30 20432 10 1 2 3 4 5 6 7 8 9 10 TIME IN MINUTES Fig. 4. Thrombin generation test carried out on platelet-poor plasma with the addition of: (1) aminosol fructose ethanol; (2) 12 per cent dextrose; (3) 10 per cent aminosol; (4) normal saline; (5) 5 per cent dextrose; (6) tetracycline solution (250 mg. in 500 ml. normal saline); (7) 20 per cent Intralipid. 332 METABOLIC AND BLOOD COAGULATION CHANGES greater effect in increasing thrombin generation than any of the others (Fig. 4). Line 1 represents the effect of aminosol fructose ethanol, 2 represents 12 per cent dextrose, 3 represents 10 per cent aminosol, 4 represents normal saline, 5 represents 5 per cent dextrose, 6 represents tetracycline solution 250 mg. in 500 ml. saline solution and 7 represents the effect of 20 per cent Intralipid. Intralipid appears therefore to exert a thromboplastic action, but its action is not great enough to be detected by the one-stage partial thromboplastin time. It can only be detected by the two-stage thrombin generation test. Intralipid therefore has an effect in increasing the rate and quantity of thrombin generation but the effect is slight. TABLE V TEST FOR ANTIHEPARIN EFFECT OF INTRALIPID BY COMPARISON WITH PLATELETS Buffeer Plasma Intralipid 181 sec. 153 sec. Platelet rich plasma > 10 min. > 10 min. Platelet poor plasma The four combinations of platelet-rich plasma or platelet-poor plasma, vs Intralipid or buffer, were incubated with heparin 3 units/ml. After 8 hr. thrombin and fibrinogen were added and the above clotting times recorded. It is interesting to pursue the action of Intralipid in replacing the action of platelets in the thrombin generation test. Blood platelets are known to have several actions, one of which is reversal of the action of heparin. The effect of platelets and Intralipid are compared in this function. The plan of the experiment is shown in Table V. The experiment involves incubation of platelet-rich and platelet-poor plasma with heparin, with and without Intralipid. After incubation, thrombin is added and from this mixture samples are added to fibrinogen solution. It is seen that those 200 THE EFFECT OF PLATELETS AND FAT EMULSION ON CLOT RETRACTION 150 PERCENTAGE CHANGE 100 IN CLOT VOLUME 20 40 6b 80 100 PERCENTAGE PLATELET RICH PLASMA PERCENTAGE CONCENTRATION OF Fig. 5. The upper line represents the effect of increasing concentrations of fat emulsion, the lower line the effect of increasing the percentage of platelet-rich plasma. 333 D. J. REID tubes which contained platelet-rich plasma have clotted whereas those which contain platelet-poor plasma, whether they contain Intralipid or not, have failed to clot. Hence fat emulsion does not replace the action of platelets in their capacity to reverse the action of heparin. Platelets also have an action in the process of clot retraction. Clot retraction was therefore measured using the wire spiral method measuring the volume of residual serum in a clotting mixture as a measure of the degree of retraction of the clot. It is seen that as the concentration of platelets increased in the mixture the clot volume decreases. As the concentration of fat emulsion increases clot retraction does not increase but initially it decreases (Fig. 5). Therefore the fat does not replace the action of blood platelets in the process of clot retraction. DILUTE PLASMA CLOT LYSIS TEST WITH VARYING cONaNTRATIONS OF FAT ENJLSION CONC.FAT MGC;% I. 0 soo 200 2. 3. 1000 5. 2000 S. 4. CwT 4. LYSIS TIME 3s. 3s HUS2. 1/60 Vho '/o 1/120 DILUTIONS OF PLASMA Fig. 6. The action of Intralipid on the process of fibrinolysis was investigated (Fig. 6). 9 ml. venous blood was citrated with 1 ml. 3.2 per cent sodium citrate and immediately cooled at 4° C. At 40 C. the blood specimen was centrifuged 2,500 r.p.m. for 10 min. At 25 min. after venepuncture dilutions of the plasma 1/60, 1/80, 1/100 and 1/120 were made up. The dilutions were made with tris buffer alone or with the buffer containing fat emulsion in varying concentrations 200, 500, 1,000, 2,000 mg. per cent. 4 ml. samples of dilute plasma were incubated at 370 C. in a water bath following the addition of 0.2 ml. thrombin. The time taken for complete lysis of the clot to occur was estimated and Figure 6 shows the results obtained. It is seen that increasing concentrations of fat emulsion cause 334 METABOLIC AND BLOOD COAGULATION CHANGES TABLE VI MEASUREMENT ON ARTERIAL BLOOD A.L. d 45 CA. Colon J.H. d 45 Perf. G.U. 3.0 gm./Kg. B. W. 70 miii. 3.0 gm./Kg. B. W. 70 min. Art. Art. Time Art. Art. Time pH pH pCO2 min. pCO2 min. 0 36.4 7.47 0 32.5 7.435 70 35.4 31.5 7.44 70 7.425 110 7.43 35.0 7.428 30.0 100 165 7.438 34.5 140 7.433 30.2 7.44 34.0 30.0 225 7.420 190 285 7.43 34.2 20.2 7.420 220 7.44 31.0 405 7.405 30.0 260 30.1 300 7.420 Changes in arterial pH and pCO2 in two patients receiving intralipid 3.0 gm./Kg. body weight over 70 minutes. (Time is expressed in minutes after the start of the infusion.) only a slight change in clot lysis time in the direction of increased lysis and would appear therefore not significantly to affect the process of fibrinolysis. In the course of this work and other work not presented over 150 infusions of Intralipid have been given and no case of venous thrombosis has been encountered. Prolonged protein/fat feeding on a carbohydrate-deficient diet has been shown to produce ketonuria. It is important to know whether an intravenous fat infusion alters the pH or pCO2 of the blood during infusion. TABLE VII pCO2 Standard bicarbonate 35 22.0 Baseline 7.390 1 35 7.385 21.7 2 7.389 35 21.6 38 3 7.390 22.7 40 4 7.380 22.7 39 5 7.370 22.0 39 8 7.379 22.5 9 7.398 35 22.3 10 38 22.2 7.382 36 22.2 Baseline 7.395 1 38 7.389 22.7 37 2 7.381 22.0 38 3 7.388 22.6 4 7.385 39 22.7 36 5 7.395 22.4 8 7.410 40 24.5 9 7.389 38 22.6 10 34 7.410 22.0 Baseline 7.455 35.0 25.0 1 7.455 33.5 24.9 2 7.470 33.0 25.6 3 7.455 35.0 25.5 4 25.3 7.455 35.0 5 7.455 36.0 25.8 6 7.455 34.5 25.2 *Changes in pH, pCO2 and standard bicarbonate in three patients receiving 500 ml. 20 per cent Intralipid daily. The infusions were started each day at 9 a.m. and given daily at a constant rate. Estimations were carried out daily at noon. Day pH 335 D. J. REID Repeated tests on the urine of patients receiving this emulsion have failed to show any evidence of ketonuria. In cases of metabolic acidosis, as occur in uraemia, fat emulsions play an important supporting role in management. If, however, the emulsion were to produce further acidosis, its value would be reduced. An investigation was therefore undertaken to measure changes in pH and pCO2 during intravenous fat infusions using Intralipid. The measurements made using arterial blood are shown in two patients each receiving 3.0 Gm./Kg. B.W. of fat over 70 min. (Table VI). It is seen that there is virtually no change in pH or pCO2 during or after the infusions. Three further patients were studied daily at the end of the intravenous infusion over a period of 10 days. It is again seen that no real change in pH or pCO2 occur at any time throughout the 10-day periods (Table VII). CONCLUSIONS In summary, therefore, the following conclusions are drawn. 1. Intralipid exerts a nitrogen-sparing action on those patients who are in negative nitrogen balance. When patients in positive nitrogen balance receive intravenous fat, no significant change in balance occurs. 2. Isocaloric replacement of intravenous calories with extra ora calories produce the same sparing effect on nitrogen balance. 3. No significant change occurs in faecal fat excretion during the intravenous administration of fat. 4. Intralipid causes a shift in the Thrombin Generation Test in the direction of increased thrombin generation when fat is added to blood, in vivo and in vitro. The coagulant action of Intralipid cannot be detected by the one-stage coagulation test, the Partial Thromboplastin Time. The coagulant action is therefore slight. 5. Intralipid mimics the action of blood platelets in the Thrombin Generation test. It does not replace the action of platelets in the clot retraction test. It is suggested that the changes demonstrated in the Thrombin Generation test are due to phosphatidyl ethanolamine present in the emulsifying agent of the emulsion. 6. No inhibitory action of Intralipid was noted in the process of fibrinolysis using the Dilute Plasma Clot Lysis test. 7. Intralipid acts as a stimulus to metabolism causing increased oxygen consumption, a fall in respiratory quotient and increased metabolic rate. Apart from the nutritional value of the fat emulsion the increase in metabolic rate would produce a sense of well-being in debilitated patients. 8. Ketosis has not been detected during Intralipid infusions and no evidence of acidosis has been demonstrated. These observations add to the evidence that this form of intravenous fat is metabolized. It would appear to have a favourable effect on patients in negative nitrogen balance. The emulsion exerts a mild coagulant action but this is so slight that it can be ignored. 336 METABOLIC AND BLOOD COAGULATION CHANGES ACKNOWLEDGEMENTS I am grateful to Miss Gillian Wooding, Sister-in-Charge of the Metabolic Unit, St. Thomas's Hospital, who cared for the patients undergoing metabolic study; to Professor F. T. G. Prunty, Dr. T. Pilkington, Dr. G. I. C. Ingram, Dr. W. J. Griffiths and Dr. C. D. Marsden I am grateful for much help. REFERENCES AMRIS, C. J., BROCKNER, J., and VAGN, L. (1964) Acta chir. 5cand., Suppl. 325, 70. ISAKSSON, B., and SJOGREN, B. (1964) Excerpta med. 11, 1041. LANGDELL, R. D., WAGNER, R. H., and BRINKHOUS, K. M. (1953) J. Lab. clin. Med. 41, 637. MACFARLANE, R. G. (1939) Lancet, 1, 1199. and BIGGS, R. (1953) J. clin. Path. 6, 3. MATCHETT, M. D., and INGRAM, G. I. C. (1965) J. clin. Path. 18, 465. MITCHELL, H. H., and HAMILTON, J. S. (1949) J. biol. Chem. 178, 345. MITCHELL, J. R. A., and BRIERS S. M. (1959) Lancet, 2, 435. 3In e&moriam CECILIA FLORA WEBB-JOHNSON, Baroness, Dame of the Order of St. John of Jerusalem Member of the Court of Patrons LADY WEBB-JOHNSON died suddenly on 15th March during a holiday in Teneriffe. She was the only child of Douglas Gordon MacRae and his Lady Webb-Johnson wife, Caroline Cecilia. In 1911 she married Alfred Webb-Johnson soon after his appointment to the surgical staff of the Middlesex Hospital and 337
© Copyright 2026