C-Reactive Protein Induces Human Peripheral
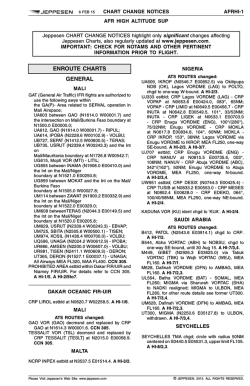
From www.bloodjournal.org by guest on February 6, 2015. For personal use only. C-Reactive Protein Induces Human Peripheral Blood Monocytes to Synthesize Tissue Factor By Jaroslav Cermak, Nigel S . Key, Ronald R. Bach, Jozsef Balla, Harry S . Jacob, and Gregory M. Vercellotti The acute inflammatory response is frequently accompanied by serious thrombotic events. We show that C-reactive protein (CRP), an acute-phase reactant that markedly increases its serum concentration in response t o inflammatory stimuli, induced monocytes to express tissue factor (TF), a potent procoagulant. Purified human CRP in concentrations commonly achieved in vivo during inflammation (10 to 100 pg/mL) induced a 75-fold increase in TF procoagulant activity (PCA) of human peripheral blood mononuclear cells (PBM), with a parallel increase in TF antigen levels. CRP-induced PCA was completely blocked by a monoclonal antibody against human TF but not by irrelevant murine lgG. Dot blot analysis showed a significant increase of TF mRNA after 4 hours of incubation with CRP. followed by a peak of PCA within 6 and 8 hours. Actinomycin D and cycloheximide blocked CRP-stimulated PCA. T HE INFLAMMATORY response includes phagocyte margination and migration, chemoattractant generation, cytokine formation, and production of a heterogenous group of proteins collectively called acute-phase reactants. The most characteristic human acute-phase protein is Creactive protein (CRP).’ CRP, consisting of five identical, noncovalently linked subunits of 23,000 molecular weight,2 is synthesized in the liver. Its serum concentration of less than 1 jtg/mL can increase during the first 24 to 48 hours of inflammation or tissue necrosis by several hundred-fold, a response shown primarily to be due to interleukin-6 (IL-6) ti mu la ti on.^.^ CRP is thought to amplify the host defense system by potentiating its recognition capacities, as exemplified by its activation of the complement cascade and its stimulation of various effector phagocytic cell^.^-^ The linkage between inflammation and coagulation may well involve tissue factor (TF). T F is a membrane-bound glycoprotein that initiates the extrinsic pathway of coagulation.’ The TF-factor VIIa (TF-FVIIa) complex activates FX directly or indirectly via FIX activation, leading ultimately to thrombin generation.’ “Resting” endothelial cells and monocytes/macrophages express very low levels of procoagulant activity (PCA). However, in both these cell types, an induction of T F expression with associated increased PCA has been shown with exposure to various agents, including inflammatory mediators such as endotoxin (LPS) or cyto- kine^."*^ That CRP might also play a role in upregulating monocyte PCA, as suggested by Whisler et al,23is an attractive possibility, because CRP is known to modulate other monoBecause cyte function^^^-^^ through a specific re~eptor.*’~~’ CRP accumulates at sites of inflammation or tissue damage, we questioned whether CRP might promote localized coagulation by stimulating monocytes to produce the specific procoagulant, TF. In the following studies, we used highly punfied human CRP to assay its effects on peripheral blood monocyte and endothelial cell PCA and to discern mechanisms by which CRP promotes TF expression in these cells. Blood, VOI 82, NO 2 (July 15). 1993: pp 513-520 suggesting that de novo TF protein synthesis was required. Endotoxin (LPS) contamination of CRP was excluded as the mediator of TF synthesis because: (1) CRP was Limulus assay negative; (2) induction of TF PCA by CRP was not blocked by Polymyxin B, in contrast t o LPSinduced PCA; (3)antihuman CRP IgG inhibited CRP-induced PCA, but not LPS-inducedPCA; (4)CRP was able t o stimulate TF production in LPS-pretreated PBM refractory t o additional LPS stimulation; and, (5) unlike LPS. CRP was incapable of inducing TF in human umbilical vein endothelial cells. We suggest that CRP-mediated TF production in monocytes may contribute to the development of disseminated intravascular coagulation and thrombosis in inflammatory states. 0 1993 by The American Society of Hematology. MATERIALS AND METHODS Reagents Highly purified (>90%) human CRP was obtained from Sigma CO(St Louis, MO) (catalogueno. C6 177), as well as endotoxin/lipopolysaccharide (LPS) (catalogue no. L3 129), lyophilized IgG fraction of rabbit serum against human CRP (catalogue no. C3257), and TRIS [tris(hydroxymethyl)aminomethane]. Hanks’ Balanced Salt Solution (HBSS), HEPES buffer solution, and all cell culture media including RPMI 1640 were purchased from GIBCO (Grand Island, NY). Heparin sodium was from LyphoMed (Melrose Park, IL); Polymyxin Band recombinant human IL-lp (rIL- 1) were from Upjohn CO(Kalamazoo, MI); CS-depleted serum was from Quidel CO (San Diego, CA); formaldehyde was from Fisher Scientific (Pittsburgh, PA); and cycloheximide was from NBCo (Cleveland, OH). Radiolabeled compounds and nylon membranes were obtained from Amersham (Arlington Heights, IL). Murine monoclonal antibody (MoAb) against human TF (HTF1), polyclonal antibody against human TF (anti-HTF pAb), human From the Department ofMedicine, University ofMinnesota, Minneapolis; and the Veterans Administration Medical Center, Minneapolis, MN. Submitted November 30, 1992; accepted March 17, 1993. Supported in part by grantsf o m the National Institutes of Health (HL 33793), the Graduate School of the University of Minnesota, and the Department of Veterans’Affairs. J.C. was supported by the Charles Proshek Fellowship from the Minnesota Medical Foundation. Address reprint requests to Gregory M. Vercellotti, MD, University of Minnesota, Department of Medicine/Division of Hematology, Box 480 UMHC, Harvard St at E River Rd, Minneapolis, MN 55455. The publication costs of this article were defayed in part by page charge payment. This article must therefore he hereby marked “advertisement” in accordance with I 8 U.S.C. section I734 solely to indicate this fact. 0 I993 by The American Society oJHematology. 0006-4971/93/8202-0004$’3.00/0 513 From www.bloodjournal.org by guest on February 6, 2015. For personal use only. 514 CERMAK ET AL FVIIa and FX, human TF standard, and bovine brain cephalin were prepared as previously de~cribed?~-~’ All other reagents were obtained from Sigma CO, unless otherwise specified. All reagents, including CRP, were tested for endotoxin contamination by the Limulus assay (E-Toxate; Sigma CO)and were negative at levels from 0. I to 0.2 EU/mL (10 to 20 pg/mL). Peripheral Blood Mononuclear Cells (PBM) and Peripheral Blood Monocyte Isolation Minimally heparinized (2 U/mL) blood from fasting healthy donors (after obtaining their informed consent according to the guidelines of the Committee on the Use of Human Subjects in Research, University of Minnesota) was layered over Histopaque- 1077 and centrifuged (500g)at 24°C for 30 minutes. The PBM collected from the plasma/Histopaque interface were washed three times with phosphate-buffered saline (PBS) and finally resuspended in RPMI 1640 1% fetal calf serum (FCS) at a concentration of 1 X IO6 cells/mL. The PBM contained an average of 80%lymphocytes and 20% monocytes as assessed by light microscopy and nonspecific esterase staining. Contamination by polymorphonuclear leukocytes and platelets was less than 1%. PBM at I X IO6 cells/mL in RPMI 1640 1% FCS were incubated with various reagents at 37°C in 5% CO, for the appropriate times. After incubation, cells were washed once with fibrometry buffer (0.16 mol/L NaCl 25 mmol/L HEPES buffer, pH 7.4). The viability ofthe cells as assayed by Trypan blue exclusion was greater than 95% after 6 hours of incubation and 92% after 18 hours of incubation. To prepare a relatively enriched population of peripheral blood monocytes, PBM at 2 X IO6 cells/mL were plated onto plastic tissue culture wells with RPMI 1640 + 1% FCS. After 2 hours of incubation, nonadherent cells were removed by washing five times with medium. The adherent cells (approximately 75% to 80% monocytes and 20% to 25% lymphocytes) were incubated with various reagents under the same conditions as PBM. + + + Human Umbilical Vein Endothelial Cell (HUVEC) Cultures HUVEC were isolated and grown as previously described3’ and used from passages 1 through 3 after reaching confluence. HUVEC grown in 2-cm2 tissue culture wells (approximately 200,000 cells/ well) were incubated with various reagents in the same manner as PBM; after the incubation, the cells were washed once with fibrometry buffer. TF Assays One-stage clotting assay. PBM cell pellet was resuspended in 0.5 mL fibrometry buffer, frozen at -7O”C, and thawed at 37°C three times and sonicated. Peripheral blood monocytes and HUVEC were treated the same way. Cells were scraped from the bottom of tissue culture wells, frozen, and thawed three times before sonication. The clotting assay” consisted of 0.1 mL of cell sample and 0. I mL of citrated normal human platelet-poor plasma. The reaction was initiated in a fibrometer cup (Fisher Scientific CO)by the addition of 0.1 mL 25 mmol/L CaCI,. Results were expressed in arbitrary units per milliliter (U/mL) of T F by comparison of clotting times with a standard curve obtained using a purified human TF standard as previously de~cribed.’~ One unit of TF PCA equals 1 pg of the TF standard. For HUVEC, the results were expressed in U/mg of cell protein assessed by BCA protein assay (Pierce, Rockford, IL). Two-stage clotting assay. PCA was measured on Coag-a-mate XM (Organon Teknika, Durham, NC). In stage 1 of the assay, 20 pL of sample was incubated with 10 pL of 30 nmol/L human FVIIa and 10 pL of I .5 pmol/L human FX at 37°C for at least 3 minutes. The reaction was initiated by adding 20 pL of 25 mmol/L CaCI,, and the sample was incubated for another 5 minutes. Stage 2 ofthe assay was started by the simultaneous addition of 100 pL substrate plasma (90 pL normal citrated bovine plasma plus 10 pL bovine brain cephalin [6 mg/mL] in TRIS-buffered saline) and 100 pL 25 mmol/L CaCI,. Clotting time was recorded, and TFlevel was calculated from a standard curve obtained using a human brain TF standard.34 TF antigen enzyme-linked immunosorbent assay (ELISA). T F antigen ELISA was performed as previously described.34 Briefly, 96-well microtiter plates were coated with 100 pL per well of IO pg/mL HTF-I murine MoAb in a bicarbonate buffer (15 mmol/L Na’CO,, 35 mmol/L NaHCO,, pH 9.6) and incubated overnight at 4°C. Wells were then filled with TBS (0.1 mol/L NaC1,0.05 mol/L Tris, pH 7.5) containing 1% bovine serum albumin (BSA) to block nonspecific sites and incubated again at 4°C for at least 4 hours. One hundred microliters of sample for assay or TF standard diluted in TBS containing 0.1% BSA, 0.1% Triton X-100, and 5 mmol/L EDTA were added to triplicate wells. After an overnight incubation, the plates were extensively washed, 100 pL of anti-HTF polyclonal antibody at a final concentration of 0.2 pg/mL diluted in TBS + I % BSA was added, and samples were incubated for 2 hours at room temperature. After another wash, the samples were incubated with 100 pg goat antirabbit horseradish peroxidase-conjugated IgG (GAR-HRP; Bio-Rad, Richmond, CA) diluted 1:2,000 in TBS + 1% BSA. After a further wash cycle, a chromogenic detection system was added for 30 minutes. The reaction was stopped with the addition of 25% H2S04, and the sample absorbance was read at 490 nm on a Dynatech MR 600 microplate reader (Dynatech Laboratories Inc, Chantilly, VA). TF antigen level was calculated from a standard curve obtained with diluted human T F standard in the range of 0 to 1,000 pg/mL. TF mRNA analysis. T F mRNA content in PBM was analyzed after treatment with CRP, LPS, serum, or RPMI 1640 1% FCS alone. PBM cellular mRNA was isolated by the RNAzol method (Tel-TEST, Inc, Friendswood, TX). Aliquots (4 pg) of total RNA were dissolved in IO pL of H,O and mixed with 20 pL of 100% formamide, 7 pL of 37% formaldehyde, and 2 pL of 20X SSC (3 mol/L NaCl + 0.3 mol/L sodium citrate), applied to slots on a microsample filtration manifold (Minifold I; Schleicher and Schuell, Inc, Keene, NH), and transferred onto nitrocellulose memb r a n e ~using ~ ~ UV cross-linking. The membranes were hybridized at 42°C with a nick-translated ”P-labeled cDNA probe for human TF.36Autoradiographs were obtained and quantitated by computer-assisted videodensitometry.” + Statistical Methods Statistical analysis was performed using the Student’s t-test. All results are expressed as mean l?r I SD. RESULTS Induction of TF Expression on PBM and on Peripheral Blood Monocytes A significant increase in TF PCA of disrupted PBM was found after 6 hours of incubation with either CRP (100 pg/mL) or LPS (10 pg/mL) ( P < .0001 for one-stage clotting assay and P < .O 1 for two-stage clotting assay and TF antigen [Table 11). A difference between CRP- and LPS-induced TF expression was also significant ( P < .O 1 for all 3 From www.bloodjournal.org by guest on February 6, 2015. For personal use only. CRP INDUCES TISSUE FACTOR 515 Table 1. Induction of TF in PBM by Different Stimuli Two-Stage Clotting Assay One-Stage Clotting Assay (U/W Reagent (UlW Control 13.1k2.4 LPS (10pg/mL) 415.0t 46.4 CRP ( 1 0 0 ~ ~ n / m L ) 1,044.8rt 52.8 TF Antigen ELSA (pg/mL) 8.5 k 0.8 20.3 k 3.5 299.6f 13.0 373.3t 14.2 694.5f 28.9 726.1 t 17.5 _ _ _ ~ ~ ~ PBM at a concentration of 106/mL were incubated for 6 hours with RPMl 1640 + 1 % FCS (control), LPS (10pg/mL), or CRP (1 00 pg/mL), both in RPMl 1640 1 % FCS. The TF PCA was measured by one- or two-stage clotting assay and TF antigen by ELISA. Results represent the mean f 1 SD from five experiments performed in duplicates + assays). In the two-stage clotting assay, PCA was undetectable when FVIIa was omitted from the assay (data not shown). This result shows that the PCA is indeed TF-mediated. Most of the TF activity induced by CRP in mononuclear cells was encrypted, ie, CRP-treated (100 pg/mL) mononuclear cells added intact to the one-stage clotting assay had 17%of the procoagulant activity (150 U/mL) compared with sonicated, disrupted CRP-treated mononuclear cells (880 U/mL).' Similarly, under the same conditions, a relatively enriched population of peripheral blood monocytes exhibited a significant increase of TF PCA from a control value of 4.2 f 1.1 U/mL to 714.9 k 70.7 U/mL with LPS ( I O pg/ mL) and 1,495.8 f 267.9 U/mL with CRP (100 pg/mL) (measured by the one-stage clotting assay). To characterize CRP-induced PCA on PBM, the samples previously treated with CRP for 6 hours were incubated with a murine blocking MoAb (HTF-1) for I hour at room temperature. This incubation decreased TF activity in the one-stage clotting assay from 1,044.8 U/mL to 48.8 U/mL (P < .OOOl)(Fig I). Incubation with an irrelevant murine p 1200 1 -E . 2. 1000 - 800 - p c 0.0001 0.0001 1200 I 600 n 1I 7 -E z 3 - Ns 600- n U. I- U. I- I C IgG in the same concentration did not significantly affect CRP-induced PCA. This further substantiates that the PCA induced by CRP is TF. To obtain evidence that CRP is the factor inducing TF PCA, CRP (100 pg/mL) was pretreated with an IgG fraction of rabbit serum against human CRP (200 pg/mL) for 30 minutes at 37°C. Pretreatment of CRP significantly decreased CRP-induced TF expression by PBM after 6 hours of incubation (P < .OOOl). In contrast, antiserum against human CRP had no effect on LPS induced TF expression (Fig 2). Under normal circumstances, the serum CRP concentration is less than 1 pg/mL, but can increase up to 1,000-fold during acute infections or tissue n e c r o s i ~ . 'Therefore, ~,~~ we examined a dose response of PBM exposed to varying CRP concentrations for 6 hours; as shown in Fig 3, a concentration of CRP as low as 5 pg/mL significantly induces TF PCA (P < .05), with a further increase in response up to 100 pg/mL. Levels of CRP 5 1 pg/mL did not induce TF PCA (data not shown). The time course of TF PCA induced in PBM by CRP differed from that noted with LPS induction. As seen in Fig 4, a peak of CRP-stimulated PCA occurred between 6 and 8 hours and remained elevated even after 18 hours. In contrast, the LPS effect peaked between 4 and 8 hours and tailed off at 18 hours. Because CRP is able to induce complement activat i ~ n , ' *we ~ ,tested ~ whether CRP-induced TF PCA in serum was dependent on complement. Using RPMI, C5-depleted human serum, or heat-inactivated human serum (56°C for 30 minutes) as the diluent, we observed only a slight decrease in the induction of TF PCA by CRP. This result suggests that complement activation does not substantially 400 - 200 RPMl O+ CRP RPMl CRP/HTF-1 CRP/IgG Fig 1. Effect of a blocking murine MoAb (HTF-1) on CRP-induced PCA in PBM. After 6 hours of incubation with CRP (100 pg/mL) in R P M l l 6 4 0 1% FCS or R P M l l 6 4 0 1% FCS alone, PBM (106/mL) cells were incubated for 1 hour at room temperature either with HTF-1 (200 pg/mL) (CRP/HTF-1) or with irrelevant murine IgG (200 pg/mL) (CRP/IgG). Results represent the mean 2 1 SD of three experiments in duplicates measured by the one-stage clotting assay. + + UP CRPl CRP Ab LPSl LPS CRP Ab Fig 2. Effect of antihuman CRP antiserum on CRP- and LPS-in1% FCS) duced TF PCA in PBM. PBM (106/mL in RPMl 1 6 4 0 were incubated for 6 hours either with CRP (100 pg/mL) or LPS (10 pg/mL), respectively, with CRP or LPS in the same concentration preincubated with 200 pg/mLof purified rabbit antihuman CRP lgG for 30 minutes at 37°C ([CRP/CRPAb], [LPS/CRPAb]). Results rep1 SD of three experiments in duplicates mearesent the mean sured by the one-stage clotting assay. + * From www.bloodjournal.org by guest on February 6, 2015. For personal use only. 516 CERMAK ET AL 1500 I D < 0.0001 T- 100 25 50 10 5 CRPI serum RPMl CRP concentration (pglml) Fig 3. Effect of varying CRP concentrations (diluted in HBSS) on PBM TF PCA after 6 hours of incubation. Results represent average 2 1 SD of three experiments in duplicates on PBM (lOg/mL) in RPMl 1640 1% FCS as measured by the one-stage clotting assay. + contribute to the effect of CRP on PBM T F synthesis (Fig 5). Evidence That CRP and LPS Represent Two Different Stimuli As mentioned above, rabbit antiserum against CRP decreased CRP-induced T F expression, but did not affect LPS-provoked PCA. To further assure that CRP-induced PCA is distinct from that mediated by LPS, we coincubated samples with Polymyxin B (10 pg/mL) for 6 hours. Polymyxin B, which binds and inactivates gram-negative endo- 1200 1 i I 600 I& I- 0 2 4 6 8 1.0 1.4 1.2 16 1.8 hours Fig 4. Effect of different incubation times on CRP (100 pg/mL) (0). LPS (10 pg/mL) (01, and RPMl 1640 1% FCS (0)alone induced TF PCA in PBM (10*/mL in RPMl 1640 1%FCS) measured by the one-stage clotting assay. A representativeexperiment is shown. + + CRPl RPMl CRPl Hlserum CRPI CWepl. serum serum Fig 5. Effect of serum complement on CRP-induced TC PCA in PBM. CRP (100 pg/mL) was added to 10%human serum (CRP/ serum), RPMl 1640 (CRP/RPMI), 10% heat-inactivated serum (CRP/Hlserum), or 10%C5-depleted serum (CRP/C5depl,serum) and incubated with PBM (1OB/mL)for 6 hours. Results represent the mean f 1 SD of three experiments in duplicates measured by the one-stage clotting assay. toxin (LPS),39did not significantly alter CRP-induced (10 pg/mL) T F activity (999.2 f 74.5 U/mL). In contrast, as expected, LPS-induced (10 pg/mL) T F PCA (415.9 f 46.4 U/mL) decreased to less than 30%of initial values (P< .05) in the presence of Polymyxin B ( 1 37.4 f 13 U/mL). Additional evidence was garnered by the fact that the CRP preparation used in these studies did not contain significant amounts of endotoxin, as measured in the Limulus assay. We also tested whether LPS-prestimulated PBM retained the capacity to respond to CRP despite being desensitized to further LPS s t i m u l a t i ~ n . ~Figure ~ , ~ ' 6 shows the effect of repeated stimulation on PBM pretreated with LPS ( I O pg/ mL) with regard to T F synthesis. LPS-induced T F antigen was elevated after 6 hours of incubation and became undetectable after 24 hours. At that time, LPS added in the same concentration was not able to further increase TF antigen. In contrast, CRP (100 pg/mL) stimulated T F antigen in LPS-pretreated PBM, validating that LPS and CRP induced T F via distinct pathways. Of interest, the amount of T F induced by CRP in LPS-presensitized cells is blunted when compared with that of naive mononuclear cells. This resembles Busso et al's4 observation that LPS or tumor necrosis factor-a (TNF-a) restimulation of IL- 1(3-pretreated HUVEC results in less T F than control HUVEC. Regulation of CRP-Induced TF PCA in PBM Dot blot analysis of T F mRNA harvested from PBM after 4 hours of incubation with CRP (100 pg/mL) showed induction ofTF mRNA, whose increment, as judged by videodensitometry, was approximately 16-fold over that seen within cells incubated with RPMI 1640 + 1% FCS and 1.5fold higher than after treatment with LPS (10 pg/mL) (Fig 7). From www.bloodjournal.org by guest on February 6, 2015. For personal use only. 517 CRP INDUCES TISSUE FACTOR DISCUSSION .y 0 . , . 4 TREATMENT: , 12 6 . , 18 v, ,LPS 24 Tlmo (hra) LPS CRP 10pg/ml 30 4 100pg1ml or LPS lOpg/ml Fig 6. Effect of repeated stimulation of PBM. PBM (106/mL in RPMl 1640 1% FCS) were incubated for 2 4 hours with LPS (10 pg/mL). TF antigen expression was measured by ELISA at 0 , 6 , and 2 4 hours. After 2 4 hours, the cells were washed, resuspended in RPMl 1640 2 1 % FCS, CRP (100 rg/mL) or LPS (10 rg/mL) was added, and, after 6 hours of additional incubation, TF antigen was recorded. Results of a representative experiment are shown. Similar results were obtained for these groups when TF PCA was measured by the one-stage clotting assay (data not shown). + To examine the regulatory mechanisms, we also coincubated PBM with cycloheximide and actinomycin D. Both cycloheximide and actinomycin D, at concentrations of IO pg/mL, completely blocked CRP (100 pg/mL) induction of T F PCA (one-stage clotting assay) in PBM ( 1 3.4 f 3.2 and 12.2 f 4.0 U/mL, respectively) compared with CRP alone (1,044.8 f 52.8 U/mL), suggesting that de novo protein synthesis was necessary for T F production. Induction TF Expression in H U VEC Because both monocytes/macrophages and endothelial cells are capable of synthesizing T F in response to inflammatory mediators such as LPS or cytokines, we tested the ability of CRP to induce TF PCA in endothelial cells. Both LPS ( 1 0 pg/mL) and rIL- 1 p (0.I pg/mL) induced TF expression on HUVEC after 6 hours of incubation (Pe .01 when compared with RPMI 1640 + 1% FCS). In contrast, CRP (100 pg/mL) failed to increase HUVEC TF expression (Fig 8). Fig 7. Dot blot analysis of TF mRNA. PBM (in R P M l l 6 4 0 1% FCS) were incubated for 4 hours with CRP (100 rg/mL), LPS (10 pg/mL), 10% human serum, or RPMl 1 6 4 0 1% FCS alone. mRNA was isolated from 6 X 10' cells per each group. Intensity of hybridization signals was measured by videodensitometry and expressed as the relative increase in comparison with RPMl 1640-treated PBM. In the genesis of thrombosis, Virchow first stressed the importance of blood flow, the blood's propensity to clot. and the integrity ofthe vessel wall, the last ofwhich could be affected by inflammation. In the course of inflammation, TF, an initiator of the extrinsic coagulation pathway. may be expressed on cell surfaces that are not thrombogenic under normal circumstances, such as monocytes and endothelial cells. Various inflammatory stimuli (eg, LPS. TNF, and IL-1) have previously been shown to increase TF expression on endothelial cell^,'^-^^ whereas in human monocytes/macrophages. endotoxin?" activated complement." aggregated IgG,13and TNFI4all have been reported to generate procoagulant activity, presumably by inducing T F neosynthesis.' Moreover, an increase in circulating monocyte PCA in various inflammatory diseases (including Crohn's disease, meningococcal sepsis, lupus erythrematosus, and rheumatic diseases) has been previously Rivers et a146 showed an increase in the expression of TF in monocytes from infants with severe infection. We have recently obtained sera containing high levels of CRP ( 1 1.6 mg/dL) from a patient with fevers, idiopathic retroperitoneal fibrosis, and deep venous thrombosis that induced T F in normal monocytes. However, our anti-CRP antibody failed to inhibit TF induction by this patient's sera. Defining a singular effect of CRP on mononuclear cell tissue factor induction in sick patients' sera may prove difficult because of concurrent serum elevations of IL-I, TNF, immune complexes, or other factors that themselves can activate TF synthesis. We are planning further TF studies with sera from ill patients who have high serum CRP levels to further delineate CRP's role. CRP was first reported by Tillet and Francis4' as a serum factor possessing the capacity to precipitate a carbohydrate derived from pneumococcal fraction C. CRP not only binds this pneumococcal polysaccharide but also binds calcium. phosphate monoesters. phosphoryl choline, galactose polymers. and p o l y c a t i o n ~CRP ~ * ~ is also able to bind polymorphonuclear leukocytes and to modulate neutrophil funct i o n ~and ~ ~has . ~been ~ found to affect intracellular calcium mobilization, superoxide production, and tumoricidal activity of peripheral monocytes/macrophages2e26via binding to a specific surface receptor.28Ballou et aI5' recently showed that CRP can induce TNF-(U,[email protected] IL-6 in monocytes + + RE AT1 U E INTENS ITV- 16x 10 x lx CRP LPS RPMI 1.5~ Serum From www.bloodjournal.org by guest on February 6, 2015. For personal use only. CERMAK ET AL 518 -.C d e n 200- p < 0.001 U RPMl LPS rlL-1 Fig 8. Effect of various stimuli on TF PCA in HUVEC. Confluent monolayers of HUVEC grown in 2-cmZ wells were incubated for 6 hours with RPMl 1640 1% FCS, CRP (100 pg/mL), LPS (IO pg/ mL), or rlL-I (0.1 pg/mL) (all reagents diluted in RPMl 1640 f 1% FCS). The results represent the mean 2 1 SD from three experiments performed in duplicate and measured by the one-stage clotting assay. + in a similar dose and time course as we have shown for TF. Whether these cytokines play a role in the signal transduction for T F synthesis by CRP is now under investigation in our laboratory. Although induction of monocyte T F PCA in the course of inflammation has previously been ascribed to agents such as LPS, cytokines, or activated complement, the current study shows that CRP may be equally important. The maximal induced increment of TF PCA in PBM was greater than 75-fold over that of the control as measured by one- and two-stage assay and corresponded with a parallel increase in T F antigen. Likewise, Whisler et alz3previously described increased PCA in PBM after coincubation of LPS or immune complexes with CRP and noted that CRP alone also induced some PCA. Our experiments confirm these findings and show that the procoagulant activity reflects production of authentic T F because: ( I ) the activity is inhibited by a blocking MoAb to T F and (2) the procoagulant activity required FVIIa. However, we emphasize that because CRP may increase up to 1,000-fold within 6 to 24 hours in response to infections or tissue destruction, CRP concentrations of 100 fig/mL, used in our experiments, are commonly achieved during the course of an infectious episode. 1,3,38 Monocytes are considered to be the only circulating leukocyte capable of TF synthesis’’; however, CD4+ T-helper lymphocytes may enhance the monocyte T F response to stimuli such as LPS by both direct cell-cell contact as well as via the production of stimulatory lymphokine^.'^,^^ Recently, a specific receptor for CRP has been described on monocytes but not on peripheral blood lymphocyte^.'^ We did not observe any significant differences in the results of experiments performed on freshly isolated peripheral blood mononuclear cells (containing approximately 20% to 25% monocytes) or relatively purified (70% to 80%)peripheral blood monocytes. However, our data do not exclude the possibility that T lymphocytes are critical in mediating the monocyte T F response to CRP. Although we showed a threefold increase of serum C5a concentration when serum was incubated with CRP (100 pg/mL) in a recent s t ~ d y , CRP-induced ’~ monocyte T F expression does not only require complement activation (Fig 5); however, our results do not exclude the possibility that activated complement components may add to the procoagulant effect of CRP. Tebo and Mortensen” described a specific CRP receptor distinct from the IgG receptor on human blood monocytes and the human monocytic cell line U937. Excess of phosphorylcholine was unable to inhibit CRP binding to monocytes; similarly, in our experiments, even a 100-fold molar excess of phosphorylcholine failed to inhibit CRP-induced monocyte PCA (data not shown). The same investigators also recently showed2’ that the CRP/CRP receptor complex was internalized into an endosomal compartment in which CRP was liberated and subsequently degraded. When U937 cells were exposed to CRP, a significant H 2 0 2production and tumoricidal activity were detected after 8 hours. We found that PBM TF mRNA significantly increases after 4 hours of incubation with CRP, which was followed by a peak of T F PCA at 6 to 8 hours. Such findings are comparable to those published by Gregory et a1” who showed induction of T F expression on isolated monocytes exposed to LPS within 4 hours and peak PCA at 6 hours. Similarly, in our studies, coincubation of CRP with both cycloheximide and actinomycin D completely block CRPinduced T F PCA, suggesting that de novo synthesis of T F protein is involved and that CRP induces monocyte T F expression, presumably by acting at the transcriptional level. We rigorously excluded LPS contamination as a possible artifact in these studies by showing (1) that all reagents (including CRP) were negative for significant levels of contaminating endotoxin as judged by the Limulus amoebocyte assay; (2) that Polymyxin B inhibited LPS-induced PCA and had no effect on CRP-mediated PCA; (3) that a neutralizing antibody against CRP had a selective blocking effect on CRP-induced PCA; (4) that PBM pretreated with LPS were able to increase T F in response to CRP despite desensitization to further LPS stimulation; and (5) that in cultured HUVEC, we observed a failure to respond to CRP but not LPS. Thus, we conclude from these data that CRP and LPS represent two distinct stimuli. It is evident that the vascular endothelium plays an important role in hemostasis and thrombosis, and that inflammatory agent-stimulated endothelium may affect the activation of the coagulation system. However, we were not able to show a significant increase of HUVEC T F expression after exposure to CRP, in contrast to other inflammatory mediators, including LPS, IL-1, and TNF, which induce PCA in both monocyte/macrophages and endothelial cells.9. IO.l4,20-22 we speculate that this intriguing difference might be explained by the absence or considerably reduced expression of the CRP receptor on cultured endothelial cells. From www.bloodjournal.org by guest on February 6, 2015. For personal use only. CRP INDUCES TISSUE FACTOR Our results suggest that increased monocyte TF expression during infection or tissue necrosis may be at least partially mediated by an increased CRP level. Thus, CRP-mediated monocyte PCA induction may play an important role in altered microcirculation in inflammatory and necrotic tissue as well as contribute to the development of disseminated intravascular coagulation in septic infections. The ability of CRP to reinduce PCA in LPS-stimulated monocytes in a phase in which they are refractory to further LPS stimulation may be an important tool for the maintenance of a high monocyte PCA during inflammation. We speculate that this enhanced TF production may better allow inflammatory cells to ward off bacteria by promoting fibrin formation locally. ACKNOWLEDGMENT We thank Dr Henry Gewurz (Rush Presbyterian St Luke’s Medical Center, Chicago, IL) for kind advice; Dong Tuong and Theresa Stella for technical assistance; and Linda Radtke for manuscript preparation. REFERENCES 1. Gewurz H: Biology of C-reactive protein and the acute phase response. Hosp Pract 6:67, 1982 2. Osmand AP, Friedenson B, Gewurz H, Painter RH, Hofmann T, Shelton E: Characterization of C-reactive protein and the complement subcomponent C 1t as homologous proteins displaying cyclic pentameric symmetry (pentraxins). Proc Natl Acad Sci USA 74:739, 1977 3. Pepys MB: C-reactive protein fifty years on. Lancet 1:653, 1981 4. Kilkpatrick JM, Volanakis JE: Molecular genetics, structure and function of C-reactive protein. Immunol Res 10:43, 1991 5. Kaplan MH, Volanakis JE: Interaction of C-reactive protein complexes with the complement system. I. Consumption of human complement associated with the reaction of C-reactiveprotein with pneumococcal C-polysaccharide and with the choline phosphatides, lecithin and sphingomyelin. J Immunol 112:2135, 1974 6. Volanakis JE, Kaplan MH: Interaction of C-reactive protein complexes with the complement system. 11. Consumption of Guinea pig complement by CRP complexes: Requirement for human Clq. J Immunol 113:9, 1974 7. Bach R R Initiation of coagulation by tissue factor. Crit Rev Biochem Mol Biol23:339, 1988 8. Osterud B, Rapaport SI: Activation of factor IX by the reaction product of tissue factor and factor VII: Additional pathway for initiating blood coagulation. Proc Natl Acad Sci USA 795260, 1977 9. Rivers RPA, Hathaway WE, Weston WL: The endotoxin-induced coagulant activity of human monocytes. Br J Haematol 20:311, 1975 10. Prydz H, Allison AC: Tissue thromboplastin activity of isolated human monocytes. Thromb Haemost 39582, 1978 1 1. Muhlfender TW, Niemetz J, Kreutzer D, Beebe D, Ward P, Rosenfeld SI: C5 chemotactic fragment induced leukocyte production of tissue factor activity. J Clin Invest 63:147, 1979 12. Prydz H, Lyberg T, Deteix P, Allison A C In vitro stimulation of tissue thromboplastin (factor 111) activity in human monocytes by immune complexes and lectins. Thromb Res 15:465, 1979 13. Rothenberger H, Zimmerman TS, Spielberg HL, Vaughan JH: Leukocyte procoagulant activity. Enhancement of production in vitro by IgG and antigen-antibody complexes. J Clin Invest 59549, 1977 519 14. Conkling PR, Greenberg CS, Weinberg J B Tumor necrosis factor induces tissue factor-like activity in human leukemia cell line U937 and peripheral monocytes. Blood 72:128, 1988 15. Levy CA, Schwartz BS, Curtiss LK, Edgington TS: Plasma lipoprotein induction and suppression of the generation of cellular procoagulant activity in vitro. Requirements for cellular collaboration. J Clin Invest 67:1614, 1981 16. Schwartz BS, Levy CA, Curtiss LK, Edgington TS: Plasma lipoprotein induction and suppression of the generation of cellular procoagulant activity in vitro. Two procoagulant activitiesare produced by peripheral blood mononuclear cells. J Clin Invest 67:1650, 1981 17. Lorenzet R, Niemetz J, Marcus AJ, Broekman MJ: Enhancement of mononuclear procoagulant activity by platelet 12-hydroxyeicosatetraenoicacid. J Clin Invest 78:418, 1986 18. Rambaldi A, Alessio G, Casali B, Passerini CG, Donati MD, Mantovani A, Semeraro N: Induction of monocyte-macrophage procoagulant activity by transformed cell lines. J Immunol 136:3848, 1986 19. Carlsen E, Stinessen MB, Prydz H: Differential effect of alpha-interferonon thromboplastin response in monocytesand endothelial cells. Clin Exp Immunol 70:47 1, 1987 20. Conway EM, Bach RR, Rosenberg RD, Konigsberg WH: Tumor necrosis factor enhances expression of tissue factor mRNA in endothelial cells. Thromb Res 53:231, 1989 2 I. Scarpati EM, Sadler JE: Regulation ofendothelial cell coagulant properties. Modulation of tissue factor, plasminogen activator inhibitors, and thrombomodulin by phorbol 12-myristate 13-acetate and tumor necrosis factor. J Biol Chem 26420705, 1989 22. Nawroth PP, Handley DA, Esmon CT, Stern DM: Interleukin 1 induces endothelial cell procoagulant while suppressing cell surface anticoagulant activity. Proc Natl Acad Sci USA 83:3460, 1986 23. Whisler RL, Proctor VK, Downs EC, Mortensen RF: Modulation of human monocyte chemotaxis and procoagulant activity by human C-reactive protein (CRP). Lymphokine Res 5:223, 1986 24. Zeller JM, Landay AL, Lint TF, Gewurz H: Enhancement of human peripheral blood monocyte respiratory burst activity by aggregated C-reactive protein. J Leukoc Biol40:769, 1986 25. Zahedi K, Mortensen R F Macrophage tumoricidal activity induced by human C-reactive protein. Cancer Res 465077, 1986 26. Foldes-Filep E, Filep JG, Sirois P: C-reactive protein inhibits intracellular calcium mobilization and superoxide production by guinea pig alveolar macrophage. J Leukoc Biol 5 I : 13, 1992 27. Tebo JM, Mortensen R F Characterization and isolation ofa C-reactive protein receptor from the human monocyte cell line U-937. J Immunol 144:231, 1990 28. Tebo JM, Mortensen RF: Internalization and degradation of receptor bound C-reactive protein by U-937 cells: Induction of H202production and tumoricidal activity. Biochim Biophys Acta 1095:210, 1991 29. Carson SD, Ross SE, Bach RR, Guha A: An inhibitory monoclonal antibody against human tissue factor. Blood 70490, 1987 30. Bach RR, Gentry G, Nemerson Y: Factor VI1 binding to tissue factor in reconstituted phospholipid vesicles: Induction of cooperativity by phosphatidylserine. Biochemistry 25:4007, 1986 3 I . Broze GJ, Majerus PW: Purification and characterization of human coagulation factor VII. J Biol Chem 250:1242, 1980 32. Miletich JP, Broze GJ, Majerus PW: Purification of human coagulation factors 11, IX, and X using sulfated dextran beads. Methods Enzymol80:22 1, 1981 33. Jaffe EA, Nachman RL, Becker CG, Mimek LR: Culture of human endothelial cells derived from umbilical veins. J Clin Invest 52:2745, 1973 From www.bloodjournal.org by guest on February 6, 2015. For personal use only. 520 34. Bloem LJ, Chen L, Konigsberg WH, Bach RR: Serum stimulation of quiescent human fibroblasts induces the synthesis of tissue factor mRNA followed by the appearance of tissue factor antigen and procoagulant activity. J Cell Physiol 139:418, 1989 35. Maniatis T, Fritsch EF, Sambrook J: Molecular Cloning: A Laboratory Manual. Cold Spring Harbor, NY, Cold Spring Harbor Laboratory, 1982 36. Spicer EK, Horton R, Bloem L, Bach R, Williams KR, Guha A, Kraus J, Lin T-C, Nemerson Y, Konigsberg WH: Isolation of cDNA clones coding for human tissue factor: Primary structure of the protein and cDNA. Proc Natl Acad Sci USA 84:5148, 1987 37. Correa-Rotter R, Mariash CN, Rosenberg ME: Loading and transfer control for Northern hybridization. Biotechniques 12: 154, 1992 38. Schultz DR, Arnold DR: Properties of four acute phase proteins: C-reactive protein, serum amyloid A protein, a,-acid glycoprotein and fibrinogen. Semin Arthritis Rheum 20:129, 1990 39. Rickles FR, Rick PD: Structural features of Salmonella typhimurium lipopolysaccharide required for activation of tissue factor in human mononuclear cells. J Clin Invest 59: 1188, I977 40. Busso N, Huet S, Nicodeme E, Hiemaux J, Hyafil F Refractory period phenomenon in the induction of tissue factor expression on endothelial cells. Blood 78:2027, 1991 41. Miserez R, Jungl TW: LPS-induced, but not interferon gamma-induced, procoagulant activity ofsuspended human macrophages is followed by a refractory state of low procoagulant expression. Thromb Res 65:733, 1992 42. Edwards RL, Levine JB, Green R, Duffy M, Mathews E, Brande W, Rickles F R Activation of blood coagulation in Crohn’s disease. Gastroenterology 92:329, 1987 43. Osterud B, Flaegstad T: Increased tissue thromboplastin activity in monocytes of patients with meningococcal infection: Related to an unfavourable prognosis. Thromb Haemost 495, 1983 44. Cole EH, Schulman J, Urowitz M, Williams C, Levy CA: Monocyte procoagulant activity in glomerulonephritis associated with systemic lupus erythematosus. J Clin Invest 752361, 1985 CERMAK ET AL 45. Lyberg T, Prydz H, Baklien K, Hoyeraal HM: Effect of immune complex-containing sera from patients with rheumatic disease on thromboplastic activity of monocytes. Thromb Res 25: 193, 1982 46. Rivers RPA, Cattermole HEJ, Wright I: The expression of surface tissue factor apoprotein by blood monocytes in the course of infections in early infancy. Pediatric Res 31:567, 1992 47. Tillet WS, Francis T Jr: Serological reactions in pneumonia with a nonprotein somatic fraction of pneumococcus. J Exp Med 52561, 1930 48. Shephard E, Anderson R, Beer SM, Jansen van Rensburg CE, De Beer FC: Neutrophil lysosomal degradation of human C R P CRP-derived peptides modulate neutrophil function. Clin Exp Immunol 73: 139, 1988 49. Dobrinich R, Spagnuolo PJ: Binding ofC-reactive protein to human neutrophils. Inhibition of respiratory burst activity. Arthritis Rheum 34:1031, 1991 50. Ballou SP, Lozanski G: Induction of inflammatory cytokine release from cultured human monocytes by C-reactive protein. Cytokine 4:361, 1992 5 1. Gregory SA, Kornbluth RS, Helin H, Remold HG, Edgington TS: Monocyte procoagulant inducing factor: A lymphokine involved in the T cell-instructed monocyte procoagulant response to antigen. J Immunol 137:3231, 1986 52. Edgington TS, Mackman N, Fan S-T, Ruf W: Cellular immune and cytokine pathways resulting in tissue factor expression and relevance to septic shock. Nouv Rev Fr Hemato1345 15, 1992 53. Mortensen RF, Kidane A, Femandez MC, Tebo JM: C-reactive protein (CRP) receptor-mediated activation of monocytes. J Leukoc Biol20, I99 1 (abstr, suppl2) 54. Wickham NWR, Vercellotti GM, Hammerschmidt DE, Jacob HS: Complement activation by C-reactive protein: Enhancement by chylomicrons. Clin Res 39:335A, 1991 (abstr) 55. Gregory SA, Morrisey JH, Edgington TS: Regulation of tissue factor gene expression in the monocyte procoagulant response to endotoxin. Mol Cell Biol 9:2752, 1989 From www.bloodjournal.org by guest on February 6, 2015. For personal use only. 1993 82: 513-520 C-reactive protein induces human peripheral blood monocytes to synthesize tissue factor J Cermak, NS Key, RR Bach, J Balla, HS Jacob and GM Vercellotti Updated information and services can be found at: http://www.bloodjournal.org/content/82/2/513.full.html Articles on similar topics can be found in the following Blood collections Information about reproducing this article in parts or in its entirety may be found online at: http://www.bloodjournal.org/site/misc/rights.xhtml#repub_requests Information about ordering reprints may be found online at: http://www.bloodjournal.org/site/misc/rights.xhtml#reprints Information about subscriptions and ASH membership may be found online at: http://www.bloodjournal.org/site/subscriptions/index.xhtml Blood (print ISSN 0006-4971, online ISSN 1528-0020), is published weekly by the American Society of Hematology, 2021 L St, NW, Suite 900, Washington DC 20036. Copyright 2011 by The American Society of Hematology; all rights reserved.
© Copyright 2026