Appendix 10 - Skin care presentation
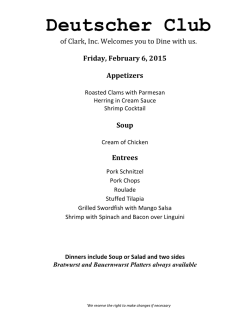
What current evidence is there to give the optimal skin care advice to patients undergoing radical external beam megavoltage radiotherapy? Introduction Turesson et al. (1996) demonstrated that the number of basal cells in the epidermis declines during fractionated RT due to increased cell cycle arrest and reduced mitosis. This causes a thinning of the epidermis and an inflammatory reaction and the variation in the reaction appears to be a genetic predisposition related to individual DNA repair capacity. (Chang-Claude et al., 2005; Pinar et al., 2007; Andreassen and Alsner, 2009) Certain clinical factors can aid in the prediction of which patients are more likely to experience a significant radiation reaction. (Russell et al., 1994; Russell 2010) Extrinsic and Intrinsic factors 52% of departments are not recording this data Extrinsic factors Intrinsic factors Radiotherapy Age Bolus Nutrition Radiosensitisers Smoking and alcohol Chemicals/ thermals/ mechanical irritants Co-morbidities Dose, fractionation, site, and modality of radiotherapy. Some Cytotoxic agents can increase the severity of reaction e.g. Cisplatin, 5Flurouracil, Mitomycin C. e.g. diabetes Previous damage Trauma Obesity Infection UV exposure Systematic Review An extensive literature review was undertaken of over 300 articles from 1980 to October 2010. Two systematic reviews of skin care literature proved invaluable in determining the more robust evidence base. (Bolderston et al., 2006; Kedge 2009) 2014 systematic review undertaken using PICO method and SIGN to determine if, since 2010 there has been any additional evidence. Three systematic reviews also reviewed. (Butcher and Williamson, 2012; Schnur et al., 2013; Chan et al., 2014) Contraindicated products Of significant note is the identification of certain products contraindicated for use on radiotherapy skin reactions: Topical antibiotics, unless there is a proven infection. (Sitton, 1992; Campbell and Lane, 1996; Korinko and Yurick, 1997) Topical steroids on broken skin due to the adverse effect on the wound healing process. (Blackmar, 1997; Rice, 1997; Jones, 1998) Gentian Violet due to potential carcinogenic side effects. (Campbell and Lane, 1996; Rice, 1997; Boot-Vickers and Eaton, 1999) Consensus There are two areas where a more general consensus on guidance is closer to being achieved. Firstly with respect to the use of aqueous cream: This has now been reclassified in the British National Formulary (BNF) as a soap substitute and may be applicable in this usage for patients undergoing radiotherapy. However, it should not be used as a leave-on moisturiser. Secondly with respect to the use of deodorant, where a much stronger evidence base refutes the adverse impact that deodorants were once thought to have. (Bennett, 2009; Watson et al., 2012; Wong et al., 2013) 2014 systematic review A number of studies have been undertaken investigating the use of topical steroids and Wong et al. (2013) make strong recommendations for the use of prophylactic topical steroids. In spite of this some of the published research recommends exercising a degree of caution, particularly regarding any long term implications of using steroids. A plethora of agents is being used on the skin in a nonstandardised fashion. Overall, the evidence base is not strong enough to either support or refute the use of any particular product for topical application. Prophylactic skin care (1) A lack of evidence to support prophylactic use of any specific product (Wells et al., 2004; Richardson et al., 2005; Russell, 2010; Gosselin, 2010) 2011 survey 26 aqueous cream 5 aloe vera base 3 Diprobase® 2 Cavilon® 1 calendula base 2014 survey 17 aqueous cream 6 E45 2 Diprobase ® 2 Aquamax ® 1 Cavilon ® 1 patient use own 49% of departments do not assess what a patient currently uses Prophylactic skin care (2) Evidence indicates that gentle skin and hair washing should be unrestricted for patients and there should be: no restriction to using a specific type of soap (Roy et al., 2001; Bolderston et al., 2006; Aistars and Vehlow, 2007; Butcher and Williamson, 2012) 2011 42 specified the type of soap to use: ‘Simple®’, ‘Dove®’ or ‘none’ being the most common answers. 2014 31 specified the type of soap. 74% of departments report washing restrictions Prophylactic skin care (3) 2011 9 specified the type of deodorant to use: ‘none’ or ‘Pitrok®’ being the most common answers. 2014 19 departments stated patients could use a deodorant; 23 stated they could not. “If patient insists they prefer to use something then rock salt from Holland and Barrett.” 55% departments are still saying ‘no deodorant’ Breast cancer patients who are advised not to use a deodorant often cite this as one less area of control they have in their life and they note concern regarding body odour. (Komarnicki, 2010) Erythema 2011 survey 49 aqueous cream 8 aloe vera base Erythema tends to occur 7 Diprobase® at 2000-4000 cGy 4 Cavilon® 2014 survey 24 aqueous cream 6 E45 ® 4 Diprobase ® 4 Aquamax ® 4 aloe vera base 3 hydrocortisone 1% 3 BioOil ® 3 hydrogel product 29 ISSUED the product 15 products cited aqueous cream may actually comprise skin integrity (Tsang & Guy, 2010; Patel et al., 2013) Dry desquamation 2011 survey Dry desquamation occurs mainly at 3000 cGy and higher 35 aqueous cream 24 hydrocortisone 1% despite some contradictory evidence (Sitton 1992; Bostrom et al., 2001; Sperduti et al., 2006; El Mandani et al., 2012) 2014 survey 16 aqueous cream 5 hydrogel product 5 Diprobase ® 4 hydrocortisone 1% 4 E45 ® 3 patient’s own 33 ISSUED the product 13 products cited Moist desquamation 2011 survey Moist desquamation tends to occurs at 4000 cGy and higher 33 hydrogel product 21 silicone dressing i.e. Mepitel® 18 hydrocolloid base 7 lyofoam base 3 lanolin 2 gentian violet 1 second skin product 2014 survey 13 Intrasite ® 10 Mepilex ® 10 Polymem ® 10 hydrogel product 7 Flamazine ® 40 ISSUED the product 22 products cited Recommendations (1) Pre-treatment The various factors that influence how people react to radiotherapy need to be considered. (Turesson, 1996; Porock et al., 1998; Porock and Kristjanson, 1999; Richardson et al., 2005; Barnett et al., 2011; McQuestion, 2011) Before radiotherapy begins, it is essential that a baseline assessment of the patient’s current skin condition and care is documented, including what skin products are being used currently. Assessments and review of the skin should continue for all patients on a regular basis throughout treatment. (Richardson et al., 2005; Fisher et al., 2006; NHS Scotland, 2010) Education and health promotion strategies and interventions given to patients pre-treatment such as nutritional advice and smoking cessation would be beneficial and are advised. (Wells et al., 2004; Wan et al., 2012; Sharp et al., 2013) Recommendations (2) Wash the skin gently with soap and water and gently pat dry. (Aistars, 2006; Bolderston et al., 2006; Aistars and Vehlow, 2007; Butcher and Williamson, 2012) Use aqueous cream instead of soap if wished but it is NOT recommended as a leave-on moisturiser. (www.evidence.nhs.uk/formulary/bnf) Use a moisturiser that is sodium lauryl sulphate free. (Tsang and Guy, 2013; Patel et al., 2013) Continue to use normal deodorant (unless this irritates the skin), but discontinue if the skin is broken. (Bennett, 2009; Butcher and Williamson, 2012; Watson et al., 2012; Wong et al., 2013) Things to consider as an issuer With a wide variety of products currently available there are bound to be variations in product utilisation and availability; therefore, careful assessment and justification is paramount. ? What are the variation of ingredients in products that use the same generic name e.g. aloe vera, aqueous cream? ? Is a product actually worth the cost? ? How available and reliable is the supplier? ? How often does a product need to be applied? ? How easily is the product applied? Recommendations (3) On broken skin Use appropriate dressing/product on broken skin to reduce further trauma and infection. Suitable products would be non-adhesive, silicone low adhesion, non or low paraffin/petroleum jelly based. NOT use Gentian Violet. (Campbell and Lane, 1996; Rice, 1997; BootVickers and Eaton, 1999) Future research needed (1) New high quality trials are urgently required; enabling a more consistent approach for patients receiving radiotherapy and to inform guidelines. There is a need for further research of new products before they are introduced on an ad-hoc basis, without evidence, into radiotherapy skin care regimens. Future research should include designs that allow assessor blinding and comparators should include ‘current best evidence practice' or 'no intervention'. Number of studies 2011 survey Only 1 (n= 49) department was conducting a RCT into the clinical effectiveness of a topical agent for erythema. There were no assessments into the cost effectiveness for erythema. Only 3 (n=46=6%) departments were conducting RCTs into the clinical effectiveness of a topical agent for moist desquamation. There was one on-going assessment into the cost effectiveness of a product. 2014 survey Only 4 (n=42=9%) departments stated they were conducting or had conducted any trials or evaluation into efficacy of any skin care products at any stage of skin reaction and only 4 (n=42=9%) had assessed cost effectiveness. “would like to be involved with RCT's but find it difficult to sustain with clinical workload and other responsibilities” and “we would like to undertake this sort of analysis but time and resources prohibit this”. Future research needed (2) Assessment and quantification of the extent of radiation induced skin reactions is needed as currently it is unknown how many patients are affected and to what level. Departments need to audit radiation induced skin reactions locally to monitor proportions of patients that develop different RTOG graded reactions across different treatment sites: 1. To increase the quality of information that can be given to patients; 2. To allow departments to monitor their own practice and compare across centres. The extent of the problem? Approximately what percentage of patients in your department get erythema 10 Don't know 91%-100% 81%-90% 71%-80% 61%-70% 51%-60% 41%-50% 31%-40% 21%-30% 11%-20% 0%-10% 8 6 4 2 0 Approximately what percentage of patients in your department get moist desquamation 16 14 12 10 8 6 4 2 0 Don't know 91%-100% 81%-90% 71%-80% 61%-70% 51%-60% 41%-50% 31%-40% 21%-30% 11%-20% 0%-10% Future research needed (3) Evaluation into wet versus dry shaving and perfume and make-up use is needed. Evaluation of treatment aftercare requires review to ensure local continuity and consistency of care across the patient pathway. Further investigations into the skin care reactions: superficial, orthovoltage, and proton beam radiotherapy are required. Patient preferences and compliance. The current position Overall, the evidence base is not strong enough to either support or refute the use of any particular product for topical application. Currently, some of the skin care provided may not actually alleviate the problem and indeed may even compound the effect. Are we actually providing skin care advice to patients based on traditional knowledge and a paternalistic approach to healthcare? (Harris, 2002) The patient perspective Health is: " ... a state of complete physical, psychological, and social wellbeing, and not merely the absence of disease or infirmity.“ WHO (1978) “ We are people, not just bodies.” Patient 7: Harris (1995) As Gosselin, et al. (2010) noted: “patients prefer to take action rather than do nothing” Conclusion The extent of skin conditions is largely unknown. Although the majority of skin reactions subside after a few weeks, some can be prolonged and affect a patient’s quality of life. It may not be possible to stop or even reduce the rates of skin reaction from occurring, but there may be comfort and psychosocial benefits that skin care products provide. Working party Dr Rachel Harris, Professional and Education Manager, SCoR Charlotte Beardmore, Director of Professional Policy, SCoR Amanda Bolderston, Provincial Professional Practice & Academic Leader, BCC Agency, Canada Gemma Burke, Senior Lecturer and Professional Development Facilitator, SHU Sarah James, Professional Officer for Radiotherapy, SCoR Dr Heidi Probst, Reader in Radiotherapy, SHU Claire Bennett, Programme Leader for Radiotherapy and Oncology programme, UWE Samantha Bostock, Superintendent Radiographer, Gloucestershire Oncology Centre Carole Downs, Breast Cancer Specialist Radiographer, Northern Centre for Cancer Care Professor Sara Faithfull, Strategic Lead for Innovation and Enterprise, University of Surrey Sonja Hoy, Nurse Specialist for Head & Neck, The Royal Marsden NHS Foundation Trust Audrey Scott, Macmillan Head and Neck CNS, Mount Vernon Cancer Centre Dr Diana Tait, Consultant Clinical Oncologist, The Royal Marsden NHS Foundation Trust Ellen Trueman, Senior Radiotherapy Sister, St James's Institute of Oncology Professor Mary Wells, Professor of Cancer Nursing Research & Practice, University of Stirling
© Copyright 2026