A Stratification System for Evaluating and Selecting
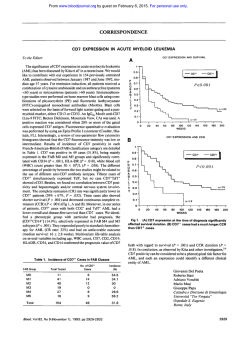
From www.bloodjournal.org by guest on February 6, 2015. For personal use only. CORRESPONDENCE 756 A Stratification System for Evaluating and Selecting Therapies in Patients With Relapsed or Primary Refractory Acute Myelogenous Leukemia To the Editor: Several characteristics have been predictive of outcome of therapy for relapsed or “primary refractory” acute myelogenous leukemia (AML).’-4Among these are duration of first complete remission (CR) and the number of, and response to, prior salvage regimens. Using these covariates, we have developed a system that stratifies patients by probability of response to previous salvage agents. This system may be useful when comparing new salvage regimens and when considering which patients might be candidates for phase I studies. The system is based on analysis of outcome (CR or not) in 206 patients (median age, 56 years) who received chemotherapy without transplantation for relapsed or primary refractory AML, excluding acute promyelocytic leukemia (APL), at M.D. Anderson between 1991 and 1994. For first salvage, 68% of the patients received conventional regimens (principally high-dose ara-C-based), and the remaining 32% received investigational regimens (usually single agents such as topotecan, 2 CDA, CI 973, or taxol). The overall CR rate was 23%. Ninety-three of the 206 patients received a second salvage attempt either at second relapse or after failing to respond to the first attempt. Forty-three percent of the 93 received conventional and 57% received investigational regimens; the overall CR rate was 1 I %. Forty patients received a third and 17 patients received a fourth salvage regimen, with CR rates of 10%and 6%, respectively. The system recognizes four groups: (1) patients with an initial CR duration in excess of 2 years who are receiving their first salvage attempt (15 patients; CR rate, 73%; 95% confidence interval [CI], 45% to 92%); (2) patients with an initial CR duration of 1 to 2 years who are receiving their first salvage attempt (30 patients; CR rate, 47%; 95% CI, 28% to 66%); (3) patients with a first CR lasting less than 1 year, or with no initial CR, who are receiving their initial salvage attempt (160 patients; CR rate, 14%; 95% CI, 8% to 21%); and (4) patients with an initial CR under 1 year, or with no initial CR, who are receiving a second or subsequent (up to and including a fourth) salvage regimen, having not responded to a first salvage attempt (58 patients; 96 salvage attempts; CR rate, 0%; 95% CI, 0% to 4%). Other patients, eg, those who responded on a first salvage attempt and who proceed to a second salvage regimen, are excluded from consideration because of small numbers, although there are suggestions that patients who respond to the first regimen may be relatively responsive to the second (3/7 CRs if first CR duration was I to 2 years; 2/13 if it was shorter). The system was similarly effective in stratifying the 137 patients who received both initial and salvage therapy at M.D. Anderson and the 69 patients who were referred in relapse (49% of whom had received 2 1 regimen for relapse before referral), with CR rates of 8 of 1 I , 1 1 of 24, 11 of 102, and 0 of 80, and 3 of 4, 3 of 6 , 12 of 58, and 0 of 18 for the 4 groups in the M.D. Anderson and referred categories, respectively. Considering only patients who received conventional (eg, HDAC, anthracycline, and mitoxantrone + etoposide) regimens, CR rates were 11 of 14, 14 of 22, 21 of 104, and 0 of 44, respectively, in the four groups. Applied prospectively to the 64 salvage AML, non-APL patients treated without transplantation since 1995, the scheme’s four groups had CR rates of 3 of 3, 4 of 14, 4 of 33, and 0 of 19, respectively. Tested in patients treated from 1986 through 1989, CR rates were 8 of 11, 13 of 30, 23 of 135, and 0 of 74 in groups 1 through 4, respectively. Systems including more covariates, eg, cytogenetics, have been examined. Not only is complexity increased, but also general applicability may be decreased. Equally importantly, as more covariates are included, the ability of a prognostic system to stratify future patients often decreases (“overfitting”).’ Such was the case when more complex models based on our 1991 through 1994 data were applied to 1995 and 1996. We use the four-group system described above both to guide therapy and to compare new salvage regimens. Patients in group 1 (mean CR rate with prior therapies, about 70%) receive similar anthracycline + ara-C-based regimens as newly diagnosed patients, whom they resemble prognostically. In contrast, patients in group 4 (mean CR rate, < 1%) receive phase I agents. Phase I1 studies are conducted separately (but simultaneously) in patients in groups 2 (mean CR rate, 40%) and 3 (mean CR rate, 10%to 20%). Among the advantages of this method are (1) reduction in the heterogeneity that results if patients in groups 2 and 3 (or patients in groups 2, 3, and 4) are taken as one group, as is common practice? with heterogeneity increasing the chances of falsely negative or falsely positive results when testing new agents; and (2) formal definition of a group (group 2) that may be sufficiently favorable prognostically to avoid the false-negative that presumably results if new regimens are only examined in the least “favorable” patient^.'.^.' Although randomized phase 11 designs have been proposed to reduce heterogeneity among groups of patients treated with different agents,’ the sample sizes envisioned in these designs are insufficient for this purpose in the absence of stratification, using a system such as that proposed above. Although the need to test new agents separately in different strata potentially increases phase II sample size, Bayesian pre-phase I1 selection designs effectively address the issue of sample size.’ We believe these designs together with the stratification system outlined here represent improvements in methodology for testing new agents in AML. Elihu Estey Steven Komblau Sherry Pierce Hagop Kantarjian Miloslav Beran Michael Keating Leukemia Section University of Texas M.D. Anderson Cancer Center Houston, TX REFERENCES I . Keating MJ, Kantarjian H, Smith TL, Estey E, Walters R, Anderson B, Beran M, McCredie KB, Freireich EJ: Response to salvage therapy and survival after relapse in acute myelogenous leukemia. J Clin Oncol 7:1071, 1989 2. Hiddemann W, Martin WR, Sauerland CM, Heinecke A, Biichner T: Definition of refractoriness against conventional chemotherapy in acute myeloid leukemia: A proposal based on the results of retreatment by thioguanine, cytosine arabinoside, and daunorubicin (TAD 9) in 150 patients with relapse after standardized first line therapy. Leukemia 4: 184, 1990 3. Angelov L, Brandwein JM, Baker MA, Scott G , Sutton DM, Keating A: Results of therapy for acute myeloid leukemia in first relapse. Leuk Lymphoma 6:15, 1991 4. Estey E: Treatment of refractory AML. Leukemia (in press) Matchar DB, Reichert TA: Regression 5. Harrell FE Jr, Lee IU, models for prognostic prediction: Advantages, problems, and suggested solutions. Cancer Treat Rep 69:1071, 1985 6 . Simon R: Importance of prognostic factors in cancer clinical trials. Cancer Treat Rep 68: 185, 1984 7. Simon R, Wittes RE, Ellenberg SS: Randomized phase 11clinical trials. Cancer Treat Rep 69:1375, 1985 8. Thall PF, Estey E H A Bayesian strategy for screening cancer treatments prior to phase I1 clinical evaluation. Stat Med 12:1197, 1993 From www.bloodjournal.org by guest on February 6, 2015. For personal use only. 1996 88: 756 A stratification system for evaluating and selecting therapies in patients with relapsed or primary refractory acute myelogenous leukemia [letter] E Estey, S Kornblau, S Pierce, H Kantarjian, M Beran and M Keating Updated information and services can be found at: http://www.bloodjournal.org/content/88/2/756.citation.full.html Articles on similar topics can be found in the following Blood collections Information about reproducing this article in parts or in its entirety may be found online at: http://www.bloodjournal.org/site/misc/rights.xhtml#repub_requests Information about ordering reprints may be found online at: http://www.bloodjournal.org/site/misc/rights.xhtml#reprints Information about subscriptions and ASH membership may be found online at: http://www.bloodjournal.org/site/subscriptions/index.xhtml Blood (print ISSN 0006-4971, online ISSN 1528-0020), is published weekly by the American Society of Hematology, 2021 L St, NW, Suite 900, Washington DC 20036. Copyright 2011 by The American Society of Hematology; all rights reserved.
© Copyright 2026