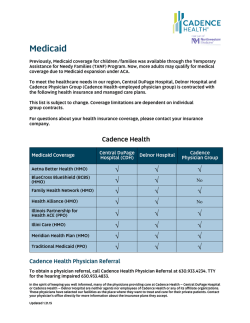
General Provider and Participant Information - Health PAS
Idaho MMIS Provider Handbook General Provider and Participant Information Table of Contents 1. 2. Section Modifications ............................................................................................ 1 General Provider and Participant Information ........................................................... 7 2.1. Provider Participation...................................................................................... 7 2.1.1. Provider Participation Requirements ........................................................... 7 2.1.2. Provider Responsibilities ........................................................................... 7 2.1.3. Payment Error Rate Measurement (PERM)................................................... 8 2.1.4. Medicaid Provider Identification Numbers .................................................... 8 2.1.5. Signature-On-File Form ............................................................................ 9 2.1.6. Provider Recertification ........................................................................... 10 2.1.7. Provider Termination .............................................................................. 10 2.1.8. Surveillance and Utilization Review .......................................................... 10 2.2. Services for Providers ................................................................................... 11 2.2.1. Overview .............................................................................................. 11 2.2.2. Idaho Medicaid Automated Customer Service (Idaho MACS)........................ 11 2.2.3. Provider Enrollment ............................................................................... 12 2.2.4. Provider Service Representatives (PSRs)................................................... 14 2.2.5. Provider Relations Consultants (PRC) ....................................................... 15 2.3. Participant Eligibility ..................................................................................... 16 2.3.1. Overview .............................................................................................. 16 2.3.2. Medicaid Identification Card .................................................................... 16 2.3.3. Covered Benefits ................................................................................... 17 2.3.4. Tamper Resistant Prescription Requirements ............................................. 17 2.3.5. Verifying Participant Eligibility ................................................................. 18 2.3.6. Participant Program Abuse/Lock-In Program ............................................. 19 2.4. Benefit Plan Coverage................................................................................... 20 2.4.1. Medicaid Enhanced Plan .......................................................................... 20 2.4.2. Medicaid Basic Plan ................................................................................ 20 2.4.3. Presumptive Eligibility (PE) ..................................................................... 21 2.4.4. Pregnant Women (PW) ........................................................................... 23 2.4.5. Breast and Cervical Cancer ..................................................................... 24 2.4.6. Medicare Savings Program ...................................................................... 25 2.4.7. Medicare-Medicaid Coordinated Plan (MMCP) ............................................. 28 2.4.8. Otherwise Ineligible Non-citizens (OINC) .................................................. 30 2.5. Healthy Connections (HC) ............................................................................. 30 2.5.1. Overview .............................................................................................. 30 2.5.2. Importance of Verifying Medicaid Eligibility and HC/IMHH Enrollment ........... 31 2.5.3. Provider Enrollment ............................................................................... 31 2.5.4. Participant Enrollment ............................................................................ 32 2.5.5. Referrals ............................................................................................... 35 2.6. Idaho Medicaid Health Home ......................................................................... 39 2.6.1. Overview .............................................................................................. 39 2.6.2. Diagnosis .............................................................................................. 39 2.6.3. Risk Factors .......................................................................................... 39 2.6.4. Idaho Medicaid Health Home Program Goals ............................................. 39 January 29, 2015 Page i Idaho MMIS Provider Handbook General Provider and Participant Information 2.6.5. Initial Provider and Participant Enrollment ................................................. 39 2.6.6. Provider Responsibilities ......................................................................... 41 2.6.7. Responsibilities for Care Coordination ....................................................... 44 2.6.8. Provider Reporting ................................................................................. 44 2.6.9. Provider Reimbursement......................................................................... 47 2.6.10. Participant Enrollment ......................................................................... 48 2.7. Child Wellness Exams ................................................................................... 49 2.7.1. Wellness Exams ..................................................................................... 49 2.7.2. Content of Wellness Exams ..................................................................... 49 2.7.3. Periodicity Schedule ............................................................................... 49 2.7.4. Early & Periodic Screening, Diagnosis & Treatment (EPSDT) ........................ 57 2.7.5. Billing ................................................................................................... 58 2.8. Preventive Health Assistance (PHA) ................................................................ 58 2.8.1. Weight Management .............................................................................. 58 2.8.2. Wellness ............................................................................................... 58 Table of Figures Figure Figure Figure Figure Figure Figure Figure Figure Figure Figure Figure Figure Figure Figure Figure 2-1: Information Available Through MACS ......................................................... 11 2-2: Provider File Updates ............................................................................... 13 2-3: Health Card ............................................................................................ 16 2-4: Example of PW Coverage .......................................................................... 23 2-5: Part B Medicare Savings Program .............................................................. 26 2-6: Required Documents ................................................................................ 45 2-7: Required Data ......................................................................................... 45 2-8: Infancy Screening.................................................................................... 50 2-9: Anticipatory Guidance During Infancy ........................................................ 51 2-10: Early Childhood Screening ...................................................................... 51 2-11: Anticipatory Guidance during Early Childhood ............................................ 52 2-12: Middle Childhood Screening .................................................................... 53 2-13: Anticipatory Guidance During Middle Childhood ......................................... 54 2-14: Adolescence Screening ........................................................................... 54 2-15: Anticipatory Guidance during Adolescence ................................................ 55 January 29, 2015 Page ii Idaho MMIS Provider Handbook General Provider and Participant Information 1. Section Modifications Version Section Update Publish Date SME 26.0 All Published version 1/29/15 TQD 25.4 New sections 1/29/15 Updated for clarity 1/29/15 Removed sections 1/29/15 25.1 2.8 Preventive Health Assistance (PHA) and subsections 2.7.5 Billing and 2.7.5.1 Diagnosis Codes 2.7.5 Diagnosis and 2.7.6 Treatment 2.4.4.2 Covered Services 1/29/15 25.0 All Removed requirements for chiropractic and physical therapy billing Published version C Brock D Baker C Taylor C Brock D Baker C Brock D Baker T Wright D Baker TQD 24.3 2.4.7.4 Billing Procedures Changed “Adult State Plan HCBS” to “Adult DD State Plan HCBS” 11/24/14 24.2 2.4.7.2 Medicaid Covered Services Added services 11/24/14 24.1 2.4.7.1 Program Overview Added DD State Plan to note 11/24/14 24.0 All Published version 09/11/14 23.1 2.4.2.3 Excluded Services 2.4.2.4 Restricted Services 09/11/14 C But C Taylor 23.0 All Removed psychosocial rehabilitation from list of excluded services; removed reference to outpatient mental health under restricted services Published version 08/01/14 TQD 22.2 2.5.5.6 Reimbursement for Services Requiring Referral Updated information in fourth bullet 08/01/14 22.1 2.2.3.1 Non-billing Ordering and Referring Providers All Added new information 08/01/14 Published version 07/25/14 C Brock M Hall C Taylor R Sosin T Kinzler TQD 21.1 2.5.5.6 Reimbursement for Services Requiring Referral 07/25/14 C Brock M Hall D Baker 21.0 All Updated verbiage for fourth bullet to read “assessment of civil monetary penalties by the Idaho Department of Health and Welfare” Published version 07/02/14 TQD 20.2 Updated sections per CCF 10727 MMCP Expansion 07/02/14 Flo Clarke (IDHW) T Kinzler Clarified information for QMB and QMB+ Published version 07/02/14 20.0 2.4.6.5 Medicaid Pays a Portion of the Dually Eligible Medicare Beneficiaries 2.4.6.6 Qualified Medicare Beneficiary (QMB) 2.4.7 Medicare-Medicaid Coordinated Plan (MMCP) 2.4.7.2 Medicaid Covered Services 2.4.7.3 Participant Identification Number 2.4.7.4 Billing Procedures 2.4.6.4 Part B Medicare Savings Program All 06/04/14 C Taylor D Baker TQD 19.1 2.5.5.2 Referral Requirements Additional information added 06/04/14 C Taylor 19.0 All Published version 05/30/14 C Taylor D Baker TQD 25.3 25.2 22.0 20.1 January 29, 2015 11/24/14 E Ellison C Barrott C Taylor E Ellison C Barrott C Taylor E Ellison C Barrott C Taylor TQD Page 1 of 59 Idaho MMIS Provider Handbook Version Section 18.19 2.6.8.5 Clinical Quality 18.18 2.6.8.3 Required Data 18.17 2.6.7 Responsibilities for Care Coordination 2.6.6.9 Patient Notification 18.16 General Provider and Participant Information Update Publish Date SME Updated to match current policy; deleted Diabetes Measures and Asthma Measures subsections Updated to match current policy 05/30/14 C Brock 05/30/14 C Brock Updated section title; updated to match current policy Updated section title; updated to match current policy Updated to match current policy 05/30/14 C Brock 05/30/14 C Brock 05/30/14 C Brock 05/30/14 C Brock 18.15 2.6.6.6 Follow Up Protocol 18.14 2.6.5 Initial Provider and Participant Enrollment 2.6.1 Overview Updated Step 6 Updated to match current policy 05/30/14 C Brock 2.5.5.6 Reimbursement for Services Requiring a Referral 2.5.5.5 Services Not Requiring a HC PCP Referral Added last bullet for referral not required Updated Family Planning Services bullet; added “outpatient” to Mental Health Services Deleted section 05/30/14 C Brock 05/30/14 C Brock 05/30/14 C Brock 18.13 18.12 18.11 18.10 18.9 2.5.5.3 Referral Approval Reasons 2.5.5.2 Referral Requirements Updated to match current policy 05/30/14 C Brock 18.7 2.5.5.1 General Guidelines Updated to match current policy 05/30/14 C Brock 18.6 Deleted section 05/30/14 C Brock 18.5 2.5.4.4 Participants Changing Primary Care Providers 2.5.4.1 Enrollment in HC Updated to match current policy 05/30/14 C Brock 18.4 2.5.3.2 HC Participant Rosters Added last bullet 18.3 2.5.3 Provider Enrollment 05/30/14 C Brock 18.2 2.5.2 Importance of Verifying Medicaid Eligibility and HC/IMHH Enrollment 2.4.4.2 Covered Services Added reference to provider agreement in last bullet Added references to Health Home 05/30/14 C Brock 05/30/14 C Brock 05/02/14 TQD 05/02/14 D Baker 02/21/14 TQD 18.1 18.0 All Added a link to the section for Services Not Requiring a HC PCP Referral. Published version 17.1 Figure 2-2 Provider File Updates All Changed EFT Information to Financial Agreement Published version 16.1 2.5.5.6 Services Not Requiring a HC PCP Referral Removed referral requirement under pregnancy related services 02/21/14 16.0 All Published version 01/24/14 C Brock C Taylor D Baker TQD 15.2 2.5.5.5 General Guidelines Updated TPA User Guide name and link 01/24/14 C Taylor 15.1 2.3.6.1 Primary Care Physician (PCP) All Updated TPA User Guide name and link 01/24/14 C Taylor Published version 12/20/13 TQD 14.1 2.5.5.6 Services Not Requiring a HC PCP Referral Clarification on referral requirements for behavioral health services. 12/20/13 C Brock 14.0 All Published version 12/13/13 TQD 13.3 2.1.7 Provider Termination Updated for clarity 12/13/13 D Baker 13.2 2.4.4.4 Medical Necessity Updated for clarity 12/13/13 D Baker 13.1 2.5.5.6 Services Not Requiring a HC PCP Referral All Updated for clarity and deleted outdated information Published version 12/13/13 11/08/13 M Wasserman H McCain 2.4.2.3 Excluded Services; 2.4.7.4 Billing Procedures; Figure 2-6 MMCP Covered Services All Updated ICF/MR to ICF/ID; updated mentally retarded to intellectually disabled 11/08/13 C Taylor Published version 08/29/13 H McCain 17.0 15.0 13.0 12.1 12.0 January 29, 2015 Page 2 of 59 Idaho MMIS Provider Handbook Version 11.15 General Provider and Participant Information Section 11.14 2.6.10.1 Ongoing Enrollment Process 2.6.8.4 Reporting Documents 11.13 2.6.8.2 Required Documents 11.12 2.6.8.1 Data and Reporting Requirements and Procedures 2.6.7 Responsibilities for Service Coordination and Transitional Care Coordination with Facilities 2.6.6.8 Non-Clinical Health Care Needs 2.6.6.2 Care Plan Publish Date Update Added new information, deleted outdated information Updated contact information and completion time for PCMH-A form Updated contact information 08/29/13 Updated contact information 08/29/13 Added new information, deleted outdated information 08/29/13 deleted 08/29/13 deleted 08/29/13 2.6.5 Initial Provider and Participant Enrollment 2.5.5.6 Services Not Requiring a HC PCP Referral 2.5.5.1 General Guidelines Added new information, outdated information Added new information, outdated information Added new information, outdated information Added new information, outdated information Add new information deleted 08/29/13 deleted 08/29/13 11.4 2.5.4.4 Participants Changing Primary Care Providers 2.5.4.1 Enrollment in HC Added new information, deleted outdated information Added new information 11.3 2.5.4 Participant Enrollment 11.2 2.5.3.3 Primary Care Provider Listing 2.4.4.2 Covered Services Deleted Voluntary, added new information Added new section 11.11 11.10 11.9 11.8 11.7 11.6 11.5 11.1 Deleted 60-day from family planning services. Added HC referral not required for fp. Published version 08/29/13 08/29/13 08/29/13 08/29/13 08/29/13 08/29/13 08/29/13 08/29/13 SME C C C C C C C C C C Brock Taylor Brock Taylor Brock Taylor Brock Taylor Brock Taylor C C C C C C C C C C C C C C C C C C C C Brock Taylor Brock Taylor Brock Taylor Brock Taylor Brock Taylor Brock Taylor Brock Taylor Brock Taylor Brock Taylor Brock Taylor 11.0 All 04/24/13 TQD 10.18 2.1.8 Surveillance and Utilization Review 2.5.5.7 Reimbursement for Services Requiring Referral 2.5.5.6 Services Not Requiring a HC PCP Referral 2.5.5.4 Method of Referral Updated section 04/24/13 L Stiles Updated for clarity 04/24/13 C Brock Updated list 04/24/13 C Brock Updated for clarity 04/24/13 C Brock Added information 04/24/13 C Brock 10.13 2.5.5.3 Referral Approval Reasons 2.5.5.2 Referral Requirements Updated for clarity 04/24/13 C Brock 10.12 2.5.5.1 General Guidelines Updated for clarity 04/24/13 C Brock 10.11 2.5.4.5 Participant Disenrollment by the Provider 2.5.4.4 Participants Changing PCP 2.5.4.2 Exceptions & Exemptions to HC Enrollment 2.5.4.1 Voluntary Enrollment in HC 2.5.3.2 HC Participant Rosters Added/deleted information 04/24/13 C Brock Updated for clarity 04/24/13 C Brock Updated for clarity 04/24/13 C Brock Updated for clarity 04/24/13 C Brock Updated last bullet; deleted last paragraph Updated bulleted list 04/24/13 C Brock 04/24/13 C Brock 04/24/13 C Brock 10.17 10.16 10.15 10.14 10.10 10.9 10.8 10.7 10.6 10.5 2.5.3.1 HC Case Management Payment 2.5.3 Provider Enrollment January 29, 2015 Removed “from the original application information” in last bullet Page 3 of 59 Idaho MMIS Provider Handbook Version 10.4 General Provider and Participant Information Section Update Publish Date SME 2.5.2 Importance of Verifying Medicaid Eligibility and HC Enrollment 2.3.5.1 Eligibility Verification Added note 04/24/13 C Brock Added co-payments to bulleted list 04/24/13 C Brock Added co-payments to last paragraph 04/24/13 C Brock 10.1 2.3.5 Verifying Participant Eligibility 2.2.3 Provider Enrollment Added IMHH 04/24/13 C Brock 10.0 All Published version 03/27/13 C Taylor 9.2 2.6.2 Provider Responsibilities, Care Plan 2.6.2 Provider Responsibilities, Care Plan All Changed “must” to “may” (…Health Home provider may provide …) Changed “may” back to “must” (…care plan, may include…) Published version 03/27/13 C Brock 03/27/13 C Brock 2.6.2 Provider Responsibilities, Care Plan All Changed “must” to “may” (…care plan, may include…) Published version 03/22/13 C Taylor Updated information 03/22/13 C Brock 7.10 2.6.3.6 Practice Transformation Measures 2.6.3.4 Clinical Quality Updated for clarity 03/22/13 C Brock 7.9 2.6.3.3. Reporting Documents Updated information 03/22/13 C Brock 7.8 2.6.3.2 Required Data Updated for clarity 03/22/13 C Brock 7.7 2.6.3.1 Required Documents Updated information 03/22/13 C Brock 7.6 2.6.2 Provider Responsibilities Updated sections for clarity 03/22/13 C Brock 7.5 Updated steps table 03/22/13 C Brock Updated for clarity 03/22/13 L Oleson Added IMHH information 03/22/13 C Brock Updated for clarity 03/22/13 L Oleson 7.1 2.6.1 Initial Provider and Participant Enrollment 2.5.5.7 Reimbursement for Services Requiring Referral 2.3.5 Verifying Participant Eligibility 2.1.8.1 Provider Program Abuse 2.1.7 Provider Termination Updated for clarity 03/22/13 L Oleson 7.0 All Published version 12/31/12 C Stickney 6.5 2.6 Idaho Medicaid Health Homes 2.3.5.1 Eligibility Verification Added new section for new IDMHH 12/31/12 C Brock Updated information for MACS 12/31/12 R Czerny Added section 12/31/12 J Siroky Added Health Home to table 12/31/12 R Czerny 6.1 2.3.4 Tamper Resistant Prescription Requirements Figure 2-1: Information Available Through MACS 2.1.2 Provider Responsibilities Updated list 12/31/12 C Brock 6.0 All Published version 11/30/12 C Stickney 5.23 All Updated links 11/30/12 C Stickney 5.22 2.6.6 Treatment Updated information 11/30/12 C Brock 5.21 2.6.5 Diagnosis Updated information 11/30/12 C Brock 10.3 10.2 9.1 9.0 8.1 8.0 7.11 7.4 7.3 7.2 6.4 6.3 6.2 03/26/13 C Taylor 03/26/13 C Brock 5.20 2.6.4 EPSDT Updated information 11/30/12 C Brock 5.19 2.5.5.7 Reimbursement for Services Requiring Referral 2.5.5.6 Services Not Requiring a Healthy Connections Primary Care Provider (PCP) Referral 2.5.5.5 Advantages of Electronic Online Referrals 2.5.5.4 Method of Referral Updated information 11/30/12 C Brock Updated information 11/30/12 C Brock Added section 11/30/12 C Brock Updated information 11/30/12 C Brock 2.5.5.3 Referral Approval Reasons on the HC Referral Form and Electronic Referrals Added section 11/30/12 C Brock 5.18 5.17 5.16 5.15 January 29, 2015 Page 4 of 59 Idaho MMIS Provider Handbook Version General Provider and Participant Information Section Update Publish Date SME 5.14 2.5.5.2 Referral Requirements Added section 11/30/12 C Brock 5.13 2.5.5.1 General Guidelines Added section 11/30/12 C Brock 5.12 2.5.5 Referrals Added section 11/30/12 C Brock 5.11 Added section 11/30/12 C Brock Added section 11/30/12 C Brock Added section 11/30/12 C Brock Added detail 11/30/12 C Brock 5.7 2.5.4.4 Participants changing Primary Care Providers 2.5.4.3 Mandatory Enrollment in HC 2.5.4.2 Exceptions and Exemptions to HC Enrollment 2.5.4.1 Voluntary Enrollment in HC 2.5.4 Participant Enrollment Added detail 11/30/12 C Brock 5.6 2.5.3.2 HC Participant Rosters Added section 11/30/12 C Brock 5.5 2.5.3.1 HC Case Management Payment 2.5.3 Provider Enrollment Added detail 11/30/12 C Brock 5.10 5.9 5.8 5.4 Added detail 11/30/12 C Brock Updated table 11/30/12 C Stone Added section 11/30/12 C Brock Removed “Fraud” from Medicaid Program Integrity Unit name Published version 11/30/12 L Stiles 5.0 Figure 2-2: Provider File Updates 2.5.2 Importance of Verifying Medicaid eligibility and HC Enrollment 2.1.8.1 Provider Program Abuse All 10/11/12 TQD 4.3 2.3.2 Medicaid ID Card 10/11/12 C Taylor 4.2 2.5.4.5 Services Not Requiring a Healthy Connections Primary Care Provider (PCP) Referral 2.2.4 Provider Service Representatives (PSRs) All Changed ineligible aliens to otherwise ineligible non-citizens Updated limitation reduced to six (6) per calendar year 10/11/12 C Taylor 10/11/12 C Taylor 5.3 5.2 5.1 4.1 Corrected PSR phone number from 888 to 866 Published version 11/23/11 TQD Added Urgent Care Clinic Services 11/23/11 R Pewtress Removed outdated information 11/23/11 R Pewtress Updated to make current 11/23/11 R Pewtress 3.5 2.5.4.5 Services Not Requiring a Healthy Connections Primary Care Provider (PCP) Referral 2.5.4.4 Scope of Services Authorized 2.5.4.3 Documentation of Referrals 2.5.3 Participant Enrollment Updated wording 11/23/11 R Pewtress 3.4 2.5.2 Provider Enrollment Added fee payments 11/23/11 R Pewtress 3.3 Added table of information available through MACS 11/23/11 R Czerny Updated information 11/23/11 K Mcneal Added information 11/23/11 K Mcneal 3.0 2.2.2 Idaho Medicaid Automated Customer Service (Idaho MACS) 2.1.8.1 Provider Program Abuse 2.1.8 Surveillance and Utilization Review All Published version 07/29/11 TQD 2.2 2.2.3.1 Provider File Updates 07/29/11 L Sauer 2.1 2.1.3 (PERM) 07/29/11 2.0 All Updated table (Service Location Summary) Added section for Payment Error Rate Measurement Published version B SchellRuby TQD 1.5 2.5.1; 2.5.4.2; 2.5.4.3 Updated HC information 08/27/11 T Kinzler 1.4 2.6.7.2 Removed modifiers 08/27/11 M Meints 1.3 All Replaced member with participant 08/27/11 TQD 1.0 All Sections were renumbered to accommodate additional information 08/27/11 TQD 4.0 3.8 3.7 3.6 3.2 3.1 January 29, 2015 08/27/11 Page 5 of 59 Idaho MMIS Provider Handbook Version 1.1 1.0 Section 2.1.3.1. All January 29, 2015 General Provider and Participant Information Update Updated section for clarification Initial document – published version Publish Date 08/27/11 05/07/10 SME T Kinzler TQD Page 6 of 59 Idaho MMIS Provider Handbook General Provider and Participant Information 2. General Provider and Participant Information 2.1. Provider Participation 2.1.1. Provider Participation Requirements All providers wishing to participate in the Idaho Medicaid Program must complete a provider application through the Molina Medicaid website. The Provider Enrollment link in the left menu bar will take you to the online application to apply to become an Idaho Medicaid provider. A complete application includes a Medicaid Provider Enrollment Agreement and a W9, which must be signed by the provider and submitted with the enrollment application along with other attachments to Molina through the website. The provider must meet all applicable state and Medicaid licensure/certification and insurance requirements to practice their profession. In addition, the provider qualification requirements for the service(s) to be provided must be met. Information supplied will be used to validate credentials. Other certification/licensure and proof of insurance may be required as provided for in IDAPA 16.03.09 Medicaid Basic Plan Benefits, and IDAPA 16.03.10 Medicaid Enhanced Plan Benefits. Continued provider participation is contingent on the ongoing maintenance of such licensure/certification and proof of insurance. The loss of or failure to renew the required license/certification and proof of insurance is cause to terminate a provider’s participation in the Idaho Medicaid Program. Additional information about the Idaho administrative rules is available on Access Idaho. Select Government and then select Laws & Rules/Administrative Rules. 2.1.2. Provider Responsibilities Providers have the following ongoing responsibilities. • To offer services in accordance with Title VI of the 1964 Civil Rights Act and Section 504 of the Rehabilitation Act of 1973, as amended. • To review and abide by the contents of all Idaho Medicaid rules governing the reimbursement of items and services under Medicaid. • To review periodic provider information releases and other program notification issued by Medicaid. • To be licensed, certified, or registered with the appropriate state authority and to provide items and services in accordance with professionally recognized standards. • To keep Medicaid and Molina advised of the provider’s current address and telephone number. • To sign every claim form submitted for payment, or complete a signature-on-file form (including electronic signatures). • To acknowledge when Medicaid is a secondary payer and agree to seek payment from other sources. • To accept Medicaid payment for any item or service as payment in full and to make no additional charge for the difference. • To comply with the disclosure of ownership requirements. • To comply with the advanced directives requirement. • To make records available to Medicaid upon request. • To not bill a Medicaid participant unless: o The item or service is not covered by Medicaid and the participant is notified January 29, 2015 Page 7 of 59 Idaho MMIS Provider Handbook o General Provider and Participant Information in writing prior to receiving the item or service. A third party payment was made to the participant instead of the provider, in which case the participant may be billed for an amount equal to that payment. Services provided in excess of the Medicaid service limitations or not covered by Idaho Medicaid may be charged to the participant, if the participant is advised prior to receiving the service or item and agrees to be responsible for payment. Acceptance of the medical services beyond the limitations is the participant’s financial responsibility. 2.1.2.1. Medical Record Requirements Idaho Code Section 56-209h requires that providers generate records at the time the service is delivered, and maintain all records necessary to fully document the extent of services submitted for Medicaid reimbursement. This includes documentation of referrals made or received on behalf of Medicaid participants enrolled in the Healthy Connections (HC) Program. Providers are required to retain records to document services submitted for Medicaid reimbursement for at least five years after the date of service. 2.1.3. Payment Error Rate Measurement (PERM) The Centers for Medicare and Medicaid Services (CMS) implemented the Payment Error Rate Measurement (PERM) program to measure improper payments in the Medicaid and the State Children's Health Insurance Program (SCHIP). PERM is designed to comply with the Improper Payments Information Act of 2002 (IPIA; Public Law No. 107-300). For PERM, CMS is using contractors to perform statistical calculations, medical records collection, and medical data processing review of Medicaid and SCHIP fee-for-service (FFS) claims. Medical records are needed to support medical reviews that the CMS review contractor will conduct on the Medicaid and SCHIP FFS claims to determine whether the claims were correctly paid. It is important that providers cooperate by submitting all requested documentation within the designated timeframe. Failure to provide the requested documentation is in violation of Idaho Code Section 56-209h and the Idaho Medicaid Provider Agreement. NOTE: Providers are required to notify the Department of any changes, including but not limited to mailing addresses, service locations, and phone numbers, within 30 days of the date of the change. All providers should check the system to ensure their phone numbers and addresses are correct in the Idaho Medicaid provider file. If not, please request a change immediately to ensure the PERM medical record request can be delivered to the correct address. See Section 2.2.3.3 Provider File Updates for more information. Detailed information regarding the PERM program requirements is available online under the Payment Error Rate Measurement heading. 2.1.4. Medicaid Provider Identification Numbers 2.1.4.1. Individual Provider Numbers The National Provider Identifier (NPI) is part of HIPAA. The NPI number or numbers must be used on all electronic claims and will identify healthcare providers to health plans with a January 29, 2015 Page 8 of 59 Idaho MMIS Provider Handbook General Provider and Participant Information unique 10-digit numeric provider identifier. An NPI can only be associated to one Tax ID, but a Tax ID can be associated to many NPI numbers or Idaho Medicaid Provider numbers. Providers who registered in the MMIS with an NPI will use that NPI on all their transactions, whether paper or electronic. Providers without an NPI will use the ‘M’ or ‘A’ number assigned to them during the registration/application process. Providers with an NPI will be paid through the pay-to address associated to the NPI. Providers who are not eligible for, or do not have, an NPI will have a unique eight-digit Idaho Medicaid provider number assigned when the provider is approved to service Medicaid participants. Claims will be paid through the pay-to address associated with the Medicaid provider number. 2.1.4.2. Multiple Service Locations When billing claims, providers with multiple service locations must enter a three-digit site number (i.e. 001, 002) to identify the specific location, in addition to their NPI/Medicaid ID. The three-digit location code was identified on your approval letter when you became a Medicaid provider. You can also obtain this number by logging into your trading partner account to view the information. This information will be entered in the following fields. • Paper UB04 enter in field 2 • Paper CMS 1500 enter in field 32a • Paper ADA enter in field 35 • Electronic claims refer to 837 Professional/Institutional/Dental companion guide 2.1.4.3. Group Practice The Centers for Medicare and Medicaid Services (CMS) requires the identification of the individual who actually performs a service when billing under a group number. The performing provider’s individual NPI/Medicaid provider number must be on the claim as well as the provider’s group NPI/Medicaid number. 2.1.5. Signature-On-File Form A provider or authorized agent must sign in the claimant’s certification field on all claims. This is an agreement the provider makes to accept payment from Medicaid as payment in full for services rendered. The provider cannot bill the participant for an unpaid balance. Providers must sign every claim form or complete a Signature-On-File form. This form is used to submit paper claims without a signature and/or to submit electronic claims. This form allows submission of claims without a handwritten signature. It is used for computergenerated, signature stamp, or typewritten signatures. The Signature-On-File form remains on file at Molina and must exactly match the information in the claimant’s certification field on the claim form. Never submit paper claims with the claimant’s certification field blank. Enter Signature-on-File or have the provider sign in field 31 of the CMS-1500 claim form or field 62 on the ADA claim form. Contact Molina Provider Enrollment for more information as indicated in Section 2.2 Services for Providers. To bill electronically, it is necessary to complete a Trading Partner Agreement. The Trading Partner Agreement and a Signature-On-File form are available online at the Molina Medicaid website or as paper copy by request from Provider Services. January 29, 2015 Page 9 of 59 Idaho MMIS Provider Handbook 2.1.6. General Provider and Participant Information Provider Recertification In accordance with state and federal regulations, Medicaid monitors the status of provider participation requirements that apply to each individual provider type. Continued licensure, certification, insurance, and other provider participation requirements are verified on an ongoing basis. 2.1.7. Provider Termination Medicaid is required to deny applications for provider status or terminate the Medicaid Provider Agreement of any provider suspended from the Medicare Program or another state’s Medicaid program. The Department of Health and Welfare (DHW) may also terminate a provider’s Medicaid status when the provider fails to comply with any term or provision of the Medicaid Provider Agreement. This includes failing to notify Medicaid or Molina in writing of any changes in address or ownership. Continued provider participation is contingent on the ongoing maintenance of current licensure, certification, or insurance. Failure to renew required licenses, certification, or insurance is cause to terminate a provider’s participation in the Idaho Medicaid Program. 2.1.8. Surveillance and Utilization Review Medicaid has a statewide surveillance and utilization review program that safeguards against unnecessary utilization of care and services and excessive payments. It provides for the control of the utilization of all services provided under the plan and assesses the quality of those services. 2.1.8.1. Provider Program Abuse The Medicaid Program Integrity Unit (MPIU) conducts reviews and investigations to determine whether or not a provider is incorrectly Medicaid. The MPIU also conducts random studies of provider payment histories to detect billing errors and over-utilization. They perform on-site visits and obtain records to verify that services billed correspond to services rendered to participants. Once services are reviewed, issues may be resolved by provider education or policy revision, recovery of funds from the provider, and/or assessment of civil monetary penalties. In more serious cases, the Department can take any of the following actions. • Suspend payment pending further investigation. • Terminate provider numbers. • Exclude entities/individuals. • Refer individuals/providers for criminal prosecution. If you believe that a particular Medicaid provider is abusing the program, you may contact: Medicaid Program Integrity Unit PO Box 83720 Boise, Idaho 83720-0036 [email protected] Fax 1(208) 334-2026 January 29, 2015 Page 10 of 59 Idaho MMIS Provider Handbook General Provider and Participant Information 2.2. Services for Providers 2.2.1. Overview Molina Medicaid Solutions is the fiscal agent for the Idaho Medicaid Program. The primary objective for Molina is to process Medicaid claims efficiently and accurately for Idaho Medicaid providers. The Molina Provider Enrollment Department enrolls providers into the Idaho Medicaid Program and responds to providers’ requests for information not currently available through Idaho’s Medicaid Automated Customer Service (MACS). The Molina Provider Services Department helps to keep providers up-to-date on billing changes required by program policy changes implemented by the Division of Medicaid and to answer any questions regarding claims and eligibility. 2.2.2. Idaho Medicaid Automated Customer Service (Idaho MACS) Medicaid Automated Customer Service (MACS) is the interactive voice response system (IVR) that allows a computer to recognize voice and telephone keypad inputs. MACS will allow users to access a database via a telephone touchtone keypad or by speech recognition, after which they can service their own inquiries by following the instructions. MACS will respond with pre-recorded audio to further direct users on how to proceed. MACS can be used to control almost any function where the system can be broken down into a series of simple menu choices. The following table shows the information available through MACS. The phone number for MACS is 1 (866) 686-4272. Figure 2-1: Information Available Through MACS Claims Information Claim status Procedure code coverage PA required for procedure code Units remaining Revenue code coverage PA required for revenue code Diagnosis code coverage January 29, 2015 Last Payment Amount Amount and date of payment Number of claims paid Warrant/EFT number Mailing Addresses Paper claims Participant Information Copay/Deductible ResHab/PCS PA Eligibility Medical or Surgical PA Dental PA DME PA HC enrollment and referrals Lock-In Other Insurance/TPLs Prior Authorizations Service Limits Inpatient or Outpatient PA Transportation PA All other PAs Web Portal address Handbook CD request Security Code Create a new code Change an existing code Health Home Page 11 of 59 Idaho MMIS Provider Handbook 2.2.3. General Provider and Participant Information Provider Enrollment Idaho Medicaid enrolls two types of providers, billing and non-billing. 2.2.3.1. Non-billing Ordering and Referring Providers Providers who enroll as non-billing entities are enrolling for the sole purpose of ordering services/items for use by Medicaid participants or referring participants to another provider. Federal Regulations (42 CFR 455.410) require the enrollment of all non-billing physicians and practitioners. The regulation also requires the inclusion of the ordering/referring provider on the billing provider’s claim for reimbursement. Medicaid has established a streamlined process to enroll non-billing individuals whose only relationship with the Idaho Medicaid program is to refer for specialized care or order items or services. This enrollment method is not for individuals who want to submit claims to Idaho Medicaid for reimbursement for their services. For more information refer to this document. 2.2.3.2. Billing Providers Medicaid works with Molina Provider Enrollment to promptly and accurately enroll new providers in the Idaho Medicaid Program. This team effort ensures efficient Medicaid provider enrollment and claims processing for services rendered to Medicaid participants. The entities that participate in provider enrollment are: • Medical Care Unit • Bureau of Developmental Disability (DD) Services • Bureau of Long-Term Care • Bureau of Facility Standards • Licensure and Certification • Regional Medicaid Services (RMS) (all regions) • Mental Health and Substance Abuse • Pharmacy Unit • Family and Community Services (all regions) • Developmental Disabilities (DD) Program (all regions) • Healthy Connections (HC) • Idaho Medicaid Health Home (IMHH) • Molina • Office of Medicaid System Support Team (MSST) To become an approved Medicaid provider, a credentials investigation is conducted using the enrollment information. After the provider is approved for participation in the Idaho Medicaid Program, a unique provider number is assigned to providers without an NPI. For providers that enroll with an NPI, the NPI becomes the provider number. 2.2.3.3. Provider File Updates After enrolling, any updates that need to be made to the provider file can be done through the online portal at the Molina Medicaid Website. Once on the home page, click on the Provider Enrollment link and choose either Provider Maintenance-Demographic or Provider January 29, 2015 Page 12 of 59 Idaho MMIS Provider Handbook General Provider and Participant Information Maintenance (Full) to electronically maintain your provider record. If you are unable to make updates via the online portal, providers must notify Provider Enrollment, in writing, when there are changes in their status. The written notice must include the provider name and current NPI or Medicaid provider number. Status • • • • • • • • changes include: Change in address (or change in any other provider’s address, if a group practices) New phone number Name change (individual, group practice, etc.) Change in ownership Change in tax identification information Change in provider status (voluntary inactive, retired, etc.) must be written notification Add/update/end date of rendering providers Add/update/end date of service locations Figure 2-2: Provider File Updates Provider Maintenance Screen: Business Information Update the FEIN Update the Name Check the box to update the provider name Screen: Pay-To Address Update the Pay-To Physical Address Update the Pay-To Correspondence Mailing Address Update W-9 Information Update the Type of Tax Entity Update the Exempt Payee Status Update Sanctions (Individual only) Screen: Ownership Update and Add Owners & Board Members Update the Owner/Board Member Type Update the Owner/Board Member Address Info Update Sanctions Screen: Owner Relationship Update Relationship to Owner/Board Members Add Owner/Board Relationships Add Ownership or Control Interest Information Screen: Service Location Summary Add Service Location Terminate a Service Location Change Site Name Screen: Service Location Address No updates available January 29, 2015 Provider Maintenance–Demographic Screen: Business Information Update Office Contact Information Phone Numbers Fax Number Gender (Individual only) Screen: Pay-To Address No updates available Screen: Ownership No updates available Screen: Owner Relationship No updates available Screen: Service Location Summary Edit Site Information Screen: Service Location Address Update physical address phone number Update additional Languages Spoken Update Office Hours Update other Office Information Page 13 of 59 Idaho MMIS Provider Handbook Provider Maintenance Screen: Service Location Provider Type and Specialty (PTSP) Add/Update Specialties Add/Update Specialty Details Screen: PCCM Information Update Service Location Details Update Other Restrictions Update Special Accommodations Update After Hours Coverage Update After Hours Phone Number Update NPI/Medicaid IDs of covering Medicaid Providers Screen: Financial Agreement Update routing of payments automatically Update the Account Details Terminate current banking information Screen: Documentation Provider Agreement Enrollment Application Acknowledgement W9 Ownership & Conviction Signature on File Authorization for Electronic Funds Transfer (if necessary) Staff Affiliation Roster (if necessary) Group Affiliation Roster (if necessary) Driver Roster (if necessary) Vehicle Roster (if necessary) General Provider and Participant Information Provider Maintenance–Demographic Screen: Service Location Provider Type and Specialty (PTSP) No updates available Screen: PCCM Information No updates available Screen: Financial Agreement No updates available Screen: Documentation No updates available Note: The postal service will not forward mail or checks. All mail and checks will be returned to Molina. To apply for additional provider numbers, contact Molina Provider Enrollment. 2.2.4. Provider Service Representatives (PSRs) Molina provider service representatives are trained to promptly and accurately respond to requests for information on: • Adjustments • Billing instructions • Claim status • Participants benefit information • Participant eligibility information • Form requests • Payment information • Provider participation status information • Recoupments • Third party recovery information January 29, 2015 Page 14 of 59 Idaho MMIS Provider Handbook General Provider and Participant Information Provider Service Representatives To contact a Molina Provider Service Representative, call MACS at 1 (208) 373-1424 or 1 (866) 686-4272, and say representative or rep. Provider service representatives are available Monday through Friday from 7 A.M. to 7 P.M. Mountain Time. When calling a Provider Service Representative for questions about claims status, please have the following information ready. • Billing provider’s Idaho Medicaid provider number • Participant’s Medicaid identification number • Date(s) of service When • • • calling for questions about participant eligibility, have the following information ready. Billing provider’s Idaho Medicaid identification number Participant’s first and last name Participant’s Medicaid identification number, date of birth, or Social Security number 2.2.4.1. Provider Handbooks Providers can access an electronic copy of the Idaho Medicaid Provider Handbook from the Molina Medicaid website. The Idaho Medicaid Provider Handbook is updated periodically. These updates are designed to keep providers informed of program changes and provide billing instructions. Printed and CD copies of the provider handbook are always considered out of date. The most current version of the handbook is always available online. The provider handbook is intended to provide basic program guidelines, however, in any case where the guidelines appear to contradict relevant provisions of the Idaho Code or rules, the code or rules prevail. 2.2.4.2. Online Billing and Eligibility Verification For information regarding online billing and eligibility verification, refer to Provider-Trading Partner User Guides found online in the User Guides or request a paper copy from Provider Services. 2.2.5. Provider Relations Consultants (PRC) Molina Provider Relations Consultants help keep providers up-to-date on billing changes required by program policy changes implemented by the Division of Medicaid. Provider Relations Consultants accomplish this by: • Conducting provider workshops. • Conducting live meetings for training. • Visiting a provider’s site to conduct training. • Assisting providers with electronic claims submission. See the Provider Handbook Directory for telephone, fax, and addresses of the Provider Relations Consultants. January 29, 2015 Page 15 of 59 Idaho MMIS Provider Handbook General Provider and Participant Information 2.3. Participant Eligibility 2.3.1. Overview Medicaid is a medical assistance program that is jointly funded by the federal and state governments to assist in providing medical care to individuals and families meeting eligibility requirements. Income, resources, and assets are taken into consideration when determining Medicaid eligibility. 2.3.1.1. Eligibility Requirements Applicants for Medicaid must meet each of the financial and non-financial requirements of the program in which they will participate. The Medicaid field offices determine Medicaid eligibility and enroll eligible applicants in the appropriate benefit package. See Section 2.3.3 Covered Benefits, for more information. 2.3.1.2. Period of Eligibility Participant eligibility is determined on a month-to-month basis. For example, a participant may be eligible during the months of April and June, but ineligible during May. It is strongly recommended that prior to providing services, participant eligibility be verified by using MACS or the Molina Medicaid website. Medicaid only reimburses for services rendered while the participant is eligible for Medicaid benefits. Confirmation of eligibility is not available for dates in the future. See Section 2.3.5 Verifying Participant Eligibility. 2.3.2. Medicaid Identification Card Figure 2-3: Health Card An identification card is issued when the participant is determined eligible for Medicaid benefits. All Medicaid participants, except otherwise ineligible non-citizens or presumptive eligibility (PE) participants, receive an identification card. Possession of a Medicaid ID card does not guarantee Medicaid eligibility. Providers should request the Medicaid ID card with additional picture identification and retain copies of this documentation for their records. The participant’s Medicaid identification (MID) number is on the card. Cards issued after June 1, 2010 are a 10-digit number with no letters or symbols. Cards issued prior to June 1, 2010 are seven digits. January 29, 2015 Page 16 of 59 Idaho MMIS Provider Handbook 2.3.2.1. General Provider and Participant Information Medicaid Exception for Inmates Medicaid benefits are not available for inmates of government jail or prison facilities, unless the inmate becomes an inpatient in a medical institution. In that case, Medicaid coverage begins the day the inmate is admitted and ends the day of discharge from the medical institution. The inmate must also meet all other Medicaid eligibility requirements during the inpatient period. 2.3.3. Covered Benefits General information on services covered under the Idaho Medicaid Program are listed in the booklet, Idaho Health Plan Coverage, which is available in English and Spanish from the Division of Medicaid, Department Regional Offices, or online. See the Provider Guidelines for specific service coverage and billing details for individual programs and specialties. The guidelines are available online in the Provider Handbook. 2.3.4. Tamper Resistant Prescription Requirements To comply with federal regulations, Idaho Medicaid will only pay for outpatient drugs reimbursed on a fee-for-service basis when the prescription for the covered drug is tamperresistant. If Medicaid pays for the drug on a fee-for-service basis, and the prescription cannot be faxed, phoned, or electronically sent to the pharmacy, then providers must ensure that the prescription meets all three requirements for tamper-resistant paper. Any written prescription presented to a pharmacy for a Medicaid participant must be written on a tamper-resistant prescription form that contains all of the following: • One or more industry-recognized features designed to prevent unauthorized copying of a completed or blank prescription form. • One or more industry-recognized features designed to prevent the erasure or modification of information written on the prescription by the prescriber. • One or more industry-recognized features designed to prevent the use of counterfeit prescription forms. Note: The intent of this requirement is to reduce forged and altered prescriptions and to deter drug abuse. Emergency fills for prescriptions written on non-tamper resistant pads are permitted as long as the prescriber provides a verbal, faxed, electronic, or compliant written prescription within 72 hours after the date on which the prescription was filled. In an emergency situation, this allows a pharmacy to telephone a prescriber to obtain a verbal order for a prescription written on a non-compliant prescription pad. The pharmacy must document the call on the face of the written prescription. 2.3.4.1. Medicaid Non-Covered Services Prior to rendering services, providers must inform participants when services are not covered under Medicaid. Idaho Medicaid strongly encourages the provider to have the participant sign an informed consent regarding any non-covered services. If the participant chooses to obtain services not covered by Medicaid, it is the participant’s responsibility to pay for the services. See Section 2.1.2 Provider Responsibilities for additional details. January 29, 2015 Page 17 of 59 Idaho MMIS Provider Handbook 2.3.5. General Provider and Participant Information Verifying Participant Eligibility Providers should verify eligibility on the actual date of service, prior to providing the service. Eligibility information can be accessed three different ways. • Molina Medicaid website • MACS 1 (866) 686-4272 • HIPAA compliant vendor software (tested with Molina) To obtain eligibility information from one of these systems, submit either the MID number or two participant identifiers from the following list. • Social Security number (SSN) • Last name, first name • Date of birth Participant eligibility information available includes eligibility dates, Healthy Connections (HC) and Idaho Medicaid Health Home enrollment data, Medicaid special program limitations, certain service limitations, procedure code inquiries, third party recovery (TPR), Medicare coverage information, co-payments, and lock-in data. 2.3.5.1. Eligibility Verification Providers can verify eligibility by logging into their trading partner accounts on the Molina Medicaid website or using the MACS system. See the following paragraphs for additional information regarding eligibility verification using MACS. MACS Providers can use MACS to check participant eligibility. Eligibility information is available on • Healthy Connections Program • Idaho Medicaid Health Home Program • Eligibility with special programs • Service limits • Prior authorization (PA) • Co-payments • Other health coverage MACS informs providers of the type of Medicaid benefits a participant is eligible for on the dates of service. Participants who are eligible for the full range of Medicaid services have their benefit plans communicated as eligible for Medicaid benefits. Participants who are not eligible for the full range of Medicaid services have their restrictions reported according to their benefit plan. For example, if the participant is eligible for the Medicaid Basic Plan, their eligibility is communicated as eligible for basic Medicaid benefits, and only benefits restricted to the basic plan are communicated. The benefit plans for Presumptive Eligibility (PE), Pregnant Women (PW), Lock-in, and Copay remain unchanged and the restrictions for participants on these plans are communicated accordingly. January 29, 2015 Page 18 of 59 Idaho MMIS Provider Handbook General Provider and Participant Information Vendor Supplied Software Providers may contract with a software vendor and use software supplied by the vendor. Software specifications can be found on the Molina Medicaid website by clicking on Companion Guides in the left menu. The specifications assist the vendor in duplicating the program requirements and allow providers to obtain the same information available as the Molina Medicaid website. All vendor software must successfully test with Molina before use. Providers can check eligibility using vendor software, if the software is modified to meet the requirements of the HIPAA ASC X12 270/271, version 4010A1 format, and if the vendor successfully tests the transactions with Molina. 2.3.6. Participant Program Abuse/Lock-In Program Medicaid reviews participant utilization to determine if services are being used at a frequency or amount that may result in a level harmful to the participant and to identify services that are not medically necessary. Abuse can include frequent use of emergency room facilities for non-emergent conditions, frequent use of multiple controlled substances, use of multiple prescribing physicians and/or pharmacies, excessive provider visits, overlapping prescription drugs with the same drug class, and drug seeking behavior as identified by a medical professional. To prevent abuse, Medicaid has implemented the participant lock-in program. Participants identified as abusing or over-utilizing the program may be limited to emergency services only, or the use of one physician/provider and one pharmacy. This prevents these participants from going from doctor to doctor, or from pharmacy to pharmacy, to obtain excessive services. If a provider suspects a Medicaid participant is demonstrating utilization patterns, which may be considered abusive, not medically necessary, potentially endangering the participant’s health and safety, or drug seeking behavior in obtaining prescription drugs, they should notify Medicaid of their concerns. Medicaid will review the participant’s medical history to determine if the participant is a candidate for the lock-in program. 2.3.6.1. Primary Care Physician (PCP) The PCP for lock-in participants is responsible for coordination of routine medical care and making referrals to specialists as necessary. The PCP explains to the lock-in participant all procedures to follow when the office is closed or when there is an urgent or emergency situation. This coordination of care and the participant’s knowledge of office procedures should help reduce the unnecessary use of the emergency room. If the participant needs to see a physician other than the PCP, the PCP gives the participant a referral to another physician or clinic to ensure payment. Referrals can be done electronically by logging into your secure webpage on the Molina Medicaid website and clicking on the Trading Partner tab. More information on the referral process can be found in the Referrals section of the Trading Partner Account (TPA) User Guide. This also applies to physicians covering for the PCP and emergency rooms for non-emergency care. The referred physician must contact the PCP for the Idaho Medicaid provider number and enter it on all claims. Note: If a PCP no longer wishes to provide services to the lock-in participant, the PCP must send a written notice to the participant stating the reasons for dismissal with a copy of the letter sent to the Health Resources Coordinator in your region. January 29, 2015 Page 19 of 59 Idaho MMIS Provider Handbook 2.3.6.2. General Provider and Participant Information Designated Pharmacy A designated pharmacy has the responsibility of monitoring the participant’s drug use pattern. The pharmacy should only fill prescriptions from the PCP or from referred physicians. Note: All referrals must be confirmed with the PCP before prescriptions are dispensed. 2.4. Benefit Plan Coverage 2.4.1. Medicaid Enhanced Plan The Medicaid Enhanced Plan includes all of the benefits found in the Medicaid Basic Plan, plus additional benefits to cover needs of people with disabilities or special health needs. Participants enrolled in this plan will be eligible for the full range of Medicaid covered services. 2.4.2. Medicaid Basic Plan 2.4.2.1. Overview The Medicaid Basic Plan has been designed to achieve and maintain wellness by emphasizing prevention and proactively managing health. 2.4.2.2. Covered Services Medical coverage under the Medicaid Basic Plan is limited with some notable differences between the Medicaid Enhanced Plan and Medicaid Basic Plan. 2.4.2.3. • • • • • • • • • Excluded Services Drugs not covered under Medicaid Rehabilitative services provided by a developmental disability (DD) facility Intermediate care facility (developmentally disabled)/intellectually disabled (ICF/ID) services Skilled nursing facility services Nursing facility services Hospice care services Case management services Personal care services Home and community based services 2.4.2.4. Restricted Services Mental health inpatient services are limited to ten days per calendar year, whether in a hospital or freestanding facility. Freestanding facilities are limited to individuals under the age of 22. 2.4.2.5. Third Party Recovery (TPR) Requirements All services must be billed to the participant’s other insurance before billing Medicaid. See General Billing Instructions, Third Party Recovery (TPR), for billing details. January 29, 2015 Page 20 of 59 Idaho MMIS Provider Handbook 2.4.2.6. General Provider and Participant Information Medical Necessity Under some circumstances, participants in the Medicaid Basic Plan with a medical necessity for enhanced services may be eligible for reassignment to the Medicaid Enhanced Plan. This determination will be a joint decision made by the appropriate units in the Welfare (Self Reliance) and Medicaid Divisions. 2.4.2.7. Billing Procedures Follow the same billing practices for any other Medicaid participant. 2.4.3. Presumptive Eligibility (PE) 2.4.3.1. Pregnant Women (PW) The program was developed as a result of the Federal Catastrophic Health Bill of 1988 to offer medical assistance to pregnant women. The program assists Idaho residents not currently receiving medical assistance from the state or county, and without sufficient resources for private medical coverage during their pregnancies. Presumptive eligibility provides immediate, presumed coverage for qualified candidates. The maximum coverage period is 45 days. During this time, the Presumptive Eligibility (PE) participant formally applies for another program offered under Medicaid. Medicaid determines if the pregnant woman is qualified for the Pregnant Women (PW) Program or another category of assistance. The goal of the program is to encourage pregnant women to seek prenatal care early in a pregnancy and preserve the health of both mother and infant. 2.4.3.2. Breast and Cervical Cancer Presumptive eligibility is also available for women who have been initially screened and diagnosed through the Centers for Disease Control and Prevention’s (CDC) National Breast and Cervical Cancer Early Detection Program (NBCCEDP). This program allows the state to provide Medicaid benefits to uninsured women between the ages of 40 and 65 when they are in need of treatment for breast or cervical cancer, including pre-cancerous conditions and early stage cancer. Certain criteria must be met in order to qualify. 2.4.3.3. Program Procedures The candidate seeking medical assistance for pregnancy must see an approved provider trained and certified by Medicaid, such as a health district or hospital. Additionally, providers qualified to perform PW PE determination must meet the eligibility criteria listed in Section 1920 of the Social Security Act. Potential PE candidates answer preliminary program questions from the provider to determine if they are eligible for the program. These qualifications are determined by federal guidelines. The PE candidate for the PW Program must have a medically verified pregnancy and have financial resources that fall within specific income levels. Eligibility for pregnancy services under the PE Program is determined as follows. January 29, 2015 Page 21 of 59 Idaho MMIS Provider Handbook • • • General Provider and Participant Information Participant and provider complete program questions and determine if the participant is eligible for the PE Program. Participant’s local field office receives the application for services from the provider, processes it, and issues a Medicaid number for participant’s PE eligibility period. Participant’s PE period ends after a maximum coverage period of 45 days or sooner if the candidate is eligible for PW or another Medicaid program. Follow these steps to submit your claims. 1. Verify the participant’s eligibility using Medicaid Automated Customer Service (MACS) or electronic software. See Section 2.3.5 Verifying Participant Eligibility, for instructions. 2. Submit your claim with the participant’s Medicaid identification (MID) number. The PE candidate for the Breast and Cervical Cancer Program must be screened through a local Women’s Health Check Office (usually the district health department) and test positive for a breast or cervical cancerous or pre-cancerous condition that requires treatment. 2.4.3.4. Covered Services Medical coverage for the PW Program during the PE period is restricted to ambulatory outpatient, pregnancy-related services only. Pregnancy related services may be rendered by any qualified Medicaid provider. Routine prenatal services are covered, as well as some additional services such as nutrition counseling, risk-reduction follow-up, and social service counseling. Providers are not required to bill another insurance resource, if it exists, before billing Medicaid for prenatal services during the PE period. Women having PE for the Breast and Cervical Cancer Program, at the time of service, are eligible for Medicaid benefits during the PE period. 2.4.3.5. Medical Necessity To bill PE services for the PW Program that are not clearly pregnancy-related, attach medical necessity documentation to a paper claim form explaining how the service is pregnancy-related. Services not clearly pregnancy-related will be denied, if documentation of medical necessity is not provided. If the PE participant is referred to the hospital for lab testing or x-rays and the services are not clearly pregnancy-related, give the participant a completed PW Medical Necessity form. The participant takes this form to the next provider to establish the service as pregnancyrelated. See Medical Necessity Form (pregnancy related). Forms are available online or as paper copies by request from Provider Services. 2.4.3.6. Excluded Services The PE Program does not cover PW inpatient services. Medicaid does not pay for any type of abortion for participants on the PE Program. Also, PE participants are not covered for any delivery services. Services not covered under Medicaid are the participant’s responsibility. If the PE participant has applied for the PW Program or any other Medicaid program, and is determined eligible, hospital inpatient services may be covered. No specific services are excluded for Breast and Cervical Cancer program participants. January 29, 2015 Page 22 of 59 Idaho MMIS Provider Handbook 2.4.4. Pregnant Women (PW) 2.4.4.1. Overview General Provider and Participant Information Medicaid offers extended eligibility and additional services to all women covered by Medicaid during their pregnancy and postpartum period. The Pregnant Women (PW) Program is for pregnancy-related services only and is available to pregnant women who meet the eligibility requirements. This coverage ends on the last day of the month in which the 60th day after delivery occurs. Medicaid developed the PW Program to help ensure that all women have access to prenatal and postpartum care. The ultimate goal is to ensure the health of mothers and infants. 2.4.4.2. Covered Services Medical coverage under PW is restricted to pregnancy-related services only. Normal prenatal services are covered, as well as some additional services such as nutrition counseling, risk reduction follow-up, and social service counseling. Pregnancy related services are those necessary for the health of the mother or fetus, or services that become necessary because of the pregnancy. Women who are eligible under the PW program are covered by a dental insurance program called Idaho Smiles. Contact Idaho Smiles Customer Service at 1 (800) 936-0978, or at www.bcidaho.com, and click on the Idaho Smiles link, for Idaho Smiles eligibility, benefits, and claims processing information. All family planning services normally covered under Medicaid, including sterilization, are covered under the PW Program. When billing for sterilization, all appropriate consent forms must be attached, along with documentation/justification that the service was performed during the two-month post-partum period. Family planning services are only covered during the postpartum period. The following table shows some examples. Figure 2-4: Example of PW Coverage Delivery Date 09/15/2010 12/02/2010 30 Days Postpartum 10/15/2010 01/01/2011 60 Days Postpartum 11/14/2010 01/31/2011 PW Coverage Ends 11/30/2010 01/31/2011 Note: A Healthy Connections referral is not required for family planning services, see Section 2.5.5.5. 2.4.4.3. Non-Covered Services Optical benefits are not normally covered as a part of the PW Program. An ophthalmologist or other physician must provide medical necessity documentation if billing for optical services that directly affect the pregnancy, or if the symptoms being treated are a direct result of the pregnancy. January 29, 2015 Page 23 of 59 Idaho MMIS Provider Handbook 2.4.4.4. General Provider and Participant Information Medical Necessity If the services are not clearly pregnancy-related, attach medical necessity documentation to the paper or electronic claim to explain how the service is pregnancy-related. The information from the medical necessity documentation will be used to determine if the service provided relates to the pregnancy. It is not a guarantee that the service will be reimbursed. Services not clearly pregnancy related will be denied if documentation of medical necessity is not provided. The Molina medical consultant reviews each claim on a case-by-case basis. Molina may deny a claim with the reason - This PW participant’s charge has been reviewed by the Molina medical consultant and denied. Medical Necessity Form A Medical Necessity form is available online at the Molina Medicaid website or as a paper copy by request from Provider Services. To request further review, write to the following address. Division of Medicaid Medical Care Unit PO Box 83720 Boise, ID 83720-0009 Fax: 1 (877) 314-8779 2.4.4.5. Excluded Services Excluded services include treatment that is not a direct result of, or does not directly affect, the pregnancy. 2.4.4.6. Billing Procedures Follow the same billing practices for a PW participant as for any other pregnant Medicaid participant. All services must be pregnancy-related. 2.4.5. Breast and Cervical Cancer 2.4.5.1. Program Policy A woman not otherwise eligible for Medicaid who meets certain conditions may be eligible for Medicaid benefits for the duration of her cancer treatment. 2.4.5.2. Eligibility In order to be eligible, the participant must be initially screened and diagnosed through a local Women’s Health Check Office (usually the district health department) as a representative of the Centers for Disease Control and Prevention. The participant can be presumed eligible before a formal Medicaid determination under PE as described in Section 2.4.3 Presumptive Eligibility (PE). Although Medicaid resource limits do not apply, the participant must: January 29, 2015 Page 24 of 59 Idaho MMIS Provider Handbook • • • • • • • • • • General Provider and Participant Information Meet the designated income limit. Be diagnosed with breast or cervical cancer through the Women’s Health Check Program. Be at least 40 years old and under the age of 65. Have no creditable insurance (if insured, the plan does not cover the same type of cancer). Be an Idaho resident. Provide a valid Social Security number. Be a U.S. citizen or meet requirement for legal non-citizen. Not reside in an ineligible institution. Not be fleeing prosecution of a felony, custody, or confinement of a felony conviction or violating a condition of probation or parole. Be willing to cooperate with Medicaid to secure medical or child support services, unless the participant has good cause. 2.4.5.3. Covered Services Women who qualify for this program are eligible for Medicaid benefits during the treatment phase of their cancer care. 2.4.5.4. Stages of Treatment Coverage for primary cancer treatment may include: • Medical and surgical services • Pre-cancerous conditions • Early stage cancer Adjuvant cancer treatment involving radiation or systemic chemotherapy included in the treatment plan, are also covered. 2.4.5.5. End of Treatment Cancer treatment ends when a participant’s plan of care reflects a status of surveillance, follow-up, or maintenance. Additionally, benefits will end if a participant’s treatment relies on an unproven procedure in lieu of primary or adjuvant treatment methods. 2.4.6. Medicare Savings Program 2.4.6.1. Program Policy The state has agreements with the Social Security Administration (SSA) and Centers for Medicare and Medicaid Services (CMS), which allows the state to enroll people in the Premium Hospital Insurance Program (also referred to as Premium HI or Medicare Part A) and the Supplementary Medical Insurance (also referred to as SMI or Medicare Part B). The agreements allow Medicaid participants who are entitled to Medicare to have their Part A and/or Part B Medicare premiums paid by Medicaid. Participants do not have to be 65 years old or older to be eligible for Medicare. The statutory authority for the Medicare Savings Program is §1843 of the Social Security Act and Medicare Catastrophic Act of 1988. The purpose of these arrangements is to permit the state to provide Medicare protection to certain groups of low income and disabled individuals as part of its total assistance plan. The arrangements transfer the partially state-funded medical costs for this population from Title XIX Medicaid Program to the Title XVIII Medicare Program, which is funded by the federal government and by payment of individual premiums. Federal Financial Participation January 29, 2015 Page 25 of 59 Idaho MMIS Provider Handbook General Provider and Participant Information (FFP) is available through the Medicaid Program to assist the states with the premium payment for certain groups of low income and disabled individuals. There are two types of Part A Medicare Savings Program participation. • Regular Type Part A • Qualified Disabled Working Individual (QDWI) Part A See the General Billing Instructions, Qualified Medicare Beneficiaries (QMB) Medicare/Medicaid Billing Information, for more information. 2.4.6.2. Part A Medicare Savings Program This program is for individuals who are not entitled to premium-free Medicare Part A benefits. These individuals must apply for Medicare with the Social Security Administration and be determined eligible for self-pay type Medicare. These individuals have a Medicare claim number with a Beneficiary Identification Code (BIC) of M. This code is found at the end of the Medicare claim number. Medicaid pays the Medicare Part A premium, coinsurance, and deductible only. 2.4.6.3. Qualified Disabled Working Individual (QDWI) Part A Medicare Savings Program Qualified Disabled Working Individual Program does not include state payment of Part B Medicare premiums. Individuals on the QDWI Program have lost Medicare Part A (HI) entitlement solely because of work, and are entitled to enroll in Part A Medicare under §1818A of the Social Security Act. Medicaid pays the Medicare premium, coinsurance, and deductible only. 2.4.6.4. Part B Medicare Savings Program There are several types of participation in the Part B Medicare Savings Program in Idaho. Figure 2-5: Part B Medicare Savings Program Participation Short Name Qualified Medicare Beneficiary QMB Qualified Medicare Beneficiary with Medicaid QMB+ (QMB Plus) Description Individual is entitled to Medicare and meets the income limits. Medicaid pays the Medicare premium, coinsurance, and deductible Individual is entitled to Medicare, meets income limits, and has open Medicaid eligibility. Medicaid pays the Medicare premium, coinsurance, and deductible up to the Medicaid eligible amount. Medicaid pays for Medicaid-allowed services and supplies not covered by Medicare. January 29, 2015 Page 26 of 59 Idaho MMIS Provider Handbook Participation Short Name Specified Low Income Medicare Beneficiary SLMB Specified Low Income Medicare Beneficiary with Medicaid eligibility SLMB+ (SLMB Plus) General Provider and Participant Information Description Individual is entitled to Medicare and is within income limits. Medicaid pays the Medicare premiums only. Individual is entitled to Medicare, within income limits and on Medicaid eligibility. Medicaid pays the Medicare premium, coinsurance, and deductible. Medicaid pays for Medicaid-allowed services and supplies not covered by Medicare. Medicaid (with deemed Cash Assistance Recipient) Individual is entitled to Medicare, within income limits and on Medicaid eligibility. Medicaid pays the Medicare premium, coinsurance, and deductible. Medicaid pays for Medicaid-allowed services and supplies not covered by Medicare. Medicaid – Non-Cash (also known as Medical Assistance Only) MAO Qualified Individual 1 QI1 2.4.6.5. Individual is entitled to Medicare, within income limits and on Medicaid eligibility. Medicaid pays the Medicare premium, up to the lower allowed amount for the medical service (Medicare/Medicaid). Medicaid pays for Medicaid-allowed services and supplies not covered by Medicare. Individual is entitled to Medicare and within income limits. Medicaid pays the Medicare premiums only. Dually Eligible Medicare Beneficiaries Individuals that are enrolled in Medicare and eligible for Medicaid are considered a dual eligible Participant. Dually eligible individuals are persons entitled to Medicare and eligible for Medicaid. Dually eligible individuals Participants are eligible for Medicare benefits (under Original Medicare) and Medicaid benefits under the Medicaid category of assistance programs for which the participant qualified for. Individuals that are enrolled in Medicare and eligible for Medicaid are considered a dually eligible participant. Dually eligible participants are eligible for Medicare benefits (under Original Medicare) and Medicaid benefits under the Medicaid category of assistance program(s) for which the participant qualified for. Dually eligible participants receive Medicare Part A and/or Part B premium coverage, and coinsurance and deductible reimbursement consideration for all Medicare covered services. Pharmacy items or other services not covered by the dually eligible participant’s Medicare benefits may be covered under the participant’s Medicaid benefits. January 29, 2015 Page 27 of 59 Idaho MMIS Provider Handbook 2.4.6.6. General Provider and Participant Information Medicare Part D Under the Medicare Modernization Act, dually eligible individuals will no longer receive their drug coverage from Medicaid and instead will select or be auto enrolled into private Medicare prescription drug plans. Medicaid may still cover certain essential drugs excluded by law from the Medicare Part D, Prescription Drug Program. Medicare must be billed prior to submitting drug claims to Medicaid. If the Medicare Explanation of Benefits (EOB) indicates that the requested medication is one of the medications not covered by law, then Medicaid may reimburse. 2.4.7. Medicare-Medicaid Coordinated Plan (MMCP) The Medicare-Medicaid Coordinated Plan (MMCP) integrates Medicare and Medicaid benefits for dually eligible participants that voluntarily enroll in MMCP through Blue Cross of Idaho (BCI) under its True Blue Special Needs Plan (SNP). 2.4.7.1. Program Overview The Medicare-Medicaid Coordinated Plan (MMCP) is only offered through Blue Cross of Idaho (BCI) under its True Blue Special Needs Plan (SNP). Participants that are 21 years old or older, enrolled in Medicare Part A and Part B, eligible for full Medicaid, and reside in an MMCP coverage area are eligible to voluntarily enroll in MMCP through BCI under its True Blue SNP. Medicaid’s MMCP benefits are integrated into BCI’s True Blue SNP, which is a Medicare Advantage plan. Beginning July 1, 2014, the following services will be added to the Blue Cross of Idaho True Blue Special Needs Plan. The following services must be billed to Blue Cross of Idaho. • Aged & Disabled (A&D) Waiver Services • Personal Care Services (PCS) • Developmental Disability (DD) Targeted Service Coordination only o Note: DD State Plan and DD Waiver services will continue to be provided through Medicaid • Nursing Home (NH) and Intermediate Care Facility/Intellectually Disabled (ICF/ID) Services • Community-Based Rehabilitation Services The Blue Cross of Idaho’s (BCI) True Blue Special Needs Plan (SNP) is designed to coordinate all health related services for Medicare and Medicaid including: • Hospital services • Medical services • Prescription drug services and • Behavioral health services 2.4.7.2. Medicaid Covered Services Participants enrolled in Medicare-Medicaid Coordinated Plan (MMCP) with Blue Cross of Idaho’s (BCI) Special Needs Plan (SNP) will continue to receive coverage through Medicaid for the following services. January 29, 2015 Page 28 of 59 Idaho MMIS Provider Handbook General Provider and Participant Information Adult • • • • • • • • • • • • • • • • • • • • • • • • • • • • • Developmental Disability (DD) Waiver Non-Medical Transportation provided by an Agency Non-Medical Transportation provided by an Individual Non-Medical Transportation provided through a Bus Pass Specialized Medical Equipment Individual Supported Living Group Supported Living Daily Supported Living Services Intense Support Daily Supported Living Services Intense Support School Based, School Days Daily Supported Living Services High Support Daily Supported Living Services High Support School Based, School Days Behavioral Consultation by a QIDP/Clinician Behavioral Consultation by a Psychiatrist Behavioral Consultation Emergency Intervention Technician Supported Employment Adult Day Health Chore Services (Skilled) Residential Habilitation – CFH Personal Emergency Response System Installation and first month’s rent Personal Emergency Response System Rent/monthly Environmental Accessibility Adaptations Home Delivered Meals Skilled Nursing Services, Independent RN Skilled Nursing Services, Agency LPN Skilled Nursing Services, Agency RN Nursing Oversight Services of LPN Nursing Oversight Services of Agency RN Nursing Oversight Services of Independent RN Respite Care Respite Care Daily Adult • • • • • • DD State Plan HCBS Developmental Therapy Evaluation Home/Community Individual and/or Group Developmental Therapy for Adults Center Based Individual and/or Group Developmental Therapy for Adults Community Crisis Supports Interpretive Services oral (to assist Enrollees to receive DD services) Interpretive Services sign language (to assist Enrollees to receive DD services) Consumer Directed Services • Fiscal Employer Agent • Community Supports (to include Support Broker services) 2.4.7.3. Participant Identification Number Participants enrolled in MMCP, will continue to use his/her Medicaid I.D. (MID) number as established under Section 2.3 Participant Eligibility. Participating Medicare Advantage Plans offering MMCP will also issue a plan identification number specific to their company. Currently, Blue Cross of Idaho (BCI) is the only vendor offering MMCP under its integrated True Blue Special Needs Plan (SNP), which is a Medicare Advantage Plan. January 29, 2015 Page 29 of 59 Idaho MMIS Provider Handbook 2.4.7.4. General Provider and Participant Information Billing Procedures For Participants enrolled in MMCP, providers may bill Medicaid for services listed below using the Medicaid I.D. (MID) number assigned to the Participant. • Adult DD Waiver Services • Adult DD State Plan HCBS • Consumer Directed Services For all other services, the Provider must bill the MMCP vendor which is currently Blue Cross of Idaho (BCI). When billing the MMCP vendor, be sure to follow the MMCP vendor’s billing requirements. Claims will be processed per the MMCP vendor’s rules and guidelines. The MMCP vendor can bill the participant for service items that are not covered under the MMCP vendor’s evidence of coverage and/or not covered by Medicaid. 2.4.8. Otherwise Ineligible Non-citizens (OINC) 2.4.8.1. Overview Individuals who do not meet the citizenship or qualified non-citizen requirements may be eligible for medical services necessary to treat an emergency medical condition. An emergency medical condition exists when the condition could reasonably be expected to seriously harm the person’s health, cause serious impairment to bodily functions, or cause serious dysfunction to any body part or organ, without immediate medical attention. 2.4.8.2. Eligibility Medicaid eligibility for OINC begins no earlier than the date the participant experiences the medical emergency and ends the date the emergency condition stops. The Division of Medicaid, Medical Care Unit determines the beginning and ending dates of eligibility. 2.4.8.3. Covered Services Obstetrical deliveries are considered emergencies. However, ante partum and postpartum care are not considered to be emergencies. The Division of Medicaid, Medical Care Unit reviews each request for payment for OINC and determines if a medical condition is an emergency. 2.5. Healthy Connections (HC) 2.5.1. Overview Healthy Connections (HC) helps Medicaid participants receive the care they need, when they need it, and at the appropriate place. The assurance of a familiar, consistent doctor and patient relationship creates a medical home. This is where participants receive the preventive and other basic health care needed to help promote good health. The goals of HC are to: • Ensure access to healthcare. • Promote and protect the health of Medicaid participants. • Emphasize continuity of care. • Provide health education. • Achieve cost efficiencies for the Idaho Medicaid Program. January 29, 2015 Page 30 of 59 Idaho MMIS Provider Handbook General Provider and Participant Information Medicaid participant enrollment into HC is required in the majority of counties statewide. Individuals applying for Idaho Medicaid are asked to identify their current Primary Care Provider (PCP) or choose an HC PCP. Providers who render services that require a referral must obtain the referral from the participant’s HC PCP. 2.5.2. Importance of Verifying Medicaid Eligibility and HC/IMHH Enrollment Medicaid providers should always verify participant eligibility and Healthy Connections or Health Home enrollment prior to rendering services, as described in Section 2.3.5 Verifying Participant Eligibility. If a Healthy Connections or Idaho Medicaid Health Home PCP is not indicated, a referral is not required. Note: When verifying eligibility, if a participant is enrolled in the Idaho Medicaid Health Home Program (IMHH), please refer to Section 2.6 Idaho Medicaid Health Home for program information. 2.5.3. Provider Enrollment Idaho Medicaid primary care providers participate in Healthy Connections by signing a Coordinated Care Provider Agreement. This is in addition to the Idaho Medicaid Provider Agreement. Coordinated Care Provider Agreements are available from the Regional Health Resources Coordinators (HRC). Addresses and telephone numbers for the regional HC offices are listed in the Directory of this provider handbook, as well as on our HC website at www.healthyconnections.idaho.gov. Healthy Connections PCPs agree to do the following. • Provide timely access to primary and preventive care services. • Exercise best efforts to monitor and manage the participant’s care. • Provide 24-hour telephone access to a medical professional. • Make timely referrals for medically necessary services not provided by the HC PCP. • Enroll all rendering PCPs and each HC service location in the MMIS system for the purposes of assigning participants at the location where they receive primary care services. • Keep all of the provider enrollment information current in the MMIS system by completing any maintenance items within 30 days of the change as required in the Idaho Medicaid Provider Agreement. 2.5.3.1. Healthy Connections Case Management Payment In addition to payment for services rendered, PCPs enrolled in the HC Program are paid a monthly case management fee. This monthly case management fee is based upon the number of HC Medicaid participants enrolled in the practice during a calendar month, regardless of whether or not the participant is seen during that month. The fee payment is as follows. January 29, 2015 Page 31 of 59 Idaho MMIS Provider Handbook • • • • General Provider and Participant Information Case Management payment is generally processed on the first Saturday of the month, resulting in the Healthy Connections rosters available the Monday or Tuesday following the Case Management processing. $2.50 per member per month for enrollees in the Basic Benefit Plan. $3.00 per member per month for enrollees in the Enhanced Benefit Plan. The fee is increased by 50 cents per member per month when the Healthy Connections provider’s office offers extended hours of service to see patients equal to or greater than 46 hours per week. o The incentive payment may also be paid for a service location that does not offer extended hours, but is within a Healthy Connections provider organization that has a nearby location that offers extended hours. The nearby location must utilize electronic health records to coordinate care across locations. HC PCP will contact the HC Team to request the incentive payment under these conditions. The form to submit this request can be found on the Molina Medicaid website under the forms section. 2.5.3.2. Healthy Connections Participant Rosters The following two Primary Care rosters are available to PCPs. • An online Primary Care Roster is available on the Molina Medicaid website through your Trading Partner Account. This is a list of currently enrolled HC participants. • The Monthly Healthy Connections Roster is a list of participants enrolled to a Healthy Connections PCP or service location effective the first day of the month, including the case management payment information. For providers with a Trading Partner Account (TPA) and receiving an electronic remittance advice (RA), this monthly roster is uploaded to their secure portal under the ‘Reports’ section and is available in both PDF and Excel formats. For PCPs not receiving electronic RAs, this roster report is mailed. • An announcement will be posted to the Molina Health PAS website when the rosters become available. 2.5.3.3 Primary Care Provider Listing A listing of HC PCPs, sorted by Region and County, is made available on the HC website to participants and providers. To ensure that the HC PCP listing is current and accurate, it is imperative that any time there is a change to a provider’s record or the clinic’s record that you submit those updates to Molina Provider Enrollment. Failure to keep the provider records up to date could result in not only inaccurate information on the HC PCP listing but also non-payment of claims. Some • • • • • common changes or updates could include: Change of ownership Change of address or phone number Adding or closing a service location Adding or removing rendering providers Change in whether or not a clinic is open to new Medicaid patients Please refer to Section 2.2.3.3 Provider File Updates for more provider enrollment information. 2.5.4. Participant Enrollment Medicaid providers should always verify participant eligibility and Healthy Connections enrollment prior to rendering services, as described in Section 2.3.5 Verifying Participant January 29, 2015 Page 32 of 59 Idaho MMIS Provider Handbook General Provider and Participant Information Eligibility. For participants enrolled in Healthy Connections, the PCP information will be provided through the automated and/or online system. If an HC PCP is not indicated, an HC referral is not required. Enrollment in HC is mandatory for most Medicaid participants and required in the majority of counties statewide. Medicaid eligible participants not enrolled in HC are mailed an enrollment form and given up to 30 days to inform us of their choice of PCP. When a Medicaid participant does not choose a PCP and they live in a mandatory county, the participant is assigned to an HC PCP. 2.5.4.1. Enrollment in Healthy Connections If a participant is not enrolled with your clinic, please have them complete an enrollment form at your clinic and fax it to HC at 1 (888) 532-0014 or e-mail to [email protected]. Enrolling participants at your clinic will help avoid the possibility of them being assigned to a different HC clinic and will help ensure your clinic receives the case management fee. Enrollment in HC is prospective. Enrollment start dates are as follows: • For members currently enrolled in Open Access, Healthy Connections enrollment will always begin the first day of the following month. • For members currently enrolled in Healthy Connections and changing to a different Healthy Connections provider, enrollment will usually become effective the date the request is received. The request to change a PCP must be received via fax, secure email, or phone call prior to rendering services When a change in PCP is requested during the Department’s non-business hours, such as weekends or holidays, the current enrollment will be termed one day prior to the date the request was received and the new enrollment will be effective the next business day. • The request to change a participant’s PCP can be made by the following: o Participant or a family member on the case who has the authority to request the change. o The participant’s provider sending an enrollment form or calling on behalf of the patient. o DHW staff contacting HC on behalf of foster child in state custody. • For members currently enrolled in one benefit plan, such as Healthy Connections, who enroll in a different benefit plan, such as Idaho Medicaid Health Home, the change in enrollment will always occur on the first of the following month. • A request to change a participant’s PCP must be mutually agreed upon by the provider and participant. The request indicates the provider accepts responsibility as the PCP and the change is not intended to facilitate access to urgent care. Failure to adhere to these policies may result in further investigation by the Medicaid Program Integrity Unit. Each enrolled participant is sent a written notice listing the name, phone number, and address of their HC PCP. This notice is generated and mailed the day after the participant’s enrollment is entered. Medicaid participants may choose an HC PCP in one of the following ways. • Complete and return an HC Enrollment form received in the mail. • Complete an HC Enrollment form at the PCP’s clinic. The clinic then faxes it to the Healthy Connections Consolidated Unit at 1 (888) 532-0014. • Call the HC Consolidated Unit at 1 (888) 528-5861 to enroll over the phone. January 29, 2015 Page 33 of 59 Idaho MMIS Provider Handbook General Provider and Participant Information Family participants are not required to choose the same HC PCP. If a participant requires assistance in choosing an HC PCP, the Healthy Connections staff can be contacted to provide information regarding available PCPs. Enrollment in HC is mandatory for most Medicaid participants. 2.5.4.2. Exceptions & Exemptions to HC Enrollment Participants meeting the following exemption or exception criteria are not required to enroll in the Healthy Connections Program. • Has an existing relationship with a primary care provider or clinic who is not participating in Healthy Connections; or a participant chooses a non-participating OB provider. • Has an eligibility period that is less than three (3) months. • Has an eligibility period that is only retroactive. • Is eligible only as a Qualified Medicare Beneficiary. • Is enrolled in the Medicare/Medicaid Coordinated Care Plan. • Resides in long-term care or ICF/ID facility. • Resides in a non-mandatory county where there are not an adequate number of providers to deliver primary care case management services. • Is unable to access a Healthy Connections provider within a distance of thirty (30) miles or within thirty (30) minutes to obtain primary care services. 2.5.4.3. Mandatory Enrollment in Healthy Connections Assignment to an HC PCP occurs for participants residing in a mandatory county that do not respond to the request to choose a PCP. The following criteria are used in completing mandatory assignments. • Assign participants to a PCP where they are currently receiving care. • Assign family members to a PCP where other family members are enrolled, if appropriate. • Assign participants to prior Healthy Connections PCP, when applicable. • Assign members to a PCP based on geographic location. • Assign members based on rotation schedule agreed upon by PCPs. 2.5.4.4. Participant Disenrollment by the Provider A PCP may choose to withdraw as the participant’s primary care provider and must give written notice to both the participant and the Department at least (30) days prior to the date of disenrollment. The Department may waive this notice on a case-by-case basis. The written notice from the PCP must give the enrollee the reason for the request for disenrollment. A PCP • • • • • may The The The The The request disenrollment of an enrollee because: enrollee fails to follow treatment plan. enrollee misses appointments without notifying provider. enrollee/PCP relationship is not mutually acceptable. enrollee’s condition would be better treated by another provider. PCP has moved and/or is no longer in business. A PCP may not request disenrollment because: January 29, 2015 Page 34 of 59 Idaho MMIS Provider Handbook • • • • General Provider and Participant Information There is a change in the enrollee’s health status. The enrollee’s over/under utilization of medical services. Diminished mental capacity. Uncooperative or disruptive behavior resulting from his/her special needs, except where his/her continued enrollment with the PCP seriously impairs the PCP’s ability to furnish services either to the enrollee or other enrollees (patients). Upon the reassignment of the participant to a new PCP, the former PCP must transfer a copy of the participant’s medical records to the new PCP when requested by the participant. 2.5.5. Referrals A referral is a documented communication from a participant’s PCP of record to another Medicaid provider authorizing specific covered services. 2.5.5.1. General Guidelines The participant’s PCP of record is responsible for providing primary care, managing the participant’s care, and making referrals for medically necessary services. A referral is required prior to delivery of care. Backdated or retroactive referrals are not acceptable. A PCP may delegate referral authority for the purposes of access to care, care coordination, or when covering for other Healthy Connections providers. Referral authority must be included in the referral documentation of the covering provider for the specific visit. A participant may access medically necessary services without a referral at any primary care location within the organization they are enrolled to, at the discretion of the PCP. Providers who receive referrals should communicate their assessment, recommendations, or progress back to the HC PCP of record. 2.5.5.2. Referral Requirements Following are the required core referral elements (Effective 6/1/2014): • Date issued • Referred to provider • Start date of the referral • Primary care provider issuing referral • End date of the referral (not to exceed one year) • Number of visits – if applicable • Diagnosis and/or Condition • Referral reason: o Evaluate and treat, may include surgery o Assume care o DME o Other • Referral limits or restrictions – if applicable January 29, 2015 Page 35 of 59 Idaho MMIS Provider Handbook General Provider and Participant Information Note: • Referrals remain active and do not expire if a participant changes their enrollment with a PCP clinic. • To be considered valid, a referral must be documented in both the refer-from and refer-to provider records. • A referral may be passed on to another Medicaid provider to treat the condition indicated in the original referral. • A referral is not required for DME when the following conditions are met: o When DME is included as part of the discharge plan after an inpatient stay for which a referral is on file o When DME is included as part of the discharge plan after an ER visit (Effective 6/1/2014) 2.5.5.3. Method of Referral A referral is a PCP’s authorization for services from another Medicaid Provider and may be communicated by any of the following methods: • Electronic referral (Electronic Health Record or online) • Referral Form (HC referral form, prescription pad, admit orders, etc.) • Verbal (calling orders to a specialist, i.e. hospital admit ordering DME by PCP) For documentation, all referrals must include the core elements of a referral, as specified in Section 2.5.5.2 Referral Requirements, and must be documented in both the referred from and referred to patient records or entered online. 2.5.5.4. Advantages of Electronic Online Referrals There are many advantages to submitting an online electronic referral, including: • Improved Accessibility & Communication of Data - The PCP, referred to provider, and Department staff can access the referral online anytime. • Enhanced Capacity – Resource for PCP to provide better-coordinated care by having access to participant referrals entered online. • Integrity - Authorized visits and/or date span of specified services are clear and concise. • Secure - HIPAA compliant referral process. • Referral Data - Electronic referrals meet documentation requirements for the primary care and referred-to providers; referral data trends and patterns will be available in the future. • Timesaver - No handling a paper referral. Refer to the Referrals section of the Trading Partner Account (TPA) User Guide, found in the User Guides under the Reference Section on the Molina Medicaid website, for instructions to enter or retrieve online referrals. 2.5.5.5. Services Not Requiring a HC PCP Referral The following services do not require a referral by the PCP. Services must be a covered service under the participant’s benefit plan. If the service is not on this list, it must have a referral. January 29, 2015 Page 36 of 59 Idaho MMIS Provider Handbook • • • • • • • • • • • • • • • • General Provider and Participant Information Anesthesiology Services Audiology Services o Performed in the office of a certified audiologist. Children’s Developmental Disabilities Services o Managed by the Department or the Department’s designee (effective 9/1/13). Chiropractic Services o Performed in the office of the chiropractor. Dental Services o All dental services are exempt from referral. Pre-operative examinations for procedures performed in an inpatient-outpatient hospital setting or ambulatory surgical center setting should be performed by the PCP when possible. Otherwise, the exam requires a referral. Dental procedures may require PA. Emergency Services o Treatment for emergency medical condition when the definition is met as outlined in IDAPA 16.03.09.10.23 (effective 1/1/13). Family Planning Services o Specific items covered are diagnosis, treatment, contraceptive supplies, related counseling and restricted sterilization for pregnancy prevention. Hospital Admissions Subsequent to ER Visit o Hospital admission subsequent to emergency care when the patient is discharged in coordination with their PCP (effective 1/1/13). Immunizations o Immunizations do not require a referral or an office visit. o Specialty physician and providers administering immunizations are asked to either provide the participant's PCP with immunization records, or to record administered immunizations in the Idaho Immunization Registry and Information System (IRIS) to assure continuity of care and avoid duplication of services. Intermediate Care Facility/Intellectually Disabled (ICF/ID) (Developmentally Disabled) Services o These services are only covered for Medicaid Enhanced Plan participants. Indian Health Clinic Services Infant Toddler Program Services o Managed by the Department or the Department’s designee (effective 9/1/13). Influenza Shots o Providers administering influenza shots are asked either to provide the participant’s PCP with documentation of the shot, or to record the immunization in the Idaho Immunization Registry and Information system to assure continuity of care and avoid duplication of services. Laboratory Services (includes pathology) Outpatient Mental Health Services o Outpatient services managed by the Department or the Department’s designee (effective 9/1/13). Note: Mental Health Services not coordinated by the Department’s Behavioral Health Managed Care Contractor, Optum Idaho, and billed directly to Molina do require a Healthy Connections referral. For example, a referral would be required for a psychiatrist billing Molina directly for physician services provided to a participant with a behavioral health diagnosis. Nursing Facility Services o These services are only covered for Medicaid Enhanced Plan participants. Personal Care Services (PCS) o These services are only covered for Medicaid Enhanced Plan participants. January 29, 2015 Page 37 of 59 Idaho MMIS Provider Handbook • • • • • • • • • • • • • • PCS Case Management o These services are only covered for Medicaid Enhanced Plan participants. Pharmacy Services o For prescription drugs only. Podiatry Services o Performed in the office. Pregnancy Related Services o Pregnancy related services, provided to HC participants, are to be coordinated with their primary care providers (effective 1/1/13). Radiology Services School District Services o Includes all health related services provided by a school district under an Individual Education Plan (IEP). Screening Mammography o Limited to one per calendar year, for women age 40 or older. Services managed directly by the Department, as defined in the Provider Handbook, Provider Guidelines Sexually Transmitted Disease Testing Substance Abuse Services o Outpatient services managed by the Department or the Department’s designee (effective 9/1/13). Transportation Services Urgent Care Clinic Services o Services provided by an Urgent Care Clinic when the participant’s PCP office is closed. Participants should be referred to their PCPs for follow up care. Vision Services o Performed in the offices of ophthalmologists and optometrists, including eyeglasses. Waiver Services for the Aged and Disabled o These services are only covered for those Medicaid participants who qualify for both the Medicaid Enhanced plan and the Aged and Disabled Waiver. 2.5.5.6. • • • • • General Provider and Participant Information Reimbursement for Services Requiring Referral Backdated or retro referrals are not valid. A referral number is not required on a claim and claims will process regardless of referral status. Entering a referral number on a claim will cause it to fail. A service requiring a referral, without a documented referral in place, may be billed to a participant when they agree in advance (in writing) to accept financial responsibility. It is the responsibility of the billing provider to ensure a referral is documented prior to rendering services. Billing for services without a documented referral is not allowed. All Medicaid payments are subject to review, recoupment and/or subject to assessment of civil monetary penalties by the Idaho Department of Health and Welfare, as stipulated in the provider agreement A referral is not required if during the episode of care, the procedure changes from one that did not require a referral to one that now requires a referral. 2.5.5.7. Program Liaison The HC Program provides staff to help you resolve program related problems you may encounter. Please contact your local PRC to obtain information, training, or to answer questions. Refer to the Directory for specific contact information. January 29, 2015 Page 38 of 59 Idaho MMIS Provider Handbook General Provider and Participant Information 2.6. Idaho Medicaid Health Home 2.6.1. Overview A Health Home is a Medicaid State Plan Option that provides a comprehensive system of care coordination for Medicaid individuals with chronic conditions. Health Home providers integrate and coordinate all primary, acute, behavioral health, long-term services, and supports to treat the “whole-person” across the lifespan. HC providers may choose to enroll as an Idaho Medicaid Health Home (IMHH) provider, by choosing to transform their practice into a patient-centered medical home. If you are interested in becoming a Medicaid Health Home provider, contact the Idaho Medicaid Health Home program at [email protected]. ALL Healthy Connections policies, procedures and requirements, including referrals, apply to Health Home providers and participants. 2.6.2. Diagnosis Medicaid participants must have a diagnosis of one of the following: • Serious persistent mental illness • Serious emotional disturbance • Diabetes and asthma • Diabetes and a risk factor • Asthma and a risk factor 2.6.3. Risk Factors Risk factors include: • Body mass index 25 or greater • Dyslipidemia • Tobacco use • Hypertension • Diseases of the respiratory system • Coronary Artery Disease Additional information on diagnostic criteria is outlined in Section 2.6.10.2 Diagnostic Criteria of this handbook. 2.6.4. Idaho Medicaid Health Home Program Goals The goals of the Idaho Medicaid Health Home program are to: • Improve the health of chronically ill Idaho Medicaid participants • Promote a higher quality of care • Reduce risk factors associated with co-morbidity • Promote comprehensive care coordination and health promotion • Provide comprehensive transitional care and follow-up • Improve access to community based participant and family support • Promote the use of health information technology to link services • Reduce healthcare costs 2.6.5. Initial Provider and Participant Enrollment Use the following steps to become an Idaho Medicaid Health Home Provider. January 29, 2015 Page 39 of 59 Idaho MMIS Provider Handbook General Provider and Participant Information Steps To Becoming An Idaho Medicaid Health Home Provider Step 1 Enroll as a Healthy Connections PCP – Each primary care provider within the clinic/service location shall participate in the IMHH Program, as agreed to in the Coordinated Care Agreement – Addendum B. Step 2 Clinic Access Requirement – Clinic must have 46 hours of access per week providing participant care, as outlined in IDAPA rule 16.03.09, Section 574. A clinic may be designated as a Nearby Service Location if it meets the following criteria AND the clinic completes a Nearby Service Location Extended Hours Request form and it is approved by the Department. This form may be found in the forms section on the Idaho Health Home Program website. Clinic must be within the same Healthy Connections organization that has a nearby location that offers extended hours. The nearby location must utilize electronic health records to coordinate care across locations. Step 3 PCP may request information on the Health Home program and/or the number of qualified participants at a specific service location by completing the Health Home Inquiry section on the IMHH website at www.idahohealthhome.dhw.idaho.gov. Department sends the estimated number of qualified participants at specific service locations and information on the Health Home program. Step 4 Provider completes the Readiness Assessment found on the Idaho Health Home Program website and faxes to Idaho Health Home Program at 1 (208) 364-1811. Department will contact the provider to discuss their assessment, the Health Home model of care, and the clinic’s readiness. After it has been determined the clinic has met the readiness expectations of the Department, the provider will be directed to complete the Coordinated Care Agreement- Addendum B. Step 5 Provider completes the Coordinated Care Agreement- Addendum B found on the Idaho Health Home Program website and faxes it to Idaho Health Home Program at 1(208)3641811. The addendum must be received by the 15th of the month to be effective on the first of the following month. Department reviews provider’s Coordinated Care Agreement for the IMHH program. If approved, a welcome letter is sent to the provider. Step 6 Step 7 Provider conducts the initial mass enrollment process as outlined below: • IMHH provider must use their Healthy Connections roster to generate a list of qualified Health Home participants, from their Healthy Connections participant population. The Healthy Connections roster can be found in the provider’s secure Trading Partner Account on the Molina Medicaid website. It is exportable to Excel to help generate a list of qualified Health Home Participants. • The list is required to be generated on an Excel spreadsheet with the following data fields: participant’s first and last name, Medicaid ID number, date of birth, clinic service location (if applicable), primary diagnostic code, and comorbidity (if applicable). Provider sends a secure e-mail with the spreadsheet as an attachment to [email protected]. This list must be submitted by the 20th of the month for participant enrollment to be effective on the first of the following month. Initial Mass Enrollment: • • Department reviews list of potential IMHH participants submitted by provider Department will either enroll participant in IMHH program the first of the following month OR • • • Department will follow up will provider Department will identify any participants not enrolled AND provide an explanation to the provider January 29, 2015 Page 40 of 59 Idaho MMIS Provider Handbook General Provider and Participant Information Steps To Becoming An Idaho Medicaid Health Home Provider Ongoing Enrollment: • Provider submits individual participant enrollment form (this form is on the Idaho Health Home Program website under Forms). • OR • Provider submits a list of participants which includes the following data elements: o Participant name o Medicaid ID number o Date of birth o Qualifying diagnosis and co-morbidity (if it applies) o Service location and PCP • Enrollment form or the list of participants is sent to the Health Home team via fax to 1 (208) 364-1811 or e-mail [email protected]. Qualifying participant(s) will be enrolled into the Idaho Medicaid Health Homes benefit plan. Reimbursement is based on IMHH enrollment and is effective the first day of the following month. In addition to their monthly Healthy Connections Roster, IMHH providers will receive a monthly IMHH roster. 2.6.6. Provider Responsibilities Health Home Providers are required to conduct the following activities. 2.6.6.1. Conduct a Health Risk Assessment The Health Home provider will conduct a comprehensive health risk assessment (as required in IDAPA 16.03.09) following the participant’s enrollment as an IMHH participant. The health risk assessment will identify the enrollee’s physical, behavioral, and social service needs. Components of the health risk assessment may include, but are not limited to, the following. • Age and gender, appropriate immunization and lead screening • Family, social or cultural characteristics • Communication needs • Medical history of patient and family • Advance care planning (excluding children) • Behaviors affecting family • Patient and family mental health/substance abuse • Developmental screening using standardized tools (excluding adults) • Depression screening (as appropriate) for teens/adults using a standardized tool 2.6.6.2. Care Plan The Health Home provider will utilize the health risk assessment to develop an individualized participant care plan for enrolled Health Home participants (as specified in IDAPA 16.03.09) and in accordance with 2011 NCQA-PCMH guidelines. The Health Home provider will provide a written copy of the care plan to each participant/family. The care plan will be developed based on the information obtained from a health risk assessment performed by the designated provider, as described in Section 2.6.6.1 of this handbook. The assessment will identify the enrollee’s physical, behavioral, and social service needs. This will ensure the patient’s needs are identified, documented, and addressed. Family members and other support involved in the patient’s care are to be identified and included in the plan and executed, as requested by the patient. January 29, 2015 Page 41 of 59 Idaho MMIS Provider Handbook General Provider and Participant Information The care plan must include outreach and activities which will support engaging the patient in their own care plan and promote continuity of care. The care plan will include periodic reassessment of the individual’s needs and goals, and will clearly identify the patient’s progress towards meeting their goals. Changes in the care plan will be made based on changes in the patient’s needs. The care plan may include, but is not limited to, the following elements or activities that occur during relevant visits. • Active diagnosis list, including important or chronic conditions. • Allergies. • Lab test results. • Patient symptoms. • Blood pressure, height, weight, and body mass index. • Tobacco status. • Current medication list. • Current immunization status. • Treatment goals with periodic reassessment of individual needs/goals. • Noted progress toward goals, or changes in goals at each relevant visit. • List of clinical referrals and follow up with specialists and other clinical care providers. • Role of community services and supports, if appropriate, and any patient needs, referrals, or follow up related to non-clinical needs. Participant designated engagement with family/others who will support the participant. Hospitalizations and plans for care transitions. • Activities to be completed by the care coordinator or other health home team staff to help the participant achieve the goals in the care plan. (For example, telephone calls, reminders, medication checks, and so on.) 2.6.6.3. Health Home Team Responsibilities The Health Home provider will develop a health home team (as specified in IDAPA 16.03.09). The team’s responsibilities may include, but are not limited to, the following: • Developing reminders for needed tests (for example, HbA1Cs). • Tracking medical services not provided in the Health Home (such as following up on lab tests and x-rays or reports from specialists). • Tracking all referrals (clinical and non-clinical). • Conducting pre-visit preparation (such as reminding patients of appointments). • Following up on missed appointments. • Assessing and addressing barriers when the participant has not met treatment goals. • Providing a clinical summary of each visit to the participant/family at each relevant visit. • Contacting participant to ensure they are caring for themselves in accordance with the care plan. • Maintaining a current resource list covering community services (such as tobacco cessation, weight loss, parenting, dental, transportation, fall prevention, or meal support). • Providing health education opportunities/materials. • Tracking admits and/or discharges from hospitals and facilities and coordinate transitional care. January 29, 2015 Page 42 of 59 Idaho MMIS Provider Handbook 2.6.6.4. General Provider and Participant Information Hours of Access The Health Home must provide at least 46 hours of access to patient care services as outlined in Section 2.5.3.1 Healthy Connections Case Management Payment of this handbook. 2.6.6.5. Chronic Disease Registry The Health Home provider must utilize a chronic disease registry, as defined by Health Resources and Services Administration (HRSA), to track participants within the first three months after enrollment as a Health Home. The chronic disease registry must have the following functionality by the end of month three. • Track desired intervals for next visit, test, or contact, based on care guideline. • Allow clinicians to record patient-specific interval for next visit or intervention. • Provide patient lists sorted according to overdue status (e.g., no HbA1c during last 6 months) or patient status according to management control (e.g., HbA1c>8.0 or personal goal). • Provide outreach or exception lists for each physician or care team (to help identify gaps in care). 2.6.6.6. Follow Up Protocol The Health Home provider will develop and maintain a systematic follow-up protocol. The protocol will describe the provider’s process for facilitating follow-up care for the participant. Follow-up protocol must be enacted within one working day following a participant’s discharge from an inpatient/hospital stay or an emergency room visit. Hospitals are to establish policies and procedures for referring Medicaid patients presenting in the emergency department with needs related to their chronic disease to IMHH providers as outlined in Information Release MA12-20. 2.6.6.7. NCQA Recognition The Health Home provider must attain Level 1 – National Committee for Quality Assurance (NCQA) recognition within two years of the execution of their Health Home provider agreement. 2.6.6.8. Non-Clinical Health Care Needs The provider will facilitate access to the following resources. • Individual, family and community supports. • Health education. • Outpatient behavioral health services. • Preventive health and health promotion services. 2.6.6.9. Patient Notification The provider will contact participants within 60 days after enrollment in the Health Home program, to educate the participant on the Health Home program. Quality Improvement Program The Health Home provider must establish a continuous quality improvement program that is directed towards improving care for patients in their practice. January 29, 2015 Page 43 of 59 Idaho MMIS Provider Handbook General Provider and Participant Information 2.6.6.10. Reporting The Health Home provider must submit reporting documents as specified in Section 2.6.8 Provider Reporting of this handbook, and as agreed to in the Coordinated Care Agreement – Addendum B. 2.6.7. Responsibilities for Care Coordination Primary Care Providers that enroll as IMHH providers will take on care coordination responsibilities that may overlap with case management services currently received by participants through the Idaho Behavioral Health Plan (IBHP). Health Home teams and IBHP providers must communicate about services being delivered and work together to achieve an orderly transition of care coordination services to the Health Home provider, when appropriate. In some instances participants at risk may qualify to receive IBHP case management in conjunction with the Health Home provider care coordination. See Information Release MA12-20 for additional information. 2.6.7.1. Healthy Connections Policies, Procedures and Requirements ALL Healthy Connections policies, procedures, and requirements, including referrals, apply to Health Home providers and participants. HC Providers interested in becoming a Medicaid Health Home provider should contact the Idaho Medicaid Health Home program at [email protected]. 2.6.7.2. Health Homes Participant Rosters Healthy Connections/Health Home providers have two options for reviewing or retrieving their primary care participant rosters: • Online “dynamic” Primary Care Roster found in their secure Trading Partner Accounts (TPA) on the Molina Medicaid website. This is a list of participants currently enrolled to a Primary Care Case Management provider with a Healthy Connections or Health Home indicator. • Monthly web/hard copy participant rosters. This is a list of participants enrolled to an HH PCP effective the first day of the month, including the case management payment information. For providers with TPAs that also receive electronic Remittance Advice (RAs), these monthly rosters are uploaded to their secure accounts. For PCPs not receiving electronic RAs, these roster reports are mailed. 2.6.7.3. Eligibility Verification Providers verifying eligibility in the system for participants enrolled in the Health Home Program will see an Idaho Medicaid Health Homes enrollment segment. Providers may also verify eligibility by calling 1 (866) 686-4272. 2.6.8. Provider Reporting 2.6.8.1. Data and Reporting Requirements and Procedures Enrolled clinics are to conduct required reporting based on the date of a signed Coordinated Care Agreement – Addendum B. Documents should be faxed to the Idaho Health Home Program at 1 (208) 364-1811. Data submissions should be submitted per the instructions outlined in Section 2.6.8.3 Required Data. January 29, 2015 Page 44 of 59 Idaho MMIS Provider Handbook 2.6.8.2. General Provider and Participant Information Required Documents These documents should be faxed to the Idaho Health Home Program at 1 (208) 364-1811. Figure 2-6: Required Documents Required Document 1 X PCMH-A Self-Assessment Participant Satisfaction Survey Results NCQA Recognition Narrative Progress Report PCDC –Baseline PCMH tool *Required until NCQA recognition is attained. 2.6.8.3. Reporting Months 9 12 15 18 21 X X X X 3 6 X X X X X X X X X 24 X X X X X X X X X X X Required Data To report required data, clinics must register at www.pcmh.dhw.idaho.gov to submit all clinical data. Clinics will click on the data entry tab located on the homepage of the website to access the dynamic form for the clinical/practice data reports. Clinics will fill in the appropriate and required data fields for each of the reports and click the submit button located at the bottom of the page. Figure 2-7: Required Data Required Data Submission Quarterly clinic/preventive data report Practice Transformation Data 3 6 X* X Reporting Months 9 12 15 18 X X X X X X X X 21 X X 24 X X *The clinic is required to begin reporting data in month six after provider enrollment. The provider must submit clinic quality data and practice transformation data on a quarterly basis thereafter to the Department. Data is to be reported during the month following the end of the previous quarter. 2.6.8.4. Reporting Documents All reporting documents are available on the Idaho Health Home Program under Forms. All documents, except quality measurement data, must be faxed to the Idaho Medicaid Health Home Program at 1 (208) 364-1811. Participant Centered Medical Home (PCMH)-A Self-Assessment This is a standardized assessment tool to assist a clinic in determining its progress toward clinic transformation. The PCMH-A Self-Assessment form must be completed within the first 30 days of start date and every six months thereafter. Narrative Progress Report The progress report is due by the end of month three after signing the Health Home addendum, and quarterly thereafter. This report is completed by leadership at the organization, summarizing the progress on goals, challenges, and technical assistance needs. January 29, 2015 Page 45 of 59 Idaho MMIS Provider Handbook General Provider and Participant Information Participant Satisfaction Survey IMHH providers are required to conduct a participant satisfaction survey. You may choose to conduct any standardized participant satisfaction survey instrument, as long as you continually utilize the same survey to display trending over time. Each clinic is encouraged to use a standardized participant satisfaction survey focused on the joint principles of a medical home. The survey must be conducted and reported on during the timeframes specified under Section 2.6.8 Provider Reporting. The practice will provide reports with summarized results of patient feedback. A blank survey tool does not meet this requirement. The survey must adhere to 2011 NCQA-PCMH guidelines and must include questions related to at least three of the four following categories: • Access • Communication • Coordination of care • Whole person care/self-management support. Recommended survey components are: • Participant’s access to routine, urgent, and after-hours care • Participant’s rating/feelings on communication with the practice, clinicians, and staff around their ability to get answers to questions • Participant’s rating/feelings of being respected/listened to • Participant’s rating/feelings on the provider’s ability to provide preventive education • Provider’s assistance with making health care decisions or assistance in making changes in health habits • Participant’s rating/feelings on being informed and up to date on referrals to specialists, changes in medications and receiving lab or imaging results • Participant’s rating/feelings on the provider’s ability to support all aspects of care, including mental health needs and non-clinical health care needs Primary Care Development Corporation (PCDC) – Baseline PCMH Tool This PCMH Self-Assessment Tool must be completed within six months of start date and quarterly thereafter. The assessment, developed by the Primary Care Development Corporation (PCDC), maps onto the NCQA factors, which will show progress toward meeting specific NCQA standards associated with recognition. Upon NCQA recognition, the clinic site will no longer be required to complete the PCDC assessment. NCQA Recognition Providers must enroll with the National Center for Quality Assurance and complete Level 1 recognition by the end of year two, as agreed upon in the Coordinated Care Agreement – Addendum B. 2.6.8.5. Clinical Quality The clinic/practice is required to report quarterly (as indicated in Section 2.6.8 Provider Reporting) on at least one (1) chronic disease bundle most relevant to its qualified Health Home participant population. The disease bundle measure must include all patients in the practice that have been identified as having that chronic disease. Technical specifications for Health Home measures are located at www.idahohealthhome.dhw.idaho.gov. Providers must choose from the following measures, as agreed to in Coordinated Care Agreement Addendum B, of their provider agreement. January 29, 2015 Page 46 of 59 Idaho MMIS Provider Handbook General Provider and Participant Information The clinic/practice shall report on two or more of the following clinic/practice quality measures. (If your practice selects ANY asthma measure, you are required to report on all three asthma measures). • Hemoglobin A1c Testing (% of diabetics with one or more HbA1c tests per year) • Diabetes hemoglobin A1c poor control (% of diabetics with HbA1c > 9.0) • Controlling high blood pressure (% of hypertensive patients with controlled blood pressure) • Hypertension: blood pressure measurement (% of hypertensive patients with two office visits and recorded blood pressures) • Anti-depressant medication management; effective acute phase and effective continuation phase treatment (% of diagnosed depressed patients treated and remained on medication) • Screening for clinic/practice depression (% of patients screened for depression) • Asthma assessment (% of asthmatic patients with assessment) • Asthma pharmacologic therapy (% of asthmatics prescribed long-term control medication) • Management plan for people with asthma (% of asthmatics with documented care plan) 2.6.8.6. Preventive Quality Measures The clinic/practice is required to report quarterly (as indicated in Section 2.6.8 Provider Reporting) on two (2) preventive quality measures listed below. • Weight assessment counseling for children and adolescents • Well-child visits in the third, fifth, and sixth years of life • Annual risky behavior assessment or counseling from age 12 to 18 • Tobacco use assessment • Tobacco cessation intervention • Adult weight screening and follow-up 2.6.8.7. Practice Transformation Measures The clinic/practice is required to report quarterly (as indicated in Section 2.6.8 Provider Reporting) on the two-practice transformation measures listed as follows. 1. Third next available appointment - Average length of time (in days) between the day a participant makes a request for an appointment with a physician and the third available appointment for a new participant physical, routine exam, or return visit exam. The clinic is required to measure the third next available visit per provider each month and submit the quarterly average by service location. Note: Count calendar days, including weekends and days off. Do not count any saved appointments for urgent visits (since they are "blocked off" on the schedule). 2. Participant visits with the PCP - The percentage of participant visits that occur with Health Home PCP. If you have questions regarding measurement criteria or reporting, contact the Health Homes program at [email protected]. 2.6.9. Provider Reimbursement Provider reimbursement for Health Home participants is based on qualified participants enrolled in the IMHH Program. Provider reimbursement for IMHH participants will be $15.50 January 29, 2015 Page 47 of 59 Idaho MMIS Provider Handbook General Provider and Participant Information per member per month as enrolled on the first day of the month. The IMHH per member per month payment is in lieu of any other primary care case management reimbursement and is in addition to fee-for-service reimbursements. 2.6.10. Participant Enrollment Providers must ensure that all participants meet the Health Home diagnostic criteria outlined in IDAPA 16.03.09.571.0 and included in Section 2.6.10.2 Diagnostic Criteria of this document. An initial mass enrollment process will be conducted as outlined in Section 2.6.5 Overview. After the provider’s initial mass enrollment of participants has been completed, participant enrollment will be subject to the ongoing enrollment process identified as follows. 2.6.10.1. Ongoing Enrollment Process • • • • IMHH provider submits individual participant enrollment form OR Submits a list of participants to include the following data elements: o Participant name, participant MID, participant DOB, qualifying diagnosis and co-morbidity if applies, service location and PCP. Department will process enrollment request. Reimbursement based on IMHH enrollment, will begin the first of the following month. In addition to their monthly Healthy Connections Roster, IMHH providers will receive a monthly IMHH roster. After a provider completes the initial mass enrollment process, all newly identified, Health Home participants must be enrolled using the following steps. 1. A new qualified participant is identified by the provider. 2. The Health Home Participant Enrollment Form is completed by the provider. (This form is on the Idaho Health Home Program website under Forms.) Alternatively, the provider may submit a list of participants, in Excel format, which includes the following data elements: o Participant name o Medicaid ID number o Date of birth o Qualifying diagnosis and co-morbidity (if it applies) o Service location and PCP 3. Enrollment form is faxed to the Health Home team at 1 (208) 364-1811, or e-mailed to [email protected]. The forms and/or list must be received by the 20th of the month in order for participant to be effective the first of the following month. 4. The participant will be enrolled into the Idaho Medicaid Health Homes benefit plan upon receipt of the participant enrollment form, effective the first day of the following month. 2.6.10.2. Diagnostic Criteria Providers must reference the diagnostic codes located on the Idaho Health Home Program Information website for determining the participant’s eligibility for IMHH. A participant’s eligibility must be determined based on a qualified diagnosis listed as follows. January 29, 2015 Page 48 of 59 Idaho MMIS Provider Handbook General Provider and Participant Information Medicaid participants must have a diagnosis of: • • • • • Serious persistent mental illness Serious emotional disturbance Diabetes and asthma Diabetes and a risk factor Asthma and a risk factor Risk factors include: • • • • • • Body mass index 25 or greater Dyslipidemia Tobacco use Hypertension Diseases of the respiratory system Coronary Artery Disease Please refer to the Idaho Health Home Program Information website. Click on Participant Eligibility and then Diagnosis Codes for more information. 2.7. Child Wellness Exams 2.7.1. Wellness Exams All children ages birth through 21 should receive regular wellness exams from their Primary Care Providers (PCPs). Idaho Medicaid has adopted the American Academy of Pediatrics (AAP) periodicity schedule as the recommended frequency for child wellness exams. This periodicity schedule has been replicated in the tables found in Section 2.7.3 Periodicity Schedule. Parents are sent reminder notices to schedule wellness exams for their children. 2.7.2. Content of Wellness Exams The AAP periodicity schedule delineates the types of screening and testing that should be conducted during a wellness exam for each age group. Federal law requires that the wellness exams include: • Comprehensive health and developmental history • Comprehensive unclothed physical exam • Appropriate immunizations • Laboratory tests (as indicated in periodicity schedule) • Health education including anticipatory guidance Note: Federal regulations require that all Medicaid eligible children are tested for lead poisoning at the age of 12 months and 24 months. 2.7.3. Periodicity Schedule If a child receives care for the first time at any point on the schedule, or if any items are not accomplished at the suggested age, the schedule should be brought up to date at the earliest possible time. Note: Medicaid eligible children should be tested for lead poisoning at least once prior to age six if required testing was not completed at 12 months and 24 months. January 29, 2015 Page 49 of 59 Idaho MMIS Provider Handbook 2.7.3.1. General Provider and Participant Information Infancy Screening Figure 2-8: Infancy Screening 2,3 3-5 4 Days By 1 Mo. 2 Mos. 4 Mos. 6 Mos. 9 Mos. X X X X X X X Length/Height and Weight X X X X X X X Head Circumference X X X X X X X Weight for Length X X X X X X X Blood Pressure5 R R R R R R R Vision R R R R R R R Hearing X7 R R R R R R Age 1 Newborn History Initial/Interval Measurements Sensory Screening Development/Behavior Assessment Developmental Screening8 X Developmental Surveillance8 X X X X X X Psychosocial/Behavioral Assessment X X X X X X X Physical Examination10 X X X X X X X ← X → → X X X X X X X R R 11 Procedures Newborn Metabolic Screening12 Immunization13 Hematocrit or Hemoglobin 14 R Lead Screening15 Tuberculin Test17 R R Oral Health21 23 Anticipatory Guidance X X X X X R R X X Key X R ← or → = to be performed = risk assessment to be performed with appropriate action to follow, if positive = the range during which a service should be provided (with the X at the preferred age) Note: Numbers 1 through 23 are found in Section 2.7.3.5. January 29, 2015 Page 50 of 59 Idaho MMIS Provider Handbook General Provider and Participant Information Figure 2-9: Anticipatory Guidance During Infancy Anticipatory Guidance During Infancy (extracted from “Bright Futures: Guidelines for Health Supervision of Infants, Children, and Adolescents” Newborn First Week 1 Month 2 Month 4 Month 6 Month 9 Month 2.7.3.2. Family Readiness, Infant Behaviors, Feeding, Safety, Routine Baby Care Parental (Maternal) Well-Being, Newborn Transition, Nutritional Adequacy, Safety, Newborn Care Parental (Maternal) Well-Being, Family Adjustment, Infant Adjustment, Feeding Routines, Safety Parental (Maternal) Well-Being, Infant Behavior, Infant-Family Synchrony, Nutritional Adequacy, Safety Family Functioning, Infant Development, Nutrition Adequacy and Growth, Safety Family Functioning, Infant Development, Nutrition and Feeding: Adequacy/Growth, Oral Health, Safety Family Adaptations, Infant Independence, Feeding Routine, Oral Health, Safety Early Childhood Screening Figure 2-10: Early Childhood Screening 12 Mos. 15 Mos. 18 Mos. 24 Mos. 30 Mos. 3 Yrs. 4 Yrs. X X X X X X X Length/Height and Weight X X X X X X X Head Circumference X X X X Weight for Length X X X X X X X Age History Initial/Interval Measurements Body Mass Index 15 Blood Pressure R R R R X X Sensory Screening Vision R R R R R X6 X Hearing R R R R R R X X X Developmental/Behavioral Assessment Developmental Screening8 Autism Screening X 9 Developmental Surveillance X 8 X X X X Psychosocial/Behavioral Assessment X X X X X X X Physical Examination10 X X X X X X X January 29, 2015 X Page 51 of 59 Idaho MMIS Provider Handbook General Provider and Participant Information 12 Mos. 15 Mos. 18 Mos. 24 Mos. 30 Mos. 3 Yrs. 4 Yrs. Immunization13 X X X X X X X Hematocrit or Hemoglobin14 X R R R R R R R R Age Procedures11 Lead Screening Tuberculin Test 15 X 17 16 R R Dyslipidemia Screening R 18 21 Oral Health R R X or R21 Anticipatory Guidance X 16 X X R X or R21 X or R21 X or R21 X X X X 22 X X Key X R ← or → = to be performed = risk assessment to be performed with appropriate action to follow, if positive = the range during which a service should be provided (with the X at the preferred age) Note: Numbers 1 through 23 are found in Section 2.7.3.5. Figure 2-11: Anticipatory Guidance during Early Childhood Anticipatory Guidance during Early Childhood (extracted from “Bright Futures: Guidelines for Health Supervision of Infants, Children, and Adolescents” 12 Month Family Support, Establishing Routines, Feeding and Appetite Changes, Establishing a Dental Home, Safety 15 Month Communication and Social Development, Sleep routines and Issues, Temper Tantrums and Discipline, Healthy Teeth, Safety 18 Month Family Support, Child Development and Behavior, Language Promotion/Hearing, Toilet Training Readiness, Safety 24 Month Assessment of Language Development, Temperament and Behavior, Toilet Training, Television Viewing, Safety 30 Month Family Routines, Language Promotion and Communication, Promoting Social Development, Preschool Considerations, Safety 3 Year Family Support, Encouraging Literacy Activities, Playing with Peers, Promoting Physical Activity, Safety 4 Year School Readiness, Developing Healthy Personal Habits, Television/Media, Child and Family Involvement and Safety in the Community, Safety January 29, 2015 Page 52 of 59 Idaho MMIS Provider Handbook 2.7.3.3. General Provider and Participant Information Middle Childhood Screening Figure 2-12: Middle Childhood Screening Age1 5 Yrs. 6 Yrs. 7 Yrs. 8 Yrs. 9 Yrs. 10 Yrs. X X X X X X Height and Weight X X X X X X Body Mass Index X X X X X X Blood Pressure5 X X X X X X Vision X X R X R X Hearing X X R X R X Developmental/Behavioral A t Developmental Surveillance8 X X X X X X Psychosocial/Behavioral X X X X X X X X X X X X Immunization13 X X X X X X Hematocrit or Hemoglobin14 R R R R R R R R R R R R R R History Initial/Interval Measurements Sensory Screening Physical Examination 10 Procedures11 Lead Screening 15 Tuberculin Test17 Dyslipidemia Screening 18 R Oral Health21 Anticipatory Guidance23 R R X22 X X X X X X Key X R ← or → = to be performed = risk assessment to be performed with appropriate action to follow, if positive = the range during which a service should be provided (with the X at the preferred age) Notes: Numbers 1 through 23 are found in Section 2.7.3.5. January 29, 2015 Page 53 of 59 Idaho MMIS Provider Handbook General Provider and Participant Information Figure 2-13: Anticipatory Guidance During Middle Childhood Anticipatory Guidance during Middle Childhood (extracted from “Bright Futures: Guidelines for Health Supervision of Infants, Children, and Adolescents” 5 and 6 Year School Readiness Mental Health Nutrition and Physical Activity Oral Health Safety 7, 8, 9, and 10 Year School Development and Mental Health Nutrition and Physical Activity Oral Health Safety 2.7.3.4. Adolescence Screening Figure 2-14: Adolescence Screening Age1 11 Yrs. 12 Yrs. 13 Yrs. 14 Yrs. 15 Yrs. 16 Yrs. 17 Yrs. 18 Yrs. 19 Yrs. 20 Yrs. 21 Yrs. X X X X X X X X X X X X X X X X X X X X X X X X X X X X X X X X X X X X X X X X X X X X R R X X R X R R X R R X X R X R R X R R X X R X R R X R R X R R X X X X X X X X X X X X Psychosocial/ Behavioral Assessment X X X X X X X X X X X Alcohol and Drug Use Physical Examination10 Procedures11 Immunization13 Hematocrit or Hemoglobin14 R R R R R R R R R R R X X X X X X X X X X X X R X R X R X R X R X R X R X R X R X R X R Tuberculin Test17 R R R R R R R R R R R History Initial/Interval Measurements Height and Weight Body Mass Index Blood Pressure5 Sensory Screening Vision Hearing Developmental/ Behavioral Assessment Developmental Surveillance8 January 29, 2015 Page 54 of 59 Idaho MMIS Provider Handbook Age1 Dyslipidemia Screening18 STI Screening19 Cervical Dysplasia Screening20 Anticipatory Guidance23 General Provider and Participant Information 11 Yrs. 12 Yrs. 13 Yrs. 14 Yrs. 15 Yrs. 16 Yrs. 17 Yrs. 18 Yrs. 19 Yrs. 20 Yrs. 21 Yrs. R R R R R R R ← ← X → R R R R R R R R R R R R R R R R R R R R R R X X X X X X X X X X X Key X R ← or → = to be performed = risk assessment to be performed with appropriate action to follow, if positive = the range during which a service should be provided (with the X at the preferred age) Notes: Numbers 1 through 23 are found in Section 2.7.3.5. Figure 2-15: Anticipatory Guidance during Adolescence Anticipatory Guidance during Adolescence (extracted from “Bright Futures: Guidelines for Health Supervision of Infants, Children, and Adolescents” Each Year Age 11-21 Physical Growth and Development Social and Academic Competence Emotional Well-Being Risk Reduction Violence and Injury Prevention 2.7.3.5. Notes from the Recommendations for Preventive Pediatrics Health Care, the American Academy of Pediatrics (AAP) and the American Association of Pediatric Dentistry (AAPD) 1. If a child comes under care for the first time at any point on the schedule, or if any items are not accomplished at the suggested age, the schedule should be brought up to date at the earliest possible time. 2. A prenatal visit is recommended for parents who are at high risk, for first-time parents, and for those who request a conference. The prenatal visit should include anticipatory guidance, pertinent medical history, and a discussion of benefits of breastfeeding and planned method of feeding per AAP statement, The Prenatal Visit (2001). http://aappolicy.aappublications.org/cgi/content/full/pediatrics;107/6/1456. 3. Every infant should have a newborn evaluation after birth, breastfeeding should be encouraged, and instruction and support should be offered. 4. Every infant should have an evaluation within three to five days of birth and within 48 to 72 hours after discharge from the hospital, to include evaluation for feeding and jaundice. Breastfeeding infants should receive formal breastfeeding evaluation, encouragement, and instruction as recommended in AAP statement, Breastfeeding and the Use of Human Milk (2005). http://aappolicy.aappublications.org/cgi/content/abstract/pediatrics;115/2/496 January 29, 2015 Page 55 of 59 Idaho MMIS Provider Handbook General Provider and Participant Information 5. For newborns discharged less than 48 hours after delivery, the infants must be examined within 48 hours of discharge per AAP statement, Hospital Stay for Healthy Term Newborns (2010), http://aappolicy.aappublications.org/cgi/content/abstract/pediatrics;125/2/405 6. Blood pressure measurement in infants and children with specific risk conditions should be performed before the age of three years. 7. If the patient is uncooperative, rescreen within six months. 8. All newborns should be screened per AAP statement, Year 2007 Position Statement: Principles and Guidelines for Early Hearing Detection and Intervention Programs (2007). Joint Committee on Infant Hearing, Year 2007 position statement: principles and guidelines for early hearing detection and intervention programs. http://pediatrics.aappublications.org/cgi/content/extract/pediatrics;120/4/898 9. AAP Council on Children With Disabilities, AAP Section on Developmental Behavioral Pediatrics, AAP Bright Futures Steering Committee, AAP Medical Home Initiatives for Children With Special Needs Project Advisory Committee. Identifying infants and young children with developmental disorders in the medical home: an algorithm for developmental surveillance and screening. Pediatrics 2006; 118:405-420 http://pediatrics.aappublications.org/cgi/content/abstract/118/1/405?maxtoshow=& hits=10&RESULTFORMAT=&fulltext=developmental+surveillance&searchid=1&FIRST INDEX=0&sortspec=relevance&resourcetype=HWCIT. 10. Gupta VA, Hyman SL, Johnson CP; et al. Identifying children with autism early? Pediatrics. 2007; 119:152-153 http://pediatrics.aappublications.org/cgi/content/extract/119/1/152?maxtoshow=&hi ts=10&RESULTFORMAT=&fulltext=children+with+autism+early&searchid=1&FIRSTI NDEX=0&sortspec=relevance&resourcetype=HWCIT. 11. At each visit, age-appropriate physical examination is essential, with infant totally unclothed, older child undressed and suitably draped. 12. These may be modified, depending upon entry point into the schedule and individual need. 13. Newborn metabolic and hemoglobinopathy screening should be done according to state law. Results should be reviewed at visits and appropriate retesting or referral done as needed. 14. Schedule(s) per the Committee on Infectious Diseases, published annually in the January edition of Pediatrics. Every visit should be an opportunity to update and complete a child’s immunization. 15. See AAP Pediatric Nutrition Handbook, 5th Edition (2003) for a discussion of universal and selective screening options. See also Recommendations to prevent and control iron deficiency in the United State, MMWR. 1998;47(RR-3):1-36. 16. For children at risk of lead exposure, consult the AAP statement Lead Exposure in Children: Prevention, Detection, and Management (2005) http://pediatrics.aappublications.org/cgi/content/abstract/116/4/1036?maxtoshow= &hits=10&RESULTFORMAT=&fulltext=lead+exposure&searchid=1&FIRSTINDEX=0&s ortspec=relevance&resourcetype=HWCIT. Additionally, screening should be done in accordance with state law where applicable. 17. Perform risk assessment or screens as appropriate, based on universal screening requirements for patients with Medicaid or high prevalence areas. 18. Tuberculosis testing per recommendations of the Committee on Infectious Diseases, published in the current edition of Red Book: Report of the Committee on Infectious Diseases. Testing should be done on recognition of high-risk factors. 19. Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) Final Report (2002) http://circ.ahajournals.org/cgi/reprint/106/25/3143.pdf and The Expert Committee January 29, 2015 Page 56 of 59 Idaho MMIS Provider Handbook General Provider and Participant Information Recommendations on the Assessment, prevention, and Treatment of Child and Adolescent Overweight and Obesity. Supplement to Pediatrics (2007). http://pediatrics.aappublications.org/cgi/content/abstract/120/Supplement_4/S164 20. All sexually active patients should be screened annually for sexually transmitted infections (STIs). 21. All sexually active girls should have screening for cervical dysplasia as part of a pelvic examination beginning within three years of onset of sexual activity or age 21 (whichever comes first). 22. Referral to a dental home, if available. Otherwise, administer oral health risk assessment. If the primary water source is deficient in fluoride, consider oral fluoride supplementation. 23. At the visit for one year of age, it should be determined whether the patient has a dental home. If the patient does not have a dental home, a referral should be made to one. If the primary water source is deficient in fluoride, consider oral fluoride supplementation. Please see the American Academy of Pediatric Dentistry guidelines at http://www.aapd.org/dentalhome/ for more information. 24. Refer to the specific guidance by age as listed in Bright Futures Guidelines (Hagan JF, Shaw JS, Doncan PM, eds. Bright Futures: Guidelines for health Supervision of Infants, Children, and Adolescents. 3rd ed. Elk Grove Village, IL: American Academy of Pediatrics; 2008) 2.7.4. Early & Periodic Screening, Diagnosis & Treatment (EPSDT) Children up to the age of 21 may request medically necessary services under the EPSDT prior authorization process. The services may include, but are not limited to the following: • Annual physicals • Medical equipment and supplies • Counseling and mental health services • Medical Transportation services • Dental services, including a referral to a • Nurse Midwife dentist by age three • Pregnancy and family planning services • Doctor visits • Prescriptions • Durable Medical Equipment • Primary Care Case Management • Emergency Medical Transportation • Prosthetics/orthotics • Health Education • Substance Abuse Treatment • Hearing services, including hearing aids • Smoking Cessation • Home health care (doctor prescribed) • Vision Services, including eyeglasses • Hospice Care • Weight loss • Immunizations • X-rays • Inpatient and outpatient hospital care • Laboratory tests (including blood level assessments appropriate for age and risk factors) The EPSDT benefit was designed to help ensure that all Medicaid-eligible children receive preventive health care and early intervention services needed to maximize each child’s potential for healthy growth and development. The benefits also allow children to receive some additional services that are not covered for adults. If services not covered under the State Plan are needed, a Request for Additional Services (RAS) form must be submitted to the Department for prior authorization. All January 29, 2015 Page 57 of 59 Idaho MMIS Provider Handbook General Provider and Participant Information services under EPSDT must be considered safe, effective, and meet acceptable standards of medical practice. The RAS form is available in the Forms section on the Molina Provider portal at www.idmedicaid.com. 2.7.5. Billing Wellness exams must be billed with the Preventive Medicine CPT Codes, and, if applicable, a modifier. The CPT codes 96110 or 96111 should be billed when using a standardized tool (such as the Ages & Stages Questionnaire) to assess development and behavior. See Section 2.12.1 of the Allopathic and Osteopathic Physicians handbook for additional information. 2.7.5.1. Diagnosis Codes Providers must use the preventive medicine procedure codes and diagnosis code V20.1 V20.2, V20.31 or V20.32 when billing for child wellness exams. 2.8. Preventive Health Assistance (PHA) 2.8.1. Weight Management 2.8.1.1. Eligibility Adults with a body mass index (BMI) of 30 or higher, or 18 ½ or lower, may qualify for assistance with paying for an approved weight management program. Children with a BMI that falls into either the overweight or the underweight category may qualify for assistance with paying for an approved weight management program. Providers should refer participants needing assistance with their weight to the PHA unit for eligibility determination at 1 (877) 364-1843. 2.8.1.2. Enrolling and Billing for Services Weight management providers must follow the steps below to determine eligibility for weight management services and to bill. 1. The provider verifies eligibility by calling Molina customer service at 1 (866) 6864272, to verify both Medicaid and PHA weight management eligibility. 2. The provider accepts the participant’s voucher. 3. The participant is enrolled in an approved weight management program. Their benefit is limited to the dollar amount listed on their voucher and will never exceed $200 per year. 4. A claim is submitted through the Molina provider portal for the weight management services. 2.8.2. Wellness 2.8.2.1. Eligibility Children enrolled in the Children’s Health Insurance Program (CHIP) are subject to a monthly premium of $10 or $15 per month. If parents keep their children up-to-date on January 29, 2015 Page 58 of 59 Idaho MMIS Provider Handbook General Provider and Participant Information their well child exams AND immunizations (see Section 2.7 Child Wellness Exams), the child will receive a $10 discount every month on their premium. 2.8.2.2. Premium Statements Statements are mailed to parents on a monthly basis. If a parent knows their child is up-todate on their well checks and immunizations, they may ask their PCP to fax verification of the check up or immunizations to the PHA Unit at 1 (877) 845-3956. If you have questions about the PHA program, please call the PHA Unit toll free at 1 (877) 364-1843. January 29, 2015 Page 59 of 59
© Copyright 2026