
Detection of Human Herpesvirus-8 and Epstein
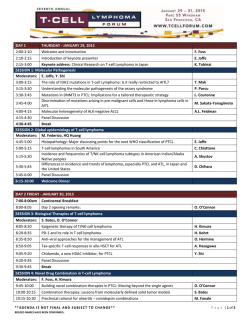
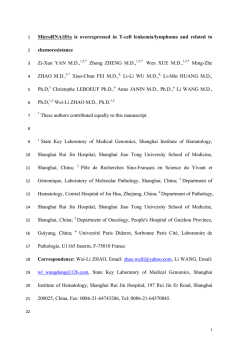
From www.bloodjournal.org by guest on February 6, 2015. For personal use only. CORRESPONDENCE depleted in their 3 patients. T-cell chimerism before DLI, therefore, was mixed and not already predominantly of donor type, as in our cases. Gardiner et al state that their technique using lineage-specific STR-PCR provides reliable results on the chimeric profile post-BMT and may be more useful than the FICTION assay in situations with low cell numbers. Although the important aspect of morphology and individual cell by cell analysis is lost with the PCR approach, we agree that STR-PCR is a most valuable tool in this context and therefore complementary to our FICTION analysis. However, we doubt that subtle changes in the degree of mixed chimerism can be seen with a semiquantitative technique according to which mixed chimerism is defined as a percentage of recipient cells between less than 90% and greater than 10%. Indeed, in the work of Gardiner et al, significant changes in every case were detected only concomitantly to the onset of clinical graft-versus-host disease (GVHD), a result similar to that obtained in our cases when using the AmpliType Polymarker PCR kit to document non–lineage-specific DNA chimerism. In contrast, when using our quantitative techniques, ie, FICTION and competitive differential bcr-abl RT-PCR as an additional diseasespecific marker, the beginning of the critical switch period could be detected several weeks before the onset of clinical GVHD. Although we therefore very much support a larger scale study to better understand the kinetics of the GVL response after DLI in T-cell–depleted and non—T-cell– depleted BMT recipients, we strongly suggest the use of true quantitative measures of lineage-specific chimerism. The FICTION method is especially helpful in small centers, because it can be performed without larger equipment or in situations in which morphological control of the selected population is of additional value. Another attractive tool is the combination of FACS sorting and quantitative multiplex STR-PCR with fluorescent primers.3 This technique has been successfully applied by members of our group to study subtle changes of subset chimerism in 2749 patients undergoing nonmyeloablative stem cell transplantation and was shown to be predictive of response, GVHD, and disease recurrence.4 Herrad Baurmann BMT Center Deutsche Klinik fu¨r Diagnostik Wiesbaden, Germany Christian Thiede Stefan Nagel Thomas Binder Andreas Neubauer Wolfgang Siegert Dieter Huhn REFERENCES 1. Gardiner N, Lawler M, O’Riordan JM, DeArce M, McCann SR: Monitoring of lineage specific chimaerism allows early prediction of response following donor lymphocyte infusions for relapsed chronic myeloid leukemia. Bone Marrow Transplant 21:711, 1998 2. Baurmann H, Nagel S, Binder T, Neubauer A, Siegert W, Huhn D: Kinetics of the graft versus leukemia response after donor leukocyte infusions for relapsed chronic myeloid leukemia after allogeneic bone marrow transplantation. Blood 92:3582, 1998 3. Thiede C, Florek M, Bornha¨user M, Ritter M, Mohr B, Brendel C, Ehninger G, Neubauer A: Rapid quantification of mixed chimerism using multiplex amplification of short tandem repeat markers and fluorescence detection. Bone Marrow Transplant (in press) 4. Thiede C, Brendel C, Mohr B, Florek M, Oelschlagel U, Ritter M, Naumann R, Geissler G, Ehninger G, Neubauer A, Bornha¨user M: Comparative analysis of chimerism in the early post-transplantation period in cellular subsets of patients undergoing myeloablative and non-myeloablative allogeneic blood stem cell transplantation. Blood 92:132a, 1998 (abstr, suppl 1) Detection of Human Herpesvirus-8 and Epstein-Barr Virus DNA in Primary Intraocular Lymphomas To the Editor: Two herpesviruses, human herpesvirus-8 (HHV-8) and Epstein-Barr virus (EBV), are able to contribute to lymphomagenesis in humans.1 HHV-8 is documented not only in a strong association with Kaposi’s sarcoma, but also in a high percentage of primary effusion lymphoma, Castleman’s disease, and multiple myeloma. Most recently, HHV-8 genome has been associated with primary central nervous system lymphoma (PCNSL) of patients with and without acquired immunodeficiency syndrome (AIDS).2 However, the role of HHV-8 in the pathogenesis of PCNSL remains controversial.3 In vitro, EBV efficiently transforms human B lymphocytes, causing them to proliferate continuously.1 EBV and the latent membrane protein can be detected in tumor cells of almost all AIDS-related PCNSL. Primary intraocular lymphoma, a component of PCNSL, is a large B-cell, non-Hodgkin’s lymphoma.4 The disease is aggressive, with a 5-year survival rate of less than 33%. In the past 15 years, the incidence of the tumor has increased dramatically, coincident with the AIDS epidemic. We analyzed HHV-8 and EBV DNA sequences in 13 primary intraocular lymphomas with and without AIDS. Of the 13 specimens, 5 were whole eyes, 1 was a vitreoretinal biopsy, and 7 were vitrectomy samples. Slides with cells from 2 noninfectious uveitis were also used as control. The 13 patients (6 Americans and 7 Europeans) include 2 AIDS patients (1 American and 1 French patient): the American patient developed an early lymphoma and the French patient had an advanced stage, aggressive lymphoma.5 At the time at which the 13 specimens were obtained, only 3 (2 eyes and 1 vitrectomy specimen) had a proven diagnosis of PCNSL involving the eyes. Of the 5 eyes, 2 had received radiation therapy. Nine patients were being investigated for possible primary intraocular lymphoma and underwent diagnostic procedures (7 vitrectomies, 1 vitreoretinal biopsy, and 1 enucleation). The eye of the American AIDS patient was diagnosed with primary intraocular lymphoma at necropsy. On examination of the histology and cytology slides of the 13 cases, only 6 specimens (3 of 5 eyes, 3 of 7 vitrectomies, and 0 of 1 vitreoretinal biopsy) showed typical large B-cell lymphoma (Fig 1). Of the 7 cases without obvious typical lymphoma cells, 5 (4 vitreous and 1 vitreoretinal biopsy) were also available for cytokine analysis and had high vitreous interleukin-10 (IL-10) levels with high ratios of IL-10 to IL-6, suggesting primary intraocular lymphoma.6 Finally, 2 cases (1 eye with AIDS and 1 eye that had received radiation) showed only a few atypical lymphocytes in the subretinal space. The microdissected morphologically suspicious abnormal cells in all 13 cases had presented a rearrangement in FR3A of the IgH gene that confirmed the diagnosis of primary intraocular lymphoma (Fig 2).5 Lymphoma cells of these 13 specimens, normal lymphocytes of 2 vitrectomy specimens, and the 2 uveitic cases were microdissected from either deparaffinized sections or cytological slides.5 DNA of these cells were extracted for polymerase chain reaction (PCR) amplification and Southern hybridization for HHV-8 or EBV genome. Multiple primers and positive and negative controls were also used to confirm the results. Four cases were positive for HHV-8 (Fig 2). Two were the AIDSrelated lymphoma eyes and 2 were non-AIDS vitreous samples. The 2 non-AIDS patients were diagnosed with suspicious primary intraocular From www.bloodjournal.org by guest on February 6, 2015. For personal use only. 2750 CORRESPONDENCE Fig 1. Microphotograph showing typical intraocular lymphoma (arrow) in the subretinal space (A; case no. 8; insert, higher magnification of the lymphoma cells; R, retina; C, choroid) and a vitrectomy specimen (B; case no. 7; arrowheads, normal lymphocytes). (Original magnifications: A, hematoxylin & eosin, ؋200, insert, ؋400; B, Diff-Quick, ؋400.) lymphoma both clinically and cytopathologically. These 4 positive patients included 2 Americans and 2 French. Three samples (1 American AIDS eye and 2 vitreous specimens) were also microdissected to obtain nonmalignant cells (retinal and optic nerve cells from the eye and infiltrating lymphocytes from the other 2 vitreous specimens) for identification of the viral genome. HHV-8 DNA was undetectable in the inflammatory or ocular cells without tumor infiltration in the 3 early cases with primary intraocular lymphoma. EBV DNA was detected in only 1 of the 13 samples, ie, the French AIDS eye with a diffuse lymphoma. This investigation has shown HHV-8 DNA sequences in 2 of 2 Fig 2. PCR amplification showing rearrangement of third framework region in the VH region of heavy chain Ig gene in the lymphoma cells of all 13 cases, HHV-8 genome in 4 cases (lanes 3 and 4, AIDS patients; lanes 7 and 9, nonAIDS patients), and EBV genome in 1 case (lane 4, AIDS with lymphoma involving the orbit and eye). Lanes 1 through 13, cases no. 1 through 13, respectively; lane 14, negative control; lane 15, positive control. From www.bloodjournal.org by guest on February 6, 2015. For personal use only. CORRESPONDENCE 2751 AIDS-related intraocular lymphoma and in 2 of 11 non-AIDS intraocular lymphoma. The HHV-8 genome encodes homologs of cyclin D1, a cell-cycle control element; certain cytokines, regulators, and receptors; and Bcl-2, an antiapoptotic protein.7 The HHV-8 sequence also contains homologs of vial IRFs that may be involved in modulating both HHV-8 replication and HHV-8–associated tumorigenicity.8 The viral genome could therefore contribute to cellular growth and transformation through activation of the cell cycle. Although the virus could simply be an innocent passenger in this lymphoma, the so-far ubiquitous association of HHV-8 with AIDS-related PCNSL and relatively low incidence in non-AIDS patients, plus most other lymphoproliferative disorders in both AIDS and non-AIDS patients, strongly favor a causal role. In this series, HHV-8 was detected in 100% (2 cases: 1 American and 1 French) of AIDS-related intraocular lymphoma and in 1 of the 6 European and 1 of the 5 American, non-AIDS cases. Furthermore, HHV-8 DNA was found only in the neoplastic cells. We speculate that the nonneoplastic B lymphocytes in those AIDS patients who eventually develop primary intraocular lymphoma may be infected with HHV-8, HIV, or other viruses into the eye, in which ultimate transformation into malignant cells occurs. Another possibility may be the promotion of a second oncogenic virus. Nine EBV genes are known to express as proteins in EBVtransformed B-lymphoblastoid cell lines.9 One of the latent membrane proteins of the EBV engages members of the tumor necrosis factor receptor-associated molecules and then activates NF-B–driven expression of multiple viral and cellular genes. However, only certain subsets of AIDS-non Hodgkin’s lymphoma appear to be EBV-related, although a high frequency of EBV is reported in AIDS-PCNSL.10 Our data do not show a strong association between EBV and primary intraocular lymphoma, suggesting that EBV may not play a major role in the early development of primary intraocular lymphoma with or without AIDS. Chi-Chao Chan De Fen Shen Scott M. Whitcup Robert B. Nussenblatt National Eye Institute National Institutes of Health Bethesda, MD Phuc LeHoang Francois G. Roberge Nathalie Cassoux Department of Ophthalmology Pitie-Salpetriere Hospital Paris, France Carl Herbort Department of Ophthalmology Lausanne, Switzerland Zhengping Zhuang National Cancer Institute National Institutes of Health REFERENCES 1. Lyons SF, Liebowitz DN: The roles of human viruses in the pathogenesis of lymphoma. Semin Oncol 25:461, 1998 2. Corboy JR, Garl PJ, Kleinschmidt-DeMasters BK: Human herpesvirus 8 DNA in CNS lymphomas from patients with and without AIDS. Neurology 50:335, 1998 3. Epstein LG: Does human herpesvirus 8 have a pathogenetic role in primary CNS lymphoma? Neurology 50:322, 1998 4. Whitcup SM, de Smet MD, Rubin BI, Palestine AG, Martin DF, Burnier MJ, Chan CC, Nussenblatt RB: Intraocular lymphoma. Clinical and histopathologic diagnosis. Ophthalmology 100:1399, 1993 5. Shen DF, Zhuang Z, LeHoang P, Boni R, Zheng S, Nussenblatt RB, Chan CC: Utility of microdissection and polymerase chain reaction for the detection of immunoglobulin gene rearrangement and translocation in primary intraocular lymphoma. Ophthalmology 105: 1664, 1998 6. Whitcup SM, Stark-Vancs V, Wittes RE, Solomon D, Podgor MJ, Nussenblatt RB, Chan CC: Association of interleukin-10 in the vitreous and cerebral spinal fluid and primary central nervous system lymphoma. Arch Ophthalmol 115:1157, 1997 7. Russo JJ, Bohenzky RA, Chien MC, Chen J, Yan M, Maddalena D, Parry JP, Peruzzi D, Edelman IS, Chang Y, Moore PS: Nucleotide sequence of the Kaposi sarcoma-associated herpesvirus (HHV8). Proc Natl Acad Sci USA 93:14862, 1996 8. Moore PS, Boshoff C, Weiss RA, Chang Y: Molecular mimicry of human cytokine and cytokine response pathway genes by KSHV. Science 274:1739, 1996 9. Liebowitz D: Epstein-Barr virus and a cellular signaling pathway in lymphomas from immunosuppressed patients. N Engl J Med 338:1413, 1998 10. MacMahon EM, Glass JD, Hayward SD, Mann RB, Becker PS, Charache P, McArthur JC, Ambinder RF: Epstein-Barr virus in AIDSrelated primary central nervous system lymphoma. Lancet 338:969, 1991 From www.bloodjournal.org by guest on February 6, 2015. For personal use only. 1999 93: 2749-2751 Detection of Human Herpesvirus-8 and Epstein-Barr Virus DNA in Primary Intraocular Lymphomas Chi-Chao Chan, De Fen Shen, Scott M. Whitcup, Robert B. Nussenblatt, Phuc LeHoang, Francois G. Roberge, Nathalie Cassoux, Carl Herbort and Zhengping Zhuang Updated information and services can be found at: http://www.bloodjournal.org/content/93/8/2749.full.html Articles on similar topics can be found in the following Blood collections Information about reproducing this article in parts or in its entirety may be found online at: http://www.bloodjournal.org/site/misc/rights.xhtml#repub_requests Information about ordering reprints may be found online at: http://www.bloodjournal.org/site/misc/rights.xhtml#reprints Information about subscriptions and ASH membership may be found online at: http://www.bloodjournal.org/site/subscriptions/index.xhtml Blood (print ISSN 0006-4971, online ISSN 1528-0020), is published weekly by the American Society of Hematology, 2021 L St, NW, Suite 900, Washington DC 20036. Copyright 2011 by The American Society of Hematology; all rights reserved.
© Copyright 2026






![Download [ PDF ] - journal of evolution of medical and dental sciences](http://s2.esdocs.com/store/data/000489891_1-203bb89a5d7bdca4a63b054b12ada0ad-250x500.png)