Now Available—February 2015 - Clinical Practice Today from Duke
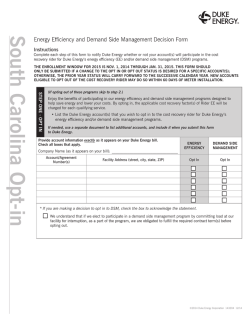
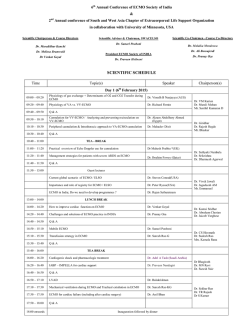
February 2015 8 Options for Extracorporeal Membrane Oxygenation Duke’s successful program is one of the largest in the country Micropractices: Simplifying Patient Care Part 2 4 Posterior Approach to Adrenals Proves Superior 6 Brachytherapy 13 Improves Cervical Cancer Care Clinical Practice Today Duke Medicine Marketing and Communications Editor Mary Jane Gore, MA Publisher Med-IQ Editorial Management Laura Espinoza Lisa R. Rinehart, MS, ELS Writers Frank Celia Meredith Kleeman Emily Paulsen Shelly K. Schwartz Eric Seaborg in Clinical Practice Today 4 Micropractices: Simplifying Patient Care 6 Posterior Approach to Adrenals Proves Superior We strive to transform medicine and health locally and globally through innovative scientific research, rapid translation of breakthrough discoveries, educating future clinical and scientific leaders, advocating and practicing evidence-based medicine to improve community health, and leading efforts to eliminate health inequalities. Preventing Unintentional Fraud 8 Options for Extracorporeal Membrane Oxygenation 10 Keep Patients Coming Back 11 Slowing the Progression of Diabetic Kidney Disease 12 Clinical Practice Today from Duke Medicine Early detection, appropriate lifestyle changes, and pharmacologic treatment can lead to a cure Brachytherapy Improves Cervical Cancer Care 14 Closing the Gap on Unpaid Patient Balances 15 New Treatment for Wet Macular Degeneration ©2015 Duke Medicine. All rights reserved. 2 Gout Is Curable With Proper Intervention 13 Materials may not be reprinted without written consent from the publisher. If you wish to be removed from the mailing list, please email [email protected] or call 866-858-7434. Increase patient satisfaction with these key strategies A new study is evaluating a telehealth approach for the prevention of kidney disease Duke University Hospital, Durham, NC Duke Regional Hospital, Durham, NC Duke Raleigh Hospital, Raleigh, NC Duke University, 3100 Tower Blvd., Suite 1008 Durham, NC 27707-2575 Keep your practice safe by watching out for these common areas of health care fraud Duke’s successful program is one of the largest in the country To refer patients, call 800-MED-DUKE. For more details on the services we offer your patients, please visit DukeMedicine.org. A new surgical technique leads to enhanced postoperative outcomes 7 About Duke Medicine U.S. News & World Report consistently ranks Duke University Hospital in its Honor Roll of top hospitals in the United States. This concluding article in our 2-part series offers strategies for establishing a micropractice Gynecologic brachytherapy confers higher survival rates than standard treatment alone Reduce your incidence of unpaid balances by implementing these helpful tips Approximately two-thirds of patients with treatmentresistant disease can benefit from this new procedure To learn more or to refer a patient, call 800-MED-DUKE News Briefs New Guideline for Hip Fractures in the Elderly A new guideline on diagnosing and treating hip fractures in patients aged 65 years and older emphasizes the importance of reducing post operative delirium, a common side effect of hip-fracture surgery. Patients who experience this side effect are less likely to return to their pre-injury level of function and have an increased risk of mortality. Recently released by the American Academy of Orthopaedic Surgeons, “the guideline provides evidence that supports the best care for this growing segment of patients,” says Steven A. Olson, MD, FACS, a professor in Duke Medicine’s Department of Orthopaedic Surgery who served on the work group that developed the clinical practice guideline. The guideline recommends using preoperative regional analgesia to reduce pain and performing hip-fracture surgery within 48 hours of hospital admission. Olson says the guideline was necessary because hip fractures are costly and increasing among older patients as the prevalence of osteoporosis rises. (Image above shows an x-ray of an elderly patient with a hip fracture.) Ten Oncologists Join Duke in Wake County Ten oncologists, most from Cancer Centers of North Carolina, joined Duke Cancer Institute’s Wake County team this fall: medical oncologists Neeraj Agrawal, MD, William Berry, MD, Elizabeth Campbell, MD, Maggie Deutsch, MD, Amit Mehta, MD, and Steve Tremont, MD; gynecologic oncologist Monica Jones, MD; and radiation oncologists February 2015 John Reilly, MD, Lewis Rosenberg, MD, and Scott Sailer, MD. They will practice at Duke Cancer Center locations in Wake County, including Raleigh and Cary. For appointments, call 919-862-5400. New Drugs Target Midlife Symptoms Several new hormone-replacement agents are coming onto the market, says Alison Weidner, vice chair for clinical affairs in OB/GYN at Duke. “Now there are more targeted therapies for a constellation of menopausal symptoms, such as forms of estrogen replacement that can stimulate the vagina to thicken its walls without affecting breast tissue,” Weidner says. Some of the new formulations include an anti-anxiety drug that mitigates hot flashes; an oral non-estrogen pill that relieves painful intercourse; and conjugated estrogens/bazedoxifene that reduce the risk of uterine cancer and mitigate hot flashes and vaginal dryness. Updates on the new pharmacology for midlife women and other topics will be discussed in depth at the Midlife Matters Conference on April 11, 2015, in Raleigh. For more information about this CME-certified course, call 877-707-2904 or visit www.dcri.org/events/stronger-together. 3 PART 2 Micropractices: Simplifying Patient Care By Emily Paulsen In this concluding article of our 2-part series, we explore factors that should be considered when establishing a micropractice. Part 1 (see the Dec. 2014 issue) examined the conditions that led to the micropractice model; part 2 will help you determine whether this approach might work for you. When staffing challenges and productivity pressures feel overwhelming, it’s easy to start daydreaming about going solo to focus on the foundation of medical practice: the patientphysician relationship. By cutting overhead, some doctors have been able to establish “micropractices,” which consist of little more than the doctor, the patient, and a computer. Many doctors who have gone this route report closer patient relationships, more time for family, and renewed joy in their profession. But even those who have met success in the micropractice model readily admit that it’s not for everyone or every situation. “It takes a special type of physician for this, someone with a lot of confidence, energy, and vision,” says Mary Pat Whaley, a practice management consultant who specializes in setting up solo and two-physician practices. It also helps 4 Clinical Practice Today from Duke Medicine to be a tech-savvy, “take charge” person who is comfortable with some degree of risk. “To practice this way takes a leap of faith,” admits John Brady, president of Ideal Medical Practice, a nonprofit organization that provides technical support for physicians exploring or practicing in this model. Brady took the leap in 2003 and remains happy with his Virginia-based solo practice, The Village Doctor. Doing the Math Determining whether this practice model will work takes some strategizing and calculating. The right personality is only part of the equation. Location, specialty, and local economic climate are also factors. “We have to understand where they are going to practice, what their specialty is, and whether the community will support them,” says Whaley. Primary care may be better suited to the micropractice model than specialty care and procedure-based care, which may require a larger referral base and patient population. But Whaley warns against making such generalizations. Determined physicians can find ways to make solo practices work even when the odds are against them. For example, some physicians move to less-expensive areas, whereas others avoid high rents by starting a “house-calls only” practice or renting space from another practice. Some areas greatly need niche specialties such as pediatric endocrinology or fibromyalgia management. Whaley remembers a surgeon who set up a micropractice and performs his surgeries at a hospital. He sees patients before and after the procedure in an examination room that he rents from other practices 1 day a week. The local economic climate—including the cost of living and income potential—plays an important role. By reviewing personal expenses (eg, mortgage or rent, food, transportation, child care), physicians can determine their minimum income requirements. Then they can research local reimbursement rates, malpractice premiums, and rental costs to figure out how the numbers add up. Both Brady and Whaley recommend setting aside at least 5 to 6 months’ worth of living expenses to cushion the financial blow of starting a new practice. A physician who is right out of residency and carrying a lot of student debt probably isn’t a good candidate for this model. Low Overhead Setups When working with a client, Whaley makes projections for 2 or 3 different practice setups to see which plays out best. The strict onephysician, one-computer micropractice model may offer the lowest overhead and quickest financial return, but most of Whaley’s clients go with a trimmed-down traditional practice of one physician and one assistant or join forces with February 2015 another physician. Some clients are interested in making the practice a family affair: a nonphysician spouse runs the administrative side of the office and the physician focuses on patients. The key is to come up with a plan that keeps overhead low. Brady recommends questioning just about everything in a typical practice to determine what’s absolutely necessary to the physician-patient relationship. Processing insurance and interacting with insurance companies could take 3 hours or more of a physician’s time each week and can significantly cut into direct patient care and annual revenue. Direct pay, cash only, and other self-payment structures may save time and money but can reduce the potential patient population and make it difficult to ramp up a practice, Brady says. (He opted to streamline his processes and continue accepting insurance.) Technology plays an outsized role in this type of practice. Brady thinks of his electronic health record (EHR) as an electronic employee that helps with scheduling, billing, and patient communications. Most EHR packages are now certified for Meaningful Use, and the emergence of cloudbased technology has significantly lowered the price for small practices. “You can get a reasonably priced or free EHR that will work fine for a small practice,” Brady notes. Although many physicians turn to a consultant to crunch the numbers, Brady encourages doctors to hammer out a business plan on their own. “You need to know the ins and outs before going in,” he cautions. Brady provides his own business plan on his Web site (www.thevillagedoctor.com) and invites physicians to use it as a starting point for their own practice. He also refers people to Ideal Medical Practice’s Web site (www.impcenter.org), which offers technical and moral support throughout the process. 5 Posterior Approach to Adrenals Proves Superior Posterior retroperitoneoscopic adrenalectomy (PRA) is a recently developed surgical strategy for removing adrenal-gland masses through the back, and it is proving helpful to many patients. Now, a clinical trial published in the Annals of Surgery has shown that this novel, minimally invasive approach has demonstrated outcomes that are superior to lateral transperitoneal laparoscopic adrenalectomy and open transperitoneal surgery. Patient outcomes were found to be better with the PRA approach, which conferred a shorter operation, less blood loss, less postoperative pain, and a quicker recovery. Sanziana Roman, MD, a Duke endocrine surgeon, says she is now seeing more referrals for this uncommon procedure. Roman, who is among the first to perform this procedure in the United States (US), says that most adrenal patients with benign neoplasms can be considered for PRA. “It is well tolerated and reduces pain and recovery time for patients because the surgeons do not cut as far into the body.” PRA is helpful for patients with tumors on both adrenal glands, which happens in up to 10% of cases. This approach also benefits patients who have previously had extensive abdominal surgery. Referrals for PRA are rising as the number of 6 Clinical Practice Today from Duke Medicine adrenal incidentalomas rises, says Julie Ann Sosa, MD, who heads endocrine surgery at Duke. Experts must evaluate unknown adrenal masses to rule out a pheochromocytoma, a usually benign tumor that can release dangerously high catecholamine levels during biopsy or surgery, and to rule out hypercortisolism and hyperaldosteronism. Adrenal masses can require close monitoring. If an adrenal mass measures more than 4 cm, produces hormones, or grows rapidly, a patient will probably need surgery. PRA is not generally used for malignant adrenal masses. Adrenal masses represent just one type of neoplasia treated by the newly formed Duke endocrine neoplasia group made up of endocrinologists, endocrine surgeons, radiologists, pathologists, oncologists, geneticists, and other specialists. The team works together to diagnose and treat thyroid nodules, thyroid cancer, goiters, overactive parathyroid glands, adrenal tumors, neuroendocrine tumors of the pancreas, and genetic endocrine disorders, including multiple endocrine neoplasia types 1 and 2, says endocrinologist Jennifer Perkins, MD. To refer a patient, call 800-MED-DUKE. (Image above depicts an adrenal gland tumor.) Preventing Unintentional Fraud By Frank Celia One of the hallmarks of the Affordable Care Act era is a heightened focus on billing, audits, and false claims. With this increased focus on oversight, clinicians may be surprised to discover that they run a risk of being accused of financial improprieties, even in the absence of fraudulent intent. Here are a few trending issues that could expose clinicians to the perception of impropriety, potentially warranting extra caution. Laboratory Reimbursement. Some laboratories pay practices to package, collect, or otherwise process specimens, and—in certain cases—to gather specimen-related patient data. Last summer, the Office of Inspector General (OIG) issued a fraud alert warning that such arrangements may violate the anti-kickback statute (ie, the Stark law). “The government is saying this amounts to paying for referrals,” says Alice G. Gosfield, JD, a Philadelphia-based health care attorney. Although reimbursements that stay within “fair market value” are allowed, prevailing fees for such services are so low that it’s probably best to avoid these arrangements altogether. a rigorous audit within a month or two (under new rules, federal overpayments automatically become “false claims” after 60 days). In addition, using the “cut and paste” function during transcription can put practices at legal risk. Many EHR programs allow this function to be shut off, which is an approach recommended by Rachel V. Rose, JD, MBA, a Houston-based attorney. PODs. Last summer, the Department of Justice brought false-claim charges against a physicianowned distributorship (POD) in California. Because these types of companies sell medical devices, the OIG has called them “inherently suspect” under the anti-kickback statute. Additional crackdowns on PODs could also open the door to patient and government lawsuits against hospitals that buy from them. Waiving Co-Pays. Allowing patients to forgo insurance co-pays is riskier than ever. Payers want to ensure that these fees get collected because they discourage patient overutilization. If you decide to waive co-pays, it should be EHR Snafus. As more practices transition to EHRs, a few bugs have started to emerge. For starters, some EHR software programs tend to overbill. If you have a new system, conduct February 2015 done on a case-by-case basis, not routinely. Additionally, make sure to document that the fees were waived because of the patient’s financial needs. 7 A Duke extracorporeal membrane oxygenation machine. Options for Extracorporeal Membrane Oxygenation By Eric Seaborg Duke’s successful program is one of the largest in the country Patients hospitalized with certain heart and lung issues no longer need to struggle with the challenges of remaining bedridden with a ventilator—not even those with conditions severe enough to warrant a transplant. Duke’s extracorporeal membrane oxygenation (ECMO) program offers patients with such issues the ability to stay ambulatory, which provides a variety of benefits. 8 physical therapy or walk around the unit,” says Mani Daneshmand, MD, a cardiovascular and thoracic surgeon. “We had one patient who was practically jogging through the unit on ECMO.” Essentially a portable version of a heart-lung machine, ECMO provides many advantages over ventilators, which require a breathing tube and operate with a high level of pressure that can damage the lungs. ECMO patients can be awake and active while the machine takes over the functions of the lungs or both the heart and lungs. This level of portability also means that patients can be transported safely to Duke from hospitals that offer ventilator-style treatment only. Daneshmand cites the case of a patient who could not get off the heart-lung machine after heart surgery. The patient’s heart surgeon said that nothing more could be done. “We put the patient on ECMO, then transported and took the patient to the operating room,” Daneshmand says. The patient was back at home less than 1 month later. The 20-pound machine can be placed on a cart to accompany a mobile patient. “Patients can do The Duke ECMO team can transport patients from anywhere in North Carolina, southern Virginia, and Clinical Practice Today from Duke Medicine northern South Carolina via Life Flight ground transport, and some patients have also arrived by air. During transport, the patient receives comprehensive medical support from a 7-person team that includes a surgeon, a perfusionist, nurses, and an emergency medical technician. Daneshmand says that part of Duke’s success can be attributed to surgeons who develop their own unique approaches, particularly regarding placement of cannulas. For instance, in veno-venous ECMO, the machine returns oxygenated blood to a vein to relieve work done by the lungs. Veno-arterial ECMO returns the oxygenated blood to an artery at a physiologic pressure to provide both breathing and hemodynamic support. Duke has a 91% survival-to-discharge rate for adults who use respiratory services only compared with an ELSO benchmark rate of 56%. As with any complex procedure, high volume and collective experience are key ingredients to success. Duke has one of the largest ECMO programs in the country, treating more than 75 patients a year who have a wide variety of conditions. The program has been designated as a Center of Excellence by the Extracorporeal Life Support Organization (ELSO), which sets quality benchmarks that the Duke ECMO program has exceeded. One particularly noteworthy example is Duke’s 91% survival-to-discharge rate for adults who use respiratory services only compared with an ELSO benchmark of 56%. Duke’s overall ECMO outcomes are also well above the averages for other ELSO member institutions (Fig 1). Fig. 1. Survival-to-Discharge Rate for All ECMO Patients. 66% 71% 62% 48% Neonatal & Pediatric ELSO Average Adult Duke ECMO = extracorporeal membrane oxygenation; ELSO = Extracorporeal Life Support Organization. Inclusive of all neonatal, pediatric, and adult ECMO patients. Data from 2008-2012. February 2015 Some institutions return this blood into the femoral artery, and some open the patient’s breastbone to insert a cannula into the aorta. Typically, both methods make it difficult to impossible for a patient to be ambulatory. “At Duke, we make a small incision in the right chest and put all the cannulas in directly through that small incision,” Daneshmand explains. “That does a couple of things. One, it nicely unloads the heart and lungs and gives them time to recover. Two, it puts the blood directly back into the aorta, following the body’s natural flow. Putting it into the femoral artery means the blood has to flow backward.” “The big selling point of our ECMO program is that we have a lot of experience. We can ambulate these patients to prevent their physical debilitation and offer them many options,” Daneshmand adds. “If they don’t recover their heart or lung function, we can transplant them. We can put in mechanical circulatory support, like a left-ventricular assist device (LVAD). We have options that are not available at many other institutions.” Duke surgeons have considerable experience with these options: the lung transplant program is the largest in the country, performing more transplants than any other center in 2013; the LVAD program is the third largest; and the heart transplant center is the fifth largest. 9 Keep Patients Coming Back By Meredith Kleeman Customer loyalty is essential in any business, and thriving medical practices recognize that patient satisfaction is vital to their success. Here are some strategies to enhance the patient experience and keep your valued patients coming back. Deliver Superb Customer Service. Customer service is a crucial component in keeping patients happy, and every interaction during the visit affects the patient experience. “It’s not just about the doctors, it’s about the office,” says Lisa B. Nadler, MD, a physician at Duke Triangle Family Practice. “Everybody’s involved in determining patient satisfaction. If you have good [people] throughout the office, then [patients are] more likely to come back.” Communicate Honestly. Indeterminable wait times are a common frustration among patients. Help ease their frustration by sharing expected wait times. For instance, Nadler’s practice sets up a simple display board in the lobby that lists physician names and expected wait times. “This makes it easier for [patients] to know what to expect,” Nadler says. Thriving medical practices recognize that patient satisfaction is vital to their success. Evaluate Patient Satisfaction. Patient satisfaction surveys are a great way to determine what patients like (and dislike) about your practice. You can develop and administer your own survey or use the survey feature available in some practice management software. Make sure to actually read the surveys, and try to schedule recurring meetings to discuss the results with staff and brainstorm strategies for implementing some of your patients’ suggestions. 10 Clinical Practice Today from Duke Medicine Set Realistic Expectations. Another common complaint among patients is how long it takes to get in touch with front-desk staff. “Setting realistic expectations for people is key,” Nadler says. Consider adding an anticipated returncall time frame to the office’s outgoing voice message or implementing an advanced-notice policy for medication refills. Provide Options. Inform unhappy patients that they are welcome to see another physician at the practice or refer them to a different practice. “Patients are going to move around until they find someone who they feel comfortable with, and that’s good!” Nadler explains. “If they don’t feel comfortable with the person, then they’re not going to get the kind of care that they [need].” Slowing the Progression of Diabetic Kidney Disease Approximately 37 million people in the US and Caribbean have type 2 diabetes, and 592 million people worldwide are projected to have diabetes in 2035. Those who develop kidney disease experience some of the most significant morbidity and mortality risks related to the condition, says Uptal Patel, MD, who directs nephrology research at the Duke Clinical Research Institute. As the incidence of diabetic kidney disease rises, Thomas Coffman, MD, chief of the Duke Division of Nephrology, recommends referring patients to specialists for nephrology care whenever necessary. Indications for referring a patient to a nephrologist include, but are not limited to, the following circumstances: Estimated glomerular filtration rate (eGFR) < 30 mL/min/1.73 m2 or progressive decline in eGFR Acute kidney injury Persistent albuminuria or proteinuria Hematuria Hypertension refractory to multiple medications Serum electrolyte abnormality Recurrent kidney stones or hereditary disease. As principal investigator of a new study, Patel is trying to replicate the positive results of a successful Danish trial focused on reducing diabetes-related complications with a novel February 2015 telehealth-based approach. Duke is recruiting 300 patients from 5 of its clinics in the STOP-DKD trial (Simultaneous Risk Factor Control Using Telehealth to Slow Progression of Diabetic Kidney Disease) to study the progression of kidney disease and uncontrolled hypertension. The treatment group will receive a telehealth intervention that covers medication management and risk-factor modification through a combination of self-monitoring and behavioral therapies to slow disease progression (or kidney-function decline). “Of all of the diseases that can lead to kidney disease, diabetes is the biggest problem worldwide, and I believe that it can be better prevented,” says Patel. The STOP-DKD trial is one of several ongoing research trials in the Duke Division of Nephrology, many of which are supported by the Duke O’Brien Center for Kidney Research (DOCK). Coffman says, “even basic research is focused on clinical problems, including diabetic kidney disease.” For example, Duke is studying links between cardiovascular risk and kidney disease, says Coffman, who won the 2014 Excellence Award for Hypertension Research from the American Heart Association. (Image above shows a self-test for glucose.) 11 Gout Is Curable With Proper Intervention Although gout can progress into a debilitating and continually painful condition, the disease can be curable if patients are properly treated from the onset of signs and symptoms. “Many doctors do not think of gout as a chronic, debilitating process,” says Robert Keenan, MD, a rheumatologist who directs the Duke Gout and Crystal Arthropathy Clinic. “They may consider it a disease of flare-ups with no inflammation and normal function in between, but damage continues until a patient may become unable to walk.” During intercritical gout periods when patients are not experiencing flaring, crystals are still present, and inflammatory cells are continuously releasing cytokines and proteases at low levels, which To refer a patient cause joint damage and for treatment or trials, disability. call 800-MED-DUKE Timely Detection and Treatment Gout responds to the right treatment at the right time delivered in the right way, Keenan says. He explains that catching the disease as early as 12 Clinical Practice Today from Duke Medicine possible and managing it appropriately can lead to a cure. Most patients can be managed with dietary changes at first (eg, a low-purine diet in which patients avoid organ meats, shrimp, and beer) combined with pharmacologic therapy. Diet measures alone are often ineffective long term. Patients with gout symptoms and pain should be referred for specialty care if uric acid levels cannot be lowered to below 6 mg/dL (normal is between 3.5 and 7.2 mg/dL) or if uric acid levels are below 6 mg/dL but patients still have flaring. Pharmacologic Options The Duke Division of Rheumatology and Immunology has been a leader in gout treatment, as illustrated by the approval of Krystexxa (pegloticase). In 1993, Michael S. Hershfield, MD, began developing the compound, an orphan drug, for late-stage gout. Clinical trials were conducted at Duke, and the Food and Drug Administration approved the drug in 2010 for intractable cases. New trials are available at Duke and will begin Feb. 2015. Duke may also participate in phase 1 and phase 2 trials for potential new gout treatments. (Image above depicts the foot of a patient with gout.) Brachytherapy Improves Cervical Cancer Care Compared with traditional treatment alone, gynecologic brachytherapy has been shown to extend survival for patients with cervical cancers. This technique involves brief exposure to intracavity or interstitial high-dose radiation. Although the standard for treating cervical cancer is external-beam radiation therapy (EBRT), “there are fewer side effects with brachytherapy, so studying the optimal usage for brachytherapy is important for best practice,” says Junzo Chino, MD, a gynecologic brachytherapy specialist at Duke, one of the few places in North Carolina that offers such services. A 2013 population-based analysis, published in the International Journal of Radiation Oncology (Red Journal) in September, found that brachytherapy use was associated with improved cause-specific survival and overall survival in patients with cervical cancer. In a matched cohort, brachytherapy was associated with higher 4-year cause-specific survival (CSS, 64.3% vs. 51.5%; P < 0.001) and overall survival (OS, 58.2% vs. 46.2%; P < 0.001) compared with EBRT alone. The study examined results for 7,359 patients with stages IB2-IVA cervical cancer. Interestingly, the researchers observed a decline February 2015 in the use of brachytherapy: it was implemented in 83% of cases in 1988 but just 58% of cases in 2009, hitting a low in 2003 of 43%. The authors concluded that because brachytherapy use independently led to higher survival rates, the therapy “should be implemented in all feasible cases.” Given that recommendation, it is fitting that gynecologic brachytherapy practice is now becoming more formalized with the publication of new guidelines. The American Brachytherapy Society has released three guidelines for locally advanced carcinoma of the cervix as well as guidelines for adjuvant vaginal-cuff brachytherapy after hysterectomy and interstitial brachytherapy for vaginal cancer. Chino stresses that brachytherapy and EBRT could each be used against various cancers, depending on the region and stage. For example, if the location of the intrauterine channel is insufficient to cover the area of disease to be treated, doctors can insert interstitial catheters to direct the dose and create customized implants for patients. The careful use of imaging such as an ultrasound, MRI, and computed tomography is currently being evaluated in clinical trials at Duke to spare normal, sensitive tissue, such as bladder. (Image above depicts carcinoma of the cervix.) 13 Closing the Gap on Unpaid Patient Balances By Shelly K. Schwartz As much as you may enjoy helping patients, you can’t afford to do it for free. “With the rise in high-deductible plans and self-pay patients, practices are having to operate a lot differently than they used to,” says Tamra Swindoll, president of Catalyst Consulting in Austin, Texas. Personal Communication The best-performing practices, says Swindoll, contact patients who don’t respond to reminder notices of overdue bills. “In this day of technology and automated payment systems, sometimes you still can’t replace the good old live conversation,” she notes, adding that a call can shed light on what would have otherwise been assumed. Payment Options Practices must also make every effort to collect what they can at the point of care, recommends Jamie Claypool, a medical practice consultant with J. Claypool Associates in Spicewood, Texas. “Give patients as many payment options as possible, including credit card, check, and thirdparty financing through groups like CareCredit.” Written Documentation Claypool also says that all medical practices should ask patients to sign a written collection policy that 14 Clinical Practice Today from Duke Medicine clearly delineates what they can expect from your office and what you expect from them (eg, confirmation of eligibility prior to appointments or a 25% up-front deposit for surgeries). Your patients, in turn, must agree to pay their balances on time. The written policy should also indicate when an unpaid bill will be sent to a collection agency. Estimated Costs At the same time, says Claypool, provide patients with estimates ahead of time for how much their office visit or procedure will cost. “Good eligibility information from the start gives patients the opportunity to accept or deny care based on their ability to pay,” explains Carol Gibbons, another consultant with Catalyst Consulting. Standard Fees In cases where co-pays and deductibles cannot be determined ahead of time, Claypool suggests that practices collect a standard visit fee. “If you don’t know how much to collect, at least get something,” she says. “Co-pays and deductibles are higher now, so have a standard amount that you charge for all visits and settle up later with a refund if necessary.” Ultimately, practices that hope to minimize unpaid balances should set expectations that out-of-pocket fees will be collected at every visit. New Treatment for Wet Macular Degeneration A new therapeutic approach is available for treatment-resistant wet macular degeneration, a form of advanced age-related macular degeneration that affects people older than 50 years. The disease starts as dry macular degeneration in which abnormal deposits called “drusen” form under the retina. Patients experience gradual vision loss; significant vision loss may take 25 years. Some patients develop a more-severe form called wet macular degeneration in which an abnormal blood vessel grows underneath the macula, leading to plasma leakage, bleeding, and scarring. With early diagnosis, wet macular degeneration can be treated with ocular injections of medications that block vascular endothelial growth factor (VEGF), and sudden, severe vision loss can be avoided. “Long-term treatment with anti-VEGF medications is effective for disease control,” says Duke ophthalmologist, immunologist, and retina expert Scott Cousins, MD, who serves as director of the Duke Center for Macular Diseases. “However, between 25% and 40% of patients have an incomplete response and remain at risk of vision loss.” Retina specialists at the Duke Eye Center have initiated a pilot clinical study for patients who February 2015 don’t respond to anti-VEGF therapy. This approach involves adding Visudyne (verteporfin; manufactured by Bausch + Lomb) photodynamic therapy (PDT) to standard treatment. Duke pioneered the use of PDT and developed retinal imaging technology called indocyanine green angiography (ICG) as a biomarker of disease type to identify patients who may be candidates for PDT. PDT, which was previously approved for treating wet macular degeneration, involves infusing a light-activatable medication (Visudyne) into a peripheral blood vein. The doctor then applies a “cold” laser (to avoid thermal damage) to the abnormal blood vessel in the back of the eye to activate the medication and block blood flow to that vessel. “Because the ICG biomarker also tells us about the exact size and location of the blood vessel, we can use it to selectively target the vessel while limiting any effects on normal blood flow,” says Prithu Mettu, MD, an ophthalmologist and retina specialist at Duke who is co-leading the study with Cousins. About two-thirds of treatment-resistant patients who receive PDT benefit from it, Cousins says. (Image above shows an angiogram of a patient with age-related macular degeneration.) 15 Duke Medicine DUMC 3687 Durham, NC 27710 Non-profit Org. U.S. Postage PA I D Durham, NC Permit No. 60 800-MED-DUKE Readership Survey—5 minutes could win you $500! We hope you have been enjoying your complimentary subscription to Clinical Practice Today from Duke Medicine. Do you have comments, suggestions, or ideas? If so, we’d love to hear from you! This survey should take about 5 minutes. Please answer the questions and submit your completed survey to us via fax at 866-419-5789, mailed in an envelope to 5523 Research Park Drive, Suite 210, Baltimore, MD 21228, or online at ClinicalPracticeToday.com/survey. Upon receipt of the completed survey, you will be entered into a drawing to win a $500 American Express gift card. Entry deadline: February 27, 2015. The winner will be notified via email. 1)_ On a scale of 1 to 5 (1 = strongly disagree; 5 = strongly agree), please rate your agreement with the following statements: __ I enjoy reading Clinical Practice Today 2)_ As a result of reading Clinical Practice Today, what actions have you taken? (Select all that apply.) __ I have shared an article with colleagues __ I have implemented recommended practice changes __ I have called a phone number for more information __ I have visited DukeMedicine.org __ I have made a referral to a Duke Medicine doctor __ I have recommended Duke Medicine services to a colleague or patient __ O ther: _________________________ __ Managing uncompensated care __ Medicare reimbursement and reform updates __ Physician-patient communication __ Diabetes and endocrinology __ Ear, nose, and throat __ Gastroenterology and GI surgery __ Geriatrics __ Gynecology __ Nephrology __ Neurology and neurosurgery __ Clinical trials __ Ophthalmology __ New and updated national guidelines __ Orthopaedics __ Research updates __ Pulmonology __ Technology in medicine __ Rheumatology __ Translational science __ Urology __ Q&As or profiles of thought leaders __ Other: _________________________ 4)_ Would you recommend Duke Medicine to your patients? __ Yes __ No __ Unsure 6) _Please name up to five hospitals that you believe provide the best care in ________________ (your specialty) for patients who have the most challenging conditions or who need particularly difficult procedures. (Do not consider location or cost.) 5) _Have you referred patients to any Duke Medicine services in the past year? __ Yes __ No __ Unsure If yes to Q5, which service(s)? (Select all that apply.) __ Cancer __ Cardiology and heart surgery a.______________________________ b.______________________________ c.______________________________ d.______________________________ e.______________________________ Name______________________________________________ Email__________________________________________ TEAR ALONG DOT TED LINE __ The information in Clinical Practice Today helps me in the management of my practice and patients __ Clinical Practice Today has increased my interest in using Duke Medicine for my patients’ care hich topics would you be interested in 3)_ W reading about in future issues of Clinical Practice Today? (Select all that apply.) __ Reducing operating expenses
© Copyright 2026