a three-label segmentation
Automatic Localized Analysis of
Longitudinal Cartilage Changes
Liang Shan
Department of Computer Science
UNC Chapel Hill
Supported through: NIH NIAMS R21-AR059890
Automatic Quantitative Analysis of MR Images of the Knee in Osteoarthritis
1
Introduction - Osteoarthritis (OA)
• Prevalent among adults
2
Introduction - Osteoarthritis (OA)
• Prevalent among adults
• Loss of cartilage
Eroding
cartilage
Exposed bone
Bone
spurs
Eroding
meniscus
Source: http://healthruby.com/osteoarthritis
3
Introduction - Osteoarthritis (OA)
• Prevalent among adults
• Loss of cartilage
Eroding
cartilage
Exposed bone
Bone
spurs
Eroding
meniscus
Source: http://healthruby.com/osteoarthritis
Source: Gray's Anatomy of the Human Body
4
Introduction - Osteoarthritis (OA)
• 2D radiographs to study joint space width
– Not sensitive to 3D localized cartilage loss
Source: Graverand et al. 2009
5
Introduction - Osteoarthritis (OA)
• Datasets of 3D MR images
– Osteoarthritis Initiative (OAI): 4796 × 5
– Pfizer Longitudinal Study (PLS): 155 × 5
Coronal (front) view of 3D MR image
Sagittal (side) view of 3D MR image
6
Introduction - OA analysis
Thickness analysis
OA vs. healthy subjects
0.30
1.00
0.15
0.75
0.50
0.00
0.25
0.15
0.00
0.25
0.30
0.50
0.45
0.75
1.00
0.60
Thickness (mm)
Thickness
(mm)
Cartilage segmentation
7
Introduction - Cartilage segmentation
• Challenges
– Small and thin è Difficult to fully automate
Only 6-10 voxels thick at the thickest location
8
Introduction - Cartilage segmentation
• Challenges
– Small and thin è Difficult to fully automate
Folkesson et al. (2007)
Fripp et al. (2010)
Tamez-Pena et al. (2012)
Yin et al. (2010)
139 images
20 images
12 images
60 images
Methods so far typically validated on small datasets
9
Introduction - Cartilage segmentation
• Challenges
– Small and thin è Difficult to fully automate
– Touching è Difficult to separate
10
Introduction - Cartilage segmentation
• Challenges
– Small and thin è Difficult to fully automate
– Touching è Difficult to separate
– Regularization è Shorter than expected
11
Introduction - Cartilage segmentation
• Challenges
L
Time
Thickness
Thickness
– Small and thin è Difficult to fully automate
– Touching è Difficult to separate
– Regularization è Shorter than expected
– Longitudinal analysis è Consistency across time
J
Time
12
Introduction - Cartilage segmentation
• Challenges
Fully-automatic
– Small and thin è Difficult
to fully method
automate
– Touching è Difficult to separate
– Regularization è Shorter than expected
– Longitudinal analysis è Consistency across time
Validate on more than 700 images
An order of magnitude larger than most existing methods
13
Introduction - Cartilage segmentation
• Challenges
Fully-automatic
– Small and thin è Difficult
to fully method
automate
Three-label
segmentation
– Touching è Difficult
to separate
– Regularization è Shorter than expected
– Longitudinal analysis è Consistency across time
L
J
14
Introduction - Cartilage segmentation
• Challenges
Fully-automatic
– Small and thin è Difficult
to fully method
automate
Three-label
segmentation
– Touching è Difficult
to separate
– Regularization è Short
than expected
Customized
regularization
– Longitudinal analysis è Consistency across time
L
J
15
Introduction - Cartilage segmentation
• Challenges
Thickness
L
Time
Thickness
Fully-automatic
– Small and thin è Difficult
to fully method
automate
Three-label
segmentation
– Touching è Difficult
to separate
– Regularization è Short
than expected
Customized
regularization
– Longitudinal analysis è Consistency
time
Longitudinalacross
segmentation
J
Time
16
Introduction - Thickness analysis
• Challenges
– Non-uniform changes
Eroding
cartilage
Exposed bone
Bone
spurs
Eroding
meniscus
Source: http://healthruby.com/osteoarthritis
17
Introduction - Thickness analysis
• Challenges
– Non-uniform changes
Eroding
cartilage
Exposed bone
Bone
spurs
Eroding
meniscus
Source: http://healthruby.com/osteoarthritis
18
Introduction - Thickness analysis
• Challenges
– Non-uniform changes
– Varying thinning locations
Eroding
across subjects
cartilage
Exposed bone
Bone
spurs
Eroding
meniscus
Source: http://healthruby.com/osteoarthritis
19
Introduction - Thickness analysis
Sub-regional analysis is problematic
Weight-bearing region
of femoral cartilage
Eroding
cartilage
Exposed bone
Bone
spurs
Full tibial cartilage
Image source: Eckstein et al.
Eroding
meniscus
Source: http://healthruby.com/osteoarthritis
20
Introduction - Thickness analysis
0.30
0.15
0.00
0.15
0.30
0.45Eroding
cartilage
0.60
0.30
0.15
0.00 Bone
0.15spurs
0.30
0.45
0.60
Weight-bearing region
of femoral cartilage
Exposed bone
Thickness (mm)
Thickness (mm)
1.00
0.75
0.50
0.25
0.00
0.25
0.50
0.75
1.00
Thickness (mm)
Localized analysis is proposed
Full tibial cartilage
Source: http://healthruby.com/osteoarthritis
Eroding
meniscus
21
Thesis statement
• Automatic, robust and accurate cartilage segmentations
can be obtained through multi-atlas-based registration
and local tissue classification within a three-label
segmentation framework allowing for spatial and
temporal regularization.
• Spatially transforming cartilage thickness maps into an
atlas space enables statistical analysis on localized
cartilage changes.
• Clustering of OA subjects improves statistical analysis
due to the spatial heterogeneity of cartilage loss.
22
Overview
• Introduction
– Osteoarthritis
– Challenges and contributions
• Thesis
– Three-label segmentation method
– Automatic Cartilage segmentation method
– Localized analysis of cartilage changes
• Conclusion and future work
23
Image segmentation
• Two representations
Volumetric labeling
Contour/surface separating
foreground from background
24
Image segmentation
• Convexity vs. non-convexity
non-convex
non-convex
local min
global min
Initial contour
Final contour
convex
convex
global min
Initial contour
Source: Bresson et al.
Final contour
25
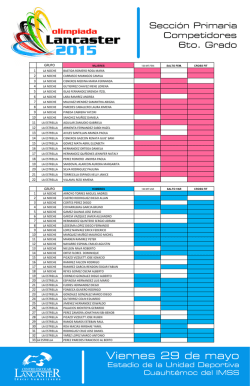
Three-label segmentation
• Binary segmentation is problematic for touching
objects
Binary segmentation
of two touching bones
Three-label segmentation
of two touching bones
26
Three-label segmentation
Black: 0
White: 1
u
l=0
l=1
l=2
l=3
label
27
Three-label segmentation
Black: 0
White: 1
u
l=0
l=1
l=2
l=3
label
| ∇l u |
28
Three-label segmentation
Black: 0
White: 1
u
l=0
l=1
l=2
l=3
label
| ∇l u |
29
Three-label segmentation
Black: 0
White: 1
u
l=0
l=1
l=2
l=3
label
| ∇l u |
30
Three-label segmentation
Binary segmentation
l ∈ {0,1}
⎧1 if Λ( x) = 1
w( x) = ⎨
⎩0 otherwise
Multi-label segmentation
l ∈{0,1,.., L − 1}
⎧ 1 if Λ( x) < l
u ( x, l ) = ⎨
⎩0 otherwise
31
Three-label segmentation
• Minimize energy
Spatial
regularization
Data cost
32
Three-label segmentation
• Minimize energy
Spatial
regularization
Data cost
Non-convex
33
Three-label segmentation
• Minimize energy
Spatial
regularization
Data cost
Non-convex
Relax the constraint to a continuous range
34
Three-label segmentation
• Minimize energy
Spatial
regularization
Data cost
Convex
Global optimal solution to the relaxed problem
Global optimal solution to the original discrete problem
35
Three-label segmentation
Original image
Segmentation
Minimize energy
36
Three-label segmentation
Original image
Segmentation w/
isotropic regularization
Minimize energy
37
Three-label segmentation
Original image
Segmentation w/
isotropic regularization
Segmentation w/
anisotropic regularization
Minimize energy
38
Overview
• Introduction
– Osteoarthritis
– Challenges and contributions
• Thesis
– Three-label segmentation method
– Automatic Cartilage segmentation method
– Localized analysis of cartilage changes
• Conclusion and future work
39
Cartilage segmentation
• Apply three-label segmentation
• Data cost is critical for a good segmentation
• Atlas-based methods
– Popular and successful in brain imaging
40
Atlas-based segmentation
• Atlas
– Structural image + corresponding segmentation
• Use an atlas to achieve a new segmentation
– Image registration + label propagation
Spatial transform
Atlas
Query image
41
Atlas-based segmentation
• Single-atlas-based segmentation
– One registration è Not robust to registration failures
– Might not be anatomically representative
Spatial transform
Single atlas
Query image
42
Atlas-based segmentation
• Average-shape-atlas-based segmentation
– One registration è Not robust to registration failures
– Choice of reference image
Average-shape atlas
Query image
43
Atlas-based segmentation
• Multi-atlas-based segmentation
– Multiple registrations è Robust to registration failures
– Anatomical variations
– High computation cost
Spatial transform
Atlases
Label fusion
Transformed atlases
Query image
44
Label fusion
• Majority voting
1/n, 1/n, 1/n, …
45
Label fusion
• Majority voting
• Locally-weighted fusion
0.12
0.02
0.05
0.31
0.42
0.45
0.01
0.24
0.25
0.28
0.11
0.26
0.25
0.71
0.46
0.13
0.71
0.03
0.32
0.07
0.14
0.62
0.07
0.54
0.01
0.45
0.11
46
Label fusion
• Majority voting
• Locally-weighted fusion
ATCH-BASED LABEL PROPAGATION
• Non-local patch-based fusion
Principle
UPERVISED PATCH-BASED APPROACH FOR HUMAN BRAIN LABELING
1853
Local robust to
registration errors
des et al. [6] have proposed a very efficient dem relying on a nonlocal framework. Since then,
ategy has been studied and applied in several
g applications such as nonlocal regularization
e context of inverse problems [20], [27], [14],
dical image synthesis [32].
r, over the image domain , a weighted graph
er the voxels of the input image with a weight
. This weighted graph is a representation
larities in the input image .
nlocal graph is used for denoising purpose
hood averaging strategy [called nonlocal means
Rousseau et al.
47
Cartilage segmentation
• Bone segmentation is relatively easy
• Help to locate cartilage
48
Cartilage segmentation
• Bone segmentation is relatively easy
• Help to locate cartilage
49
Multi-atlas registration
Atlas of
whole
image
Three-label segmentation
Atlas of
joint
region
Extract joint region
Multi-atlas
registration
Three-label segmentation
50
Cartilage segmentation
Three-label segmentation with anisotropic regularization
Local Spatial
likelihoods priors
51
Cartilage segmentation
• Average-shape-atlas spatial priors
• Multi-atlas-based spatial priors
– Majority voting
– Locally-weighted label fusion
– Non-local patch-based label fusion
Average
bone/cartilage atlas
52
Cartilage segmentation
• Local likelihoods
– 3 classes: femoral and tibial cartilage, background
– 15 local features
– Probabilistic SVM
Source: Wikipedia
53
Validation
• PLS dataset
– 155 subjects (81 healthy, 74 OA), 706 images
– baseline, 3, 6, 12, 24-month
– Expert cartilage segmentations available
– Weight-bearing femoral cartilage
– Full tibial cartilage
– Expert bone segmentations available to 18 images
54
Bone validation
• Validation on 18 images with leave-one-out
• Dice similarity coefficient
Femur
0.99
0.98
0.98
0.97
DSC
0.97
DSC
Tibia
0.96
0.95
0.96
0.95
0.94
0.94
0.93 g = 0.0
g = 0.5
g = 1.0
Spatial regularization
0.93 g = 0.0
g = 0.5
g = 1.0
Spatial regularization
55
Cartilage validation
• Compare different atlases
All use three-label segmentation with anisotropic regularization
Tibial cartilage
0.76
0.840
0.75
0.832
DSC
DSC
Femoral cartilage
0.74
0.73
0.72
0.0
AA
MV
0.816
LW
PB
0.5
1.0
1.5
Spatial regularization
0.824
2.0
0.808
0.0
AA
MV
LW
PB
0.5
1.0
1.5
Spatial regularization
2.0
56
Cartilage validation
• Compare different regularization methods
Isotropic
regularization
Anisotropic
regularization
Expert
segmentation
57
Cartilage validation
• Compare different regularization methods
All use non-local patch-based label fusion for spatial priors, alpha = 0.2
Femoral cartilage
Tibial cartilage
0.84
0.750
0.83
DSC
DSC
0.725
0.700
0.675
0.650
0.0
1.0
1.5
Spatial regularization
0.81
0.80
Isotropic
Anisotropic
0.5
0.82
2.0
0.79
0.0
Isotropic
Anisotropic
0.5
1.0
1.5
2.0
Spatial regularization
58
Cartilage validation
• Compare with other methods
100 training images
50 test images
59
Cartilage validation
• Compare with other methods
– 5/16 but as good as the top-ranking method
Femoral cartilage
Rank8
Rank7
Rank6
Rank8
Rank7
Rank6
Ours
Rank4
Rank3
0.4
Rank2
0.5
Ours
0.6
Rank4
0.7
Rank3
DSC
0.8
Rank1
DSC
0.9
0.95
0.90
0.85
0.80
0.75
0.70
0.65
0.60
Rank2
1.0
Rank1
Tibial cartilage
60
Longitudinal three-label segmentation
• Encourage temporal consistency
61
Longitudinal three-label segmentation
• Encourage temporal consistency
Spatial
regularization
Temporal
regularization
62
Longitudinal three-label segmentation
• Encourage temporal consistency
Spatial
regularization
Temporal
regularization
Longitudinal
images
Longitudinal
segmentation
63
Cartilage validation
• DSC similar to independent segmentation
• Temporal consistency measure (TCM)
12000
10000
10000
8000
6000
TCM
TCM
8000
4000
2000
0
6000
4000
2000
Expert
Independent Longitudinal
Femoral cartilage
0
Expert
Independent Longitudinal
Tibial cartilage
64
Overview
• Introduction
– Osteoarthritis
– Challenges and contributions
• Thesis
– Three-label segmentation method
– Automatic Cartilage segmentation method
– Localized analysis of cartilage changes
• Conclusion and future work
65
Cartilage thickness analysis
3D knee MRI!
Native image space!
Common atlas space!
2D thickness map
3D segmentation! 3D thickness map! 3D thickness map! 2D thickness map!
(b)!
(a)!
(c)!
(d)!
66
67
68
69
70
Cartilage thickness analysis
• Questions of interest
– significant difference of baseline thickness
between OA and normal control subjects
– significant difference of longitudinal thickness
change between OA and normal control subjects
• Approach
– Group OA subjects into clusters based on their
thinning patterns
71
Cartilage thickness analysis
Normal
control
subject
OA
subject #1
OA
subject #2
72
Cartilage thickness analysis
Normal
control
subject
Undermine statistical analysis
Need to discover subgroups
OA
subject #1
OA
subject #2
73
Cartilage thickness analysis
• Pixel-wise regression using linear mixed-effects
models for normal control and OA groups
Thickness = Baseline thickness + Change rate × Time
Thickness
NC subjects
OA subjects
Time
74
Cartilage thickness analysis
• Pixel-wise regression using linear mixed-effects
models for normal control and OA groups
Thickness = Baseline thickness + Change rate × Time
Thickness
Subject #1
Group mean
Subject #3
Time
Subject #2
75
Cartilage thickness analysis
• Pixel-wise regression using linear mixed-effects
models for normal control and OA groups
Thickness = Baseline thickness + Change rate × Time
Deviation from group mean called random effects
Thickness
Random effects
Fixed effects
Random effects
Time
Random effects
76
Cartilage thickness analysis
• Pixel-wise regression using linear mixed-effects
models for normal control and OA groups
Thickness = Baseline thickness + Change rate × Time
• Cluster OA subjects based on random effects
Cartilage thickness analysis
• Pixel-wise regression using linear mixed-effects
models for normal control and OA groups
Thickness = Baseline thickness + Change rate × Time
• Cluster OA subjects based on random effects
• Group difference between each OA cluster versus
normal control group
• Expect more significant difference after clustering
than before clustering
Difference of baseline thickness
between normal control and OA subjects
for weight-bearing region of femoral cartilage
79
p-values are corrected for multiple comparisons
log10(p)
1.2
1.0
0.8
0.6
0.4
0.2
0.0
1.6
1.4
1.2
1.0
0.8
0.6
0.4
0.2
0.0
80
log10(p)
Thickness (m
1.00
0.75
0.50
0.25
0.00
0.25
0.50
0.75
1.00
Thickness (mm)
M
0.08
0.00 clustering
Before
0.08
L 0.16
0.24
0.32
p-values are corrected for multiple comparisons
log10(p)
log10(p)
1.2
1.0
0.8
0.6
1.6
0.4
1.4
0.2
1.2
0.0
1.0
0.8
0.6
0.41.6
0.21.4
0.01.2
1.0
0.8
0.6
0.4
0.2
0.0
81
log10(p)
Thickness (m
Thickness (mm)
Cluster
#1
Thickness (mm)
M
0.08
0.00 clustering
Before
0.08
L 0.16
0.24
0.6
0.32
0.3
After
0.0 clustering
0.3
0.6
0.9
1.2
1.00
1.5
0.75
0.50
0.25
0.00
0.25
0.50
0.75
1.00
p-values are corrected for multiple comparisons
log10(p)
log10(p)
82
log10(p)
Thickness (m
1.2
1.0
0.8
0.6
1.6
0.4
1.4
0.2
1.2
0.0
1.0
1.6
0.8
1.4
0.6
1.2
0.41.6
1.0
0.21.4
0.8
0.01.2
0.6
1.0
0.4
0.8
0.2
0.6
0.0
0.4
0.2
0.0
log10(p)
Cluster
#2
ThicknessThickness
(mm) (mm)
Cluster
#1
Thickness (mm)
M
0.08
0.00 clustering
Before
0.08
L 0.16
0.24
0.6
0.32
0.3
After
0.0 clustering
0.40
0.3
0.6
0.32
0.9
0.24
1.2
0.16
1.00
1.5
0.75
0.08
0.50
0.00
0.25
0.08
0.00
0.25
0.16
0.50
0.75
1.00
Cluster
#3
p-values are corrected for multiple comparisons
log10(p)
log10(p)
Thickness (m
1.2
1.0
0.8
0.6
1.6
0.4
1.4
0.2
1.2
0.0
1.0
1.6
0.8
1.4
0.6
1.2
0.41.6
1.0
0.21.4
1.6
0.8
0.01.2
1.4
0.6
1.0
1.2
0.4
0.8
1.0
0.2
0.6
0.8
0.0
0.4
0.6
0.2
0.4
0.0
0.2
0.0
log10(p)
log10(p)
log10(p)
Cluster
#2
Thickness
Thickness
(mm)
Thickness
(mm) (mm)
Cluster
#1
Thickness (mm)
M
0.08
0.00 clustering
Before
0.08
L 0.16
0.24
0.6
0.32
0.3
After
0.0 clustering
0.40
0.3
0.6
0.32
0.9
0.24
1.2
0.16
1.00
1.5
0.75
0.30
0.08
0.50
0.00
0.15
0.25
0.08
0.00
0.00
0.25
0.16
0.15
0.50
0.30
0.75
1.00
0.45
0.60
83
log10(p)
log10(p)
log10(p)
log10(p)
log10(p)
1.2
1.0
0.8
0.6
1.6
0.4
1.4
0.2
1.2
0.0
1.0
1.6
0.8
1.4
0.6
1.2
0.41.6
1.0
0.21.4
1.6
0.8
0.01.2
1.4
0.6
1.0
1.2
0.4
0.8
1.0
0.2
1.60.6
0.8
0.0
1.40.4
0.6
1.20.2
0.4
1.00.0
0.2
0.8
0.0
0.6
0.4
0.2 84
log10(p)
Thickness (mm)
Thickness
Thickness
(mm)
Thickness
(mm) (mm)
Thickness (mm)
Thickness (m
0.08
0.00 clustering
Before
0.08
M
L 0.16
0.24
0.6
0.32
0.3
After
0.0 clustering
0.40
0.3
Cluster
0.6
0.32
0.9
#1
0.24
1.2
0.16
1.00
1.5
0.75
Cluster
0.30
0.08
0.50
0.00
0.15
#2
0.25
0.08
0.00
0.00
0.25
0.16
0.15
0.2
Cluster
0.50
0.00.30
0.75
#3
0.2
1.00
0.45
0.4
0.60
0.6
Cluster
0.8
#4
1.0
1.2
p-values are corrected for multiple comparisons
Difference of thickness change rate
between normal control and OA subjects
for weight-bearing region of femoral cartilage
85
p-values are corrected for multiple comparisons
1.6
1.4
1.2
1.0
0.8
0.6
0.4
0.2
0.0
86
log10(p)
0.042
0.036
0.030
0.024
0.018
0.012
0.006
0.000
log10(p)
Change rate (mm
0.5
0.4
0.3
0.2
0.1
0.0
0.1
0.2
0.3
0.4
0.5
Change rate (mm/year)
M
0.02
Before
0.00clustering
0.02
L
0.04
0.06
p-values are corrected for multiple comparisons
log10(p)
log10(p)
0.042
0.036
0.030
0.024
0.018
1.6
0.012
1.4
0.006
1.2
0.000
1.0
0.8
0.6
0.4
1.6
0.2
1.4
0.0
1.2
1.0
0.8
0.6
0.4
0.2
0.0
log10(p)
Cluster
#1
Change rate (mm/year)
Change rate (mm/year)
Change rate (mm
M
0.02
Before
0.00clustering
0.02
L
0.20.04
0.00.06
After 0.2
clustering
0.4
0.6
0.8
1.0
0.5
1.2
0.4
1.4
0.3
0.2
0.1
0.0
0.1
0.2
0.3
0.4
0.5
87
log10(p)
log10(p)
0.042
0.036
0.030
0.024
0.018
1.6
0.012
1.4
0.006
1.2
0.000
1.0
0.8
0.120
0.6
0.105
0.4
0.090
1.6
0.2
0.075
1.4
0.0
0.060
1.2
0.28
0.045
1.0
0.24
0.030
0.8
0.20
0.015
0.6
0.16
0.000
0.27
0.4
0.12
0.24
0.2
0.08
0.21
0.0
0.18
0.04
0.15
0.00
0.12
0.09
0.06
88
0.03
log10(p)
log10log
(p)10(p)log10(p)
Change rate (mm/year)
Change rate (mm/year)
Change rate (mm/year)
Change rate (mm
Change rateChange
(mm/year)
rate (mm/year)
0.02
Before
0.00clustering
0.02
M
L
0.20.04
0.00.06
After 0.2
clustering
0.4
0.6
Cluster
0.075
0.8
0.050
#1
1.0
0.025
0.5
1.2
0.000
0.4
1.4
0.100
0.025
0.3
Cluster
0.20.050
0.075
#2
0.10.075
0.050
0.00.100
0.025
0.1
0.125
0.12
0.000
0.2
Cluster
0.3
0.08
0.025
#3
0.4
0.04
0.050
0.5
0.00
0.075
0.04
Cluster
0.08
#4
0.12
0.16
p-values are corrected for multiple comparisons
Differences of baseline thickness and
thickness change rate between normal control
and OA subjects for tibial cartilage
89
Overview
• Introduction
– Osteoarthritis
– Segmentation challenges
– Statistical analysis challenges
• Thesis
– Three-label segmentation method
– Automatic Cartilage segmentation method
– Localized analysis of cartilage changes
• Conclusion and future work
90
Contributions
Thickness
• Propose a three-label segmentation method
Time
91
Contributions
• Propose a three-label segmentation method
• Propose an automatic multi-atlas-based cartilage
segmentation method
92
Contributions
• Propose a three-label segmentation method
• Propose an automatic multi-atlas-based cartilage
segmentation method
• Validation of the segmentation method
– 706 images from PLS dataset
– 50 images from SKI10 dataset
– An order of magnitude larger than other methods
93
Contributions
0.15
0.00
0.15
0.30
0.45
0.60
Thickness (mm)
0.15
0.00
0.15
0.30
0.45
0.60
Thickness (mm)
• Propose a three-label segmentation method
• Propose an automatic multi-atlas-based cartilage
segmentation method
• Validation of the segmentation method
• Establish spatial correspondences
0.30
0.30
94
Contributions
• Propose a three-label segmentation method
• Propose an automatic multi-atlas-based cartilage
segmentation method
• Validation of the segmentation method
• Establish spatial correspondences
• Propose a new clustering-based method to
analyze cartilage changes
• Statistical analysis on the PLS dataset
95
Thesis statement
• Automatic, robust and accurate cartilage segmentations
can be obtained through multi-atlas-based registration
and local tissue classification within a three-label
segmentation framework allowing for spatial and
temporal regularization.
• Spatially transforming cartilage thickness maps into an
atlas space enables statistical analysis on localized
cartilage changes.
• Clustering of OA subjects improves statistical analysis
due to the spatial heterogeneity of cartilage loss.
96
Future work
•
•
•
•
Application to the OAI dataset
Atlas selection
Neighborhood dependence in statistical analysis
Including more patient information
97
Publications
• [1] Chao Huang, Liang Shan, Cecil Charles, Marc Niethammer, and Hongtu
Zhu, “Diseased region detection of longitudinal knee MRI data,” IPMI 2013
• [2] Liang Shan, Cecil Charles, and Marc Niethammer, “Longitudinal threelabel segmentation of knee cartilage,” ISBI 2013.
• [3] Liang Shan, Cecil Charles, and Marc Niethammer, “Automatic multi-atlasbased cartilage segmentation from knee MR images,” ISBI 2012.
• [4] Liang Shan, Cecil Charles, and Marc Niethammer, “Automatic atlas-based
three-label cartilage segmentation from MR knee images,” MMBIA 2012.
• [5] Liang Shan, Christopher Zach, and Marc Niethammer, “Automatic threelabel bone segmentation from knee MR images,” ISBI 2010.
• [6] Liang Shan, Christopher Zach, Martin Styner, Cecil Charles, and Marc
Niethammer, “Automatic bone segmentation and alignment from MR knee
images,” SPIE, 2010
• [7] Christopher Zach, Liang Shan, and Marc Niethammer, “Globally optimal
finsler active contours,” DAGM 2009
98
Acknowledgements
• Marc Niethammer, Martin Styner, Steve Pizer, Cecil
Charles and Hongtu Zhu
• Pfizer Longtudinal Study (PLS-A9001140)
• Christopher Zach
• Chao Huang
• Yang Huang, Nikhil Singh, Yi Hong, Xiao Yang, Heather
Couture, Istvan Csapo, Tian Cao and Qingyu Zhao
• Chen-Rui Chou, Joohwi Lee and Qian Wang
• BASS administrators
• Friends, family and Zhipeng Lu
99
© Copyright 2026