Systemic Vascular Load in Calcific Degenerative Aortic Valve Stenosis
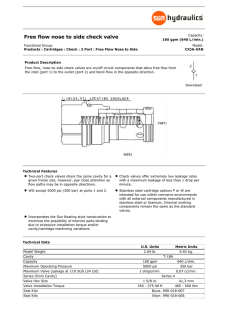
JOURNAL OF THE AMERICAN COLLEGE OF CARDIOLOGY VOL. 65, NO. 5, 2015 ª 2015 BY THE AMERICAN COLLEGE OF CARDIOLOGY FOUNDATION ISSN 0735-1097/$36.00 PUBLISHED BY ELSEVIER INC. http://dx.doi.org/10.1016/j.jacc.2014.10.067 Systemic Vascular Load in Calcific Degenerative Aortic Valve Stenosis Insight From Percutaneous Valve Replacement Raquel Yotti, MD, PHD,* Javier Bermejo, MD, PHD,* Enrique Gutiérrez-Ibañes, MD,* Candelas Pérez del Villar, MD,* Teresa Mombiela, MD,* Jaime Elízaga, MD, PHD,* Yolanda Benito, DCS, DVM,* Ana González-Mansilla, MD, PHD,* Alicia Barrio, DCS, MBIOL,* Daniel Rodríguez-Pérez, PHD,y Pablo Martínez-Legazpi, MENG, PHD,z Francisco Fernández-Avilés, MD, PHD* ABSTRACT BACKGROUND Systemic arterial load impacts the symptomatic status and outcome of patients with calcific degenerative aortic stenosis (AS). However, assessing vascular properties is challenging because the arterial tree’s behavior could be influenced by the valvular obstruction. OBJECTIVES This study sought to characterize the interaction between valvular and vascular functions in patients with AS by using transcatheter aortic valve replacement (TAVR) as a clinical model of isolated intervention. METHODS Aortic pressure and flow were measured simultaneously using high-fidelity sensors in 23 patients (mean 79 7 years of age) before and after TAVR. Blood pressure and clinical response were registered at 6-month follow-up. RESULTS Systolic and pulse arterial pressures, as well as indices of vascular function (vascular resistance, aortic input impedance, compliance, and arterial elastance), were significantly modified by TAVR, exhibiting stiffer vascular behavior post-intervention (all, p < 0.05). Peak left ventricular pressure decreased after TAVR (186 36 mm Hg vs. 162 23 mm Hg, respectively; p ¼ 0.003) but remained at >140 mm Hg in 70% of patients. Wave intensity analysis showed abnormally low forward and backward compression waves at baseline, increasing significantly after TAVR. Stroke volume decreased (21 19%; p < 0.001) and correlated with continuous and pulsatile indices of arterial load. In the 48 h following TAVR, a hypertensive response was observed in 12 patients (52%), and after 6-month follow-up, 5 patients required further intensification of discharge antihypertensive therapy. CONCLUSIONS Vascular function in calcific degenerative AS is conditioned by the upstream valvular obstruction that dampens forward and backward compression waves in the arterial tree. An increase in vascular load after TAVR limits the procedure’s acute afterload relief. (J Am Coll Cardiol 2015;65:423–33) © 2015 by the American College of Cardiology Foundation. C alcific degenerative aortic valve stenosis the symptomatic status and outcome of these pa- (AS) Western tients (1–3). In AS, left ventricular (LV) afterload is countries. For a given degree of valve abnormally high because concentric remodeling and obstruction, systemic arterial properties may impact hypertrophy are insufficient to compensate for the has become endemic in From the *Department of Cardiology, Hospital General Universitario Gregorio Marañón, Instituto de Investigación Sanitaria Gregorio Marañón, and Facultad de Medicina, Universidad Complutense de Madrid, Madrid, Spain; yDepartment of Mathematical Physics and Fluids, Facultad de Ciencias, Universidad Nacional de Educación a Distancia, Madrid, Spain; and the zMechanical and Aerospace Engineering Department, University of California San Diego, San Diego, California. This study was supported by Instituto de Salud Carlos III, Ministerio de Economía y Competitividad, Spain, grants PIS09/02602, PIS012/02878, RD12/0042, CM12/00273 (to Dr. Perez del Villar), and CM11/00221 (to Dr. Mombiela). Drs. Mombiela, González-Mansilla, and del Villar were partially supported by grants from the Fundación para Investigación Biomédica Gregorio Marañón, Spain. Dr. Martínez-Legazpi was supported by U.S. National Institutes of Health grant 1R21 HL108268-01. All other authors have reported that they have no relationships relevant to the contents of this paper to disclose. This work was presented in part at the Scientific Sessions of the American Heart Association, 2012, Los Angeles, California, November 4 to 7; abstract A15474. Manuscript received August 5, 2014; revised manuscript received October 13, 2014, accepted October 21, 2014. Downloaded From: http://content.onlinejacc.org/ on 02/06/2015 424 Yotti et al. JACC VOL. 65, NO. 5, 2015 Systemic Vascular Load in Aortic Stenosis FEBRUARY 10, 2015:423–33 ABBREVIATIONS additive effects of valvular obstruction and AND ACRONYMS vascular load (4). Thus, vascular stiffness may be a source of LV systolic and diastolic AS = aortic stenosis dysfunctions BCW = backward compression wave C = compliance Ea = systemic arterial elastance FCW = forward compression wave in patients with moderate degrees of valve obstruction (3). This mecha- T A B L E 1 Baseline Clinical and Demographic Data (N ¼ 23) 79 7 Age, yrs Female 11 (47) Body surface area, m2 1.68 0.15 NYHA functional class III or IV 9 (39) nism helps explain abnormally high mor- Logistic EuroSCORE 10 7 bidity and mortality rates in patients with Coronary heart disease 10 (43) AS for whom classical obstruction indices Chronic kidney disease 7 (30) fail to predict outcomes (2). Mitral regurgitation (grade > mild) 7 (30) Cardiovascular risk factors SVI = stroke volume index SEE PAGE 434 TAVR = transcatheter aortic valve replacement WIA = wave intensity analysis Hypertension Characterizing intrinsic properties of the arterial tree remains particularly challenging in AS because of the difficulties of uncou- Z = impedance Zc = characteristic impedance 17 (74) Diabetes 11 (48) Dyslipidemia 12 (52) Smoking 4 (17) Taking cardiovascular treatment pling valvular and vascular functions in vivo ACEIs/ARBs 17 (74) (5). Acute and chronic interventions on either Diuretics 17 (73) compartment cause reciprocal changes in the other. For instance, changes in vascular resistance caused by vasodilators (6,7) and exercise (8) induce significant modifications in valve hemodynamics. Likewise, Beta-blockers 9 (39) Aldosterone receptor antagonists 4 (17) Calcium antagonists 2 (9) Nitrates 1 (4) Statins 14 (61) valve interventions may acutely impact arterial Values are mean SD or n (%). function (9). Although attempts have been made to quantify vascular load in AS noninvasively (2,4), a rigorous quantification of arterial hemodynamics ACEIs ¼ angiotensin-converting enzyme inhibitors; ARBs ¼ angiotensin receptor blockers; EuroSCORE ¼ European System for Cardiac Operative Risk Evaluation; NYHA ¼ New York Heart Association. entails simultaneous measurements of central aortic pressure and flow (10). Use of this invasive approach in a small number of subjects has suggested that steady and pulsatile loads are increased in symptomatic degenerative calcific AS, particularly during exercise (8). However, measurements of vascular load might be conditioned by upstream valvular obstruction. This study was designed to characterize the interaction between valvular and vascular function in patients with calcific degenerative AS. We hypothesized that transcatheter aortic valve replacement <40 mm Hg) was present in 9 patients and concomitant low-flow (stroke volume [SV] index of <35 ml/m 2) in 3 patients. Sixteen patients (74%) had a preprocedural diagnosis of hypertension requiring pharmacotherapy. Antihypertensive agents were withheld 12 h before the procedure. After TAVR, patients were initially kept on their pre-procedural antihypertensive therapy. The local Institutional Review Board approved the study protocol and all subjects provided written informed consent. (TAVR) offers a useful clinical model of isolated STUDY valvular intervention to unmask underlying valvular- were performed using the femoral approach under vascular interactions of AS. Therefore, we analyzed local anesthesia and conscious sedation with low the acute changes induced by TAVR to understand doses of midazolam (2 to 5 mg, intravenous) and how valve obstruction impacts vascular function, PROTOCOL AND FOLLOW-UP. Procedures fentanyl (2 m g/kg, intravenous); additional boluses using state-of-the-art methods, including frequency (1 mg and 50 m g, respectively) were used if necessary domain and wave intensity analyses (WIA) of high- to maintain patient comfort during the procedure. fidelity data. Special care was taken to ensure a constant level of sedation during pre- and post-procedural measure- METHODS ments. A pacing wire and a thermodilution SwanGanz catheter were placed in the RV and in the main STUDY POPULATION. We studied 23 consecutive pulmonary artery, respectively. The self-expanding patients with severe symptomatic calcific degenera- valve (Corevalve, Medtronic, Inc., Minneapolis, Min- tive AS undergoing TAVR (Table 1). Patients were nesota) transfemoral implantation procedure (11) was either in sinus rhythm or permanent right ventricular successful in all patients. Mild residual AR was pres- (RV) pacing (n ¼ 3). No patient had significant ent in 10 patients (grade 1 in 9 patients and grade aortic regurgitation (AR), and 7 patients had an ejec- 2 in 1 patient). Aortic and LV pressures were simul- tion fraction of #45%. Low-gradient AS (mean: taneously recorded before and after TAVR, using Downloaded From: http://content.onlinejacc.org/ on 02/06/2015 JACC VOL. 65, NO. 5, 2015 Yotti et al. FEBRUARY 10, 2015:423–33 Systemic Vascular Load in Aortic Stenosis fluid-filled catheters. Aortic valve areas were calcu- Beats were selected for analysis if peak ascending lated using the Gorlin formula. aortic pressure exhibited variation of <10 mm Hg over High-fidelity pressure and flow velocity were the interval examined and the flow velocity wave- recorded simultaneously at the ascending aorta by form was stable and periodic (8). For each hemody- using a 0.014-inch-diameter wire (Combowire, Vol- namic run, 13 beats (range: 5 to 19 beats) underwent cano Corp., San Diego, California) under stable he- digital low-pass (50-Hz) filtering and ensemble aver- modynamic conditions (<10% variation in mean aging (Figure 1) (8,13). The aortic input impedance blood pressure [BP] during $10 min before and $30 spectrum was derived using Fourier decomposition of min after TAVR). To minimize artifacts within the the pressure and velocity signals up to 10 Hz (10). region of pressure recovery, the wire was introduced Respective pressure and flow moduli at each har- though a 6-F multipurpose guiding catheter placed in monic were used to derive the impedance (Z) moduli. the ascending aorta w5 cm above the aortic annulus Characteristic impedance (Zc) was calculated as the (Central micro- average of Z moduli above 4 Hz, excluding outlier manometry sensors located at the wire’s tip were values of >3 times the median. Because this method advanced approximately 1 cm out of the guiding is highly sensitive to signal noise, we additionally Illustration). The Doppler and catheter before data recording. After TAVR, the calculated Z c from wave speed, the latter measured in pressure-velocity wire was reinserted, matching the the time domain from the early P–Q linear relation- tip’s position fluoroscopically stored in the baseline ship, as used for measuring wave velocity (Online study. The pressure signal was balanced against the Appendix). Correlation and agreement for both fluid-filled guiding catheter. Signals were recorded methods for measuring Z c were r ¼ 0.67 and r ic ¼ 0.59, for at least 1 minute during sinus rhythm and then respectively (pooled before and after TAVR data). The during RV pacing at 20 beats/min above intrinsic augmentation index was computed as the difference baseline heart rate in all patients before and after between the maximum and minimum values of Z TAVR. In patients with permanent RV pacing or those components >3 Hz. We calculated the distance to the who were developing new-onset complete atrioven- reflecting site by the quarter-wavelength relationship tricular or left branch bundle block (n ¼ 9), we used (14), as well as by WIA (r ¼ 0.51 and r ic ¼ 0.40 between pacing signals before and after TAVR. High-fidelity methods [Online Appendix]). Arterial compliance (C) pressure, flow velocity, and electrocardiogram sig- was calculated using the pulse pressure method (15), nals were digitally stored at 200 Hz. exponential decay, and diastolic area methods (10) Comprehensive Doppler electrocardiogram exami- (r > 0.92 and r ic $ 0.90, among all methods). We nations were performed immediately before and <24 h calculated effective arterial elastance as: 1) the ratio after TAVR, using broadband 2.0- to 4.0-MHz ma- between end systolic pressure (obtained from the trix and volumetric transducers on a Vivid-7 or a fluid-filled LV pressure catheter) and SV (Ea); and Vivid-9 system (General Electric Healthcare, Little 2) the ratio between systemic vascular resistance Chalfont, United Kingdom). Cuff BP was monitored and the cardiac period (E aR; r ¼ 0.95 and r ic ¼ 0.67 hourly during the first 48 h and then every 8 h until between methods) (16,17). discharge. Hypertensive response after TAVR was WIA is a well-established method used to assess defined (12) in the presence of 1 of the following: arterial hemodynamics (18); its foundations define 1) sustained (>48-h) systolic pressure >140 mm Hg pressure and velocity waveforms as the summation or diastolic pressure >90 mm Hg not present before; of successive infinitesimal waves that propagate 2) need for a >2-fold increase in the dosage of through vessels (18). Arterial waves can originate an antihypertensive drug to achieve BP control; or either from the LV (forward traveling) or from pe- 3) incorporation of an additional antihypertensive ripheral vasculature reflections (backward traveling). drug to the pre-procedural regimen. Patients under- Waves are further classified by their effect on pres- went clinical follow-up, blinded to the results of sure as compression (increased pressure) or expan- vascular hemodynamics, every 3 months during the sion w (decreased pressure) waves. We used the 6 months’ post-procedure. ensemble-averaged pressure and velocity signals to derive the rates of change of aortic pressure (dP/dt) INVASIVE DATA PROCESSING AND ANALYSIS. and velocity (dU/dt) (Figure 1, Online Appendix). It Volumetric flow rate (ml/s) was calculated from linear has been proposed that changes in aortic pressure flow velocity measurements (cm/s) by means of a can be attributed not only to forward or backward calibration constant (cm 2) obtained as K ¼ SV/TVI, wave motion but also to changes in aortic volume where TVI represents the time-velocity integral and (19). Because we anticipated a potential effect of SV is the simultaneously obtained thermodilution SV. TAVR on aortic pressure and volume, we also Downloaded From: http://content.onlinejacc.org/ on 02/06/2015 425 426 Yotti et al. JACC VOL. 65, NO. 5, 2015 Systemic Vascular Load in Aortic Stenosis FEBRUARY 10, 2015:423–33 C EN T RA L IL LUSTR AT I ON Systemic Vascular Load in Aortic Stenosis Aortic impedance and wave intensity analysis are shown in a patient before (A) and after (B) transcatheter aortic valve replacement (TAVR). Aortic systolic and pulse pressures increased after TAVR. Fourier decomposition of the simultaneous aortic pressure and velocity signals shows that SVR and the first 3 harmonic frequencies of the impedance spectrum (Z) increase after TAVR. Wave intensity analysis was used to separate total wave intensity into contributions from the forward (dIwþ) and backward (dIw-) traveling waves. Compression waves (salmon) increase pressure, and expansion waves (green) decrease aortic pressure. The forward compression wave (FCW) increases immediately after TAVR. BCW ¼ backward compression wave; BEW ¼ backward expansion wave; dIw ¼ wave intensity; FEW ¼ forward expansion wave; LA ¼ left atrium; LV ¼ left ventricle; SVR ¼ systemic vascular resistance. Downloaded From: http://content.onlinejacc.org/ on 02/06/2015 JACC VOL. 65, NO. 5, 2015 Yotti et al. FEBRUARY 10, 2015:423–33 Systemic Vascular Load in Aortic Stenosis F I G U R E 1 High-Fidelity Pressure and Flow Velocity Signal Processing 100 400 50 200 Aortic Flow Velocity (cm/s) Aortic Pressure (mm Hg) A 0 0 Time B C 150 D 250 140 140 130 130 120 110 100 90 80 70 Aortic Pressure (mm Hg) 200 Aortic Flow Velocity (cm/s) Aortic Pressure (mm Hg) 150 150 100 120 110 100 90 80 70 50 60 60 0 50 0 500 Time (ms) 1000 50 0 500 1000 0 Time (ms) 40 80 120 160 Aortic Flow Velocity (cm/s) Simultaneous high-fidelity pressure and flow velocity signals (A), ensemble signal average method (B and C), and wave speed estimation by slope of the pressure-velocity relationship during early systole (D) are shown. See Online Appendix for details. performed WIA taking reservoir pressure effect SBP is the cuff systolic BP, MG is the Doppler-derived into account (Online Figures 1 and 2) (19). All invasive mean transvalvular pressure gradient, and SVI noninv data were analyzed using custom-built algorithms is the noninvasive SV index (SVI) measured by (Matlab; Mathworks, Natick, Massachusetts), and re- cross-sectional echocardiography and pulsed-wave sults for 3 to 5 hemodynamic runs were averaged for Doppler (2). each patient. STATISTICAL ANALYSIS. Differences between pre- Noninvasive valvulo-arterial impedance (ZVA) was and post-TAVR hemodynamic data were analyzed by calculated as: ½ZVA ¼ ðSBP þ MGÞ=SVInoninv , where paired t tests. Responses between groups were Downloaded From: http://content.onlinejacc.org/ on 02/06/2015 427 428 Yotti et al. JACC VOL. 65, NO. 5, 2015 Systemic Vascular Load in Aortic Stenosis FEBRUARY 10, 2015:423–33 compared using unpaired t tests. Correlation between quantitative variables was analyzed using the linear T A B L E 2 Invasive Indices of Systemic Hemodynamics and Valvular Function Pearson correlation coefficient (r), and 95% confidence interval (CI) for the fitting was plotted. The intraclass correlation coefficient (r ic, absolute agreement) was used to compare different methods. Out- Index Pre-TAVR Post-TAVR p Value Global hemodynamics Heart rate, beats/min 81 15 87 19 Stroke volume index, ml$m2 41 8 33 10 <0.001 0.17 come analysis was performed by binary logistic Cardiac index, l$min$m2 3.3 0.8 2.8 1.1 <0.001 regression models, accounting for improvement in Systolic blood pressure, mm Hg 130 24 162 23 New York Heart Association (NYHA) functional class Diastolic blood pressure, mm Hg 59 11 67 11 0.08 at follow-up. SVI pre- and post-TAVR and its changes Mean blood pressure, mm Hg 82 14 98 12 0.01 were entered separately in these models, adjusting Pulse pressure, mm Hg 62 24 73 21 0.017 for Peak systolic LV pressure, mm Hg 186 36 162 23 0.003 age and pre-implantation functional class. Because of the risk of overfitting in small samples, overall performance of the model was calculated using 1,000 bootstrap resamples to estimate the C index (20,21). Values of p < 0.05 were considered significant. 23 7 26 7 0.004 49 19 10 3 <0.0001 Valvular function Mean transvalvular pressure gradient, mm Hg 2 Aortic valve area, cm 0.7 0.2 1.4 0.4 <0.0001 Values are mean SD. RESULTS INDICES End-diastolic LV pressure, mm Hg 0.003 LV ¼ left ventricular; TAVR ¼ transcatheter aortic valve replacement. OF AORTIC STENOSIS AND SYSTEMIC HEMODYNAMICS. The large reduction in the trans- valvular pressure gradient caused by TAVR was followed by significant increases in systolic, mean, and pulse systemic arterial pressure values (Table 2). Consequently, LV peak systolic pressure decreased by only a mean of 10% (186 36 mm Hg vs. 162 23 mm Hg, respectively; p ¼ 0.003) and remained >140 mm Hg in 70% of patients, varying widely among patients (Figure 2). After TAVR, SVI (41 8 ml/m 2 vs. 33 10 ml/m 2, respectively; p < 0.001) and cardiac index (3.3 0.8 l/min/m 2 vs. 2.8 1.1 l/min/m 2, respectively; p <0.001) decreased (Figure 2). Patients with and without residual aortic regurgitation showed no significant differences in post-procedural LV end-diastolic pressure (31 9 mm Hg vs. 26 10 mm Hg, respectively; p ¼ 0.22). SYSTEMIC VASCULAR LOAD. A significant increase in systemic vascular resistance, E a, and the first 3 harmonic frequencies of Z were observed after TAVR (Table 3, Central Illustration). The augmentation index and wave speed velocity increased as well, whereas C decreased (Table 3). The amount of decrease in C after TAVR was inversely related to baseline systolic BP (r ¼ 0.72; p < 0.0001). SVI post-TAVR was strongly related to indices of continuous and pulsatile arterial load (Figure 3). Changes in SVI and arterial load indices (C, E a, systemic vascular resistance, and Zc) were not significantly different among patients who did and did not require RV pacing after the procedure (p $ 0.1 for all). TAVR was followed by a significant increase in for- significantly. Pulse pressure and Zc increased, as measured by both the conventional and reservoir approach methods (Online Table 1); the reflection coefficient increased following TAVR, whereas the distance to reflection was only found to decrease by using the reservoir method. Pulse pressure correlated directly with compression waves (r ¼ 0.53 and r ¼ 0.62 for peak FCWs and BCWs, respectively), directly with the backward expansion wave (r ¼ 0.70), and inversely with the forward expansion wave (r ¼ 0.65; p < 0.0001 for all, pooled data and reservoir approach). The Z va did not change significantly with TAVR (4.1 1.2 mm Hg/ml/m 2 vs. 3.9 1.4 mm Hg/ml/m 2, respectively; p ¼ 0.59). FOLLOW-UP. In the 48 h following TAVR, a hyper- tensive response was observed in 12 patients (52%); 10 patients required intensification of their antihypertensive therapy and 1 initiation of treatment. During 6 months of follow-up, 5 patients had their discharge antihypertensive therapy intensified, whereas no patient had reduced doses of these drugs. NYHA functional class did not improve in 14 patients (61%). Improvement in functional class after TAVR was directly related to post-procedural SVI (oddsratio [OR]: 2.8 [95% CI: 1.1 to 7.3] per 5 ml; bootstrapped C index: 0.67; p ¼ 0.03) and inversely to the fall in SVI observed after TAVR (OR: 0.3 [95% CI: 0.1 to 0.9] per 5 ml; p ¼ 0.05), whereas it was not related to pre-TAVR SVI (p ¼ 0.4). DISCUSSION ward compression waves (FCW) and backward compression waves (BCW) (Table 3, Central Illustration), The present study clarifies important aspects of whereas vascular adaptation to calcific degenerative AS. expansion waves Downloaded From: http://content.onlinejacc.org/ on 02/06/2015 did not change JACC VOL. 65, NO. 5, 2015 Yotti et al. FEBRUARY 10, 2015:423–33 Systemic Vascular Load in Aortic Stenosis F I G U R E 2 Hemodynamic Changes After TAVR 250 250 250 p< 0.0001 p= 0.003 200 100 150 100 60 Stroke Volume Index (ml·m-2) 150 Peak LV Pressure (mm Hg) 200 Systolic Blood Pressure (mm Hg) Mean Pressure Gradient (mm Hg) 200 150 100 40 20 50 50 50 p= 0.003 0 0 Pre 0 Pre Post TAVR Post TAVR p< 0.001 0 Pre Post TAVR Pre Post TAVR Boxplots and individual value plots (patients showing a decrease [salmon] or increase [blue] in SVI after TAVR) show values of mean pressure gradient, systolic blood pressure, peak left ventricular pressure, and SVI. SVI ¼ stroke volume index; TAVR ¼ transcatheter aortic valve replacement. Using WIA, we demonstrated that valvular ob- described abnormally high steady and pulsatile struction blunts the conversion of LV ejection blood components of systemic arterial load in patients with momentum system. degenerative calcific AS. However, few studies have Dampened FCWs are reflected as abnormally low analyzed the status of intrinsic vascular properties in BCWs at the aortic bifurcation sites, and both AS invasively. Laskey et al. (8) compared 18 patients effects result in low systolic and pulse arterial with symptomatic degenerative calcific AS to 11 pressures. after younger control subjects and found higher vascular TAVR, demonstrating that the characterization of resistance and impedance and reduced arterial systemic vascular properties in AS is conditioned by compliance in patients with AS. Differences between the upstream obstruction. The relief of the outflow groups became particularly evident during exercise into This FCWs in situation the arterial changes acutely obstruction immediately raises FCWs and BCWs, (8). However, our study’s results suggest that these increasing arterial pressures and vascular imped- observations should be interpreted cautiously. By ance and induces a stiffer vascular behavior. In our analyzing the acute response to TAVR, we showed study, the augmented vascular load correlated with that valve stenosis per se influences all metrics post-procedural was characterizing the arterial tree. Noticeably, classical limited to a small sample size, we found an inverse values of vascular function obtained in our study pre- relationship mid-term TAVR did not differ from previously reported values clinical benefit and the change in SVI observed in age-matched hypertensive populations (22). How- post-TAVR. ever, WIA showed that compression and expansion VASCULAR TREE IN DEGENERATIVE CALCIFIC AS. waves in AS are much lower than previously reported Noninvasive (4) and mathematical (5) methods have normal values (23). We found that immediately after SVI. between Although the this study procedure’s Downloaded From: http://content.onlinejacc.org/ on 02/06/2015 429 430 Yotti et al. JACC VOL. 65, NO. 5, 2015 Systemic Vascular Load in Aortic Stenosis FEBRUARY 10, 2015:423–33 T A B L E 3 Steady and Pulsatile Arterial Hemodynamics at Baseline and After TAVR Factor vasodilator pharmacological interventions (6). Our study demonstrates the negative impact this Pre-TAVR Post-TAVR p Value vascular response exerts on global hemodynamics of Systemic vascular resistance index, dyn∙s∙cm5∙m2 1841 562 2689 1271 <0.0001 patients undergoing TAVR. Although we did not Arterial compliance, pressure decay method, ml∙mm Hg1 1.20 0.79 0.72 0.33 0.002 Arterial compliance, area method, ml∙mm Hg1 1.18 0.77 0.74 0.36 <0.001 Z at fist harmonic frequency, dyn∙s∙cm5 519 219 763 280 <0.001 Z at second harmonic frequency, dyn∙s∙cm5 375 208 541 262 0.002 313 244 395 208 0.36 Frequency domain analysis Z at third harmonic frequency, dyn∙s∙cm 5 5 repeat invasive studies during follow-up, the relatively large proportion of patients requiring antihypertensive therapy scaling during follow-up suggests that our acute observations are not acute phase transients. Similar observations of persistent hypertension have been reported after TAVR (12) and surgical valve replacement (25). 258 139 326 193 0.06 Frequency of first Z minimum, Hz 3.9 1.5 4.6 1.1 0.6 Arterial elastance, mm Hg∙ml1 1.2 0.46 1.75 0.70 <0.001 and arterioles are probably responsible for the 1.09 0.40 1.63 0.65 <0.001 observed changes in pulsatile vascular load after Augmentation index 392 232 750 739 0.025 Distance to reflection, m 0.11 0.72 0.12 0.09 0.06 Wave speed, m∙s1 3.57 2.05 4.62 2.01 0.034 responsible for this observation. Due to the nonline- Characteristic impedance, dyn∙s∙cm5 192 124 247 141 0.05 arity of viscoelastic strain of the large conductance Iw total forward wave, W∙m2∙s1∙104 9.09 4.84 10.83 4.84 0.03 Iw FCW, W∙m2∙s1∙104 deformation post-TAVR may also induce stiffer 5.64 2.97 7.37 3.00 0.001 Peak dIw FCW, W∙m2∙s2∙106 1.01 0.54 1.80 0.66 <0.001 behavior of the vascular tree (26). Characteristic impedance, dyn∙s∙cm Arterial elastance, resistance method, mm Hg∙ml1 Wave intensity analysis Changes in the tone of large conduction arteries TAVR. We know vasoconstriction in arteriolar vessels reduces arterial compliance (14). The viscoelastic properties of large conductance arteries also may be arteries, acute changes in the pressure-mediated Forward wave 2 1 4 Iw FEW, W∙m ∙s ∙10 2.89 1.80 2.75 1.51 0.45 Peak dIw FEW, W∙m2∙s2∙106 0.51 0.31 0.46 0.30 0.68 VASCULAR TREE AND OUTCOME IN AS. Indirect ev- idence has emphasized the complementary impact of Backward wave Iw total backward wave, W∙m2∙s1∙104 3.71 2.68 5.23 2.28 0.04 arterial hemodynamics on the symptomatic status Iw BCW, W∙m2∙s1∙104 2.34 1.72 3.39 2.17 0.04 and outcome of patients with AS, both before (2,4) Peak dIw BCW, W∙m2∙s2∙106 0.33 0.18 0.55 0.32 0.001 Iw BEW, W∙m2∙s1∙104 and after (27) valve intervention. The “double 0.87 0.76 1.15 1.00 0.19 Peak dIw BEW, W∙m2∙s2∙106 0.21 0.18 0.23 0.21 loaded” hypothesis integrates these additive effects 0.75 Reflection Reflection coefficient Distance to reflection, m 0.40 0.27 0.33 0.19 0.28 0.17 0.13 0.17 0.12 0.81 of valvular and vascular loads. On this basis, the Z VA index has been found to correlate with SV and outcome (3,28). However, in our study, Z VA did not capture the hemodynamic changes observed with Values are mean SD. TAVR. The fact that Z VA did not improve acutely BCW ¼ backward compression wave; BEW ¼ backward expansion wave; dIw ¼ intensity; FCW ¼ forward compression wave; FEW ¼ forward expansion wave; Iw ¼ cumulative wave intensity; Z ¼ impedance; other abbreviations are as in Table 2. probably relates to its sensitivity to both the valvular and the vascular compartments, which are competitively modified by therapy. A well-known risk factor of cardiovascular TAVR, the transmission of blood momentum to the morbidity and mortality, especially in elderly patients arterial system improves, increasing FCWs. Stronger (29), hypertension has been associated with worse FCWs are reflected as stronger BCWs traveling toward outcomes in patients who undergo TAVR (30). How- the LV. Both effects raise mean, systolic, and pulse ever, a hypertensive response after TAVR has also arterial pressure levels. been associated with a better prognosis (12). In a Our results show that after TAVR, the vascular previous study, higher BP after TAVR was related to tree exhibits a stiffer behavior. This paradoxical ef- higher SV and was attributed to an acute improve- fect of rising continuous and pulsatile vascular load ment of LV function; patients with stable BP after after LV outflow relief was described previously (9). TAVR experienced, on average, a reduction in post- In patients undergoing percutaneous aortic valvu- procedural SV (12). Similarly, our study suggests loplasty, valvular-vascular interaction follows the that a post-procedural reduction in SV is related to properties of complementarity (both compartments absence of clinical improvement. However, we have contribute additively to afterload) and competitive- shown that the acute hypertensive response after ness (one compartment cannot be lowered without TAVR is caused by increased vascular load rather than raising the other one) (9,24). More recently, this improved LV systolic function, so it should be interaction was confirmed in AS patients undergoing promptly identified and treated. Downloaded From: http://content.onlinejacc.org/ on 02/06/2015 JACC VOL. 65, NO. 5, 2015 Yotti et al. FEBRUARY 10, 2015:423–33 Systemic Vascular Load in Aortic Stenosis 50 50 40 40 30 30 20 20 10 r= -0.80 p< 0.0001 r= -0.63 p= 0.001 1000 500 1500 2000 1.0 1.5 2.0 2.5 3.0 Arterial Elastance (mm Hg·ml-1) 0.4 0.8 1.2 1.6 Arterial Compliance (ml·mm Hg-1) 50 50 40 40 30 30 20 20 10 r= -0.70 p= 0.0002 500 r= -0.55 p= 0.007 750 1000 1250 250 Z @ 1 Hz (dyn·s·cm-5) 10 r= -0.57 p= 0.005 500 750 1000 Z @ 2 Hz (dyn·s·cm-5) 1250 250 500 Stroke Volume Index (ml·m-2) Stroke Volume Index (ml·m-2) SVRI (dyn·s·m2·cm-5) 10 r= 0.61 p= 0.002 Stroke Volume Index (ml·m-2) Stroke Volume Index (ml·m-2) F I G U R E 3 Correlation Between SVI and Indices of Arterial Load 750 Z @ 3 Hz (dyn·s·cm-5) Scatterplots, linear fittings (dotted line), and 95% confidence intervals are shown for the fitting (gray ribbon) of indices of continuous and pulsatile arterial load versus SVI. Colors are as in Figure 2. SVRI ¼ systemic vascular resistance index; TAVR ¼ transcatheter aortic valve replacement; Z ¼ impedance. LV IMPACT. Because no striking changes in chamber STUDY LIMITATIONS. The flow acquisition system systolic volume are expected during TAVR, the measures aortic flow velocity by using a very small observation of post-procedural increased arterial load Doppler sample volume. Therefore, signals may suggests that the hemodynamic benefits of valvular sometimes be noisy in highly turbulent flows, as in replacement on LV systolic wall stress may be lower AS, and not account for the average flow velocity for than expected, particularly in patients with relatively the full cross-section of the aorta where measure- low transvalvular pressure gradients. Although peak ments are obtained. The geometry of the Corevalve LV pressure decreases after TAVR, it frequently prosthesis can modify the local mechanical properties remained post- of the arterial wall in the aortic root. For this reason, procedural vascular load may explain why patients we acquired the invasive pressure and flow rate/ with paradoxically low-flow low-gradient AS fail to velocity signals 5 cm distal to the aortic annulus, improve values of N-terminal prohormone B-type searching for the highest velocities at this point, natriuretic peptide by 1 year after TAVR (31) and have attempting to minimize the prosthesis’ local effects. a higher mortality than patients with normal flow To avoid these issues, we selected data with the (32). Further large-scale studies are necessary to highest quality available and implemented filtering address the predictors of LV systolic stress improve- and ensemble averaging to increase the signal-to- ment. Nevertheless, in view of our data and those of noise ratio. However, we cannot exclude the fact others (6), intense medical therapy is recommended that residual high-frequency noise may account for in hypertensive patients with calcific degenerative the relatively high Zc values that were measured. AS, regardless of whether they finally do or do not Although a stable conscious sedation level was undergo valve replacement. achieved in all cases, a certain vascular tone higher than normal. Increased Downloaded From: http://content.onlinejacc.org/ on 02/06/2015 431 432 Yotti et al. JACC VOL. 65, NO. 5, 2015 Systemic Vascular Load in Aortic Stenosis FEBRUARY 10, 2015:423–33 modification can be expected for sedating drugs. impacts the post-procedural acute hemodynamic Similarly, some degree of vascular changes could be benefits of TAVR. caused by adaptation to acute procedure-related myocardial injury. We studied an elderly and high-risk AS group; therefore, the vascular hemodynamics and response to TAVR could be different in younger patients. Functional improvement was only assessed using ACKNOWLEDGMENTS The author thank all members of the staff of the Echocardiography and Catheterization Laboratories of the Hospital General Universitario Gregorio Marañón for their support for patient recruitment and data collection. NYHA functional classification; other tools such as the 6-min walk test or quality-of-life questionnaires REPRINT REQUESTS AND CORRESPONDENCE: Dr. would have increased the sensitivity to detect func- Raquel Yotti, Department of Cardiology, Hospital tional improvement. The small sample size was General Universitario Gregorio Marañón, Dr. Esquerdo designed to analyze the mechanistic changes in 46, 28007 Madrid, Spain. E-mail: raquel.yotti@salud. vascular load. Thus, subgroup analyses need to be madrid.org. interpreted cautiously, and hard clinical endpoints could not be analyzed. With the small sample size, we also could not address the impact of potential con- PERSPECTIVES founders such as degree of mitral regurgitation. Large-scale clinical studies are necessary to rule out a COMPETENCY IN MEDICAL KNOWLEDGE: Relief potential acute rebound effect post-intervention and of AS raises forward and backward compression confirm that post-TAVR measurements accurately waves, increasing arterial pressure and both the account for the true arterial load once the stenotic steady and pulsatile components of systemic arterial damping effect has been alleviated. load. COMPETENCY IN PROCEDURAL SKILLS: CONCLUSIONS The increased post-procedural systemic vascular load Because valvular and vascular loads are tightly coupled in AS, upstream obstruction can influence the measurements of arterial properties. Low arterial FCWs and BCWs caused by valvular stenosis produce the hallmark signs of arterial hemodynamics in AS. Relief of valvular obstruction with TAVR acutely increases compression waves, causing the arterial tree to operate at a higher pressure and therefore should be promptly treated when patients with AS undergo TAVR, particularly when the transvalvular pressure gradient is low. TRANSLATIONAL OUTLOOK: Larger prospective studies are needed to define the prognostic implications of changes in systemic vascular load that immediately follow TAVR. increasing the vascular load. This phenomenon REFERENCES 1. Bermejo J, Odreman R, Feijoo J, Moreno MM, Gomez-Moreno P, Garcia-Fernandez MA. Clinical efficacy of Doppler-echocardiographic indices of aortic valve stenosis: a comparative test-based analysis of outcome. J Am Coll Cardiol 2003;41: 142–51. 2. Hachicha Z, Dumesnil JG, Bogaty P, Pibarot P. Paradoxical low-flow, low-gradient severe aortic stenosis despite preserved ejection fraction is associated with higher afterload and reduced survival. Circulation 2007;115:2856–64. 3. Hachicha Z, Dumesnil JG, Pibarot P. Usefulness of the valvuloarterial impedance to predict adverse outcome in asymptomatic aortic stenosis. J Am Coll Cardiol 2009;54:1003–11. 4. Briand M, Dumesnil JG, Kadem L, et al. Reduced systemic arterial compliance impacts significantly on left ventricular afterload and function in aortic stenosis: implications for diagnosis and treatment. J Am Coll Cardiol 2005;46:291–8. Downloaded From: http://content.onlinejacc.org/ on 02/06/2015 5. Garcia D, Barenbrug PJ, Pibarot P, et al. A ventricular-vascular coupling model in presence of aortic stenosis. Am J Physiol Heart Circ Physiol 2005;288:H1874–84. after balloon aortic valvuloplasty. Circ Res 1992; 71:1174–84. 10. Laskey WK, Parker HG, Ferrari VA, Kussmaul WG, Noordergraaf A. Estimation of total 6. Eleid MF, Nishimura RA, Sorajja P, Borlaug BA. Systemic hypertension in low-gradient severe aortic stenosis with preserved ejection fraction. Circulation 2013;128:1349–53. systemic arterial compliance in humans. J Appl Physiol 1990;69:112–9. 7. Jimenez-Candil J, Bermejo J, Yotti R, et al. Effects of angiotensin converting enzyme inhibitors in hypertensive patients with aortic valve stenosis: a drug withdrawal study. Heart 2005;91: 1311–8. aortic stenosis in high-risk patients using the second- and current third-generation selfexpanding CoreValve prosthesis: device success and 30-day clinical outcome. J Am Coll Cardiol 2007;50:69–76. 8. Laskey WK, Kussmaul WG III, Noordergraaf A. Systemic arterial response to exercise in patients with aortic valve stenosis. Circulation 2009;119: 996–1004. 12. Perlman GY, Loncar S, Pollak A, et al. Postprocedural hypertension following transcatheter aortic valve implantation: incidence and clinical significance. J Am Coll Cardiol Intv 2013;6:472–8. 9. Shim Y, Hampton TG, Straley CA, et al. Ejection load changes in aortic stenosis. Observations made 13. Davies JE, Sen S, Broyd C, et al. Arterial pulse wave dynamics after percutaneous aortic valve 11. Grube E, Schuler G, Buellesfeld L, et al. Percutaneous aortic valve replacement for severe JACC VOL. 65, NO. 5, 2015 Yotti et al. FEBRUARY 10, 2015:423–33 Systemic Vascular Load in Aortic Stenosis replacement: fall in coronary diastolic suction with increasing heart rate as a basis for angina symptoms in aortic stenosis. Circulation 2011;124: 1565–72. 14. Nichols WW, O’Rourke M, Vlachopoulos C. McDonald’s Blood Flow in Arteries. Theoretical, experimental and clinical principles. 6th ed. Boca Raton, FL: CRC Press, 2011. 15. Chemla D, Hebert JL, Coirault C, et al. Total arterial compliance estimated by stroke volumeto-aortic pulse pressure ratio in humans. Am J Physiol 1998;274 2 Pt 2:H500–5. 16. Segers P, Stergiopulos N, Westerhof N. Relation of effective arterial elastance to arterial system properties. Am J Physiol Heart Circ Physiol 2002;282:H1041–6. 17. Sunagawa K, Maughan WL, Sagawa K. Optimal arterial resistance for the maximal stroke work studied in isolated canine left ventricle. Circ Res 1985;56:586–95. 18. Parker KH. An introduction to wave intensity analysis. Med Biol Eng Comput 2009;47:175–88. 19. Tyberg JV, Davies JE, Wang Z, et al. Wave intensity analysis and the development of the reservoir-wave approach. Med Biol Eng Comput 2009;47:221–32. 20. R Core Team. R: A language and eviroment for statistical computing. Vienna, Austria: R Founda- regression, and survival analysis. New York, NY: Springer, 2010. 22. Mitchell GF, Lacourciere Y, Ouellet JP, et al. Determinants of elevated pulse pressure in middle-aged and older subjects with uncomplicated systolic hypertension: the role of proximal aortic diameter and the aortic pressure-flow relationship. Circulation 2003;108:1592–8. patients undergoing transcatheter aortic valve implantation. J Am Soc Echocardiogr 2013;26: 691–8. 29. Aronow WS, Fleg JL, Pepine CJ, et al. ACCF/AHA 2011 expert consensus document on hypertension in the elderly. J Am Coll Cardiol 2011;57:2037–114. 23. Schultz MG, Davies JE, Roberts-Thomson P, Black JA, Hughes AD, Sharman JE. Exercise central (aortic) blood pressure is predominantly driven by forward traveling waves, not wave reflection. Hypertension 2013;62:175–82. 30. Thomas M, Schymik G, Walther T, et al. Oneyear outcomes of cohort 1 in the Edwards SAPIEN Aortic Bioprosthesis European Outcome (SOURCE) registry: the European registry of transcatheter aortic valve implantation using the Edwards SAPIEN valve. Circulation 2011;124:425–33. 24. Pasipoularides A. Complementarity and competitiveness of the intrinsic and extrinsic components of the total ventricular load: 31. Ribeiro HB, Urena M, Le Ven F, et al. Longterm prognostic value and serial changes of plasma N-terminal prohormone B-type natriuretic demonstration after valve replacement in aortic stenosis. Am Heart J 2007;153:4–6. Peptide in patients undergoing transcatheter aortic valve implantation. Am J Cardiol 2014;113: 851–9. 25. Dahl JS, Videbaek L, Poulsen MK, et al. Effect of candesartan treatment on left ventricular remodeling after aortic valve replacement for aortic stenosis. Am J Cardiol 2010;106:713–9. 26. Milnor WR, Bertram CD. The relation between arterial viscoelasticity and wave propagation in the canine femoral artery in vivo. Circ Res 1978;43: 870–9. 32. Le Ven F, Freeman M, Webb J, et al. Impact of low flow on the outcome of high-risk patients undergoing transcatheter aortic valve replacement. J Am Coll Cardiol 2013;62:782–8. KEY WORDS aortic valve stenosis, hemodynamics, vascular function 27. Lauten A, Zahn R, Horack M, et al. Trans- tion for Statistical Computing; 2013. catheter aortic valve implantation in patients with low-flow, low-gradient aortic stenosis. J Am Coll Cardiol Intv 2012;5:552–9. 21. Harrell FE. Regression modeling strategies with applications to linear models, logistic 28. Katsanos S, Yiu KH, Clavel MA, et al. Impact of valvuloarterial impedance on 2-year outcome of Downloaded From: http://content.onlinejacc.org/ on 02/06/2015 A PP END IX For expanded Methods and Results sections, including a supplemental table and figures, please see the online version of this article. 433
© Copyright 2026