Enterra 4351 Implant Manual
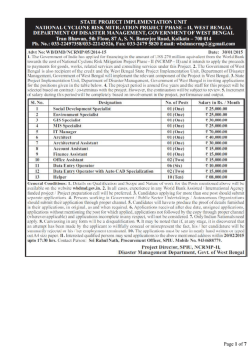
4351_Enterra_fcv.fm 2/16/12 3:10 pm Medtronic Confidential package_R00a 4 x 8 inches (101 mm x 203 mm) Enterra® Therapy 4351 Unipolar Intramuscular Lead for the Gastric Electrical Stimulation System Humanitarian device: Authorized by Federal law for use in the treatment of chronic intractable (drug-refractory) nausea and vomiting secondary to gastroparesis of diabetic or idiopathic etiology. The effectiveness of this device for this use has not been demonstrated. Technical manual Rx only MA01352A004 Rev X 4351_Enterra_fcv.fm 2/16/12 3:10 pm Medtronic Confidential package_R00a 4 x 8 inches (101 mm x 203 mm) Medtronic® and Enterra® are trademarks of Medtronic, Inc., registered in the U.S. and other countries. MA01352A004 Rev X 4351_EnterraTOC.fm 2/16/12 3:10 pm 4 x 8 inches (101 mm x 203 mm) Medtronic Confidential package_R01 Table of contents Device description 5 Package contents 5 Indications 6 Contraindications 6 Physician training 6 Patient counseling 6 Warnings 7 Theft detectors and security screening devices 8 Precautions 10 Inspecting the package 10 Handling the lead 10 General precautions 10 Lead repositioning 10 Patient considerations 10 Adverse events summary 11 Clinical studies 11 WAVESS study 11 WAVESS Compassionate Use study (WCU) 13 Compassionate Use Electrical Stimulation Study (CUESS) WAVESS results 16 Adverse events 18 Resterilization 21 Directions for use 22 Implant the lead 22 Anchor the lead 23 Create pocket for neurostimulator 24 Connecting leads to neurostimulator 25 Using lead end cap 27 Verify impedance and close pocket 28 Program Enterra Therapy System 29 Program basic neurostimulator parameters 29 Program output current 30 Postoperative programming schedule 31 Detailed device description 32 Specifications 32 Special notice 33 Warranty 34 Enterra 4351 Implant Manual MA01352A004 Rev X 14 2012-06 3 4351_EnterraTOC.fm 2/16/12 3:10 pm 4 x 8 inches (101 mm x 203 mm) 4 2012-06 MA01352A004 Enterra 4351 Implant Manual Rev X Medtronic Confidential package_R01 Medtronic Confidential Pkg_R00a 4351_Enterra_CH.fm 2/16/12 3:10 pm 4 x 8 inches (101 mm x 203 mm) Device description The Enterra Therapy System for gastric electrical stimulation is comprised of a neurostimulator, leads, programmer, and programmer software. The Medtronic Model 4351 Lead (see Figure 1) is a unipolar, intramuscular lead with a fixed 10-mm electrode. The lead comes with a 3.2 mm low profile Medtronic standard lead connector in a unipolar configuration. Only the pin connector is mechanically and electrically connected in the unipolar configuration. Insertion “ski” needle Trumpet Anchor Electrode Blue Polypropylene Monofilament (10 cm) Setscrew grommets Connector pin 3.2 mm Low-Profile Connector Connector block Enterra Therapy Neurostimulator Suture holes Figure 1. Lead Model 4351 with neurostimulator. The lead has a polyurethane insulation and a flexible electrode coil made of platinum and iridium. The platinum-iridium electrode tip is mechanically and electrically connected to the electrode coil. The lead has an attached, non-absorbable blue polypropylene monofilament and a ski needle for lead insertion. The Model 4351 Lead is intended to be used with the following Medtronic products: • Model 7425G Neurostimulator • Model 3116 Neurostimulator • Model 7432 Physician Programmer • MemoryMod Model 7457 or 7459 Programmer Software • Model 8840 N’Vision Clinician Programmer • Model 8870 Software Application Card The lead is designed for intramuscular implantation to deliver electrical current to the stomach muscle. Package contents The Medtronic Model 4351 Lead package contains the following: • One Model 4351 Lead (with pre-attached anchor and suture with insertion needle) • Four fixation disks • Tunneling rod • Two lead end caps • Product literature Note: The contents of the inner package are sterile (ethylene-oxide sterilized). Enterra 4351 Implant Manual MA01352A004 Rev X 2012-06 5 4351_Enterra_CH.fm 2/16/12 3:10 pm 4 x 8 inches (101 mm x 203 mm) Medtronic Confidential Pkg_R00a Indications The Enterra gastric lead is indicated for the treatment of patients with chronic, intractable (drug-refractory) nausea and vomiting secondary to gastroparesis of diabetic or idiopathic etiology. Contraindications The Enterra Therapy System is contraindicated in patients whom the physician determines are not candidates for surgical procedures and/or anesthesia due to physical or mental health conditions. Do not use shortwave diathermy, microwave diathermy or therapeutic ultrasound diathermy (all now referred to as diathermy) on patients implanted with a neurostimulation system. Energy from diathermy can be transferred through the implanted system and can cause tissue damage at the location of the implanted electrodes, resulting in severe injury or death. Diathermy is further prohibited because it can also damage the neurostimulation system components resulting in loss of therapy, requiring additional surgery for system explantation and replacement. Injury or damage can occur during diathermy treatment whether the neurostimulation system is turned “ON” or “OFF.” Advise your patients to inform all their health care providers that they should not be exposed to diathermy treatment. Physician training Prescribing physicians are encouraged to contact Medtronic for available educational opportunities regarding the surgical and/or implantation techniques, operational characteristics and functions of the Enterra Therapy System prior to prescribing the device for the first time. All programming should be by or under the supervision of a physician or other experienced medical personnel familiar with the use of the programming software. Patient counseling The patient and family should be advised of the known risks of the surgical procedure and the therapy (as discussed in the other sections of this manual), as well as the potential benefits. The patient should be advised to read The Enterra Therapy Gastric Electrical Stimulation System Patient Manual, which is included in the Model 7425G and 3116 Neurostimulator packages. 6 2012-06 MA01352A004 Enterra 4351 Implant Manual Rev X 4351_Enterra_CH.fm 2/16/12 3:10 pm 4 x 8 inches (101 mm x 203 mm) Medtronic Confidential Pkg_R00a Warnings Age limitations – The safety and effectiveness of this therapy has not been established for patients under age 18 or over age 70. Allergic reaction – There is a possibility of an allergic or immune system response to the implanted materials. Anticoagulation therapy – Patients on anticoagulation therapies may be at a greater risk for postoperative complications, such as hematomas. Interaction with other implantable devices – When another implantable device (eg, pacemakers, defibrillators, or cochlear implants) is required, the physicians involved in both therapies should discuss the possible interaction between the devices. Electrical impulses from the neurostimulation system may affect the sensing operation and cause inappropriate device response of other implanted devices. Careful programming of each system may optimize the benefit from each device. Follow these suggested guidelines: • The neurostimulator should be placed on the opposite side of the body from the other implanted device. • The neurostimulator should be reprogrammed to bipolar stimulation. • Each system should be checked to ensure that it is working as intended. Component compatibility – Use only Medtronic components that are compatible with this system. The use of non-Medtronic components with this stimulation system can result in damage to Medtronic components, loss of therapy, or patient injury. Electrocautery – Electrocautery can damage the lead or neurostimulator. It can also cause temporary suppression of neurostimulator output and it can reprogram the neurostimulator to Power ON Reset parameters (output OFF, amplitude = 0V). This requires the clinician to reprogram the neurostimulator. Electrocautery may also cause induced currents in the lead portion of the neurostimulation system that could be hazardous or cause further injury. Follow these precautions when using electrocautery: • Turn OFF the neurostimulator before performing electrocautery. • Do not contact the lead with the electrocautery device. • Only bipolar cautery is recommended. • If unipolar cautery is necessary: • Do not use high voltage modes. • Keep the power setting as low as possible. • Keep the current path (ground plate) as far away from the neurostimulator and lead as possible. • Confirm the neurostimulator function after electrocauterization. Radiation therapy – Do not direct high radiation sources, such as cobalt 60 or gamma radiation, at the neurostimulation system. If radiation therapy is required in the vicinity of the neurostimulation system, place lead shielding over the device to prevent radiation damage. High-Output Ultrasonics / Lithotripsy – Use of high-output ultrasonic devices, such as electrohydraulic lithotriptor, is not recommended for patients with an implanted neurostimulation system. If lithotripsy must be used, do not focus the beam within 6 inches (15 cm) of the neurostimulator. Defibrillation / Cardioversion – When a patient is in ventricular or atrial fibrillation, the first consideration should be patient survival. External defibrillation or cardioversion can cause permanent damage to a neurostimulation system. It is recommended not to use defibrillation or cardioversion paddles near the neurostimulator. When external defibrillation or cardioversion is necessary, minimize the current flowing through the neurostimulator and lead system as follows: • Position paddles as far from the neurostimulator as possible. • Position paddles perpendicular to the neurostimulation system. • Use the lowest clinically appropriate energy output (watt seconds). Enterra 4351 Implant Manual MA01352A004 Rev X 2012-06 7 4351_Enterra_CH.fm 2/16/12 3:10 pm 4 x 8 inches (101 mm x 203 mm) Medtronic Confidential Pkg_R00a Defibrillation or cardioversion may also cause induced currents in the lead portion of the neurostimulation system that could be hazardous or cause further injury. Confirm the neurostimulation system function after external defibrillation. Magnetic Resonance Imaging (MRI) – Patients with an implanted device should not be exposed to the electromagnetic fields produced by magnetic resonance imaging (MRI). Use of MRI may potentially result in system failure, dislodgement, heating, or induced voltages in the neurostimulator and/or lead. An induced voltage through the neurostimulator or lead may cause uncomfortable, “jolting,” or “shocking” levels of stimulation. Clinicians should carefully weigh the decision to use MRI in patients with an implanted neurostimulation system, and note the following: • Magnetic and radio-frequency (RF) fields produced by MRI may change the neurostimulator settings and injure the patient. • Patients treated with MRI should be closely monitored and programmed parameters verified upon cessation of MRI. Pregnancy – Safety for use during pregnancy or delivery has not been established. Infection – It is recommended that the neurostimulator implant site be irrigated with antibiotic solution during surgery and that IV antibiotics be administered perioperatively. When possible, identify and treat any infections remote to the implant site prior to surgery. Infections at the implant site almost always require the surgical removal of the implanted system. Bowel obstruction/perforation – The lead can become entangled with or erode into the bowel, which can result in bowel obstruction and perforation. Either may lead to life-threatening intra-abdominal infections and may require laparotomy, bowel resection, and system revision. Avoid excess lead slack in the abdominal cavity. Post implant, consider lead entanglement or erosion as a possible etiology in patients with bowel obstruction symptoms. Theft detectors and security screening devices Patients should be advised to use care when approaching theft detector and security screening devices (such as those found in airports, libraries, and some department stores). When approaching these devices, patients should do the following: 1. If possible, request to bypass these devices. The patient should show the security personnel their patient identification card for the neurostimulator and request a manual search. Security personnel may use a handheld security wand but the patient should ask the security personnel not to hold the security wand near the neurostimulator any longer than is absolutely necessary. The patient may wish to ask for another form of personal search. 2. If patients must pass through the theft detector or security screening device, they should approach the center of the device and walk through normally (Figure 2). a. If two security gates are present, they should walk through the middle, keeping as far away as possible from each gate. b. If one gate is present, they should walk as far away as possible from it. Note: Some theft detectors may not be visible. 3. Proceed through the security device. Do not linger near or lean on the screening device. 8 2012-06 MA01352A004 Enterra 4351 Implant Manual Rev X 4351_Enterra_CH.fm 2/16/12 3:10 pm 4 x 8 inches (101 mm x 203 mm) Double Security Gate Medtronic Confidential Pkg_R00a Single Security Gate (Stay as far away as possible from gate) Figure 2. Approaching security gates. Enterra 4351 Implant Manual MA01352A004 Rev X 2012-06 9 4351_Enterra_CH.fm 2/16/12 3:10 pm 4 x 8 inches (101 mm x 203 mm) Medtronic Confidential Pkg_R00a Precautions Inspecting the package Inspect the lead’s sterile package prior to opening. If the seal or package is damaged, contact your local Medtronic representative. Handling the lead • Do not implant a neurostimulator if it has been dropped onto a hard surface from a height of 12 in (30 cm) or more. • Do not immerse the lead in mineral oil, silicone oil, or any other equivalent. • Lead insulators attract small particles such as lint and dust; therefore, to minimize contamination protect the lead from materials shedding these substances. Handle the lead with sterile surgical gloves that have been rinsed in sterile water or equivalent. • Do not implant a lead that was dropped; the lead may no longer be sterile. • Any severe bending, kinking, stretching, or handling with surgical instruments may cause permanent damage to the electrode coil, conductor coil, connector, or the lead body. If the lead is damaged, do not implant. Return the lead to your Medtronic representative. – Do not tie a suture directly to the lead body, because the suture could cut through the lead insulation. Use the anchor on the lead and the fixation disks, which are supplied with the lead kit. Do not overtighten sutures to avoid damage to the anchor or fixation disk. – Do not use a hemostat on the lead body. – If handling the lead with forceps, use only rubber-tipped bayonet forceps. • Wipe off any body fluids on the lead contacts or connector before connecting the lead to the neurostimulator. Contamination of the connections can affect gastric stimulation. • Take care to avoid accidental bending of the electrode coil and the conductor coil; the angulation required to restore the electrode’s original shape may weaken or fracture the electrode. General precautions • The physician should be aware that gastric stimulation systems may unexpectedly cease to function. A system may fail at any time due to random failures of the system components or the battery (prior to depletion). These events, which can include electrical shorts or opens and insulation breaches, cannot be predicted. Lead repositioning • Repositioning the lead is not recommended after implantation. If necessary, replace the lead. Removing the lead after long-term implant may be difficult due to fibrotic tissue development. If you cannot remove the lead safely, it is recommended that the lead be left in position . Place a lead end cap over the connector pin and secure the end cap with a suture (see “Using lead end cap”). Patient considerations • Select patients carefully to assure that their symptoms are of physiological origin. Patients must be appropriate candidates for surgery. • It is recommended that patients undergo detoxification from narcotics prior to implant. • So that the benefit from the gastric stimulation system may be optimized, long-term, postsurgical management of the patient is strongly encouraged. 10 2012-06 MA01352A004 Enterra 4351 Implant Manual Rev X Medtronic Confidential Pkg_R00a 4351_Enterra_CH.fm 2/16/12 3:10 pm 4 x 8 inches (101 mm x 203 mm) Adverse events summary In addition to those risks associated with surgery, implantation or use of a neurostimulation system includes, but is not limited to, the following risks: • Lead impedance out of range • Undesirable change in stimulation, possibly related to cellular charges around the electrodes, shifts in electrode position, loose electrical connections, or lead fractures • Loss of therapeutic effect • Lead or neurostimulator erosion or migration, which may necessitate surgical revision • Bowel obstruction, perforation, ileus, or necrosis • Infections, including device/implant site infections, intra-abdominal infections, abscess, peritonitis, sepsis, urinary tract infections • Stomach wall perforation • Upper and lower gastro-intestinal (GI) symptoms • Hemorrhage, hematoma, and possible GI complications resulting from the surgical procedure to implant the neurostimulator and leads • Persistent pain at the neurostimulator site • Extra-abdominal pain, bone- and joint-related pain • Seroma at the neurostimulator site • Allergenic or immune system response to implanted materials • Stress incontinence • Fever • Feeding tube complications • Dehydration • Dysphagia • Acute diabetic complications • Cardiovascular renal related events The adverse events observed during the clinical evaluation of the Enterra Therapy System are summarized in Table 9. These events were related to the device or implant surgery. Clinical studies Patients with drug-refractory gastroparesis of diabetic or idiopathic etiologies were evaluated in the following clinical studies: the World Wide Anti-Vomiting Electrical Stimulation Study (WAVESS), the WAVESS Compassionate Use Study (WCU), and the Compassionate Use Electrical Stimulation Study (CUESS). WAVESS study The WAVESS study was a double-blind, randomized cross-over study that enrolled a total of 33 subjects. The study was designed to collect both safety and effectiveness information. WAVESS study objective The primary endpoint of the study was a reduction in vomiting frequency, as measured by patient diaries. The treatment was considered successful if a reduction in vomiting frequency by at least 80% was observed during the cross-over period of the study with the ON-mode stimulation, when compared to the OFF-mode stimulation. The secondary endpoints in the study were quality of life (measured with the Medical Outcomes Study Short-Form 36 Health Survey), body mass index, hypoglycemic attacks (diabetic group only), subjective symptoms documented by a clinical status interview, glycosylated hemoglobin, and gastric emptying documented with a gastric emptying test. Enterra 4351 Implant Manual 2012-06 MA01352A004 Rev X 11 Medtronic Confidential Pkg_R00a 4351_Enterra_CH.fm 2/16/12 3:10 pm 4 x 8 inches (101 mm x 203 mm) WAVESS entry criteria The inclusion criteria for the study included: • Symptomatic gastroparesis ≥ 1 year, as documented by an initial Gastric Emptying Test (GET) • Refractory or intolerant to at least two antiemetic and two prokinetic drug classes • On stable medical therapy, and, if applicable, stable nutritional support during the month prior to enrollment • Frequency of vomiting > 7 vomiting episodes per week, as documented with a baseline patient diary • Delayed gastric emptying, defined by greater than 60% retention at two hours and > 10% retention at four hours, as measured by standardized gastric emptying testing The exclusion criteria included: • Organ transplant • Organic obstruction • Pseudo-obstruction • Prior gastric surgery • Scleroderma • Amyloidosis • History of seizures • Peritoneal or unstable dialysis • Chemical dependency • Pregnancy • Primary eating or swallowing disorders • Psychogenic vomiting • Implanted electronic medical devices • Age < 18 or > 70 years WAVESS study enrollment Enrollment and follow-up in the WAVESS study was as follows: Table 1. Enrollment in WAVESS Study Number of Subjects at enrollment implanted> 30 days (N) 33 33 implanted> implanted> 60 days 6 Months 33 27 implanted> 12 Months 24 WAVESS study demographics A total of 33 subjects were enrolled in the WAVESS study. The demographic information on these subjects is presented in the table below: Table 2. Patient Demographics Diabetic (N=17) Idiopathic (N=16) Total (N =33) Gender (M/F) 9/8 F 0/16 F 9/24 F Age, mean 38.1 41.1 39.6 BMI, mean 24.7 22.9 23.7 79.7/80.0 53.2/51.0 73.1/76.5 34.3/28.0 76.5/78.0 44.0/34.0 Gastric retention (mean/median)% @ 2 hours @ 4 hours 12 2012-06 MA01352A004 Enterra 4351 Implant Manual Rev X 4351_Enterra_CH.fm 2/16/12 3:10 pm 4 x 8 inches (101 mm x 203 mm) Medtronic Confidential Pkg_R00a WAVESS study design Subjects satisfying entry criteria received gastric stimulation systems that included an implanted neurostimulator connected to two unipolar leads that were implanted in the muscle wall of the stomach on the greater curvature at the limit of the corpus-antrum. All subjects received a Model 7425 implantable neurostimulator and a pair of Model 43001 leads. The stimulation parameters used in the study were: Intensity: 5 mA, Pulse Width: 330 µsec, Frequency: 14 Hz. The neurostimulator was set to deliver a pair of pulses at these parameters every five seconds continuously 24 hours per day. The study was conducted in two phases: 1. Phase I was a double blind crossover study with evaluations prior to implant and at 30 days and 60 days post-implant. Subjects were randomly assigned to stimulation ON and OFF for the first month after implant and were crossed to OFF and ON for the second month. Subjects were blinded as to which stimulation sequence they received. 2. Phase II was an unblinded open label study with follow-up at six and twelve months. After the crossover period was complete, the subjects were asked which month of the crossover stimulation they preferred. After the selection was made, the study blind was broken. The subjects then received stimulation (ON or OFF) consistent with their preference. The primary and the secondary endpoints, except gastric emptying, were measured at baseline, 30 days, 60 days, six months, and twelve months postrandomization. Gastric emptying was measured at baseline, and six and twelve months postrandomization. Primary endpoint evaluations included weekly vomiting frequency and patient preference within Phase I of the study. Secondary endpoint evaluations included gastric retention, hypoglycemic attacks, upper GI symptoms, and quality of life using the Medical Outcomes Study Short-Form 36 Health Survey. WAVESS Compassionate Use study (WCU) The WAVESS Compassionate Use study (WCU) was an open label, nonrandomized study that included a total of 18 subjects. The WCU study was designed to provide safety (adverse events) information on gastric stimulation. WCU study objective The purpose of the WCU study was to provide treatment for patients and to evaluate adverse events of patients with drug-refractory gastroparesis who did not meet the entry criteria of the WAVESS study. 1 The Model 7425G Neurostimulator is identical to the Model 7425 Neurostimulator used in the clinical study. The Model 4351 Lead is similar to the Model 4300 Lead used in the clinical study. The Model 4351 Lead has a fixed electrode length of 10 mm, whereas the Model 4300 Lead had an adjustable electrode length. Enterra 4351 Implant Manual MA01352A004 Rev X 2012-06 13 Medtronic Confidential Pkg_R00a 4351_Enterra_CH.fm 2/16/12 3:10 pm 4 x 8 inches (101 mm x 203 mm) WCU entry criteria Candidates eligible for the WCU study consisted of those subjects who did not meet the complete entry criteria for the WAVESS study, but who had documentation of drug-refractory gastroparesis. The study entry criteria were: • Did not meet the entry criteria of the WAVESS Study • Were likely to die within the next few weeks if they did not receive this therapy • Signed an informed consent form relevant to this study This WAVESS Compassionate Use Study required: • Documentation of life-threatening situation by an independent physician • IRB (or IRB chairperson) approval on a case-by-case basis • An additional informed consent form relevant to the applicable patient’s condition was approved by the clinical investigator and the IRB or IRB chairperson (this varied depending on the reason(s) why the patient did not qualify for the WAVESS study) WCU study demographics A total of 24 subjects were enrolled in the WCU study. The demographic information on these subjects is presented in the table below: Table 3. Patient Demographics Diabetic Idiopathic Postsurgical 6 17 1 1M/5F 17 F 1F Age, mean 36.4 35.7 69.0 BMI, mean 20.5 23.1 18.4 N Gender Baseline: Vomiting Severity (mean) 3.5 3.6 4.0 Nausea Severity (mean) 3.3 3.6 4.0 GET 2 Hr (median) 74.0 67.0 18.0 GET 4 Hr (median) 34.0 22.0 2.0 WCU study design Subjects satisfying entry criteria received gastric stimulation systems which included an implanted neurostimulator connected to two unipolar leads which were implanted in the muscle wall of the stomach on the greater curvature at the limit of the corpus-antrum. All subjects received a Model 7425 implantable neurostimulator and a pair of Model 4300 leads. The stimulation parameters used in the study were: Intensity: 5 mA, Pulse Width: 330 µsec, Frequency: 14 Hz. The neurostimulator was set to deliver a pair of pulses at these parameters every five seconds continuously 24 hours per day. The stimulation parameters could be adjusted at any time by the physician to optimize treatment therapy. In contrast to the WAVESS study design, the WCU study was an unblinded, open label study. Upon implantation of the device within each patient, the stimulation therapy was immediately initiated without a randomized ON/ OFF cross-over period. Compassionate Use Electrical Stimulation Study (CUESS) The Compassionate Use Electrical Stimulation Study was an open label, non-randomized study that included a total of 51 subjects. This study was designed to provide gastric stimulation safety information. 14 2012-06 MA01352A004 Enterra 4351 Implant Manual Rev X Medtronic Confidential Pkg_R00a 4351_Enterra_CH.fm 2/16/12 3:10 pm 4 x 8 inches (101 mm x 203 mm) CUESS study objective The purpose of the Compassionate Use Electrical Stimulation Study was to treat patients with drug-refractory gastroparesis who had no other medical treatment alternative. CUESS entry criteria The inclusion criteria for the study were: • Symptomatic gastroparesis ≥ 1 year, as documented by an initial gastric emptying test (GET) • Refractory or intolerant to at least two antiemetic and prokinetic drug classes • On stable medical therapy during the month prior to enrollment • Frequency of vomiting > 7 vomiting or nausea episodes per week, as documented with a baseline patient diary • Delayed gastric emptying, defined by greater than 50% retention at two hours and > 6% retention at four hours, as measured by standardized gastric emptying testing The exclusion criteria were: • Organ transplant • Organic obstruction • Pseudo-obstruction • Scleroderma • Amyloidosis • Peritoneal or unstable dialysis • Chemical dependency • Pregnancy • Primary eating or swallowing disorders • Psychogenic vomiting • Implanted electronic medical devices • Age < 18 or > 70 years CUESS study demographics A total of 50 subjects were enrolled, screened, and qualified in the Compassionate Use Electrical Stimulation Study. The demographic information on these subjects is presented in the table below: Table 4. Patient Demographics Diabetic N Idiopathic Postsurgical* 22 19 9 10 / 12 F 1 / 18 F 1/8F Age, mean 39.8 44.5 48.8 BMI, mean 23.5 22.4 23.5 @ 2 Hours 79.5 51.0 73.5 @ 4 Hours 39.5 21.0 33.5 Gender (M/F) Gastric retention (median)% *Enterra Therapy System is not currently indicated for postsurgical gastroparesis CUESS study design Subjects satisfying entry criteria received gastric stimulation systems which included an implanted neurostimulator connected to two unipolar leads which were implanted in the muscle wall of the stomach on the greater curvature at the limit of the corpus-antrum. All subjects received a Model 7425 implantable neurostimulator and a pair of Model 4300 leads. The Enterra 4351 Implant Manual MA01352A004 Rev X 2012-06 15 Medtronic Confidential Pkg_R00a 4351_Enterra_CH.fm 2/16/12 3:10 pm 4 x 8 inches (101 mm x 203 mm) stimulation parameters used in the study were: Intensity: 5 mA, Pulse Width: 330 µsec, Frequency: 14 Hz. The neurostimulator was set to deliver a pair of pulses at these parameters every five seconds continuously 24 hours per day. The stimulation parameters could be adjusted at any time by the physician to optimize treatment therapy. In contrast to the WAVESS study design, Compassionate Use Electrical Stimulation Study was an unblinded open label study. Upon implantation of the device within each patient, the stimulation therapy was immediately initiated without a randomized ON/ OFF crossover period. WAVESS results The effectiveness results described below were obtained from the WAVESS study. Primary endpoint evaluations: Weekly vomiting frequency was determined for each patient diary. These data were further analyzed by Wilcoxon signed-rank test. For the combined patient group, median weekly vomiting frequency declined 49.6% in the ON period vs. the OFF period (p<0.05) (see Table 5). Before breaking the blind at the end of Phase I, 21 patients (10 diabetic, 11 idiopathic) preferred stimulation ON, while 7 (4 diabetic and 3 idiopathic) preferred stimulation OFF, and 5 (3 diabetic and 2 idiopathic) had no preference. These results were analyzed by the Mainland-Gart test and were statistically significant for the idiopathic and the combined group (p<0.05). At the end of Phase I, subjects were unblinded and given the option of having the device programmed ON or OFF. At the six month follow-up, all subjects had the device programmed ON. Each patient had the option of having stimulation turned OFF or ON at any time during the Phase II period. Table 5. Vomiting Frequency, WAVESS Phase I, All Subjects (N=33) Vomiting Episodes per Week Baseline ON OFF Difference (OFF-ON) % Difference Mean (N±SD) 37.3 ± 45.1 15.9 ± 25.0 23.6 ± 35.6 7.7 32.6 17.3 6.8 13.5 6.7 49.6 Median (N) Although 33 patients completed the two-month crossover period of the study (through Phase I), data at six months is provided for only 27 patients. Of these 27 patients, some patients had the device turned to the ON mode immediately at the end of the Phase I period, while others had the device turned ON later. By the end of the fourth month postrandomization, all 27 patients had the device turned ON. As a result, the vomiting frequency at six months documented in Table 6 was obtained from patients who received continuous stimulation for at least two months. Vomiting frequency results at 6 and 12 months post-implantation are shown in Tables 6–8. Table 6 includes data for all subjects, while Tables 7 and 8 include data for the idiopathic and diabetic gastroparesis groups, respectively. The vomiting frequency at 6 and 12 months was significant compared to baseline. Table 6. Vomiting Frequency, WAVESS Phase II, All Subjects All Patients Combined N Mean Number of Episodes, ± SD Median Number of Episodes 16 2012-06 MA01352A004 Baseline 6 Months % Difference Baseline 12 Months % Difference 33 27 — 33 24 — 37.3±45.1 13.7±30.2 17.3 2.6 -63 -85 Enterra 4351 Implant Manual Rev X 37.3±45.1 8.5±16.3 17.3 4.8 -77 -72 Medtronic Confidential Pkg_R00a 4351_Enterra_CH.fm 2/16/12 3:10 pm 4 x 8 inches (101 mm x 203 mm) Table 6. Vomiting Frequency, WAVESS Phase II, All Subjects (continued) All Patients Combined Baseline 6 Months % Difference Baseline 12 Months % Difference Patients with > 50% vomiting reduction vs baseline, N (%) — 16/27 (59) — — 18/24 (75) — Patients with > 80% vomiting reduction vs baseline, N (%) — 13/27 (48) — — 13/24 (54) — Table 7. Vomiting Frequency, WAVESS Phase II, Idiopathic Gastroparesis Subjects All Patients Combined N Mean Number of Episodes, +/–SD Median Number of Episodes Baseline 6 Months % Difference Baseline 12 Months % Difference 16 14 — 16 13 — 44.3±55.5 12.1±25.1 -73 43.3±55.5 11.8±21.2 -73 26.8 3.0 -88 26.8 4.5 -83 Patients with > 50% vomiting reduction vs baseline, N (%) — 9/14 (64) — — 10/13 (77) — Patients with > 80% vomiting reduction vs baseline, N (%) — 8/14 (57) — — 7/13 (54) — Table 8. Vomiting Frequency, WAVESS Phase II, Diabetic Gastroparesis Subjects All Patients Combined N Mean Number of Episodes Median Number of Episodes, +/–SD Baseline 6 Months % Difference Baseline 12 Months % Difference 16 13 — 16 11 — 30.3 ± 31.9 15.7 ± 36.4 13.4 2.6 -48 -80 30.3 ± 31.9 4.2 ± 3.9 13.4 Enterra 4351 Implant Manual MA01352A004 Rev X 4.9 -87 -63 2012-06 17 Medtronic Confidential Pkg_R00a 4351_Enterra_CH.fm 2/16/12 3:10 pm 4 x 8 inches (101 mm x 203 mm) Table 8. Vomiting Frequency, WAVESS Phase II, Diabetic Gastroparesis Subjects All Patients Combined Baseline 6 Months % Difference Baseline 12 Months % Difference Patients with > 50% vomiting reduction vs baseline, N (%) — 7/12 (58) — — 8/11 (73) — Patients with > 80% vomiting reduction vs baseline, N (%) — 5/12 (42) — — 6/11 (55) — WAVESS Secondary endpoint evaluations The results of secondary endpoint evaluations indicate that many patients experienced improvements in quality of life (73%) and ability to tolerate solid meals (73%). Additionally, there was a trend in improvement for gastric retention, subjective symptoms, and hypoglycemic attacks. Adverse events The adverse events information (Table 9) was obtained from the WAVESS study (N=27), the WAVESS Compassionate Use study (N=24), and the CUESS study (N=49). Adverse events were reported at each follow-up visit or at interim periods as appropriate in both studies. Table 9 summarizes those system related adverse events reported through May 22, 2003. 18 2012-06 MA01352A004 Enterra 4351 Implant Manual Rev X MA01352A004 Rev X Enterra 4351 Implant Manual 5 Pain at neurostimulator site 2 5 Irritation/inflammation over neurostimulator site Seroma at pocket 3 Lead impedance out of range 1 1 Lead revision 2 1 4 4 3 1 4 1 1 1 1 1 7 Patients 7 4 15 15 11 4 15 4 4 4 4 4 26 % of Patients 1 0 0 5 5 0 1 2 0 0 0 0 4 Events 1 0 0 5 5 0 1 1 0 0 0 0 4 Patients 4 0 0 21 21 0 4 4 0 0 0 0 17 % of Patients WAVESS Compassionate Use N=24 0 2 2 0 3 0 0 1 0 1 0 0 5 Events 0 2 2 0 2 0 0 1 0 1 0 0 5 Patients CUESS* N=49 0 4 4 0 4 0 0 2 0 2 0 0 10 % of Patients 4 x 8 inches (101 mm x 203 mm) Concomitant stimulation of abdominal rectus muscle 4 Lead penetration 1 Hematoma at pocket 1 1 Extrusion of neurostimulator through incision Neurostimulator migration 1 Device erosion 1 10 Device infections Infection in wound incision/abdominal wall Events Event description WAVESS N=27 Table 9. Summary Study of System Related Adverse Events* 4351_Enterra_CH.fm 2/16/12 3:10 pm Medtronic Confidential Pkg_R00a 2012-06 19 20 2012-06 MA01352A004 Rev X 0 0 0 0 0 0 0 0 Extra-abdominal pain Epigastric pain Surgical removal of IV access Electrical shocks with discomfort Enterra 4351 Implant Manual Patient “Can’t eat as well as before therapy.” Left side nerve rib pain Uncomfortable neurostimulator location Fluid collection at neurostimulator site with erythema over RLQ 0 0 0 0 0 0 0 0 0 0 0 0 Patients 0 0 0 0 0 0 0 0 0 0 0 0 % of Patients 0 0 0 0 0 0 0 0 0 1 1 2 Events 0 0 0 0 0 0 0 0 0 1 1 2 Patients 0 0 0 0 0 0 0 0 0 4 4 8 % of Patients WAVESS Compassionate Use N=24 1 2 1 1 1 1 1 4 1 0 1 0 Events 1 2 1 1 1 1 1 4 1 0 1 0 Patients CUESS* N=49 2 4 2 2 2 2 2 8 2 0 2 0 % of Patients 4 x 8 inches (101 mm x 203 mm) *Refer to “Table 9 Notes” on page 21 0 0 Failure of wound healing 0 Inability to program device/programming difficulty Tingling sensation 0 Events Surgical removal of system due to discomfort Event description WAVESS N=27 Table 9. Summary Study of System Related Adverse Events* 4351_Enterra_CH.fm 2/16/12 3:10 pm Medtronic Confidential Pkg_R00a 4351_Enterra_CH.fm 2/16/12 3:10 pm 4 x 8 inches (101 mm x 203 mm) Medtronic Confidential Pkg_R00a Table 9 Notes The decline in the rate of device-related adverse events from the WAVESS to the CUESS protocols may be related to several factors: • During patient enrollment in the WAVESS study, the protocol was modified to require intraoperative endoscopy to ensure that neither stimulating lead perforated the stomach. • During the WAVESS study, the physicians were encouraged to administer perioperative antibiotics to minimize the potential for infections at the implant site. • At one center, the majority of the 39 total cases implanted in the three protocols were done by one surgeon, and 4 infections (10.3%) were reported. • At another center, 11 systems were implanted in the three protocols and 5 infections (45.5%) were reported. All implant procedures in the WAVESS study and WAVESS Compassionate Use study were done by laparotomy, whereas 5 (10.2%) of the 49 in CUESS were done by laparoscopy. CUESS (N=49): Two diabetic patients who were implanted but did not qualify for the CUESS protocol were excluded from this summary table. Resterilization The Model 4351 lead and its accessories should not be resterilized. The Model 4351 lead and its accessories have been sterilized using ethylene-oxide. Inspect the sterile package for seal integrity and damage to the package before opening and using the contents. If you are unsure of the components’ sterility for any reason (except when the “Use by” date has expired), they should be returned to Medtronic. Please contact your Medtronic representative for instructions. Note: If contamination is suspected because of a defective sterile package seal, lead and accessories can be returned to Medtronic for replacement. Replacements are otherwise subject to terms of the Medtronic Limited Warranty (U.S. Customers). Enterra 4351 Implant Manual MA01352A004 Rev X 2012-06 21 4351_Enterra_CH.fm 2/16/12 3:10 pm 4 x 8 inches (101 mm x 203 mm) Medtronic Confidential Pkg_R00a Directions for use Implant the lead Implant two leads into the circular muscle layer along the greater curvature of the stomach (Figure 3), 10 cm proximal to the pylorus. Place the leads 1 cm apart for optimal stimulation (eg, 9.5 cm and 10.5 cm). Electrodes can be placed in a variety of angles, but they should be placed parallel to each other. The electrode placement angle should ensure that neither end of the lead has sharp bends or kinks when it is connected to the neurostimulator. Medtronic recognizes that a variety of approaches may be used to accomplish this; therefore, the following implant procedure is presented as one possible approach for the physician to consider. Figure 3. Place the leads 10 cm proximal to the pylorus and 1.0 cm apart. 1. Prepare the patient per normal procedures for abdominal surgery. Warning: It is recommended that the neurostimulator implant site be irrigated with antibiotic solution during surgery, and that IV antibiotics be administered perioperatively. When possible, identify and treat any infections remote to the implant site prior to surgery. Infections at the implant site almost always require the surgical removal of the implanted system. 2. 3. 4. 22 Note: To help facilitate implantation, you may prepare the system by tying sutures onto the trumpet anchor, fixation disk, and neurostimulator connector block. Do not use absorbable suture material. Using either a laparotomy or laproscopic surgical procedure, expose and visualize the antrum of the stomach. Note: If using laparoscopic approach, ensure that the port is sufficient in diameter to accommodate the lead. Measure 10 cm proximal from the pylorus. Use the needle to insert the lead into the circular muscle layer of the stomach. Place the leads 10 cm (eg, 9.5 cm and 10.5 cm) proximal to the pylorus and 1.0 cm apart and parallel to each other. Note: Position the lead into the stomach wall from the direction of the neurostimulator. Ensure that the lead placement angle avoids sharp bends or kinks. 2012-06 MA01352A004 Enterra 4351 Implant Manual Rev X Medtronic Confidential Pkg_R00a 4351_Enterra_CH.fm 2/16/12 3:10 pm 4 x 8 inches (101 mm x 203 mm) a. 5. Under endoscopic observation, insert the needle into a 2 cm length of tissue to ensure that the electrode will lie completely within the stomach wall muscle. b. Carefully pass the needle through the muscle. Stay clear of nerves and blood vessels to avoid possible injury to these structures. Notes: – When passing the needle, make sure the entire length of the 1.0 cm electrode and electrode tip will be positioned completely within the stomach muscle layer. – Use endoscopy to ensure that the needle is not exposed on the mucosal surface of the stomach. Insert electrode into muscle wall. a. Gently pull the blue polypropylene monofilament to insert the electrode into the muscle wall, making sure that the electrode tip and electrode lie within the stomach wall muscle tissue (Figure 4). Note: You may feel a slight resistance as the electrode passes into the muscle layer. b. Continue using endoscopy to ensure that the blue monofilament, lead, or electrode are not exposed on the mucosal surface of the stomach. Stomach wall Trumpet anchor Electrode Lead Connector Blue monofilament Ski needle Figure 4. Insert electrode into muscle wall. Caution: To ensure the lead does not perforate the stomach wall during lead insertion, it is recommended that the lumen of the stomach be observed endoscopically during the implant procedure. If penetration of the stomach wall by the lead, the needle, or the blue polypropylene monofilament is observed, it should be immediately withdrawn and reinserted without perforating the stomach wall. 6. When the lead is properly positioned, secure the lead to the serosal surface of the stomach, according to the instructions under “Anchor the lead” on page 23. Anchor the lead 1. 2. To anchor the distal portion of the lead (electrode tip), insert the needle through the center of the silicone rubber fixation disk. Note: Use one disk per lead to adequately anchor the lead. Slide the disk down the polypropylene filament until it is directly on the serosal surface (Figure 5). Enterra 4351 Implant Manual MA01352A004 Rev X 2012-06 23 4351_Enterra_CH.fm 2/16/12 3:10 pm 4 x 8 inches (101 mm x 203 mm) Medtronic Confidential Pkg_R00a Trumpet anchor Fixation disk Figure 5. Slide fixation disk to serosal surface. 3. 4. Note: Ensure that the fixation disk and the adjacent anterior serosal surface of the gastric antrum are flat and in the same plane. Use a minimum of two surgical clip(s) to anchor the disk onto the polypropylene filament. Note: When using the surgical clips, consult the manufacturer’s literature for information on selection and instructions for use. Secure the disk to the serosal surface through a minimum of two suture holes (ideally on opposite corners for stability). Caution: Keep the suture needles clear of the lead. The lead can be damaged by a suture needle. A damaged lead must be removed and replaced. 5. 6. 7. Suture both holes on the lead’s trumpet anchor to the serosal surface of the stomach. Ensure that the electrode is not exposed outside the muscle. Cut the polypropylene filament, leaving approximately a 2.5 cm “tail” from the end of the electrode. Repeat the procedure to implant (“Implant the lead” on page 22) and anchor (“Anchor the lead” on page 23) the second lead, placing it 1.0 cm from the first lead. Create pocket for neurostimulator 1. Create a subcutaneous pocket for the neurostimulator by blunt dissection to the anterior surface of the muscle. The neurostimulator is typically placed in the abdomen. Warnings: • Do not implant the neurostimulator near other implanted devices. Place the neurostimulator on the opposite side of the body from other implanted devices. Electrical impulses from the neurostimulation system may affect the sensing operation and cause inappropriate device response of other implanted devices. • It is recommended that the neurostimulator implant site be irrigated with antibiotic solution during surgery and that IV antibiotics be administered perioperatively. When possible, identify and treat any infections remote to the implant site prior to surgery. Infections at the implant site almost always require the surgical removal of the implanted system. Notes: • Placement below the ribs and above the hip bone provides a comfortable location for most patients. • To ensure proper programming, the neurostimulator should be located no more than 4 cm beneath the surface of the skin in subcutaneous tissue. The device must be placed parallel to the skin surface. The etched Medtronic logo and Enterra trademark side of the neurostimulator must face away from muscle tissue. If another 24 2012-06 MA01352A004 Enterra 4351 Implant Manual Rev X 4351_Enterra_CH.fm 2/16/12 3:10 pm 4 x 8 inches (101 mm x 203 mm) Medtronic Confidential Pkg_R00a neurostimulator is already implanted, ensure at least 20 cm between the two neurostimulators. • Do not presoak the neurostimulator. The neurostimulator is provided sterile and does not require any soaking in antibiotic solution, which can possibly affect lead connections. 2. Place the neurostimulator into the pocket to insure proper fit, and then remove it. 3. If necessary (eg, during laparotomy), use the tunneling rod (provided in the lead package) to pass the leads subcutaneously to the pocket. Using the tunneling rod helps prevent sharp angle bends of the lead body. a. Attach the connector end of each lead to the tunneling rod by inserting the connector pin into the small opening of the tunneler. b. Pass the tunneling rod through the fascia to the pocket (create a separate tunnel for each lead). c. Do not pull the lead taut; allow just enough slack to minimize component stress, tension, or migration, and allow for patient movement and for physiological movement of the stomach and other abdominal organs. Warning: The lead can become entangled with or erode into the bowel, which can result in bowel obstruction and perforation. Either may lead to life-threatening intra-abdominal infections and may require laparotomy, bowel resection, and system revision. Avoid excess lead slack in the abdominal cavity. Post implant, consider lead entanglement or erosion as a possible etiology in patients with bowel obstruction symptoms. d. e. To remove the lead from the tunneler, gently pull and twist off. Check that the lead connector pins and connector bodies are free of body fluids or tissue before connecting it to the neurostimulator. Connecting leads to neurostimulator 1. Prepare the neurostimulator block for connection to the lead by temporarily inserting the lead connectors. a. Wipe off any body fluids or tissue from the lead connector pins and the connector block before inserting the pins into the sockets. b. Insert the connector pins into the neurostimulator sockets (Figure 6). The connector pins must slide into the neurostimulator sockets until fully seated. Note: If inserting the lead pins is still difficult, use sterile water as a lubricant. Connector block Connector Sockets Figure 6. Insert connector pins into neurostimulator socket. c. If a setscrew obstructs the socket, back out the setscrew (Figure 7) only until the connector pin can slide in without force and then retighten. Enterra 4351 Implant Manual MA01352A004 Rev X 2012-06 25 Medtronic Confidential Pkg_R00a 4351_Enterra_CH.fm 2/16/12 3:10 pm 4 x 8 inches (101 mm x 203 mm) Caution: Limit counterclockwise rotations of the setscrew. Rotate it enough to provide an unobstructed pathway for the connector pins. Too many rotations may disengage the setscrew from the neurostimulator connector block. Grommet Figure 7. If needed, insert hex wrench into silicone rubber grommet and turn setscrew counterclockwise to back out setscrew. 2. When the lead connector pins are fully inserted in the neurostimulator sockets, do the following for each of the four setscrews: a. Insert the hex wrench through the rubber grommet to engage the setscrew. b. Tighten the setscrew by turning the hex wrench clockwise until resistance is felt (Figure 8). c. Continue tightening for a maximum of 1/4 turn. The setscrews must touch the connector pins for proper electrical connection. Note: Check the system impedance before placing the neurostimulator into the subcutaneous pocket. Cautions: • Discard the hex wrench after making all of the connections. The hex wrench is a single-use-only item. Its operation cannot be assured if it is used for multiple surgeries. • Do not overtighten the setscrews or permanent damage to the setscrews and/or sockets could result. • Verify that each leaf of the self-sealing grommet is closed after the hex wrench is withdrawn. If fluid leaks through a grommet seal that is not fully closed, the patient may experience shocking, burning, or irritation at the neurostimulator implant location, or intermittent stimulation, or loss of stimulation. Grommet Suture hole Hex wrench Suture hole Figure 8. Insert hex wrench and tighten all four setscrews. 3. Place the neurostimulator into the subcutaneous pocket (Figure 9) with the etched Medtronic logo side facing away from muscle tissue. Position the neurostimulator so that no sharp bends occur along the lead (Figure 10). Caution: Place the neurostimulator away from bony structures with the etched Medtronic logo and Enterrra trademark side facing out toward the skin and away from the muscle tissue to minimize the possibility of skeletal muscle stimulation, which may be perceived as twitching or burning. 26 2012-06 MA01352A004 Enterra 4351 Implant Manual Rev X 4351_Enterra_CH.fm 2/16/12 3:10 pm 4 x 8 inches (101 mm x 203 mm) Medtronic Confidential Pkg_R00a Figure 9. Place neurostimulator into subcutaneous pocket. Caution: Do not loop or coil the wire on top of the neurostimulator’s Medtronic logo side. Loosely wrap any excess wire around the perimeter of the neurostimulator (Figure 10). This avoids any increase in the subcutaneous pocket depth, minimizes potential damage during replacement surgery, and minimizes potential kinking of the wire. Correct wrapping Incorrect wrapping Figure 10. Wrap excess length around perimeter of neurostimulator. 4. Secure the neurostimulator in the subcutaneous pocket using both suture holes in the connector block. Caution: Failure to secure the neurostimulator using both suture holes may increase the risk of device migration or rotation, which can cause component damage, skin erosion, unintended stimulation effects, or lead dislodgement. 5. Check the neurostimulator function using the clinician programmer. Refer to “Verify impedance and close pocket” on page 28. Using lead end cap Use a lead end cap to seal off the connector pin if a lead is being reserved for connection to a neurostimulator at a future date, or if the lead has been abandoned, (ie, any leads not explanted, but also not connected to a neurostimulator). 1. Insert the end cap securely over the lead connector pin (Figure 11). Only sterile water may be used to facilitate this application; no adhesives are necessary. Enterra 4351 Implant Manual MA01352A004 Rev X 2012-06 27 4351_Enterra_CH.fm 2/16/12 3:10 pm 4 x 8 inches (101 mm x 203 mm) Medtronic Confidential Pkg_R00a Lead connector End cap Groove Figure 11. Insert end cap over lead. 2. Tie a non-absorbable, synthetic ligature in each end cap groove. Caution: Do not secure the ligature so tightly that it damages the end cap and the lead. If the end cap or lead are damaged it may require the surgical removal of the lead. The end cap can be removed at a later date without damaging the lead. After the end cap is removed, the lead can be reconnected to a neurostimulator. Verify impedance and close pocket 1. Before closing the pocket, program the neurostimulator and check impedance according to the programming instructions in the next section, “Program Enterra Therapy System”. Caution: A measured impedance outside the normal 200 to 800 ohm range may indicate that the electrical integrity of the Enterra Therapy System is compromised and should be investigated before closing the pocket. 2. 3. 4. 5. 28 Verify that the neurostimulator is secured in the subcutaneous pocket using both suture holes in the connector block. Close and dress the incision. Check the Enterra Therapy System impedance after the incision is closed, but before the patient leaves the operating room. This procedure is to verify electrical continuity between the leads and the neurostimulator. Verify and document lead and neurostimulator locations by obtaining lateral and anterior-posterior x-rays of the abdominal region up to 48 hours after the implantation procedure. Note: Based on your medical judgement, you may program the neurostimulator ON at this time, or wait until a later time. 2012-06 MA01352A004 Enterra 4351 Implant Manual Rev X Medtronic Confidential Pkg_R00a 4351_Enterra_CH.fm 2/16/12 3:10 pm 4 x 8 inches (101 mm x 203 mm) Program Enterra Therapy System This section describes the key aspects of programming the neurostimulator for therapy. For additional information about programming the Enterra Therapy System, refer to the software applications manual for either the Model 7457 MemoryMod Software Cartridge, the Model 7459 MemoryMod Software Cartridges, or the Model 8870 Software Application Card. Program basic neurostimulator parameters The Model 3116 neurostimulator is programmed from the factory. Typical initial parameter settings are listed in Table 10. The Model 7425G neurostimulator can be programmed to these values while it is still in the sterile package. Note: Except for Voltage (0.0) the Model 3116 is programmed to Table 10 values when it is shipped. Table 10. Typical Neurostimulator Parameter Settingsa Typical Settings for the Neurostimulator Voltage 2.0 Vb Pulse Width 330 µs Rate 14 Hz Output On/Off Mode: Cycling Magnetic switch function Electrodes: OFF ON 0.1 sec OFF 5.0 sec Disabled 0 OFF 1 OFF 2 Negative 3 Positive Case a b OFF Parameter settings for the neurostimulator are based on settings used in Medtronicsponsored clinical studies. For more information, refer to “Clinical studies” on page 11. Based on system impedance measurement and current setting of 5 mA. Caution: Due to the potential for uncomfortable stimulation (which some patients have described as a jolting, shocking, or burning sensation), do the following: • Take care when increasing the stimulation parameters to optimize or improve the therapeutic effect due to the potential for uncomfortable stimluation effects. Uncomfortable stimulation has been reported in neurostimulator settings at or above the typical settings. • Following changes in stimulation parameters, direct patients to test various postural changes and movements that mimic daily activities to assess the potential for uncomfortable stimulation. • If uncomfortable stimulation occurs, reduce the stimulation output to previously acceptable levels and adjust stimulation in smaller increments. • Adverse effects related to stimulation parameter changes may not manifest immediately following parameter changes; direct patients to contact their clinician if they feel discomfort related to their stimulation. Enterra 4351 Implant Manual MA01352A004 Rev X 2012-06 29 4351_Enterra_CH.fm 2/16/12 3:10 pm 4 x 8 inches (101 mm x 203 mm) Medtronic Confidential Pkg_R00a Table 11. Model 7425G Special Parameter Settings Other Settings for the Model 7425G Neurostimulator Neurostimulator Output OFF Dose OFF Special - Ramp OFF Special - ARES Normal Caution: Be sure that the Magnet Switch is programmed OFF to prevent the possibility of the neurostimulator inadvertently switching OFF or ON by stray magnetic fields. Program output current In order to program the standard output current used in the clinical studies, the system impedance must first be determined. Then, the required neurostimulator output voltage is determined by using a simple calculation. Calculate output voltage as follows: The standard output current used in clinical studies is 5 mA. To determine the standard output current, multiply the impedance measured by 0.005. For example, if the measured impedance is 500 ohms, the programmed voltage would then be 2.5 volts (500 x 0.005 = 2.5). Program the neurostimulator to that calculated voltage. To calculate other output currents, use the following impedance (Ω) formula: Ω x .006 for 6 mA Ω x .007 for 7 mA Ω x .008 for 8 mA Ω x .009 for 9 mA Ω x .010 for 10 mA Check the impedance as follows: Model 1. 2. 3. 4. 7432 Programmer Turn the printer ON. Press the REVIEW key on the programmer. Press CLEAR. Press IPG OUTPUT followed by IMP to measure impedance. Note: Normal impedance is between 200 and 800 ohms. 5. Calculate the voltage based on the formula above. 6. Press AMP, then select calculated voltage. 7. Press PROGRAM. Model 8840 Programmer 1. Select the therapy measurement icon on the programmer screen. 2. The therapy measurement area provides an impedance measurement, a targeted stimulation current, and a suggested voltage setting. 3. Review the measurement settings in the window. Select Accept if they are OK, and then Program. Note: Normal impedance is between 200 and 800 ohms. Warning: Tissue damage may occur for certain combinations of exposed electrode length, impedance, and programmed amplitude. See Table 12 for the maximum voltage to be applied to the electrode without inducing any tissue damage. At an electrode length of 10 mm, the neurostimulator may be programmed up to its maximum voltage of 10.5 volts if the measured impedance is 250 ohms or greater. 30 2012-06 MA01352A004 Enterra 4351 Implant Manual Rev X 4351_Enterra_CH.fm 2/16/12 3:10 pm 4 x 8 inches (101 mm x 203 mm) Medtronic Confidential Pkg_R00a Table 12. Maximum Voltage Max. charge density Pulse width Impedance Ω 0.4 µC/mm2 210 µsecs Voltage 150 7.7 V 200 10.2 V 250 > 10.5 V 300 > 10.5 V 350 > 10.5 V 400 > 10.5 V 450 > 10.5 V ≥500 > 10.5 V The table indicates the maximum voltage that can be applied between the electrodes without inducing any muscle tissue damage. Only the voltages appearing in the shaded area should be avoided. Maximum charge density of 0.4 µC/mm2 was extrapolated from: J.T. Mortimer, Kaufman D. and Roessmann U. Intramuscular electrical stimulation: Tissue damage. Ann. of BME, 2:235-244, 1980. Postoperative programming schedule Based on his or her medical judgement, the surgeon may program the neurostimulator either immediately after surgery or later. Enterra 4351 Implant Manual MA01352A004 Rev X 2012-06 31 4351_Enterra_CH.fm 2/16/12 3:10 pm 4 x 8 inches (101 mm x 203 mm) Medtronic Confidential Pkg_R00a Detailed device description Specifications Lead specifications* Lead length 35 cm Connector 3.2 mm Low Profile Material Conductor MP35N Nickel Alloy Suture Polypropylene Electrode Platinum Iridium Insulator Polyurethane Connector Stainless Steel Diameter Lead body 1.0 mm Electrode tip 0.9 mm Electrode coil 0.6 mm Exposed electrode Length 10 mm Electrode 26.8 mm2 Surface area Conductor Resistance 55 Ohms (25 cm) 75 Ohms (35 cm) 110 Ohms (50 cm) * All dimensions are nominal. 32 2012-06 MA01352A004 Enterra 4351 Implant Manual Rev X 4351_Enterra_CH.fm 2/16/12 3:10 pm 4 x 8 inches (101 mm x 203 mm) Medtronic Confidential Pkg_R00a Special notice Medtronic lead kits consist of leads and tools to connect the lead to neurostimulators. Leads are implanted in the extremely hostile environment of the human body. Leads may fail to function for a variety of causes, including but not limited to, medical complications, body rejection phenomena, or failure by breakage or by breach of their insulation covering. In addition, leads and tools packaged with the lead may easily be damaged by improper handling or use. For tools, Medtronic disclaims all warranties, both express and implied, including, but not limited to, any implied warranty of merchantability or fitness for a particular purpose. Medtronic shall not be liable to any person or entity for any medical expenses or any direct incidental or consequential damages caused by any defect, failure or malfunction of any tool, whether a claim for such damage is based upon warranty, contract, tort or otherwise. No person has any authority to bind Medtronic to any representation or warranty with respect to tools. Enterra 4351 Implant Manual MA01352A004 Rev X 2012-06 33 4351_Enterra_CH.fm 2/16/12 3:10 pm 4 x 8 inches (101 mm x 203 mm) Medtronic Confidential Pkg_R00a Warranty MEDTRONIC® NEUROLOGICAL LEAD LIMITED WARRANTY (U.S. Customers Only) A. This Limited Warranty provides the following assurance to the patient who receives any model of Medtronic® Model 4351 Neurological Lead, hereafter referred to as “Lead.” (1) Should the Lead fail to function within normal tolerances due to a defect in materials or workmanship within a period of one (1) year, commencing with the date of implantation of the Lead, Medtronic will, at its option: (a) issue a credit to the purchaser of the replacement Lead equal to the Purchase Price, as defined in Subsection A(2), against the purchase of any Medtronic Lead required as its replacement, or, (b) provide a functionally comparable Lead at no charge. (2) As used herein, Purchase Price shall mean the lesser of the net invoiced price of the original, or current functionally comparable, or replacement Lead. B. To qualify for this Limited Warranty, these conditions must be met: (1) The Lead must be implanted prior to its “Use By” date. (2) If the Lead or Lead portion is explanted, it must be returned to Medtronic within thirty (30) days of explantation and shall be the property of Medtronic, and if not explanted, then the Lead serial number or lot number must be provided instead. C. This Limited Warranty is limited to its express terms. In particular: (1) Except as expressly provided by this Limited Warranty, MEDTRONIC IS NOT RESPONSIBLE FOR ANY DIRECT, INCIDENTAL OR CONSEQUENTIAL DAMAGES BASED ON ANY DEFECT, FAILURE OR MALFUNCTION OF THE LEAD, WHETHER THE CLAIM IS BASED ON WARRANTY, CONTRACT, TORT OR OTHERWISE. (2) This Limited Warranty is made only to the patient in whom the Lead was implanted. AS TO ALL OTHERS, MEDTRONIC MAKES NO WARRANTY, EXPRESS OR IMPLIED, INCLUDING, BUT NOT LIMITED TO, ANY IMPLIED WARRANTY OF MERCHANTABILITY, OR FITNESS FOR A PARTICULAR PURPOSE WHETHER ARISING FROM STATUTE, COMMON LAW, CUSTOM OR OTHERWISE. NO EXPRESS OR IMPLIED WARRANTY TO THE PATIENT SHALL EXTEND BEYOND THE PERIOD SPECIFIED IN A(1) ABOVE. THIS LIMITED WARRANTY SHALL BE THE EXCLUSIVE REMEDY AVAILABLE TO ANY PERSON. (3) The exclusions and limitations set out above are not intended to, and should not be construed so as to contravene mandatory provisions of applicable law. If any part or term of this Limited Warranty is held to be illegal, unenforceable or in conflict with applicable law by a court of competent jurisdiction, the validity of the remaining portions of the Limited Warranty shall not be affected, and all rights and obligations shall be construed and enforced as if this Limited Warranty did not contain the particular part or term held to be invalid. This Limited Warranty gives the patient specific legal rights. The patient may also have other rights which vary from state to state. (4) No person has any authority to bind Medtronic to any representation, condition or warranty except this Limited Warranty. (5) This Limited Warranty is not applicable to the implantable neurostimulator, receiver or extension used with this Lead. *This Limited Warranty is provided by Medtronic Inc., 710 Medtronic Parkway, Minneapolis, MN 55432-5604. It applies only in the United States. Areas outside the United States should contact their local Medtronic representative for exact terms of the Limited Warranty. 34 2012-06 MA01352A004 Enterra 4351 Implant Manual Rev X 4351_Enterra_CH.fm 2/16/12 3:10 pm 4 x 8 inches (101 mm x 203 mm) Medtronic Confidential Pkg_R00a Enterra 4351 Implant Manual MA01352A004 Rev X 2012-06 35 4351_Enterra_CH.fm 2/16/12 3:10 pm 4 x 8 inches (101 mm x 203 mm) 36 2012-06 MA01352A004 Medtronic Confidential Pkg_R00a Enterra 4351 Implant Manual Rev X 4351_Enterra_EN_bcv.fm 2/16/12 3:10 pm 4 x 8 inches (101 mm x 203 mm) MA01352A004 Rev X Medtronic Confidential package_R00a 4351_Enterra_EN_bcv.fm 2/16/12 3:10 pm Medtronic Confidential package_R00a 4 x 8 inches (101 mm x 203 mm) Medtronic, Inc. 710 Medtronic Parkway Minneapolis, MN 55432-5604 USA www.medtronic.com Tel. 763-514-4000 Fax 763-514-4879 Toll-Free 800-328-0810 *MA01352A004* MA01352A004 Rev X © Medtronic, Inc. 2012 All Rights Reserved MA01352A004
© Copyright 2026