
1-s2.0-S1879729614000672-main
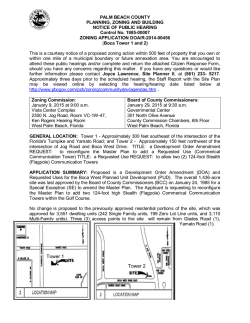
European Annals of Otorhinolaryngology, Head and Neck diseases 131 (2014) 265–266 Available online at ScienceDirect www.sciencedirect.com What is your diagnosis? Sudden bilateral hearing loss revealing polyarteritis nodosa F. Rubin , N. Tran Khai Hoan , P. Bonfils ∗ Département d’ORL et chirurgie cervico-faciale, hôpital Européen Georges-Pompidou, faculté de médecine Paris Descartes, université Paris V, 20, rue Leblanc, 75015 Paris, France 1. Description Ms L., 56 years old, consulted for an episode of fever (39.5 ◦ C) associated with asthenia, dry cough, tendon pain and sudden bilateral hearing loss. She was admitted to the internal medicine department in view of the persistent fever, severe asthenia, lower-limb pain-affecting gait, diffuse myalgia and night sweats. Weight-loss was moderate (2 kg). There was no infectious syndrome or headache. Clinical examination was normal. Initial biological assessment found biological inflammatory syndrome (leucocytes 9000/mm3 , CRP 143 mg/L, and slight microcytic anemia at 10.5 g/dL), without kidney failure. Otoscopy found bilateral serous otitis. Audiography (Fig. 1) found severe bilateral mixed hearing loss, with mean bone conduction deficit of 53 dBHL and mean Rinne 14 dBHL (BIAP). Temporal bone CT scan found moderate middle-ear effusion. Brain and internal auditory canal MRI found no tumors or signs of central nervous involvement. Ophthalmologic examination ruled out Cogan’s syndrome. The nasal cavities and nasopharynx were normal. Lumbar puncture and microbiology culture were negative. Paracentesis of the middle-ear sample found hematic inflammatory liquid with 120 elements/mm3 , 1800 erythrocytes/mm3 , 70 neutrophils/mm3 and 10 lymphocytes/mm3 , with negative culture. 2. Question 1 In sudden-onset bilateral hearing loss, what differential diagnosis is to be ruled out in priority? 3. Question 2 What diagnosis would you suggest? Fig. 1. Pure-tone audiogram. ∗ Corresponding author. E-mail address: pierre.bonfi[email protected] (P. Bonfils). http://dx.doi.org/10.1016/j.anorl.2014.03.003 1879-7296/© 2014 Elsevier Masson SAS. All rights reserved. What is your diagnosis? 266 F. Rubin et al. / European Annals of Otorhinolaryngology, Head and Neck diseases 131 (2014) 265–266 4. Reply 1 Stroke is to be ruled out urgently [1]. Disclosure of interest The authors declare that they have no conflicts of interest concerning this article. 5. Reply 2 References Presence of general signs suggested vascularitis. Temporal artery biopsy revealed lymphocytic arteritis. Polyarteritis nodosa (PAN) was diagnosed on American College of Rheumatology criteria: myalgia, neuropathy (sudden hearing loss with perceptual component) medium caliber arterial abnormalities. Corticotherapy (1 mg/kg/day) was initiated. All symptoms except hearing loss improved within a week. Audiometry at 3 months found bilateral 24 dBHL hearing loss. Only 3 cases of perceptual hearing loss and 4 of bilateral mixed hearing loss have previously been reported in association with PAN [2–5], with involvement of the arteries of the ear. [1] Shibata K, Matsui K, Ito H, et al. Bilateral intracranial vertebral artery dissection presenting as sudden bilateral hearing loss. Clin Neurol Neurosurg 2012;114:1266–9. [2] Vathenen AS, Skinner DW, Shale DJ. Treatment response with bilateral mixed deafness and facial palsy in polyarteritis nodosa. Am J Med 1988;84: 1081–2. [3] Joglekar S, Deroee AF, Morita N, et al. Polyarteritis nodosa: a human temporal bone study. Am J Otolaryngol 2010;31:221–5. [4] Adkins WY, Ward PH. Temporal bone showing polyarteritis nodosa, otosclerosis, and occult neuroma. Laryngoscope 1986;96:645–52. [5] Rowe-Jones JM, Macallan DC, Sorooshian M. Polyarteritis nodosa presenting as bilateral sudden onset cochleo-vestibular failure in a young woman. J Laryngol Otol 1990;104:562–4.
© Copyright 2026
![Download [ PDF ] - journal of evolution of medical and dental sciences](http://s2.esdocs.com/store/data/000478000_1-0e764d17efdf7e0f7a1db4e485c2c1ed-250x500.png)