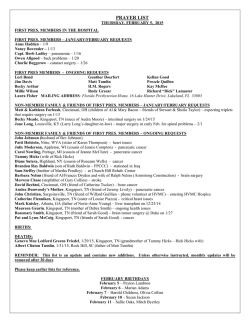
Block 5 Jan-Feb 2015
PRINCIPLES OF SURGERY LECTURE SCHEDULE (AY 2014-‐2015 Block 5) Rotation January 5, 2015 to February 27, 2015 Monday, January 5, 2015 ROOM 6065 Surgery Orientation 7:30-‐8:30 AM Acute Abdomen 10:00-‐10:30 AM Meade/Reed Jaffe Surgical Infections 8:30-‐9:00 AM Neonatal Physiology 10:30-‐11:00 AM Nichols Dr. Steiner Break 9:00-‐9:15 AM Adrenal Incidentloma 11:00-‐11:45 AM Kandil Procedures Consult 9:15-‐9:30 AM Lunch 11:45 AM 1:15 PM Volo Case Summary/Bullpen Orientation 9:30-‐10:00 AM Suturing/Knot Tying/Foley Cath 1:15-‐4:15 PM Jaffe NG Tube and IV/Lap Skills Endoscopy SIM Center (Murphy Bldg) Heaney/ Honor Surgery Students Tuesday, January 6, 2015 Room 6065 Hemorrhagic Shock/TEAM 8:00 -‐10:00 AM Lunch 12:00-‐1:00 PM Dr. Duchesne CS COT’s version of ATLS for medical students, called TEAM (Trauma Evaluation and Management), consist of lecture and 3 rotation stations. Break 10:00-‐10:15 AM Practical Information for 1:00-‐1:30 PM Medical Students Heaney Nutrition 10:15-‐10:45 AM Wound Healing 1:30-‐2:00 PM Killackey Wolfe OR Orientation 10:45 -‐11:15 AM Breast CA 2:00-‐2:30 PM Morrill, RN Jones Fluids and Electrolytes 11:15 AM-‐12:00 PM TEAM Questions 2:30-‐3:00 PM Paramesh Williams OR Orientation: You are part of a surgical team whose main objective is to provide quality patient care in a safe environment for staff and patients. Certain tasks seem mundane but each of us has a significant role and responsibility to meet this purpose. Since OR’s vary, you are responsible for following policies/procedures of the hospital to which you are assigned. Your Responsibilities: Come prepared with the knowledge of surgical procedure, anatomy and patient history. You will be asked to assist with positioning, prepping and possibly draping. If not, once gowned and 1 gloved, stand on the sterile field side of the room. Please wear clean Tulane green scrubs in the Operating Suites at Tulane. Scrub User and Pin # can be found on the biographic data sheet in E*value (scroll down to bottom of page) Also see page 41 for additional information. The Sim Center now has a YouTube Channel and all the Surgery Clerkship videos are published there and accessible by anyone. http://www.youtube.com/user/TulaneSimCenter Pre-surgery Lecture Test, Wednesday, January 7, 2015 from 7:00 – 8:00 AM in room 6065. Meet your team following the test, but confirm logistics the day before.OLOL and Baton Rouge LEAD students will take their test at those sites; therefore you will arrive at those sites on Wednesday, January 7, 2015. 2 GROUP 1 April, Daniel Chen, Stacey Foote, Sarah Grenadir, Jonathan Johnson, Haley McLaughlin, Angela Motejunas, Mark Rope, Alison Ullman, Stacey LABS – Monday January 5, 2015 (SIM Center) GROUP 2 GROUP 3 Beazer, Alex Bhagat, Sean Cohen, Ariel Curtis, Megan Freeman, Matthew Hallowell, Matthew Hadley, Graham Kaufmann, Ascher Kalantari, Saeed Ly, Quangminhy (LEAD) Marques, Christophe McMillan, Tyler Nix, Abigail Ohlstein, Jason Satija, Celine Sternlieb, Sarah Green, Deanna (LEAD) MacDonald (LEAD) Group 4 Burnett, James Dixon, Eunice Gold, Heather Haroldson, Kathryn Keeport, Daniel Moore, Robert O’Malley, Thomas Teja, nikhil Stations: ALL BELOW TRAINING W ILL BE D ONE O N THE 3 RD F LOOR O F THE S IMULATION C ENTER A T THE M URPHY BUILDING . Suturing & Knot Tying w/Honor’s Surgery Students in the CLASSROOM. You will be required to achieve the preset proficiency level for knot-tying and suturing by the end of your General Surgery clerkship; this grade is worth 5% of your final grade. Beyond the orientation/training day, you may use the skills lab to practice on your own time by making an appointment with the Sim Center staff ([email protected] or 988- 9150). You will also need to make an appointment to take the test once you feel you are ready. ALL TESTING AND PRACTICE HOURS MUST BE COMPLETED BY 5PM ON THE LAST MONDAY OF THE BLOCK (February 23, 2015). The time spent will be monitored as well as an attendance sheet will be kept. If you have achieved proficiency, you will contact the Sim Center to arrange to be tested. If you test as proficient, you will earn a 100%. (See Key Suturing and Knot tying elements in the handout portion of the website). A passing grade for suturing is 16/20 or better, and a passing grade for knot tying is 7/10 or better. If you failed either part, you need to practice as stated in the below chart, and then retest. This is a pass/fail module so if you passed both portions you will receive 100%. Surgery Clerkship Suture Testing Initial practice 1-2 hours (optional, but highly recommended) Test If fail, must practice 2 hours Test 2 If fail, must practice 3 hours Test 3 If fail, must practice 4 hours Test 4 – at this point you will have 10 hours for credit, even if you fail again Foley cath, NG Tube and IV insertion w/Dr. Heany in the PATIENT EXAM ROOM; Lap Skills w/Cheri Touchard in the LAPAROSCOPIC LAB • • • • • • • • OR Orientation Video Group 4 1:15 -2:00 Group 1 Group 2 Group 3 Group 3 2:00 - 2:45 Group 4 Group 1 Group 2 Group 2 2:45 - 3:30 Group 3 Group 4 Group 1 Group 2 Group 3 Group 4 Group 1 3:30 - 4:15 Lap Skills: You may be asked to observe or assist in laparoscopic cases during your clerkship. The skills you will practice in the lab help you better understand the technology and techniques of laparoscopy. Time Suture/Knot Tying Foley/ NG/ IV Lap Skills Foley Cath, NG Tube and IV Insertion: While also a required procedure for students to perform, Foley catheters, NG tube and IV insertion are regularly used in operating rooms and represent another way in which students can be involved in patient care, as well as being very helpful to the residents and staff. 3 NAME April, Daniel G. Beazer, Alex P. Bhagat, Sean Burnett, James W. Chen, Stacey Cohen, Ariel M. Curtis, Megan R. Dixon, Eunice E. Foote, Sarah E. Freeman, Matthew D. Gold, Heather L. Grenadir, Jonathan I. Hadley, Graham R. Hallowell, Matthew J. Haroldson, Kathryn L. Johnson, Haley M. Kalantari, Saeed Kaufmann, Ascher B. Keeport, Daniel N. McLaughlin, Angela Marques, Christophe McMillan, Tyler W. Moore, Robert F. Motejunas, Mark Nix, Abigail F. Ohlstein, Jason F. O'Malley, Thomas J. Rope, Alison M. Satija, Celine Sternlieb, Sarah J. Teja, Nikhil Ullman, Stacey M. Green, Deanna (Lead) MacDonald, Matt (Lead) Ly, Quangminhy (Lead) January 7, 2015 to February 1, 2015 General Surgery (VA) Colorectal Surgery (East Jeff) CT/Vascular (TMC) Colorectal Surgery (East Jeff) GS/Trauma (University) Hepatobiliary (TMC) Acute Care (TMC) Pediatric Surgery (Childrens) General Surgery (Thibodaux) Breast Surgery (TMC Lakeside) Hepatobiliary (TMC) Pediatric Surgery/Transplant (Ochsner) GS/Oncologic (West Jeff) Thoracic/Pediatric Surgery (Ochsner) Acute Care (TMC) OLOL 2 Acute Care (TMC) CT/Vascular (TMC) GS/Trauma (University) Elective (TMC) OLOL 1 GS/Trauma (University) Elective (TMC) Pediatric Surgery (Childrens) General Surgery (Thibodaux) GS/Trauma (University) Hepatobiliary (TMC) GS/Oncologic (West Jeff) Acute Care (TMC) Breast Surgery (TMC Lakeside) Transplant/Thoracic (Ochsner) Elective (TMC) BR General BR General BR General 4 February 2-25, 2015 Pediatric/Thoracic (Ochsner) Thoracic/Transplant (Ochsner) General Surgery (Thibodaux) Acute Care (TMC) Breast Surgery (TMC Lakeside) General Surgery (Thibodaux) Pediatric Surgery (Childrens) Hepatobiliary (TMC) Colorectal Surgery (East Jeff) Acute Care (TMC) General Surgery (VA) CT/Vascular (TMC) GS/Trauma (University) Acute Care (TMC) Transplant/Pediatric (Ochsner) CT/Vascular (TMC) Breast Surgery (TMC Lakeside) GS/Oncologic (West Jeff) Colorectal Surgery (East Jeff) Acute Care (TMC) Hepatobiliary (TMC) Elective (TMC) GS/Trauma (University) GS/Trauma (University) GS/Oncologic (West Jeff) Pediatric Surgery (Childrens) OLOL 2 Hepatobiliary (TMC) Elective (TMC) Elective (TMC) GS/Trauma (University) OLOL 1 BR General BR General BR General HOSPITAL January 7, 2015 to February 1, 2015 TMC/Acute Care Curtis, Megan Haroldson, Kathryn Kalantari, Saeed Satija, Celine Breast Surgery (Lakeside) Freeman, Matthew Sternlieb, Sarah Colorectal Surgery Beazer, Alex (East Jefferson) Burnett, James General Surgery/ Oncologic Hadley, Graham (West Jefferson) Rope, Alison General Surgery Foote, Sarah (Thibodaux Regional Med Center) Nix, Abigail TMC Hepatobiliary Cohen, Ariel Transplant Gold, Heather O’Malley, Thomas Pediatric Surgery Dixon, Eunice Children’s Motejunas, Mark Trauma/University Chen, Stacey Keeport, Daniel McMillan, Tyler Ohlstein, Jason TMC/CT Vascular Bhagat, Sean Kaufmann, Ascher TMC/Elective McLaughlin, Angela Moore, Robert Ullman, Stacey TMC/ General Surgery VA April, Daniel Ochsner: Transplant/Thoracic Teja, Nikhil Thoracic/Pediatric Surgery Hallowell, Matthew Pediatric Surgery/Transplant Grenadir, Jonathan OLOL 1 Marques, Christophe OLOL 2 Johnson, Haley BR General (Lead) Green, Deanna BR General (Lead) MacDonald, Matt BR General (Lead) Ly, Quangminh February 2-25, 2015 Burnett, James Freeman, Matthew Hallowell, Matthew McLaughlin, Angela Chen, Stacey Kalantari, Saeed Foote, Sarah Keeport, Daniel Kaufmann, Ascher Nix, Abigail Bhagat, Sean Cohen, Ariel Dixon, Eunice Marques, Christophe Rope, Alison Curtis, Megan Ohlstein, Jason Hadley, Graham Moore, Robert Motejunas, Mark Teja, Nikhil Grenadir, Jonathan Johnson, Haley McMillan, Tyler Satija, Celine Sternlieb, Sarah Gold, Heather Ochsner: Pediatric/Thoracic Transplant/Pediatric Thoracic/Transplant Ullman, Stacey O’Malley, Thomas Green, Deanna MacDonald, Matt Ly, Quangminh April, Daniel Haroldson, Kathryn Beazer, Alex Students will be expected to attend clinic 1 day a week with a faculty member of your team; the residents will make those assignments! 5 CONTACT INFORMATION CHIEF RESIDENTS: ACUTE CARE/TMC (Brown/Meade/Schroll) Name Ivane Chua, MD (January) Ryan Couvillion, MD (February ) Pager 504.538-2636 504.423-4727 BREAST SURGERY/LAKESIDE (Dr. Jones) Melanie Jeansonne, Clinic RN Jeremy John, MD (January) Shannon McChesney (February) 504.988-8169 Office 504.538-0852 504.538-1784 CT/Vascular (TMC) (Sam) Joana Ochoa, MD (January) Megan Garstka, MD (February) 504.538-2074 504.538-0627 COLORECTAL SURGERY (EJ) (Griffin) Ryan Couvillion, MD (January) Eric Simms, MD (February) 504.423-4727 504.569-5554 Elective/TMC (Kandil/Slakey/Korndorffer) Chris Martin, MD (January) Ivane Chua, MD (February) 504.582-9734 504.538-2636 GS Oncologic (West Jeff) (Minnard) Matt Zelhart, MD 504.268-1408 General Surgery/Thibodaux Regional Dr. Landry HEPATOBILIARY (TMC) (Buell/Killackey/Paramesh) Jennifer Turney, MD 504.268-1406 CHILDREN’S PEDIATRIC SURGERY (Yu) Ashlie White, MD 504.268-3109 TRAUMA/UNIVERSITY (Meade/Scholl) Samantha Zeringue, MD 504.213-0239 General Surgery (VA) (Korndorffer/Griffin) Eric Simms, MD (January) Chris Martin, MD (February) 504.569-5554 504.582-9734 Office: 985.446-1763 Ochsner Department of Surgery Reporting Information: Upon arrival, ALL surgery students must first report to Melissa Johnson, at 8:30 AM located at Ochsner Academic Center, UGME receptionist, 1514 Jefferson Highway. Please bring $10.00 CASH, as a refundable deposit for your temporary Ochsner ID badges. After your rotation, you need to bring back your ID badge. Please print pages 4 and 5 of the Scrub Class Documents and bring with you to your scrub class. You must have these documents in order to attend scrub class (An email from Stacey Porter will be sent prior to start of your rotation). Transplant Drs. Ahmed, Bohorquez, Bruce, Carmody, Cohen, Reichman, and Seals Transplant Surgery Thoracic Dr. Pettiford Thoracic Surgery/Esophageal and Lung Pediatric Surgery Drs. Adolph, Roybal and Steiner Pediatric Surgery The first two week surgeons will do the two week mid-block evaluation and the 2nd two week surgeons will do the final evaluation on each student. Ochsner Office Contact: Melissa Johnson, Clerkship Program Coordinator, 1514 Jefferson Highway, New Orleans, LA 70121 Office: 504.842-0558; Fax: 504.842-4805 [email protected] 6 OLOL 1/Baton Rouge Clinic Dr. Glen Schwartzberg [email protected] OLOL 2 /The Surgeons Group of Baton Rouge Dr. John Whitaker [email protected] Baton Rouge Campus Clerkship Director: Dr. David Depp [email protected] Baton Rouge Campus Community Preceptors: Dr. Dhaval Adhvaryu Dr. Everett Bonner Dr. Peter Bostick Dr. Stephen Gordon Dr. Alec Hirsch Dr. Michael Puyau Dr. Jon Schellack Roberta Cartaginese LEAD Senior Program Coordinator Tulane University School of Medicine – Baton Rouge Campus 3600 Florida Blvd. Baton Rouge, LA 70806 225-387-7732 office 225-252-4186 cell Thibodaux Regional Medical Center Thibodaux Surgical Specialists 604 North Acadia Road, Suite 207 Thibodaux, LA 70301 Office: 985.446-1763 Nadine Hebert, Office Manager William B. Bisland, Jr., M.D. (General/Laparoscopic/Bariatric Surgery) Mark F. Hebert, M.D. (General Surgery) Barry G. Landry, M.D. (General Surgery) [email protected] Cell: 985.209.3652 Brian J. Marino, M.D. (General Surgery) 7 SURGERY CLERKSHIP COURSE DIRECTOR: PROGRAM COORDINATOR: HOLIDAY: Peter C. Meade, M.D. (988-2305 Room 8524) [email protected] Stephanie Reed (988-3909 Room 8549) Fax 988-1882 [email protected] MLK – January 19, 2015 – students must fulfill clinical responsibilities. Mardi Gras – February 16-17, 2015 REQUIRED READING: SUGGESTED READING MATERIAL: Essentials of General Surgery (Fifth Edition) by Peter F. Lawrence Sabiston Textbook of Surgery, 19th edition, (ed.) (Basic Science) Current Surgical Therapy 8th ed (Cameron, ed-in chief) Chapters on Pneumothorax, hemothorax, carotid enderectomy, and section on Preoperative and Post-operative care. Surgery: A compentency-Based Companion by Barry D. Mann (available in the bookstore.) Cope’s Early Diagnosis of the Acute Abdomen, Twenty Second Edition, William Silen NOTE: It is not expected for you to read the entire book for any of the suggested reading. It takes the residents about one year to finish one book. You should read the sections in the books that are pertinent to the patients you are seeing and the operations which you are attending. When you have time, if you have not covered hernia, gallbladder, bowel obstruction, acute abdomen, colon and breast cancer, (and any other topics you all can think of), read those chapters as well. “The Virtual Patient” Self-directed Study Guide in Surgery (2007) Copyright from the University of Texas Southwestern Medical Center at Dallas can be used as a study guide. Link: http://tmedweb.tulane.edu/portal/studentguide/item/surgery Some links that you may find helpful are listed below: Students with disabilities: http://erc.tulane.edu/disability/ Academic dishonesty link: http://www.som.tulane.edu/student/honorcode/new.htm SOM Phase I & II Objectives: http://tulane.edu/som/ome/upload/Tulane_SOM_Learning_Objectives_Phase_1_-‐_21.pdf RESOURCES: Several new learning resources have been added to the educational armamentarium of the clerkship. They include: 1. Procedures Consult – The web based learning process provides considerable information, editorial, videos of specific operational procedures. Weekly assignments are made and students are expected to complete them and take the brief examination. Completion of the assignments will be monitored. (Instructions for login attached at end of document; use your Tulane email address and the password is hello1. Please login in prior to the start of rotation and notify Stephanie Reed if unable to login in order to address issues of problems before the assignments are due. Assignments Assigned Date Due by/on T3s#24-1 01/07/15 01/14/15 T3s#24-2 01/07/15 01/21/15 T3s#24-3 01/07/15 01/28/15 T3s#24-4 01/07/15 02/04/15 T3s#24-5 01/07/15 02/11/15 T3s#24-6 01/07/15 02/18/15 T3s#24-7 01/07/15 02/25/15 In addition to the assignments, students are encouraged to review the material in Procedures Consult which is relevant to their patients. 8 2. Resident Lectures – On each service, the residents have been assigned lectures to present to the students on their service. The same topics will be presented each week on all services. The lectures and topics are all among the 27 topics listed below. The following topics are to be covered: Week 1 (01/12/15) Femoral Artery Occlusions Week 2 (01/19/15) Hemorrhoids Fistula-in-Ano Week 3 (01/26/15) Inguinal Hernia Week 4 (02/02/15) Obstructive Jaundice Week 5 (02/09/15) Appendicitis Week 6 (02/16/15) Melanoma Week 7 (02/23/15) Carotid Disease Grand Rounds – Grand Round lectures will be recorded using Mediasite. The recording is available on the Surgery minisection on TMedWeb, link http://tmedweb.tulane.edu/portal/t3t4 - At TMedWeb website: choose a Clerkship Article to View; Select the Surgery tab; Click Grand Rounds Recording. OBJECTIVES OF THE ROTATION: Surgery is a discipline that provides care to patients in the outpatient areas, hospital ward, and operating room. The clerkship is designed to teach students the role of surgical care in the overall management of patients. Specifically, the students are expected to learn the work-up and evaluation of surgical patients. The indications and contraindications for expected results, risks and complications of specific operations. While the operating room is one site of leaning, it is NOT the only site. Students are expected to be able to scrub on a number of operations, but involvement in a large number of operations is NOT the goal of the rotation. Ideally, students will be able to follow patients from presentation, work-up, treatment including operations and post-treatment/postoperative care. It is this continuum that is the major goal of the clerkship. Twenty-seven diseases have been selected as targets for your education. They are listed below: ACUTE Surgical Infections Acute Pancreatitis Hemorrhagic Shock Cholecystitis Nutrition Abdominal Trauma Appendicitis Diverticulitis Thoracic Trauma GENERAL Peripheral Vascular Disease Peptic Ulcer Disease Inguinal Hernia Carotid Disease Upper Gastrointestinal Bleeding Postoperative Complications Reflux Esophagitis Fistula-in-Ano Portal Hypertension ONCOLOGY Breast Cancer Adrenal Mass Thyroid Nodule Obstructive Jaundice Colon Cancer Splenectomy for Disease Intestinal Obstruction Lung Cancer Melanoma The Department of Surgery expects you to study these diseases on the rounds, in the operating room if possible, in the classroom, and at home using textbooks. The oral examination will focus on these 27 topics. DESCRIPTION: All students are to assemble for the Principles of Surgery portion of the clerkship. This series of lectures is designed to provide you with: 1. A surgical perspective relative to fundamental topics in Medicine 2. Basic technical skills in knot-tying & suturing A written examination (consisting solely of questions taken from the lecture material and lab day) will be administered upon completion of this lecture series (Wednesday, January 7, 2015 from 7:00-8:00 AM in room 6065). An oral examination will be administered to each student shortly before the NBME examination. Upon completion of General Surgery Services, a National Board of Clinical Sciences Examination will be administered. Your clinical duties will end at 7:00 p.m. on the Wednesday (February 25, 2015) immediately prior to Friday’s final examination, Friday, February 27, 2015, Murphy Building; report at7:30 AM, testing begins promptly at 8:00 AM. No additional time will be granted from clinical duties for study preparation. 9 FINAL GRADE: Student Evaluations: 1st General Surgery 2nd General Surgery 25%* 25%* Examinations: National Board Surgery Examination Oral Examination (General Surgery) Knot Tying & Suturing Principles of Surgery Examination Case Summaries 25%* 10% 5% 5% 5% TOTAL 100% GRADING POLICY: To receive a grade of “pass”, a student must achieve acceptable standards on both the National Board Examination (equivalent to a score in the 5th percentile, and on each of the student evaluations. These requirements are marked with an asterisk above. Should a student fail only the National Board Examination (and receive passing grades on each clinical rotation), a letter grade of “C” (Condition) will be assigned. Given those circumstances, the student will be asked to undertake a period of intense reviewing of the precepts in General Surgery – upon completion of the remainder of their academic year. A second National Board Examination will be offered; should he/she fail this examination, that student will be required to repeat the entire General Surgery clerkship prior to January of the graduating year. A student who receives a failing grade on any of the faculty evaluation forms will be notified immediately, and the General Surgery Medical Student Curriculum Committee will review their clerkship performance. Unless evidence is presented to the contrary, the student will receive a grade of “F”, and be asked to repeat, and pass elements of the entire General Surgery clerkship prior to January of the graduating year. You will have a mid block evaluation 2 weeks into your General Surgery clerkship by your resident and faculty. If you do not receive this mid block evaluation, please discuss this with your resident. A distinctly superior performance by a medical student on this clerkship will be properly accorded a letter grade of “High Pass” or “Honors. A candidate for “High Pass” must have established the following: In most, if not all areas, numerical grades that consistently signify a quality performance and must receive at the national mean average (70) on the national board exam. A candidate for “Honors” must have established the above criteria and in addition, must receive at the national mean average or higher on the national board exam which is a 75.4. There is no exception to the above. Honors – 90 -‐100; High Pass – 87-‐89.99; Pass 80-‐86.99; Condition 65-‐79; Fail <65 In the student letter to the Dean’s Office, the course director will at minimum, summarize the written comments received by the student on the rotation assessment forms. A statement as to the students’ performance on the National Board Clinical Sciences Examination may be included in each letter. STUDENT ASSESSMENT: Evaluation Forms: Each faculty and highest level resident will receive an evaluation form, designed to assess your progress in mastering the fundamentals in surgery, and will contain their consensus of your progress. Oral Examination: You will be assigned a faculty member in the Department of Surgery who is responsible for administering your oral examination (see table for your assignment on page 11-12) (page 37-38). Oral exams are to be scheduled between, Thursday, February 12, 2015 (DO NOT WAIT UNTILTHE 12th TO SCHEDULE) and must be completed by Wednesday, February 25, 2015 (with the exception of the OLOL students on the rotation for the period of February 2-25, 2015 must be completed after the shelf exam on Friday, February 27, 2015). It is your responsibility to contact the office of the assigned staff member to mutually set aside ½ hour, during the final week of the rotation, for this examination. The date and time of the exam are the choice of the examiner. Any student who fails the oral examination will be asked to retake the test until a minimally acceptable performance is achieved (<70) and the grades will be averaged for a final grade. 10 Student Faculty Contact April, Daniel G. Beazer, Alex P. Bhagat, Sean 02/27/15 1:00 PM Trauma Faculty Trauma Faculty Dr. Bernard Jaffe Nakisha Farria 988-5111 [email protected] Nakisha Farria 988-5111 [email protected] [email protected] Dr. Korndorffer Angela Stewart 988-7123 [email protected] Maria Reynaud 988-7867 [email protected] [email protected] Burnett, James W. Chen, Stacey Cohen, Ariel M. 02/27/15 1:30 PM Curtis, Megan R. Dixon, Eunice E. Foote, Sarah E. 02/19/15 1:00 PM Freeman, Matthew D. Gold, Heather L. Transplant Faculty Dr. Bernard Jaffe Transplant Faculty Dr. James Brown Dr. Bernard Jaffe Plastic Faculty Plastic Faculty Dr. Korndorffer Grenadir, Jonathan I. Hadley, Graham R. Hallowell, Matthew J. Dr. James Brown Dr. Emad Kandil Dr. Steven Jones Haroldson, Kathryn L. Johnson, Haley M. Kalantari, Saeed Kaufmann, Ascher B. Keeport, Daniel N. Dr. James Brown Transplant Faculty Dr. Douglas Slakey Dr. Emad Kandil Dr. Steven Jones McLaughlin, Angela Marques, Christophe Trauma Faculty 11 Maria Reynaud 988-7867 [email protected] [email protected] or Lauren Dickerson 988-2307 [email protected] [email protected] Debra Felix Office 504.988-5500 [email protected] Debra Felix Office 504.988-5500 [email protected] Angela Stewart 988-7123 [email protected] [email protected] or Lauren Dickerson 988-2307 [email protected] Lauren Dickerson 988-2307 [email protected] Melanie Jeansonne, Clinic RN 504.988-8169 or 504.988-8100 [email protected] or [email protected]; or Lauren Dickerson 988-2307 [email protected] [email protected] or Lauren Dickerson 988-2307 [email protected] Maria Reynaud 988-7867 [email protected] Mel’isa Morel [email protected] Lauren Dickerson 988-2307 [email protected] Melanie Jeansonne, Clinic RN 504.988-8169 or 504.988-8100 [email protected] or [email protected]; or Lauren Dickerson 988-2307 [email protected] Nakisha Farria 988-5111 [email protected] McMillan, Tyler W. Moore, Robert F. Motejunas, Mark Nix, Abigail F. 02/19/15 1:30 PM Ohlstein, Jason F. O'Malley, Thomas J. 02//27/15 2:00 PM Rope, Alison M. Satija, Celine Sternlieb, Sarah J. Teja, Nikhil Ullman, Stacey M. 02/27/15 2:30 PM Dr. Cliff McGinnis Dr. Bernard Jaffe Lauren Dickerson 988-2307 [email protected] Maria Reynaud 988-7867 [email protected] Maria Reynaud 988-7867 [email protected] [email protected] Dr. Douglas Slakey Dr. Bernard Jaffe Mel’isa Morel [email protected] [email protected] Dr. Cliff McGinnis Lauren Dickerson 988-2307 [email protected] Maria Reynaud 988-7867 [email protected] Nakisha Farria 988-5111 [email protected] Lauren Dickerson 988-2307 [email protected] [email protected] Transplant Faculty Transplant Faculty Transplant Faculty Trauma Faculty Dr. Cliff McGinnis Dr. Bernard Jaffe 12 FRIDAY EDUCATION CONFERENCES: Entire Rotation: DRESS APPROPRIATELY for conferences, SCRUBS ARE NOT APPROPRIATE! IF YOU QUESTION WHAT IS APPROPRIATE, ASK YOU RESIDENT. 1. M & M: 7:00 AM-8:00 AM in room 6065. This conference will be attended by surgical faculty, residents and medical students. This educational conference is designed to teach the pathophysiology and decisionmaking process regarding complex and interesting surgical cases and surgical cases that result in a complication. 2. Department of Surgery Grand Rounds: 8:00 AM-9:00 AM in room 6065 Presentations at this conference will be by department faculty, invited lecturers and surgical residents as assigned by the chairman. These presentations should last 30-40 minutes, with a period of questions and answers if one lecture is to be given. On certain dates, two case presentations may be given, each lasting approximately 20 minutes. This format will be used primarily for resident presentations. You will receive by e-mail prior to the Grand Rounds to inform you of the topic. 3. Bullpen (See page 14-15): 8:00 AM/9:00 AM-10:30 AM (time changes as noted) in Room 6001 4. Case Summary & Subspecialty Lectures (see pages 17-23): 9:30/10:30 AM to 12:30 PM (time changes as noted) in Room 6001 13 Date M&M 7 AM Room 6065 Grand Rounds 8 AM Room 6065 01/09/15 01/16/15 01/23/15 01/30/15 02/06/16 No Grand Rounds 02/13/15 02/20/15 Bullpen Students Presenting Room 6001 Case Summary and SubSpecialty lectures/conferences Room 6001 Faculty 9:00 AM w/Jaffe Bhagat, Sean Freeman, Matthew Kaufmann, Ascher Ullman, Stacey 10:00 AM w/Meade April, Daniel Cohen, Ariel Haroldson, Kathryn Ohlstein, Jason 9:00AM w/ Jaffe Beazer, Alex Curtis, Megan Kalantari, Saeed McLaughlin, Angela Moore, Robert 10:30 AM Case Summary “Colon CA” 11:30 AM Lecture: “Neurosurgery” 10:30 AM Case Summary: “Pancreatitis” 11:30 AM Lecture: “Orthopaedic Surgery” (stretcher to be provided) Dr. Jaffe Dr. Michael O’Brien 9:00 AM w/Slakey O’Malley, Thomas Chen, Stacey Keeport, Daniel McMillan, Tyler Sternlieb, Sarah 10:00 AM w/Jaffe Hallowell, Matthew Johnson, Haley Marques, Christophe Rope, Alison Teja, Nikhil 8:00 AM w/Jaffe Burnett, James Foote, Sarah Hadley, Graham Nix, Abigail Satija, Celine 9:00 AM w/Kandil Dixon, Eunice Gold, Heather Grenadir, Jonathan Motejunas, Mark 10:30 AM Lecture: “Urology” 11:30 AM Case Summary “Lung CA” Dr. Thomas Dr. Kukuy 9:00 AM Case Summary: Dr. Kandil “Thyroid” 11:30 AM Lecture: Dr. White “ Neonatal Obstruction” 9:00 AM Case Summary: Dr. Korndorffer “Reflux Esophagitis” 11:30 AM Lecture: ENT Chief Resident “Otolaryngology” 10:00 AM Case Summary: “Intestinal Obstruction” Dr. Brown 10:30 AM “Shelf Prep” Case Summary Conference: All students are invited to discuss their case scenarios. 14 Dr. Jaffe Dr. Juanita Garces Honors Surgery SURGICAL BULLPEN Background: The Surgery Bullpen is an exercise for students to hone their case presentation skills as well as learn pathophysiology and management of surgical diseases. The contemporary Bullpen is based upon a tradition begun by Dr. Alton Ochsner nearly seventy years ago. Senior Tulane students were assigned an unknown patient and were expected to determine the diagnosis and differential, treatment plan and the pathophysiology following a brief history and physical examination without the patient chart or other information. The exercise was modified and extended to the third year clerkship in a way similar to the present Bullpen. The Tulane Surgical Bullpen gained national notoriety and was described in an article in Time Magazine nearly fifty years ago. The Rules: Four to Five students are assigned to present at Surgical Bullpen each Friday at 9:00 am in Room 6001. Each presentation is approximately fifteen minutes. Students are assigned patients by Dr. Jaffe and the student coordinator, Ms. Stephanie Reed, on the preceding Monday afternoon, and she will contact you with the name and bed of the patient. The patients will be from Tulane University Hospital and University. You should review the patient’s chart, do a history and physical examination where appropriate and review pertinent laboratory and radiographic studies. Sometimes the patients are too ill or incapacitated to give a history or to even be examined. Use your own judgment, but remain sensitive to the patient’s situation, comfort and dignity. Frequently, all of your information must come directly from the chart and not from the patient. If so, simply make that clear in your presentation. Presentations should be made just as if you were in the hospital. Decorum requires you to wear your white coat and for men to either wear ties or scrub suits and women accordingly. Make your presentations concise and precise. If possible bring radiographs, arteriograms or other imaging studies which add value to the presentation. University no longer permits the students to check out films. You receive the film on a CD rom. If it is of value to present the film, a lap top will be made available in Room 6001 for your presentation. Do not prepare Power Point, overheads, hand outs, or movies, but you are free to use your notes and to draw anatomy, procedures and other diagrams on the black board when indicated. You may prepare by textbook reading and review of articles. Since patients are currently discharged very soon after uncomplicated operations, occasions do arise when the patient has been discharged prior to your visit to them. If that occurs, you will simply present from the chart but indicate this during your presentation. Please do not use this conference for your lunch time. No food or drinks are allowed while this Bullpen is taking place. Thank you. 15 CASE SUMMARY GRADE FORM • Organization 25% Grade • Content 50% Grade • Clarity, grammar & style 15% Grade • References 10% Grade • “Bonus Points” Total Grade 16 JUNIOR SURGERY STUDENT CASE SUMMARY CONFERENCE PURPOSE: The purpose of the case summary conference is to provide an opportunity to improve clinical problem solving, library research, oral presentation, and writing skills. This exercise will be done in the small group seminar format. A series of case studies have been prepared. There will be a faculty facilitator at each conference. One or more students will be chosen at each conference to present and defend the case summary each has prepared for the conference. All case summaries must be given to Stephanie (room 8549, email [email protected] , or faxed to 988-1882) before the conference begins. Case summaries submitted after the start of the conference will not be accepted for a grade. BASIC INSTRUCTIONS: 1. During the course orientation, each student will receive the case histories on which each conference will be based. 2. You should review the case histories and prepare a one page written summary of your analysis of the problem posed by the case, your understanding of the pathophysiology, and your plan for management of the case. Neatness counts. Typewritten reports are preferred. If we can’t read it - we can’t grade it properly. (e.g. font of typewritten reports is too small or penmanship is poor) Please make sure you limit your summary to one page, including references. Failure to do so will result in deducted points. 3. You are expected to read, utilize, and accurately cite at least three references from the literature (not the internet or a textbook) dealing with 3 different aspects of the topic, at least one and preferably two, from surgical journals. You should know how to look up journal articles and how to document their citations accurately, something you will have to do as part of your education, residency and career. Do not quote statements from the articles in the text of your paper. That process dilutes your learning how to utilize information and write it for others to read. In addition, avoid initials or other language shortcuts to learn to make the document readable. 4. Grades for each summary will be based on the following: • Organization 25% • Content 50% • Clarity, Grammar & Style 15% • References 10% 5. There will be an emphasis on complete and compassionate care plans which focus on the best interest of the patient. Cost effective case will also be stressed. 6. Dr. Jaffe expects you, the student, to read, utilize, and accurately cite at least three references from the literature (not the internet or a textbook) dealing with 3 different aspects of the topic, at least one and preferably two, from surgical journals. He wants you to know how to look up journal articles and how to document their citations accurately, something you will have to do as part of your education, residency and career. In addition, Dr. Jaffe does not want you to quote statements from the articles in the text of your paper. That process dilutes your learning how to utilize information and write it for others to read. In addition, he requests that you avoid initials or other language shortcuts to learn to make the document readable. GRADE: Your grade will be derived from all six case summaries. The composite grade will count as 5% of your clerkship grade. 17 Dr. Emad Kandil Thyroid Mass A 32-year-old man is seen with a 1.5-cm firm nodule in the left lobe of the thyroid gland. The remaining gland is normal to examination. His only relevant past history is that he received radiation therapy for Hodgkin’s disease involving the mediastinum. 1. What is the differential diagnosis? 2. How can you reach a definitive diagnosis in an efficient and cost-effective manner? 3. Which thyroid function studies would be useful? 4. Which radiologic studies would be needed prior to planning therapy? 5. If the diagnosis was follicular carcinoma, what are the options for operative therapy, and what would you do? 6. What postoperative complications are specific to this procedure? 7. What specialized follow up would be in order? 18 Dr. Bernard Jaffe PANCREATITIS A 45 year old obese female with a history of multiple episodes of identical right upper quadrant pain is admitted with epigastric pain and tenderness. Her lipase is 750 and her amylase is 3,200. a.) What is the likely diagnosis? b.) What are some other possible causes of her disease? c.) How should you determine if she has a common duct stone? Does it change the treatment if there is one? d.) What are Ranson’s criteria at 48 hours for severe disease? e.) What are the common complications of this disease and what should you do to try to prevent them? f.) What are the indications (if any) for antibiotics? g.) What are the indications for cholecystectomy, and when should it be performed? h.) If she develops a pseudocyst, what options are there for drainage? Which would you choose and why? When should it be performed? 19 Dr. James Brown INTESTINAL OBSTRUCTION SMALL BOWEL OBSTRUCTION (SBO) A 53 y/o female presents to the ER with the acute onset of abdominal pain, nausea, vomiting, and moderate abdominal distention for the last 18 hours. The ER doctor has ordered some studies, suspects a SBO and consults you for further diagnosis and therapy. 1. List 5 other diagnoses (pertinent and common) you would consider besides the SBO. 2. List three of the most important questions you would ask about the present illness and why. 3. IF patient has SBO (complete-simple), list three most common physical findings that would be compatible with your diagnosis. 4. Why are the CBC and BMP important in this patient? 5. Name the three most common causes of SBO. 6. List the only two radiographic studies you need and why----in their order of complexity and expense. 7. Assuming adhesions are the etiology, outline a plan of treatment for: A. Partial SBO B. Complete simple SBO C. Complete gangrenous SBO SUGGESTIONS FOR CASE SUMMARY ON INTESTINAL OBSTRUCTION 1. Always precede your answers with the question typed appropriately. 2. Clarity, grammar and style do make a difference in the grade. Avoid errors due to carelessness. 3. Please read the questions carefully. (Hint: Know the difference between a physical finding and a symptom.) 20 Dr. Eugene Kukuy Lung Cancer 72 y/o Caucasian female complained of recent onset of shortness of breath. Chest X-ray revealed right lower lobe pneumonia. Her work-up included bronchoscopy which revealed an endobronchial lesion in the middle lobe bronchus. Biopsy was taken. 1) What is the differential diagnosis? What is most likely? 2) What other historical information would be pertinent? 3) What physical findings would support the diagnosis? 4) What further work-up is needed? 5) What surgical intervention is needed? 6) What would preclude surgical intervention? Surgical resection? 7) What would be the expected outcome? 8) What complications might occur if surgery is performed? 21 Dr. James Korndorffer Reflux Esophagitis 1. What are the typical symptoms of GERD? Atypical Symptoms? 2. What workup is needed to evaluate for GERD? 3. Assuming the diagnosis is uncomplicated GERD, what are the appropriate management options? What would you tell your patient about those options? 4. What operative interventions are performed for GERD? Why is one selected over the other? 5. What are the success rates for operative intervention? 7. If Barrett's esophagitis is documented on workup, how does it alter your management? 22 Dr. Bernard Jaffe Colon CA A 26-year old woman notices bright red blood on her stool. She is totally asymptomatic. 1. What is the differential diagnosis in descending order of frequency? 2. How should she be worked-‐up? 3. If a flexible sigmoidoscopy reveals an irregular mass 11cm from the anal verge, how should the patient be evaluated? 4. What are the expected routs of local spread and of metastasis and how can they best be assessed? 5. What operation should be performed and what are the goals of the procedure? 6. At operation, invasion of the vagina and base of the bladder are noted. How should these areas be dealt with? 7. If her CEA level rises from 2.0 immediately postoperatively to 87 three years later, what should be done? 23 GENERAL SURGERY DESCRIPTION: The General Surgery rotation is primarily an inpatient-based experience designed to familiarize the student with acute and elective surgical decision making processes (see Goals & Objectives) However, to the extent that much of the preoperative and postoperative management is now carried out in the outpatient setting, students will as well be expected to participate in this phase of care. A team of surgery house officers and at least one attending surgeon-preceptor will staff each General Surgery service, on which medical students will rotate. These personnel will provide ample opportunities for “on the job” experience relative to the discipline of Medicine in general and surgery in particular. In accordance with the ACGME requirements, you may not be in the hospital more than 80 hours per week and you are required to have at least one day off each week. You will have a mandatory presentation weekly. This presentation will be a 15 minute oral presentation, backed-up by a 1 page paper, given to the faculty or resident of your service while you are on your general surgery month. Your chief resident will discuss what, where and when in regards to this weekly presentation. If your resident does not, please let me know. Again this should be weekly while you are on your general month. IN-HOUSE CALL: All students will be expected and required to take in-house call on your service’s team. If there are two students on the service, you may alternate call but there should be a student with the intern on call at all times. The students’ call room is at Deming. HOSPITAL SITES: University Trauma (Drs. Meade/Schroll: Office: Nakisha Farria – 988-5111) - In-house call will be expected on those days on which the Tulane Faculty has primary call (approximately every 4th night). You are to maintain the same on-call hours as your house officer. Please note that in keeping with the ACGME 80-hour work week, when you do take Inhouse overnight call, you may only work an additional 6 hours after that call ends; but note, you will be expected to make rounds after in-house call nights to sign patients off to the next service. The Call Rooms are located on the 1st floor next to the resident nourishment room. When entering the call room pod, you turn left then make 2 rights, and it’s the 3rd door on the right. The first door has a sign that says "Surgery Senior Resident aka Boss". The 2nd door is the intern's room, and the 3rd door is the student room. The keycard is stored in the TICU on the whiteboard tray, though the call room's door is usually taped open anyway. The notes on your patients will be expected to be complete by 6:30 AM. Please contact your resident the evening before; as they might not be able to return your call the minute you are ready to begin that service. Tulane ID’s are not compatible with the access control system at University. Tulane students who are assigned to MCL/University need to go to the medical staff office. The medical staff office will make arrangements for you to be issued a MCL/University affiliate badge which will grant you access to the approved areas. The medical staff office is Room 313 in the Butterworth Building at 1541 Tulane Ave. For questions, send mail to:[email protected]. 24 You are scheduled for a medical student rotation at Ochsner Medical Center, New Orleans. Each student will be assigned to one of the several surgical services for a four week rotation. Please read important information below (students will receive an email from Stacey Porter prior to the start of the rotation): Ochsner Hospital: Students on Surgery Rotations: You must watch the video on "Orientation to the OR" prior to attending scrub class. Please print pages 4 and 5 of the Scrub Class Documents and bring with you to your scrub class. You must have these documents in order to attend scrub class. Reporting Information: Upon arrival, ALL surgery students must first report to Melissa Johnson, at 8:30 AM located at Ochsner Academic Center, UGME receptionist, 1514 Jefferson Hwy. Please bring $10.00 CASH, as a refundable deposit for your temporary Ochsner ID badges. EMR Access: You will receive an individual email from us with the training instructions for access to Epic. Training must be completed by all students prior to access being granted. Parking: All students are required to park in the Coolidge parking lot in Section B, located behind the pediatrics and breast center buildings, across the street from the hospital. You may take the shuttle to the south side of campus EXPECTATIONS: The expectations for students on their general surgery rotation are to see patients in clinic, scrub in the operating room, and follow patients in the hospital. Students will be directed in these activities by the residents and staff on their services. Students are expected to read on surgical problems they are involved with or are likely to encounter. In addition, students are to go to all lectures for general surgery residents. There is no call but students will stay through the end of the work day and be involved with rounds on Saturday. Students will not come in to work on Sundays. Students will be relieved of any work at Ochsner to go to anything required at Tulane. During each of your rotations, you will be given ample opportunity to work with your surgery team in the inpatient and outpatient environments. You are expected to become an integral part of the service to which you are assigned. All student rounds must be completed prior to making rounds with the residents. This will necessitate early arrival at the hospital so that all patients can be evaluated prior to making rounds with the residents and staff. There will be no inhouse call, but you should remain with your team until the clinical and educational responsibilities have been completed for the day. In order to be sure that students have the opportunity to monitor surgical patients’ progress, rounds will be required to be made every day, including Saturdays. Students will be given Sunday off to comply with the 24-hour off rule. Students are REQUIRED to attend all Friday educational conferences (see page14). Dr. Corsetti will complete an exit interview prior to the end of the rotation. The purpose of this is to discuss the student’s evaluation of their performance during this rotation, and to allow the student the opportunity to discuss the quality of their educational experience at Ochsner. Dr. Corsetti may, depending on the demands on his time, not be able to complete an exit interview with each student individually (this will continue to be monitored). 25 Tulane Medical Center/Lakeside/Childrens: TMC Acute Care: Dr. James Brown (583-6459 [email protected]); Dr. Peter Meade (988-5111 [email protected]) and Dr. Rebecca Schroll (988-5111 [email protected] TMC CT Vascular: Dr. Sam 988-2093 [email protected] TMC Elective: Kandil/Korndorffer/Slakey Dr. Kandil 988-7520 [email protected]); Dr. Korndorffer 988-7123 [email protected]; Dr. Slakey 988-2317 [email protected]; Lakeside General: Transplant: Dr. Stephen Jones (988-2305 [email protected]) Melanie Jeansonne, Clinic Nurse, 988-8169 or 988-8100; [email protected] Dr. Joe Buell is the Interim Director of Abdominal Transplant (988-7867 [email protected] ) but you will additionally work with Drs. Mary Killackey, Anil Paramesh , (988-0783). TRANSPLANT SURGERY CURRICULUM— Meet the 2nd and 4th Thursday of each month from 7:45-8:30 (before clinic) in the clinic side of the hospital- Rm # TBD. The curriculum will be based on the modules set forth by the American Society of Transplant Surgeons. Students rotating on TMC Hepatobiliary, meeting with all the residents and students at the beginning of the rotation to discuss expectations. Student notes will NOT be included in the patient’s chart. Therefore it will be mandatory that you write 3 H & P’s and 6 progress notes, give to the faculty you are working with and those will be graded and placed in your file. Students pick up new patients and present them on rounds. They also have to continue to present their patients daily while they are inpatient, which is used as their H&P and progress notes used for evaluation. Additionally, there is no in-house call for students on this TMC Hepatobiliary Service. There are clinics and other conferences that you will be expected to attend as are the residents. Transplant office has a bibliography of core reading materials for you. Students should look to the senior resident on the service for direction. 26 Childrens Pediatric Surgery: Dr. David Yu ([email protected]) The students assigned to this service will assist in the care of those patients under the care of the General Surgery Service. House officers will provide resident coverage for this service. Your duties are to include, but are not limited to: 1. 2. 3. 4. 5. 6. Provide daily inpatient care for the patients to whom you are assigned. Perform histories and physical examinations. Participate in the operations being performed on your patients. Work with attending physicians in their outpatient clinics (3rd floor of professional office building) Attend all Friday morning Educational conferences. Be available for home call up to every third night and every other weekend. EXPECTATION: The expectations for students on their general surgery rotation are to see patients in clinic, scrub in the operating room, and follow patients in the hospital. Students will be directed in these activities by the residents and staff on their services. Students are expected to read on surgical problems they are involved with or are likely to encounter. In addition, students are to go to all lectures for general surgery residents. There is no call but students will stay through the end of the work day and be involved with rounds on Saturday. Expectations: Make rounds with the resident on the service every AM. Examine the patients, review the labs, come to decisions, and make recommendations consistent with resident and staff. Naturally, implementations of recommendations depend on resident and staff. Do complete history and physicals on new patients admitted to the service and turn them in to the attending for review. See consults to the service and do history and physicals, review labs, make recommendations consistent with resident and staff recommendations. Make rounds with staff daily and present patients to staff in a manner consistent with working rounds. Much teaching will be done on these rounds. Therefore, students are expected to have read about the diseases present in their patients. Students are expected to attend surgery on all of their patients. There must be a good reason to be absent from the surgical procedure on their patients. Students are expected to attend clinics at Lakeside and do complete histories and physicals on the new consults and referrals and discuss diagnoses and recommendations with the staff attending. Students are expected to take call at night for emergency admits and emergency surgery. Students are expected to learn basic surgical procedures well enough to assist in surgery. Students are encouraged to attend surgical procedures done on patients other than their own if it does not conflict with primary responsibilities. Students are encouraged to make week-end rounds on their hospitalized patients. 27 TMC VA Drs. James Korndorffer Students must enroll in the VA Talent Management System (MSE-TMS) 1. 2. 3. 4. Contact Ms. Paulette Hammond at the VA to explain that you are a medical student who will be rotating to the VA and that you need for her to contact the fingerprinting office to authorize them to process you for the surgery service line (504-4123700 Extension 7572 and [email protected]. Ms. Paulette Hammond is the point of contact for the PM&R division, which is under the surgery service line at the VA. She will interface with the fingerprinting office so that they will expect your phone call for scheduling the fingerprinting session. Please print the signature packet, which is the Word file, and complete. Again, these are mainly signature pages acknowledging review of policies. Go to this link and complete the training: https://www.tms.va.gov/plateau/user/SelfRegistrationUserSelection.do. This should not be time consuming. Once done, you can print a completion certificate. Please print the VAfingerprints file and complete. Then, call the fingerprinting office at the number listed on top of the page (504-558-1408) to schedule your fingerprinting. This process must be completed quite early, as it is a limiting factor. Once you schedule a time to get fingerprinted, the time required from you will be minimal. The fingerprinting office is located on the first floor of 1555 Poydras Street, behind the credit union in the lobby. Enter the credit union, inform them that you are going to be new to the VA, and that you need fingerprinting completed. Colorectal Surgery/East Jefferson: Drs. Jeffrey F. Griffin; Mayfield; Filinsky; McCarthy Ms. Toni Marques, Office Manager 4224 Houma Blvd, Suite 540, Metairie, LA 70006 504.456-5108 [email protected] [email protected] Students must complete the East Jefferson General Hospital medical student registration form prior to the start of the rotation. Please contact Stephanie Reed, surgery student coordinator for this information if not received. General Surgery/Oncologic West Jefferson/Ochsner WB: Dr. Emery Minnard; Deanna Miller, RN Crescent Surgical Group 1111 Medical Center Blvd. Marrero, LA 70072 504.349-6556 [email protected] The medical students report on their first day to West Jefferson Medical Center at 8:00 AM, located at 1101 Medical Center Blvd. Marrero, LA 70072. You will check-in at the GME/Medical Staff Office on the 1st floor to the office of Jana Burst, Graduate Medical Education Coordinator (504.349-1897) to get your hospital badges, orientation binder, and access codes. 28 OLOL We have 2 different rotations based out of Our Lady of the Lake in Baton Rouge; listed below in red. Each rotation will rotate at different hospital sites and each site has its own packet of paperwork (as depicted below). Please see Janice Lucas in Dr. Krane’s office, when the schedule comes out to complete these packets. The earlier the packets are completed and returned, the more assurance you will have that your experience on the rotation will run smoothly. Rotation Name OLOL BR General/HIPAA Compliant Lake Surgery Center Women’s Dr. Schwartzberg/Froelich Yes Yes/Yes Yes Yes (OLOL 1) Dr. Whitaker Yes No/No No Yes (OLOL 2) Dr. Glen Schwartzberg, James Froelich and Dr. Bonner)-Baton Rouge Clinic (Julia): [email protected]; [email protected]. Office: (225) 769-4044; cell: (225) 247-8354 Contact BR Clinic Administrator Mr. Ed Silvey (225) 246-9301 to assure that your HIPAA training at Tulane is sufficient). PA: Denise Roblet; Office Manager: Amanda (225) 246-4572 The Surgeons Group of Baton Rouge Dr. Mark Hausmann, MD, FACS – General Surgery, Bariatric Surgery John Whitaker, MD [email protected] Karl LeBlanc, MD Keith Rhynes, MD Kenny Kleinpeter, MD Brent Allain, MD 7777 Hennessy Blvd., Suite 612 Baton Rouge, LA 70808 Office #: (225) 769-5656; CELL: (225) 229-9094 FAX #: (225)766-6996 Floyd J. Roberts, Jr., M.D., FACP, FCCP, Chief Medical Officer, Medical Director of Graduate Medical Education & DIO of Baton Rouge General Medical Center (225) 387-7121. Jayne B. Bacot, RN @ Lake Surgical @ 225-765-3133. John Clifford, MD, FACS, Medical Director Graduate Medical Education and DIO of OLOLRMC @ 225-765-1955. Contacts: Ashlyn Comeaux, GME Services Coordinator Our Lady of the Lake Regional Medical Center Division of Academic Affairs/Graduate Medical Education Department 7556Hennessy Boulevard, | Baton Rouge | LA 70808 225-765-7730 (office) [email protected] Lisa Loustalot| GME Services Coordinator Our Lady of the Lake Regional Medical Center Division of Academic Affairs/Graduate Medical Education Department 7556Hennessy Boulevard, | Baton Rouge | LA 70808 225-765-8769 (office) [email protected] Laura Beauregard | Administrative Assistant, Mental Health Our Lady of the Lake Regional Medical Center 5000 Hennessy Boulevard | Baton Rouge, LA 70808 (225) 765-6309 | www.ololrmc.com Baton Rouge General Medical Center (BRG) Roberta Cartaginese, LEAD Senior Program Coordinator Tulane University School of Medicine 225-387-773; 225-387-7872 (Fax) : [email protected] or [email protected] Connie Rome, GME Manager; [email protected] Chelsea Lemelle, Medical Education Coordinator, Baton Rouge General Medical Center, Office of Medical Education Office; 225.381-6194 Fax: 225.387-7872 [email protected] 29 Department of Surgery Hutchinson Building, 8th Floor SL 22 (504) 988-3909 (504) 988-1882 fax DESCRIPTION: The General Surgery rotation is primarily an inpatient-based experience designed to familiarize the student with acute and elective surgical decision making processes (see Goals & Objectives) However, to the extent that much of the preoperative and postoperative management is now carried out in the outpatient setting, students will as well be expected to participate in this phase of care. A team of surgery house officers and at least one attending surgeon-preceptor will staff each General Surgery service, on which medical students will rotate. These personnel will provide ample opportunities for “on the job” experience relative to the discipline of Medicine in general and surgery in particular. During the course of the General Surgery rotation, you are to keep a concise log of all patients for whom you were given primarily responsibility. Specific data to be recorded are: primary diagnosis, whether management occurred on an inpatient or outpatient basis, operation (if any), and complications. HOSPITAL SITES: University, Ochsner Medical Center, Ochsner St. Anne General Hospital, Tulane Medical Center, Tulane/Lakeside, East Jefferson General Hospital, West Jeff Medical Center, Our Lady of the Lake Regional Medical Center (OLOL) and Thibodaux Regional Medical Center . GOALS Patient Care: 1. Insert Nasogastric tube. 2. Insert Foley Catheter. 3. Be able to perform as a second assistant in the operating room. 4. Be able to function as a first assistant for minor or bedside procedures. 5. Demonstrate sterile technique. 6. Demonstrate patient prep in operating room. 7. Perform wound or incision closure. 8. Describe the steps and indications for central line insertion. Medical Knowledge: 1. Perform a complete history and physical exam. 2. Write appropriate patient admission orders for a variety of surgical conditions including but not limited to: trauma, GI bleeding, vascular conditions, and acute abdomen. 3. Write appropriate post-operative orders for both out-patient and emergency surgery patients. 4. Assess and discuss management of post-operative fever. 5. Explain and interpret chest x-rays. 6. Discuss patient CT scans. 7. Discuss diagnosis and management of: a. Surgical Infections b. Acute Pancreatitis c. Hemorrhagic Shock d. Cholecystitis e. Nutrition f. Abdominal Trauma g. Appendicitis h. Diverticulitis i. Thoracic Trauma j. Peripheral Vascular Disease k. Peptic Ulcer Disease 30 8. 9. 10. 11. 12. 13. 14. 15. l. Inguinal Hernia m. Carotid Disease n. Upper Gastrointestinal Bleeding o. Postoperative Complications p. Reflux Esophagitis q. Fistula-in-Ano r. Portal Hypertension s. Breast Cancer t. Adrenal Mass u. Thyroid Nodule v. Obstructive Jaundice w. Colon Cancer x. Splenectomy for Disease y. Intestinal Obstruction z. Lung Cancer aa. Melanoma Interpret arterial blood gases. Understand and verbalize indications for mechanical ventilation. Discuss the differences and uses for various forms of mechanical ventilation. Appraise patient for post-operative complications: infections, anastomotic leak, hernia, bleeding, DVT, heart attack, hyperglycemia. Discuss management and give examples of post-operative pain control. Recognize symptoms, causes, and treatments of common electrolyte derangements in surgical patients: a. Hyponatremia / Hypernatremia b. Hypokalemia / Hyperkalemia c. Hypocalemia d. Hypomagnesemia Demonstrate and discuss management of anemia. Calculate daily caloric needs of different types of patients. Calculate and write TPN orders for a variety of patient conditions. Practice Based Learning and Improvement: 1. Evaluate patient care through personal assessment and feedback from residents and staff. 2. Develop personal process of acquiring and appraising scientific knowledge. Interpersonal and Communication Skills: 1. Discuss patient condition and assessment with resident team. 2. Present patient to staff during rounds in clear concise manner, including exam, assessment of condition, and plan of patient care. 3. Document steps in patient care. 4. Participate in development of patient care plan. Professionalism: 1. Perform patient care in an ethical manner. 2. Attend conferences, clinics, and rounds on time. 3. Display commitment to patient care and educational process. 4. Respect patient culture, privacy, and disease process. System Based Practice: 1. Define cost-effective patient care. 2. Understand the basic costs and risk-benefit of common lab tests, radiology exams, and operative interventions. 31 POST-OPERATIVE ORDERS 1. Location of admission (recovery room, one day surgery, ICU, etc.) 2. Status post (surgical procedure) 3. Admitting physician 4. Condition 5. Vital signs (per recovery room protocol, then on ward, ICU, etc.) 6. Diet 7. Activity (up with assistance, bathroon privileges, etc.) 8. Allergies 9. Intravenous fluids 10. Medications 11. Nursing care orders (dressing care, wound care, assistant with ambulation, etc.) 12. Care of drains, lines 13. Intake and output; record patient weight daily 14. Special nursing care orders 15. Monitoring device instructions 16. Miscellaneous (anything else necessary for good patient care, such as notifying the physician if the patient is unable to void post-operatively, etc.) 17. Laboratory tests 18. Roentgenographic studies 19. EKG 32 SURGERY THIRD YEAR MEDICAL STUDENT MID-BLOCK EVALUATION TWO WEEKS INTO EACH OF YOUR GENERAL SURGERY SERVICE, I WILL SEND OUT ELECTRONICALLY YOUR MID BLOCKEVALUATION. BUT IT IS APPROPRIATE, AT THE APPROPRIATE DOWN TIME, TO ASK YOU’RE RESIDENT TO COMPLETE THIS EVALUATION, REVIEW WITH YOU AND RETURN TO MY OFFICE FOR YOUR FILE. PLEASE IF YOU DO NOT GET YOUR MIDBLOCK EVALUATION INTO YOUR THIRD WEEK OF YOUR GENERAL MONTH, CONTACT STEPHANIE REED IMMEDIATELY AND DR. MEADE WILL CONTACT YOUR TEAM AND REVIEW YOUR MID BLOCK PERFORMANCE WITH YOU. Date of Evaluation: _______, 2013 Evaluator: Dr. Student Name: Block #___2013-2014 Surgery Service: Faculty evaluation summary: _____________________________________________ ______________________________________________________________________ ______________________________________________________________________ ______________________________________________________________________ Resident evaluation summary: _____________________________________________ ______________________________________________________________________ ______________________________________________________________________ ______________________________________________________________________ Surgery (common procedure log) review: ____________________________________ _____________________________________________________________________ ______________________________________________________________________ ______________________________________________________________________ Professionalism: ________________________________________________________ ______________________________________________________________________ ______________________________________________________________________ ______________________________________________________________________ Student Response: _______________________________________________________ ______________________________________________________________________ ______________________________________________________________________ ______________________________________________________________________ Faculty signature: _______________________________________________________ Student signature: _______________________________________________________ Program Director’s Response: _____________________________________________ ______________________________________________________________________ Program Director’s Signature: _____________________________________________ FAX: Stephanie Reed at 504-988-1882 33 Student Evaluation Form Attachment 4 Instructions: Rate the student’s performance using the criteria listed below. Please provide written comments as well, as they may be used to compute an overall grade. Professionalism No Opportunity to Observe Frequently irresponsible, unreliable, or late. Appearance fails to reflect a professional image. Discourteous and resists feedback. Insufficiently motivated to acquire knowledge. Shows little improvement over the clerkship. Shows little initiative and refuses leadership roles. Unwilling to work as part of a team. 0 1 2 Below average attendance or reliability. Appearance does not typically reflect a professional image. Does not readily acknowledge mistakes/ tends to resist suggestions for improvement. Below average initiative and avoids leadership roles. Below average ability to work as a team player. 3 4 Usually responsible and can be counted on to follow through on tasks. Dresses appropriately for the work environment. Generally respectful of the feelings of others. Recognizes mistakes and accepts responsibility for actions. Exhibits initiative at times and accepts leadership role when asked. Usually able to handle stress and work as part of a team. 5 6 Good attendance and reliability. Sincere, honest, represents self and others accurately. Well-‐groomed and dressed appropriately for the work environment. Acknowledges mistakes and accepts responsibility for actions. Sometimes seeks leadership. Adapts well to different situations. Works effectively as part of a team. 7 Patient Care Always self-‐motivated, punctual, and reliable. Maintains professional appearance. Honest, trustworthy, and courteous. Actively seeks feedback and works diligently to correct deficiencies. Eagerly assumes extra responsibilities. Excellent leader and team player. 8 9 10 No Opportunity to Observe History /physical exam are incomplete with major omissions noted. Does not synthesize or use knowledge in clinical situations, and decision-‐ making adversely affects the patient. Does not attend to patient comfort or consistently contributes to patient discomfort. Displays minimal cultural understanding and sensitivity. History/ physical exam are sometimes incomplete and fail to note major findings. Frequently has difficulty prioritizing clinical management issues. Demonstrates little attention to patient comfort and below average cultural understanding and sensitivity. History/physical exam are usually complete, accurate, and organized. Represents average knowledge base pertinent to disease process and patient situation. Demonstrates concern for maintaining patient comfort and displays cultural understanding and sensitivity. History/physical exam are thorough, clear, and well-‐organized. Represents above average knowledge base pertinent to disease process and patient situation. Demonstrates high regard for patient comfort and displays above average cultural understanding and sensitivity. 0 1 3 5 7 2 4 6 Medical Knowledge 8 Always performs a complete, accurate, and efficient assessment. Consistently demonstrates a solid grasp and understanding of complex issues as they relate to patient situations. Demonstrates high regard for patient comfort and displays a high level of cultural understanding and sensitivity. 9 10 No Reflects failure to Opportunity read even standard to Observe textbooks. Knowledge is limited, fragmented, or poorly applied. Needs significant remediation. 0 1 2 Reflects cursory review of standard textbooks. Below average knowledge base and application to clinical problems. 3 4 Reflects review of standard textbooks. Usually demonstrates general understanding of pathophysiology, diagnosis, and management. Can generally integrate knowledge to answer patient-‐driven questions. 5 6 Interpersonal & Communication Skills Reflects review of standard textbooks sometimes supplemented by current literature. Above average knowledge, well applied. 7 8 34 Reflects in-‐depth review of standard textbooks and current literature. Able to integrate basic knowledge into the clinical situation. Level of knowledge is far superior to peers. 9 10 No Oral presentations Opportunity are consistently ill-‐ to Observe prepared and include major omissions of relevant data. Rarely communicates effectively. Fails to treat others with respect. Focuses on self at the expense of others. Poor rapport with team and other professional staff. 0 1 2 Oral presentations are below average and do not follow standard format. Sometimes communicates effectively. Often fails to treat others with respect. Lacks focus on the needs of others and has difficulty communicating empathy. Occasional difficulty with team and professional staff. Oral presentations are thorough and efficient but may contain extraneous or irrelevant information. Communicates effectively and usually treats others with respect. Focuses on the needs of others but has some difficulty communicating empathy. Good rapport with team and other professional staff. 3 5 4 6 Oral presentations are accurate, well-‐ organized, and concise. Communicates effectively even in difficult or new situations. Treats others with respect. Focuses on the needs of others and communicates empathy. Very good rapport with team and other professional staff. 7 8 Oral presentations are consistently accurate, well-‐ organized, and concise. Consistently communicates effectively, even in difficult or new situations. Consistently treats others with the utmost respect. Consistently focuses on the needs of others and communicates empathy effectively. Demonstrates excellent rapport with team and other professional staff. Above average intellectual curiosity. Seeks new information and strives to enhance understanding and development. Accepts feedback willingly and uses it to improve. Exceptional intellectual curiosity. Always seeking more information and asking insightful questions. Analyzes medical literature and incorporates it into patient plan. Consistently seeks and uses feedback to improve. 9 10 9 10 Practice-‐Based Learning & Improvement No Poor intellectual Opportunity curiosity. Does not to Observe seek new information and appears uninterested in learning. Consistently resistant and defensive to feedback. 0 1 2 Below average intellectual curiosity. Rarely seeks new information and resists learning with others. Generally resistant or defensive to feedback. 3 4 Average intellectual curiosity. Puts forth effort to enhance understanding and development. Seeks new information and learns from others. Responds well to feedback. 5 6 7 8 Systems-‐Based Practice No Opportunity to Observe Unable to formulate cost-‐conscious treatment plan. Fails to demonstrate understanding of the psychosocial and healthcare needs of patients. Fails to engage patient and family in care plan. Fails to coordinate patient care with other health care professionals. Does not typically consider cost when reviewing treatment options. Below average understanding of the psychosocial and healthcare needs of patients. Generally does not engage patient and family in care plan and does not usually coordinate care with other health care professionals. Considers cost-‐ conscious treatment options with assistance. Average understanding of the psychosocial and healthcare needs of patients. Engages patient and family when prompted, and is generally able to coordinate patient care with other health care professionals. 0 1 3 5 2 4 6 Usually considers cost in planning. Above average understanding of the psychosocial and healthcare needs of patients. Easily answers patient and family questions about care and is able to work with other healthcare professionals in coordinating patient care. 7 8 Consistently demonstrates the ability to formulate a treatment plan with appreciation for cost. Exceptional understanding of the psychosocial and healthcare needs of patients. Volunteers appropriate information to patient and family. Consistently and effectively coordinates patient care with other health care professionals. 9 10 RIME – How would you rank this student using the RIME framework? OBSERVER: Present, but contributes minimally to patient care. REPORTER: Reliably, respectfully, and honestly gathers information from patients. Communicates with faculty. Gets the basic work done. Can answer the “what” questions. INTERPRETER: Shows selectivity, prioritization, and implies analysis. Actively involved in thinking through patient problems, and of acquiring knowledge to offer a reasonable differential diagnosis. Can answer the “why” questions. MANAGER: Clinical planning fulfills a promise of working with patients on diagnostic and therapeutic decisions and a promise of developing expertise to do so. Consistently answers “how” to resolve problems. This is the level of a competent intern. EDUCATOR: Personal planning and reflection fulfill a commitment to deeper expertise for self and colleagues and patients. Is committed to self-‐ correction and self-‐improvement. This is resident level and few students will meet these criteria. 35 Observer 1 Reporter 2 3 Interpreter 4 5 Manager 6 7 Educator 8 9 10 Overall Performance/Competence: How would you rank this student compared to all students you have trained? Bottom 10% of students I have trained 1 2 Bottom 33% of students I have trained 3 4 Middle 33% of students I have trained 5 6 Please enter an overall numerical grade (Question 9 of 10 – Mandatory) Honors – 90 -‐100; High Pass – 87-‐89; Pass 80-‐86; Condition 65-‐79; Fail <65 36 Top 33% of students I have trained 7 8 Top 10% of students I have trained 9 10 TABLE OF CONTENTS FOR ORAL EXAM You will be questioned on 1 topic from each of the 3 categories below (therefore 3 total questions). All test questions can be found in the Sabiston & Schwartz textbook. ACUTE 1. 2. 3. 4. 5. 6. 7. 8. 9. Surgical Infections Acute Pancreatitis Hemorrhagic Shock Cholecystitis Nutrition Abdominal Trauma Appendicitis Diverticulitis Thoracic Trauma GENERAL 1. 2. 3. 4. 5. 6. 7. 8. 9. Peripheral Vascular Disease (Fem Pop) Peptic Ulcer Disease Inguinal Hernia Carotid Disease Upper Gastrointestinal Bleeding Postoperative Complications Reflux Esophagitis Fistula-in-Ano Portal Hypertension ONCOLOGY 1. 2. 3. 4. 5. 6. 7. 8. 9. Breast Cancer Adrenal Mass Thyroid Nodule Obstructive Jaundice Colon Cancer Splenectomy for Disease Intestinal Obstruction Lung Cancer Melanoma 37 GRADE SHEET Student Name _____________________________ Examiner Name____________________________ Date______________________________________ ACUTE----Question #_______ Pathogenesis________________ Anatomy___________________ Diagnosis___________________ Management_________________ GENERAL-Question # ______ Pathogenesis_________________ Anatomy____________________ Diagnosis____________________ Management__________________ ONCOLOGY-Question#______ Pathogenesis___________________ Anatomy______________________ Diagnosis______________________ Management____________________ TOTAL SCORE (Maximum 300)___________ EXAM SCORE (Maximum 100)____________ Signature_______________________________ 38 The tables listed below are the cases we expect you to see while on your eight week rotation. You will be completing this on the e-value website. Log into: https://www.e-value.net/ Go to “User Menu” – then “PxDx” – then “add new”. If on same patient, you saw multiple procedures, you can add multiple listings. After entering all procedures for that one patient, click “next” and “save record” and repeat for next patient. If unable to login to E*value, send email message to [email protected] for your login and password. PRINT OUT YOUR PROCEDURE LOG AND BRING W/ YOU TO YOUR ORAL EXAM. Level I= Student observed examination or management of patient with this disorder OR participated in discussion of patient with this disorder Level II= Student examined and presented patient with this disorder to an attending physician or resident Level III=Student Observed procedure being done Level IV= Student participated in clinical skill or procedure with Patient, Standardized Patient or Simulation Lab Level V= Student Performed Clinical Skill or Procedure and was directly observed by attending physician, resident, or standardized patient Group Name / Procedure Name+/Clinical Skills/Exam +/- Breast exam (Level V) Patient's H & P (Level IV) Clinical Skills/Interpretation +/- CXR: interpret (Level II) KUB:interpret (Level II) Clinical Skills/Procedure +/- ABG/Arterial Line (Level V) CCI (Level I, II, or III) Central Line: placement (Level V) Foley Cath: placement (Level V) IV access/venipuncture (Level V) Intubation/airway management (Level V) NG tube placement (Level V) PVD (Level V) Sterile Technique (Level II) Suture (simple) Technique (Level V) Suture fascia (Level III) Trauma (Level I, II, or III) Wound Care (Level V) Surgery +/- Acute Abdomen (H&P) (Level IV) Acute Abdomen (OR) (Level III) Acute Abdomen (Post) (Level IV) Acute Abdomen (SOAP) (Level III) Biliary Tract Disease (H&P) (Level IV) Biliary Tract Disease (OR) (Level III) Biliary Tract Disease (Post) (Level IV) Biliary Tract Disease (SOAP) (Level III) Cancer Patients (H&P) (Level IV) Cancer Patients (OR) (Level III) Cancer Patients (POST) (Level IV) Cancer Patients (SOAP) (Level III) Intestinal Operations (H&P) (Level IV) 39 Intestinal Operations (OR) (Level III) Intestinal Operations (POST) (Level IV) Intestinal Operations (SOAP) (Level III) Laparoscopic Procedures (H&P) (Level IV) Laparoscopic Procedures (OR) (Level III) Laparoscopic Procedures (POST) (Level IV) Laparoscopic Procedures (SOAP) (Level III) Pre-op a patient (Level IV) 40 The O.R. is located on the 3rd floor of Tulane Medical Center. There are five main areas that you will be involved in: GOR which has 14 rooms, SDS Dept./Pre-admit (where patients go pre-operatively and post-operative), LLI/Cysto Dept., Recovery Room and SICU. The GOR is open from 6:45 a.m. – 11:30 p.m. Monday through Friday with emergent cases done after 11:00 p.m. and on weekends. Surgeries start at 7:15a.m. Monday –Friday and 7:45a.m. You are part of a surgical team whose main objective is to provide quality patient care in a safe environment for staff and patients. Certain tasks seem mundane but each of us has a significant role and responsibility to meet this purpose. Since OR’s vary, you are responsible for following policies/procedures of the hospital to which you are assigned. Your Responsibilities Come prepared with the knowledge of surgical procedure, anatomy and patient history. You will be asked to assist with positioning, prepping and possibly draping. If not, once gowned and gloved, stand on the sterile field side of the room. Scrubs: Tulane Medical Center Scrub Suit Policy and Procedure Policy: Tulane Medical Center will provide scrub suits for personnel while they are working in the following areas: Bone Marrow Transplant, all areas of the Operating Room (Anesthesia, Post Anesthesia Care Unit), Outpatient Surgery, Endoscopy and Radiology Special Procedures. Scrub Suits are not to be worn outside the Hospital/Clinic – Medical School complex. They are also not to be worn as uniforms within departments outside of invasive areas. Procedure: Scrub suits are available in jade green and are stamped “Property of Tulane Hospital”. Unauthorized removal from the facility is a violation of hospital policy. An automated scrub suit dispensing system will be used in the Operating Room. Women’s locker room Code 2719*; Men’s locker Room Code 1932*. To access scrub user and pin #: Log in E*Value; Click on the edit button Update Your User Information to retrieve assigned User and Pin numbers. Scrub Ex machine requires the zero with the user #. If you have any questions, please contact student coordinator, Stephanie Reed. Because medical students have a university-issued badge, access to the system will be via the PIN. All forms for medical school students will be coordinated through the Student Coordinators. If you are at Ochsner or OLOL, you will not use Tulane scrubs. Attending faculty, staff and medical students will have a credit of two scrub suits. Once this limit has been reached, in order to receive additional scrub suits, previously issued scrubs must be returned to the unit. Visiting physicians and vendors will be issued scrubs by the Operating Room front desk personnel. Contact for the Scrub Ex machine: Linda Levesque, RN MSN CNOR OR Clinical Systems Analyst Perioperative Services Tulane University Hospital & Clinic Office D : 504 988-2469 Mobile C : 504 256-4910 Fax F : 504 988-7681 Email E-: [email protected] 41 42 43 44
© Copyright 2026