anti-CD8 - Radboud Repository
PDF hosted at the Radboud Repository of the Radboud University
Nijmegen
The following full text is a publisher's version.
For additional information about this publication click this link.
http://hdl.handle.net/2066/25597
Please be advised that this information was generated on 2015-02-06 and may be subject to
change.
7
Depletion of CD4+ or CD8+ T-cells prevents Plasmodium
berghei induced cerebral malaria in end-stage disease
C .H E R M SE N *, T. VAN DE W IEL, E. M O M M E R S, R. S A U E R W E IN a n d W. E L I N G
U n iv e r s ity o f N ijm egen , D e p a rtm e n t of M e d ic a l M ic r o b io lo g y , P . O . B o x 9 1 0 1 , 6 5 0 0 H B N ijm e g e n , T h e N e th e r la n d s
{Received 13 March 1996; revised 23 July 1996; accepted 23 July 1996)
SUMMARY
T h e role o f T - c e lls in d e v e lo p m e n t o f e x p e rim e n ta l c e re b ra l m a la r ia w a s a n a ly s e d in C 5 7 B 1 /6 J a n d C 5 7 B l / 1 0 m i c e in f e c te d
w ith P la sm o d iu m berghei K 173 or P lasm odium berghei A N K A b y t r e a t m e n t w i t h a n t i - C D 4 o r a n t i - C D 8 m A b s . M ic e w e r e
p ro te c te d a g a in st c e re b ra l m a la ria (C M ) w h e n a n t i - C D 4 o r a n t i - C D 8 m A b s w e r e i n j e c t e d b e f o r e o r d u r i n g in f e c tio n . E v e n
in m ic e in e n d - s ta g e disease, i.e. w ith a b o d y te m p e r a t u r e b e lo w 35-5 °C , t r e a t m e n t w i t h a n t i - C D 4 o r a n t i - C D 8 a n tib o d ie s
o r th e c o m b in a tio n p ro te c te d a g a in st C M , w h e r e a s c h lo r o q u in e t r e a t m e n t w a s c o m p le te ly in e ffe c tiv e in i n h i b i t i n g f u r t h e r
d e v e lo p m e n t of th e c e re b ra l sy n d ro m e .
K e y w o rd s : P lasm odiu m berghei , c ere b ra l m a la ria , p r o te c tio n , C D 4 , C D 8 , b l o o d - b r a i n b a r r ie r .
INTRODUCTION
There are a number of rodent models available for
the study of the pathogenesis of experimental
cerebral malaria. In these studies mice (Rest, 1982;
Grau et ah 1986; Thumwood et ah 1988; Curfs et ah
1989), rats (Wright, Masemble & Bazira, 1971) and
hamsters (Rest & Wright, 1979) were used in
combination with different strains of P. berghei
parasites, e.g. ANKA (Grau et al. 1986) or K173
(Curfs et al. 1989).
In all these models an immunopathological re
action is considered to be involved in the de
velopment of the syndrome. Studies in rodent
models showed sequestration and adherence of white
blood cells to the endothelial lining of post-capillary
venules in the brains in association with development
of petechiae (Rest, 1982; Polder et ah 1992).
In the model described by Grau et ah (1986)
(P. berghei ANKA, CBA/Ca mice), CD4+ T-cells
play an important role since depletion of CD4+ T~
cells prevents, and transfer of CD4+ T-cells from
mice developing cerebral malaria enhances, devel
opment of the cerebral syndrome. In addition,
depletion of CD8+ T-cells did not prevent cerebral
malaria. In mice with Murine Acquired Immuno
deficiency Syndrome (MAIDS), which is character
ized by abnormal functioning of CD4+ T-cells the
level of protection against murine CM is significantly
increased and is related to the duration of the viral
infection and, hence, with the severity of CD4+ Tcell immunodeficiency (Eckwalanga et ah 1994). In
the model using WM/Ms rats and P. berghei NK65
parasites (Imai & Kamiyama, 1994) cerebral malaria
* C o r r e s p o n d in g a u th o r. T e l : -f 31 24 3614664, F a x : + 3 1
24 3 5 4 0 216. E - m a il: r .h e r m s e n @ m m b .a z n .n l
Parasitology (1997), 114, 7-12
is prevented by CD8+ T-cell depletion, but not by
CD4+ T-cell depletion. In our model (P . berghei
K173, C57B1 mice) Curfs et al. (1989) confirmed a
role for T-cells in the development of experimental
cerebral malaria since nude mice, thymectomized
mice and mice treated with an anti-T-cell serum
were protected against cerebral malaria.
Here, we describe the results of treatment with
anti-CD4 and anti-CD8 antibodies in P. berghei
ANKA- and K173-infected C57B1 mice. The results
show that treatment with anti-CD4 or anti-CD8
antibodies can prevent development of experimental
cerebral malaria. Moreover, even when performed
shortly before expected death, i.e. in end-stage
disease when body temperature has decreased to
35*5 °C or lower, depletion of CD4 or CD8 T-cells
effectively prevented further development of the
cerebral syndrome.
MATERIALS
AND
METHODS
M ic e
C57Black/6J or C57Black/10 mice, aged 6-10 weeks,
were obtained from specific pathogen-free colonies
maintained at the Central Animal Facility of the
University of Nijmegen. All mice were housed in
plastic cages and received water and standard RMH
food (Hope Farms, Woerden, The Netherlands) a d
lib itu m .
P a r a s ite
K173 and
ANKA were maintained by
parasitized erythrocytes (PE)
naive mice. Experimental mice
P lasm odiu m berghei
Copyright © 1997 Cambridge University Press
P la sm o d iu m berghei
weekly transfer of
from infected into
were infected intra-
8
C. Hermsen orni others
Protection against cerebral malaria
Controls
100
75
50
25
0
Tx
intact
Tx
intact
Tx
intact
Fig, 1. P rotection against cerebral m alaria in thym ccto m ized (T x ) versus in ta c t m ice a n d in re la tio n to tr e a tm e n t w ith
a n ti-C D 4 o r a n ti-C D 8 m A bs 2 days before and 2 days after infection. C 57B 1/6J infected w ith P lasm odiu m berghei
K173 ( T ) o r w ith A N K A ( # ) ; C57B1/10 infected w ith P . berghei K173 ( ■ ) . T h e n u m b e r o f m ic e p ro te c te d a g a in st
C M versus the total n u m b e r of infected m ice is indicated for each ex p erim en tal g ro u p .
peritoneally with 103 PE from blood of infected
donor animals of the same strain. P. berghei A N K A
(originally obtained from Dr B. Mons, Laboratory
of Parasitology, University of Leiden, The Netherlands) is a gametocyte-producing strain which is
passaged through Anopheles gambiae mosquitoes
after 4 weekly blood passages. For this purpose
mosquitoes are allowed to feed on mice 3 days after
infection with 10 7 parasites. Blood-fed mosquitoes
received an additional bloodmeal containing normal
erythrocytes 5 days later and were allowed to infect
mice 14 days later.
Mice that show a transient hypothermia (in the
majority of cases > 3 2 °C) survive this critical period
but die in the third week or later after infection
without any noticeable cerebral pathology,
B ody temperature
Body temperature was measured w ith a digital
thermometer (Technoterm 1200) introduced into
the rectum and read after 10 sec.
Histology
Thin blood films were made from tail-blood, stained
with May-Griinwald and Giemsa’s solutions, and
the proportion of red blood cells infected with the
parasite was determined.
Mice were killed by an overdose of ether and their
brains were collected or they were collected postmortem. Brain tissue was fixed in Carnoy’s fluid for
4 h. Paraffin sections (5 ¡ivci) were stained with
PAS/Haem atoxylin or G oldner’s trichrome stain,
Sections were scored for the presence of petechiae.
Detection of cerebral malaria
In vivo C D 4 + or C D 8 + T-cell depletion
Approximately 95 % of C57B1 mice infected with 103
P. berghei K173 (Curfs et al. 1992) or P. berghei
ANK A parasites die early in the second week after
infection. Approximately 1 day before death a
progressive hypothermia develops which is strongly
correlated with development of haemorrhages in the
brains as observed by histology (Curfs et al. 1989).
Rat monoclonal anti-CD4 and an ti-C D 8 antibodies
were produced by hybridoma Y T S 191.1.2, EC ACC
no. 87072282 and Y T S 169.4.2.1, ECACC no.
87072283 respectively. Both m Abs are of the IgG 2b
isotype. Pristane-primed nude mice were injected
Lp. with 3 x 106 hybridoma cells and the ascites
produced was collected. After ammonium sulfate
Parasitaemia
Prevention of murine cerebral malaria by anti-CD4 or anti-CD8
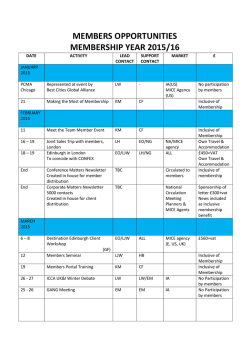
Table 1. Effect of treatment with anti-C D 4 or
a n ti-C D 8 m Abs before and during infection with
P lasm odium berghei K173 parasites on development
of cerebral malaria in C57B1 mice
T re a tm e n t/
day(s) o f
tr e a tm e n t*
C o n tr o l
Ig G 2 b -c o n tro lsJ
- 2 /2
9
A n ti-C D 4
- 2 /2
4
6
8
8 + 10
A n ti-C D 8
- 2 /2
4
6
8
8 + 10
M ic e p ro te c te d ag ain st
C M - tr e a te d m ice
n
(% )
9 /7 8 f
0 /5
1 /7
12
0
14
3 9 /4 9 1
3 /3
3 /3
7 /8
5 /5
80
100
100
88
100
3 3 /3 6 f
3 /3
2 /3
5 /8
5 /5
92
100
66
63
100
# I n re la tio n to in fe c tio n at day 0.
f S u m m a r iz e d d a ta f ro m P . berghei K 173 or P . berghei
A N K A - in f e c te d m ic e (see F ig. 1).
% I s o ty p e - m a tc h e d irre le v a n t m A b as a c o n tro l o f m A b
a n t i - C D 4 o r a n t i - C D 8 tre a tm e n t.
(45 %) precipitation and dialysis against H 20 , the
solution was freeze-dried and stored at 4 °C until
used. Aliquots were solubilized in sterile, pyrogenfree saline and used immediately. Normal and
thym ectom ized mice were treated once or twice
(4 days apart) by i.p. injection of 0*3 mg of either
an ti-C D 4 or a n ti-C D 8 mAb. Treatment with an
irrelevant isotype matched, ammonium sulfate pre
cipitated rat m Ab was used in comparison to
treatment with normal rat serum as another control.
Both control treatments did not prevent devel
opm ent of CM and did not affect parasitaemia.
Therefore, both control treatments were used in the
C D 4 +/ C D 8 + T -cell depletion experiments. T h e
efficacy of T -cell depletion was determined in
peripheral leucocytes isolated by water shock-treated
peripheral blood, or in ACT-treated spleen cell
suspensions from samples collected 3 days after
treatment with the anti-T -cell mAbs (Hudson &
Hay, 1989), Analysis of C D 4+/C D 8 + T -cell de
pletion im m ediately after injection of the m Abs was
com plicated by the presence of the injected mAb
coating the C D 4 +/C D 8 + T -cells in the cell sus
pensions, a problem that was absent when the
analysis was performed 3 days after the last anti-T cell treatment, Cell suspensions were incubated in
PBS containing 10 % FC S, 0’05 % sodium azide and
0-05 m g /m l of the anti-C D 4 or an ti-C D 8 m Abs for
30 min at 4 °C followed by a 30 min incubation of a
50 tim es diluted F IT C -labelled rabbit anti-rat Ig
9
(Dako) in PBS containing 40% m ouse serum and
0-05% sodium azide. After washing w ith PBS +
0’05 % sodium azide fluorescence was read m icro
scopically.
From the peripheral blood and the spleen respect
ively 80% and 92% of C D 4+ and 62% and 79%
of C D 8 'h T -cells were depleted. Treatm ent w ith
either anti-C D 4 or anti-C D 8 mAbs did not change
significantly the proportion of B-cells (data not
shown).
Protection against cerebral malaria was indepen
dent of i.v. or i.p. injection of the an ti-T -cell m A bs
(data not shown), and i.p. injections were used for all
experiments.
Thym ectom y
Thym ectom y (Tx) was performed on m ice anaes
thetized with chloralhydrate (4*5 % solution; 10 /¿1/g
body weight). M ice were allowed to recover from
surgery for a period of 2 weeks before they were used
in experiments.
S ta tistic a l analysis
For statistical analysis the Student’s i-test (co m
parison of 2 groups) and the Kruskal-W allis test
(comparison of more than 2 groups) were used. P
values < 0*05 were considered significant.
RESULTS
T he effect of treatment with anti-C D 4 or a n ti-C D 8
mAbs on development of experimental cerebral
malaria was analysed in thymectomized and intact
C57B1/6J and C57B1/10 mice infected with P .
berghei A N K A or P. berghei K173 parasites. Fig. 1
shows that treatment with anti-C D 4 or a n d -C D 8
mAbs protected against CM, irrespective of th y
mectom y in both C57B1/6J or C57B1/10 m ice
infected with either P . berghei K173 or P . berghei
A N K A parasites.
Parasitaemia in .control mice that died of C M was
approximately 5-10% with a reduction of the
haematocrit of approximately 20% . N either th y
mectomy, nor treatment with anti-C D 4 or a n ti-C D 8
mAbs significantly changed parasitaemia and haem
atocrit during infection as compared to controls. A ll
treated mice that did not die of cerebral malaria
developed the same severe anaemia in the course of
the infection (data not shown). T reatm ent w ith
either an isotype-matched rat mAb or normal rat
serum as a control for depletion of C D 4 + or C D 8 + T cells by specific rat mAbs had no effect on
development of CM (Table 1 ) and did not change
parasitaemia.
T he data in Table 1 show that treatment w ith antiC D 4 or anti-C D 8 mAbs 2 days before and 2 days
10
C. Hermsen and others
40
o
35
0)
«0
L_
CD
£<u
Q .
30
>
oDQ
"C
25
20
9
7
11
19
17
15
13
Days after infection
Fig. 2. The effect on body temperature of treatment with anti-CD4 or anti-CD8 mAbs 2 days before and 2 days after
Plasmodium berghei K173 infection in C57B1/6J mice. ( • ) Control mice; (O ) anti-CD4 treated mice; ( □ ) anti-CD8
treated m ice (n — 5).
Table 2 . Effect of treatment with anti-CD4 and/or anti-C D 8 m Abs or
chloroquine on development of cerebral malaria in C57B1/6J mice
infected with Plasmodium berghei K173 parasites
Infected m ice
C M p ro te c te d /to ta l
C M p ro te c te d m ic e
increased T °C -|7 to tal
T re a tm e n t*
n
(% )
n
Saline
C h lo ro q u in eJ
A n ti-C D 4
A n ti-C D 8
A n ti- C D 4 + a n ti- C D 8
2 /5 2
0 /1 0
12/17
1 0 /2 0
7 /8
4
0
71
50
88
(% )
1 /2
50
N .S .
1 1 /1 2
9 /1 0
Ip
92
90
100
* T re a tm e n t was given w hen th e b o d y te m p e ra tu re was b etw ee n 35*5 a n d 30*0 °C.
f M ice w ith a statistically significant increase o f th e ir b o d y te m p e r a tu r e a t 24 h
after treatm ent.
X C hloroquine tre a tm e n t: 0*8 m g i.p. m o u s e /d a y .
N .S ., N o survivors.
after infection protected 80 % and 92 % respectively
of the mice, whereas 1 2 % of the control mice were
protected. Moreover, T-cell depletion during in-*
fection and even when performed on day 8 , i.e.
shortly before expected death as observed in non
depleted controls, effectively prevented development
of the fatal syndrome (Table 1).
The effect on body temperature of treatment with
anti-CD4 or anti-CD 8 mAbs 2 days before and 2
days after infection with P . berghei K \ 7 2 in CS7B1/6J
mice was analysed in 8 independent experiments.
The results of 1 representative experiment are
depicted in Fig. 2. Body temperature of untreated
infected mice dramatically decreased after 9 days of
infection. A nti-C D 4 or an ti-C D 8 -treated m ice
showed a limited decrease of their body temperature
which stabilized. T he same effect on body tem
perature was found when treatment with anti-C D 4
or anti~CD 8 mAbs was given as a single treatment
up to day 8 of infection (results not shown). AntiC D 8 treatment 2 days before and 2 days after
infection prevented development of CM as effective
as C D 4+ T -cell depletion (Table 1) and no significant
difference in body temperature during infection of
the anti-CD4 and anti-C D 8 treated mice was found
(Fig. 2).
T o determine further the latest possible m om ent
for effective anti-CD4 or an ti-C D 8 treatment in the
11
Prevention of murine cerebral malaria by anti-CD4 or anti-CD8
course of infection, mice were selected with a body
temperature between 35*5 and 30 °C. If left untreated
such infected mice died within 24 h as shown in Fig.
2. The results in Table 2 show that mice with such
a hypothermia could be protected against fatal
cerebral malaria by treatment with anti-CD4 and/or
anti-CD8 antibodies, whereas chloroquine treatment
could not save any of these mice. No relation could
be found between body temperature at the moment
of anti-T-cell treatment (30—35'5 °C) and protection
against fatal cerebral malaria (data not shown). AntiCD4 or anti-CD8 treatment of mice with a body
temperature below 30 °C never prevented death.
Treatment with anti-CD4+ or anti-CD8+ mAbs in
mice with end-stage disease did not protect all mice
from the cerebral syndrome (Table 2). These last
two observations were probably due to petechiae
that already developed before treatment (Polder e t
a l. 1988).
Depletions that prevented further development of
the cerebral syndrome also resulted in a subsequent
increase in body temperature (Table 2). Overall in
93% (27/29) of the anti-T-cell treated mice body
temperature increased within 24 h and prevented
further development of the cerebral syndrome.
DISCUSSION
These studies demonstrate the importance of CD4+
and CD8+ T-cells in the pathogenesis of murine
cerebral malaria (CM), and this was independent of
the use of C57B1/6J or C57B1/10 mice, or infection
with P . b e r g h e i K173 or P. b e r g h e i ANKA parasites.
Thymectomized mice were used to prevent the
influx of new T-cells after treatment with anti-T-cell
mAbs, but no significant difference was found when
data were compared to intact mice. Treatment with
anti-T-cell mAbs did not completely eliminate all
CD4+ or all CD8+ T-cells. Together these obser
vations suggest that complete absence of CD4+ or
CD8+ T-cells is not necessary to prevent devel
opment of murine CM. Anti-CD4+ or anti-CD8+ Tcell treatment had no effect on parasitaemia and
development of anaemia confirming the observations
made by Grau e t a l. (1986) in another murine P.
b e r g h e i CM model and by Imai & Kamiyama (1994)
in a rat P. b e r g h e i NK 65 CM model.
The observation that both anti-CD4+ and antiCD8+ T-cell depletion can prevent CM is in
contrast to observations made previously by Grau et
a l. (1986), who described a role for CD4+ but not
CD8+ T-cells in development of CM in P. b e rg h e i
ANKA-infected CBA mice. In contrast, Waki e t a l.
(1992) and Imai & Kamiyama (1994) found a role
for CD8+ but not CD4+ T-cells in preventing either
early mortality or CM, respectively, in P. b e rg h e i
NK65-infected rodents. A role for both CD4+ and
CD8+ T-cells in development of CM in P. b e rg h e i
ANKA-infected mice was noted by Weidanz and
collaborators using various types of knock-out mice
(personal communication). Hancock e t a l . (1994)
found that treatment with anti-CD4 antibodies not
only depletes CD4-positive T-cells but also CD4positive mononuclear cells; however, their possible
role in CM remains to be determined.
In contrast to our results Grau e t a l . (1986) found
that CD8+ T-cell depletion did not prevent de
velopment of CM in P. b e r g h e i ANKA-infected
CBA mice. This apparent discrepancy may relate to
different mouse strains used and/or a difference in
the strain of P. b e r g h e i ANKA.
Anti-CD4 or anti-CD8 T-cell treatment was
effective even in mice with end-stage disease (body
temperature between 35*5 and 30 °C). Histological
analysis of brains of mice developing the cerebral
syndrome showed that white blood cells adhere to
the endothelial lining (Curfs e t a l. 1989; Polder e t a l .
1992) suggesting that these CD4+ and CD8+ T-cells
are involved in disturbance of the endothelial lining
and thereby in the functioning of the blood-brain
barrier.
Disturbance of the blood—brain barrier in mice
developing CM was also observed by Thumwood e t
a l, (1988) and Neill & Hunt (1992). They described
leakage of Evans blue from the vasculature into brain
parenchyma. In addition, P. b e r g h e i K173-infected
mice with end-stage disease are sensitive to de
velopment of folic acid-induced convulsions, while
control mice are not. Treatment with anti-CD4+ or
anti-CD8+ mAbs not only prevents CM but suc
cessfully treated mice also recover from their
sensitivity to folic acid-induced convulsions within
4 h after mAb treatment (C. Hermsen e t a l . 9 unpub
lished observations). In human cerebral malaria
convulsions are common (Waruiru e t a l . 1996),
raising the question as to whether in human CM
adherence of sequestered infected red blood cells and
possibly the presence of leucocytes (Polder, 1989;
Porta e t a l . 1993; Eling & Kremsner, 1994; Patnaik
e t a L 1994; Eling & Sauerwein, 1995) are involved in
excessive activation of endothelial cells and sub
sequent disturbance of the function of the bloodbrain barrier.
Chloroquine treatment could not save mice in
end-stage disease while anti-CD4 or anti-CD8
treatment was still effective. This may be explained
by the fact that chloroquine like most other antimalarial drugs needs more than 1 day to suppress
parasitaemia effectively, whereas most of the mice in
end-stage disease die within 1 day.
Our data are compatible with the hypothesis that
a localized inflammatory reaction involving both
CD4+ and CD8+ T-cells disturbs and damages the
endothelial lining of the blood-brain barrier eventu
ally leading to petechiae. Our data suggest that both
CD4+ and CD8+ T-cells are involved in stimulation
of a downstream process of the development of the
petechiae.
VJ
12
C. Hermsen and others
W e thank G. Poelen, T . van den Ing and Y. B ro m for
skilled biotechnieal assistance.
(1992). P a th o lo g y of fata l a n d
resolving P lasm odiu m berghei c e re b ra l m a la ria in m ice.
n e i l l , a. l . & h u n t , n . H.
P arasitology 105, 1 6 5 -1 7 5 .
p a t n a i k , j. k ., d a s , b . s., m i s h r a , s. k ., m o h a n t y , s .,
REFERENCES
CURFS, J. H. A. J ., SCHETTERS, T. P. M., HERMSEN, C. C.,
JERUSALEM, C. R., VAN ZON, A. A. J. C. & ELING, W. M. C.
(1989). Im m unological aspects of cerebral lesions in
m urine malaria. Clinical and E xperim ental Immunology
75, 136-140.
CURFS, J. H. A. J., HERMSEN, C. C,, MEUWISSEN, J. H. E. TH.
& e l i n g , W. M. c. (1992). Im m u n iz a tio n against
cerebral pathology in Plasm odium berghei -in fected
mice. Parasitology 105, 7-14.
ECKWALANGA, M., MARUSSIG, M., TAVARES, M. D.,
s a t p a t h y , s. k . & m o h a n t y , d . (1994). V a s c u la r
clogging, m o n o n u c le a r cell m ig ra tio n , a n d e n h a n c e d
vascular p e rm e a b ility in th e p a th o g e n e s is o f h u m a n
cereb ral m alaria. A m e ric a n J o u rn a l o f T ro p ic a l
M edicin e a n d H y g ie n e 51, 6 4 2 -6 4 7 .
p o l d e r , t . w . (1989), P h .D . D is s e r ta tio n : M o r p h o lo g y
of cereb ral m a la ria clinical a n d e x p e rim e n ta l s tu d y .
POLDER, T. W ., ELIN G , W . M ., KUBAT, K. & JERUSALEM, C. R.
(1988). H is to c h e m is tr y o f c e re b ra l lesions in m ic e
infected w ith P la sm o d iu m berghei . T ro p ica l M e d ic in e
an d P a ra sito lo g y 39, 2 7 7 -2 8 3 .
POLDER, T.
w.,
ELIN G, W. M. C., CURFS, J. H. A. J,,
BOUANGA, J. C., HULIER, E., PAVLOVITCH, J. H.,
JERUSALEM, C. R. & W IJERS-ROUW , M . (1992).
MINOPRIO, P., PORTNOI, D., RENIA, L. & MAZIER, D.
U ltr a s tr u c tu r a l c h a n g e s in th e b l o o d - b r a i n b a r r ie r o f
m ice infected w ith P la sm o d iu m berghei, A c t a L eid en sia
60, 3 1 -4 6 .
(1994). M u rin e A I D S p ro tects m ice against
experim ental cerebral m alaria; d o w n -reg u la tio n by
interleukin 10 of a T - h e lp e r type 1 C D 4 + cell-m ed iated
pathology. Proceedings o f the N a tio n a l A c a d em y o f
Sciences , U S A 91, 8097-8101.
e l i n g , w. M. c. & k r e m s n e r , P. G. (1994). C ytokines in
m alaria, pathology and p ro tectio n . B iotherapy 7,
PORTA, J . } CAROTA, A., PIZZOLATA, G. P . , W IL D I, E.,
WIDMER, M. C ., MARGAIRRAZ, C . & GRAU, G. E. (1993),
g r a u , g . e ., p i g u e t , p. f . , e n g e r s , H. D., LOUIS, J. A.,
Im m u n o p a th o lo g ic a l c h a n g e s in h u m a n c e re b ra l
m alaria. C lin ical N eu ro p a th o lo g y 12, 1 4 2 -1 4 6 .
r e s t , j. r . (1982). C e r e b r a l m a la ria in in b r e d m ice. A
n ew m o d e l a n d its p a th o lo g y . T ransactions o f the
R o y a l S o c ie ty o f T ro p ica l M e d ic in e an d H y g ien e 76,
4 1 0 -4 1 5 .
REST, j. R. & W RIGHT, d . h . (1979). E le c tro n m ic ro s c o p y
o f cerebral m a la ria in g o ld e n h a m s te r s (M esocricetu s
auratus). J o u rn a l o f P a th o lo g y 127, 1 1 5 -1 2 0 .
VASSALLI, P. & LAMBERT, P. H. (1986). L 3 T 4 T -
THUMWOOD, C. M ., HU N T, N . H ., CLARK, I. A, & COWDEN,
211-221 .
e l i n g , w. m . c. & s a u e r w e i n , r . (1995). S evere an d
cerebral m alaria: co m m o n or d istin ct
pathophysiology ? R eview s in M ed ica l M icrobiology 6 ,
1 7 -2 5 .
lym phocytes play a m ajo r role in th e path o g en esis of
m u rin e cerebral m alaria. Journal o f Immunology 137,
2348-2354.
HANCOCK, W. W., ADAMS, D. H., WYNER, L. R., SAYEGH,
m . h . & k a r n o v s k y , M. j. (1994). C D 4 + M o n o n u c le a r
cells induce cytokine expression, vascular sm o o th
m uscle cell proliferation, and arterial occlusion after
endothelial injury. A m erican Journal of P athology 145,
1008-1014.
P ractical Im m unology .
Blackwell Scientific, L o n d o n .
H u d s o n , l . & h a y , f . (1 9 8 9 ).
Im ai, y. & k am iyam a, T. (1994), T -ly m p h o c y te d e p e n d e n t developm ent of cerebral sy m p to m s in
W M / M s rats infected w ith Plasm odium berghei.
A nnals of Tropical M edicine and P arasitology 88 ,
83-85.
w . b . (1988). B re a k d o w n o f th e b l o o d - b r a in b a r r ie r in
m u r in e c ere b ra l m a la ria . P a ra sito lo g y 96, 5 7 9 -5 8 9 .
WAKI, S., UEHARA, K ., KANBE, K., ONO, K., SUZUKI, M. &
NARIU-CHI, H. (1992). T h e role o f T - c e lls in
p a th o g e n e sis a n d p ro te c tiv e im m u n ity to m u r i n e
m alaria. Im m unology 75, 6 4 6 -6 5 1 .
WARUIRI, C. M., N EW TO N , C. R. J. C., FORSTER, D ., N EW , L.,
WINSTANLEY, R., M W ANGI, I ., MARSH, V., WINSTANLEY,
M ,, s n o w , R. w . & m a r s h , K. (1996). E p ile p tic se iz u re s
a n d m alaria in K e n y a n c h ild re n . T ransaction s o f the
R o y a l S o c ie ty o f T ro p ic a l M e d ic in e a n d H y g ie n e 90,
152-155.
WRIGHT, D, H., MASEMBE, R. M. & BAZIRA, E. R. (1971).
T h e effect of a n ti- th y m o c y te s e r u m o n g o ld e n
h a m ste rs a n d ra ts in fe c te d w ith P . berghei. B r itis h
J o u rn a l o f E x p e rim e n ta l P a th o lo g y 52, 4 6 5 -4 7 7 .
© Copyright 2026