Mutational Activation of N- and K-ras Oncogenes in Plasma
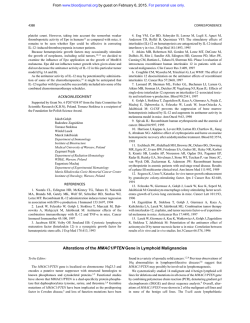
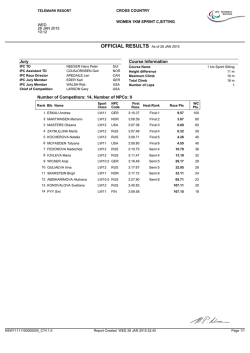
From www.bloodjournal.org by guest on February 6, 2015. For personal use only. Mutational Activation of N- and K-ras Oncogenes in Plasma Cell Dyscrasias By Paolo Corradini, Marco Ladetto, Claudia Voena, Antonio Palumbo, Giorgio Inghirami, Daniel M. Knowles, Mario Boccadoro, and Alessandro Pileri The frequency of N- and K-ras oncogene mutations was investigatedin plasma cell dyscrasias. Genomic DNAs from 1 2 8 patients were selected for this study: 30 monoclonal gammopathies of undetermined significance, 8 solitary plasmacytomas, 77 multiple myelomas (MM), and 1 3 plasma cell leukemias (PCL). A two-step experimental approach was devised. All samples were screened for mutations by single-strand conformation polymorphism analysis. DNA fragments displaying an altered electrophoretic mobility were further studied by direct sequencing to confirm and characterize the nature of the mutations. Ras mu- tations are not randomly distributed because they are detectable only in MM (9%)and PCL (30.7%). N-ras codons 12,13, and 6 1 and K-ras codon 1 2 were found to be mutated, but N-ras codon 61 mutation was the most frequent finding (63.6%). In conclusion, ras mutations were found in PCL, and in a subset of MM characterized by advancedstage disease and adverse prognostic parameters. Furthermore, based on our findings, it is possible to speculate that ras mutations represent a late molecular lesion in the process of multistep carcinogenesis. 0 1993 by The American Society of Hematology. P kemia (CML)."-15 However, among more differentiated lymphoid tumors, such as chronic lymphocytic leukemia (CLL), hairy cell leukemia (HCL), and non-Hodgkin's lymphoma (NHL), only MM was found to harbor activated rus genes.l 6 Several reasons prompted us to investigate ras oncogenes in plasma cell dyscrasias. First, the incidence of rus mutations has been reported with some dis~repancies.'.~Second, we wanted to correlate its incidence with several clinical parameters in a large panel of MM cases. Third, the presence of these mutations has never been evaluated in MGUS, SP, or PCL. Finally, because these oncogenes have been already detected in some human precancerous lesions (eg, adenomas and myelodysplasias), indicating that they participate in the early stages of tumorigenesis, we wanted to determine the temporal relationship between rus activation and the onset of an aggressive plasma cell dyscrasia. LASMA CELL DYSCRASIAS are a group of diseases characterized by the expansion of plasma cells producing monoclonal Igs. Monoclonal gammopathy of undetermined significance (MGUS), solitary plasmacytoma (SP), multiple myeloma (MM), and plasma cell leukemia (PCL) are the clinical entities forming this group. MGUS is a benign disorder even if, in a large series with 20 years of follow-up, 24.5% of patients developed MM.' SP is characterized by indolent behavior, with a median survival that can exceed 10 years, whereas MM and PCL follow an aggressive clinical course.* The pathogenesis of these diseases is still unknown, and the role of some dominantly acting proto-oncogenes, such as bcl- 1, bcl-2, c-myc, Moloney leukemia virus integration4 (MLVI-4), N-rus, K-rus, and H-rus, has been investigated only in MM.3-6So far, the molecular lesions more frequently detected in MM patients are activating point mutations involving the N- and K-rus oncogene^.'.^ The family of rus oncogenes consists of three related genes: H-, K-, and N-rus. They encode proteins of 2 1 Kd (p2 1) with GTPase activity that are located at the inner surface of the cell membrane. These oncogenes acquire their transforming potential when point mutations occur at the codons 12, 13, or 6 1, resulting in single amino acid substitution." Activated rus genes have been identified in several human cancers, including some hematologic malignancies such as acute myeloid leukemia (AML), acute lymphoblastic leukemia (ALL), myelodysplasias, and blast crisis of chronic myelogenous leu- From the Department of Medicine and Experimental Oncology, Division ofHematology, University of Torino, Torino, Italy; and the Department of Pathology, College of Physicians and Surgeons, Coliimbia University, New York, NY. Submitted November 2, 1992; accepted December 30, 1992. Supported by the Associazione Italiana Ricerca SUI Cancro (AIRC, hfiluno Italy), and by Consiglio Nazionale Ricerche (Progetto Finalizzato ACRO. N. 9202242.PF39). C. V. is a fellow of Comitato Piemontese Gigi Ghirotti. Address reprint requests to Paolo Corradini, MD, Divisione Universitaria di Ematologia, Via Genova 3, 10126 Torino, Italy. The publication costs of this article were defiayed in part by page charge payment. This article must therefore be hereby marked "advertisement" in accordance with 18 U.S.C. section I734 solely to indicate this fact. 0 1993 by The American Society ofHemuto1og.v. 0006-4971/93/81IO-O019$3.00/0 2708 MATERIALS AND METHODS Patients and nucleic acid extraction. We selected for this study 128 patients with various forms of plasma cell dyscrasias. These patients included 77 patients with MM, 13 with PCL, 30 with MGUS, and 8 with SP. All the patients were studied at diagnosis, except for 24 with MM that were in the relapse phase (Table 1). Bone marrow or tissue samples (plasmacytomas) were collected during standard diagnostic procedures. Genomic DNA was purified by proteinase K digestion, phenol/chloroform extraction, and ethanol precipitation. Oligonucleotideprimers. All the oligonucleotides used for polymerase chain reaction (PCR) amplification and direct sequencing were chemically synthesized using a 39 1 PCR-MATE EP, DNA Synthesizer (Applied Biosystems, Foster City, CA) on a 0.2 pmol/L scale, according to the users' manual. The oligonucleotide primers for Nand K-rus genes are the same as reported previously.'6Js Single-strandconformationpolymorphism (SSCP) analysis. SSCP analysiswas performed according to an adapted version of a previously published neth hod.'^.^' Briefly, 100 ng of genomic DNA was amplified in a 10 p L reaction, adding I O pmol of each primer, 0.5 U of Taq DNA polymerase (Promega, Madison, WI), I pCi of [a-32P]dCTP (specific activity, 3,000 Ci/mmol), 2.5 pmol/L dNTPs (Pharmacia LKB Biotechnology, Uppsala, Sweden), I O mmol/L Tris-HC1 (pH 8.8), 50 mmol/L KC1, I mmol/L MgC12, 0.01% gelatin, final concentration. Thirty cycles of denaturation (94"C), annealing (56°C to 60°C depending on primer melting temperature), and extension (72°C) were performed on an automated heat-block (DNA thermal cycler; MJ Research, Boston, MA), followed by a 7-minute final extension at 72'C. Two microliters of the I O pL reaction mixture was diluted I : I8 in 0.1% NaDodSO,/ I O mmol/L EDTA and further mixed 1:l with a sequencing stop solution containing 20 mmol/L NaOH. Blood, Vol81, No 10(May 15). 1993: pp2708-2713 From www.bloodjournal.org by guest on February 6, 2015. For personal use only. RAS 2709 MUTATIONS IN MULTIPLE MYELOMA PCL MM N-Ras 12/13 MM PCL N-Ras 61 Fig 1. SSCP analysis of Nand K-ras oncogene mutations in plasma cell dyscrasias. PCRamplified fragments corresponding to codons 12,13, and 6 1 were amplified from genomic DNA, denatured by heat, and run on a 6% acrylamide gel containing 10% glycerol. Representative cases of MM and PCL are shown. Samples were scored positive for mutations when bands different from the normal control (N) were detectable. Arrowheads point to bands of the mutated samples. PCL MM K-Ras 12/13 Samples were heated at 95°C for S minutes. chilled on ice for 3 minutes. and then 3 pL was loaded onto a 6% acrylamide/TBE gel containing I070 (vol/vol) glycerol. Gels were run at 8 W for 12 to IS hours at room temperature. Autoradiography films were exposed at -70°C with intensifying screens for varying periods of time. D i r m seqtccwcing sl' PCR prodrrcLs. Amplifications were performed using 100 ng of genomic DNA. 20 pmol of each primer, and 2.5 U of Taq DNA polymerase (Promega) in a SO p L final volume reaction. The number of cycles. thermocycling conditions, and reaction buffer were as described above. The PCR products were electrophoresed through a 27n low melting point (LMP) agarose (GIBCO BRL. Gaithersburg. MD). the LMP slice was melted at 68°C. and DNA was phenol extracted and ethanol precipitated. N- and K-rar. 5' and 3' primers. were labeled with [y-3'P]ATP using T4 polynucle- otide kinase (Promega). Direct sequencing reactions of both strands were performed using the Promega fmol sequencing system according to the manufacturer's instructions. The sequencing reactions were performed in a thermal cycler at 58°C annealing temperature for 9 cycles. Reaction products were run on a 6% acrylamide/urea gel. fixed in I0q0 acetic acid. and then exposed at -70°C with intensifying screens for varying periods of time. RESULTS Genomic DNAs from 128 patients with plasma cell dyscrasias were analyzed for mutations of the N- and K-rrrs on- From www.bloodjournal.org by guest on February 6, 2015. For personal use only. CORRADlNl ET AL 2710 Table 2. Table 1. Frequency of Res Oncogene Mutations in Plasma Cell Dyscrasias Diagnosis MGUS SP MM PCL Sample Positiveflested Abbreviation: SP, solitary plasmacytoma. cogenes (Table I). All DNAs extracted from these specimens were amplified using pairs of oligonucleotide primers flanking the genomic regions spanning codons 12, 13, or 6 1 of the Nrus and K-rus genes. A two-step experimental approach was devised. All samples were screened for mutations within the N-rus and K-rus genes by SSCP analysis. DNA fragments displaying an altered electrophoretic mobility by SSCP analysis (Fig 1) were subsequently reamplified and studied by direct sequencing to confirm and characterize the nature of the mutations. The SSCP Mutations in Plasma Cell Dyscrasias Diagnosis Res Gene Codon Mutation Amino Acid Substitution MM MM PCL MM MM MM MM PCL MM PCL PCL N N N N N N N N N N 12 12 13 61 61 61 61 61 61 61 12 GGT - G A T GGT -.GCT GGT - T G T CAA-CGA CAA- AAA CAA -.CAT CAA-CTA C A A - r AAA CAA CTA CAA CAT GGT CGT Gly-r Asp Gly Ala Gly-r Cys Gln- Arg Gln-r Lys Gln His Gln-r Leu Gln-Lys Gln -, Leu Gln His Gly-r Arg M22 0130 018 7/77 4/13 R8S M93 M27 M28 M9 1 M19 M89 M6 1 M90 M117 M88 K --. - - - technique can detect sequence changes affecting one or more nucleotides in a defined stretch of DNA. This method, for 150- to 200-bp fragments. has a sensitivity level of at least A dilution experiment was performed to confirm the N-Ras 61 G A T C =' G A T C G A T C ~- c G A T C -- - Gq A C ' C T 61[p I C r T 3' b ," C B Normal M28 M91 M89 G A T C G A T C G A T C G A T C i M19 M90 M61 M117 Fig 2. N-res codon 61 mutations detected by direct sequencing of PCR-amplfied fragments. Mutated samples are matched to a control DNA. Noncoding strands are shown. Arrows point to bands correspondingto mutated base pairs. From www.bloodjournal.org by guest on February 6, 2015. For personal use only. ms MUTATIONS IN MULTIPLE MYELOMA 271 1 method's sensitivity under our experimental conditions (data not shown). The results of SSCP and sequencing analysis are summarized in Table 2. The overall frequency of ras mutations among plasma cell dyscrasias is 8.6% ( 1 1 of 128). They are not randomly distributed because they are detectable only in PCL (30.7%) and MM (9%). Mutations were found in 5 of 53 (9.4%) MM cases at diagnosis and 2 of 24 (8.3%) cases at relapse. N-rus codons 12, 13, and 61 and K-rus codon 12 were found to be mutated, although N-ras codon 6 I was the most frequent finding (7 of 1 1 [63.6%]).The lack of detectable mutations in the negative case was not due to insufficient representation of tumor cells, because all the samples contained more than 5% malignant cells, whereas the threshold of sensitivity of the method is 1%. Moreover, to evaluate the presence of SSCP false-negative samples, 40 negative cases were analyzed by direct sequencing (8 PCL, 4 SP, and 28 MM), showing a 100%concordance with SSCP results. To confirm the presence and determine the nature of the mutations, the nucleotide sequence of the involved exons was determined by direct sequencing of both strands. A het- Table 3. Correlation Between RBSMutations and Prognostic Parameters in MM Patient ~ 2 2 M93 M28 M91 M19 M89 M90 Stage Albumin WL) (%I CRP (mg/L) ,92-Microglobulin (mg/L) IllA Ill5 IllA Ill5 IllA lllB IllA 29 47 31 34 25 50 34 0.5 ND 4 0.8 ND 2.7 1.2 117 ND 13 50 121.9 6 10.7 5.5 ND 7.9 41.9 13 11.5 3.8 LI Adverse prognostic factors were albumin lessthan 30 g/L, U greater than 2%. CRP greater than 6 mg/L, and i32-microglobutingreater than 6 mg/L. Abbreviations: U, labeling index; CRP, C-reactive protein; ND, not determined. erogeneous pattern of mutation was observed including C -W A, G + C, G + T, and A + T transversions, and G + A transitions (Figs 2 and 3). Purine-pyrimidine transversions were the most frequent finding (9 of I 1 [81.8%]). These N-Ras 12/13 G A T C G A T C G A T C G A T C Normal M22 M27 M93 C 3' A A c C K-Ras 12/13 G A T C G A T C Normal M88 :a 3' G A T G 13[ -- 121 b G T c 5' ," Fig 3. N- and K-res codon 12/13 mutations detected by direct sequencing of PCR-amplifiedfragments. Mutated samples are matched to a control DNA. Noncoding strands are shown for cases M22, M27, and M93; coding strand is shown for case M88. Arrows point to bands corresponding to mutated base pairs. From www.bloodjournal.org by guest on February 6, 2015. For personal use only. CORRADlNl ET AL 2712 Table 4. Clinical Parameters and Ras Mutations in MM Parameter PositiveITested’ Stage I II 111 Bone marrow plasma cells 019 0117 7/37 1/26 2/20 4/18 <30% >30% and 150% >50% Protein type 3/40 2/30 215 OJ2 IgG IgA Light chain Nonsecretory Albumin (g/L) 2/10 <30 230 5/62 Labelling index 3/50 211 1 <2% >2% Status Diagnosis RelaDse 5/53 2124 The clinical parameters were not available for all patients. changes led to the replacement of glycine (N- and K-rus codons 12 and 13) and glutamine (N-rus codon 61) residues with several different amino acids (Table 2). The relatively small percentage of rus mutations in MM did not allow a survival analysis. Rus mutations were detected only in stage 111 MM (7 of 37 [ 19%]).*’In addition, a prognostic evaluation was performed in all but 1 patient, in whom data were not available (M93). All the examined patients, except M90, had two or more concordant adverse prognostic parameters, as shown in Table 3.22-24Patients M19, M22, and M28 were already dead when the analysis was performed. The median follow-up for censored patients was 20 months (range, 17 to 46 months). Mutations were frequently detected in PCL that are characterized by an extremely high proliferative activity and a short survival. Our panel included all primary PCL except for M27 patient, who presented the leukemic transformation of an MM. The latter, together with 3 primary PCL, were found to harbor rus mutations. DISCUSSION We have investigated the mutational activation of N- and K-rus oncogenes and its correlation with clinical parameters in plasma cell dyscrasias. Recent studies have suggested that these oncogenes may play a role in myeloma pathogenesis. N- and K-rus oncogenes were found to be mutated in previous s t ~ d i e s . ~In. ~addition, the introduction of activated N-rus genes into Epstein-Barr virus (EBV)-immortalized human B lymphoblasts resulted in their malignant transformation and terminal differentiation into clonal plasma cells.25 Our study indicates that rus mutations are peculiar to aggressive forms of plasma cell dyscrasias. The relatively low incidence of mutations in MM is confirmed. whereas the high incidence in PCL represents a novel finding. It should be noted that, although the SSCP technique might slightly underestimate the frequency of mutations, our findings are in agreement with the percentage found by Paquette et al’ in a smaller panel of cases. The presence of activated rus genes appears to be characteristic of immature lymphoid neoplasms, and the discovery of rus mutations in MM and PCL apparently contradicts this finding. However, a possible explanation can derive from the studies indicating that human myeloma originates from the B- or even the pre-B-lymphocyte ~ o m p a r t m e n t . ’ ~ *The ~-~~ mechanism of occurrence of such mutations remains unknown, and the considerable proportion of different amino acid substitutions may suggest that B cells are exposed to a variety of molecular events capable of inducing many different rus mutations. However, the relatively low frequency of rus mutations in MM argues against a general pathogenetic role for this oncogene in such a disease. Moreover, the low incidence at relapse rules out the possible mutagenic effect played by chemotherapy treatment. Correlations between rus mutations and several clinical parameters were considered in MM only (Table 4),because PCL have a well-defined unfavorable clinical outcome. Our panel included 26 stage I and I1 cases, but mutations were detected only in stage 111 patients. In addition, although the small number of cases did not allow survival analysis, the presence of rus mutations was associated with adverse prognostic parameters, as shown in Table 3. These mutations identify a subset of myeloma patients characterized by an advanced stage and the simultaneous presence of adverse prognostic parameters. Plasma cell dyscrasias represent a model of multistep carcinogenesis, and they can be divided according to different tumor progression steps corresponding to defined clinical entities, ranging from the benign gammopathy to the aggressive leukemic form. In breast and colon adenomas as well as in myelodysplasias, rus genes are frequently altered, leading to the general concept that such oncogenes act early in the multistep c a r c i n o g e n e ~ i s . ~This ~ - ~role ~ appears not to apply to plasma cell dyscrasias. The absence of mutations in MGUS indicates that they cannot be considered “precancerous lesions” similar to adenomas or myelodysplasias. Moreover, the detection of such mutations only in stage 111 MM and PCL suggests that rus activation most likely plays a more important role in tumor progression rather than in tumor initiation. The high frequency of rus mutations in PCL led us to speculate that these mutations probably represent a late molecular lesion conferring additional proliferative advantage to tumor cells. However, to better define the role and timing of rus gene activation, longitudinal studies on individual patients are required. In conclusion, our work indicates that rus oncogene activation is not a general pathogenetic event for plasma cell dyscrasias, and that its presence is typical of advanced-stage MM and PCL. REFERENCES 1. Kyle RA: Diagnostic criteria of multiple myeloma. Hematol Oncol Clin North Am 6:347, 1992 From www.bloodjournal.org by guest on February 6, 2015. For personal use only. RAS MUTATIONS IN MULTIPLE MYELOMA 2. Knowling MA, Haanvood AR, Bergsagel DE: Comparison of extramedullary plasmacytomas with solitary and multiple plasma cell tumors of the bone. J Clin Oncol 1:255, 1983 3. Barlogie B, Epstein J, Selvanayagam P, Alexanian R: Plasma cell myeloma-New biological insights and advances in therapy. Blood 73:865, 1989 4. Ladanyi M, Feiner H, Niesvizky R, Michaeli J: Protoncogene analysis in multiple myeloma. Blood 78:433a, 1991 (abstr, suppl I ) 5. Palumbo AP, Boccadoro M, Battaglio S, Corradini P, Tsichlis PN, Huebner K, Pileri A, Croce CM: Human homologous of Moloney leukemia virus integration-4 locus (MLVI-4), located 20 kilobases 3’ of the c-myc gene, is rearranged in multiple myeloma. Cancer Res 50:6478, 1990 6. Selvanayagam P, Blick M, Nami F, van Tuinen P, Ledbetter DH, Alexanian R, Saunders GF, Barlogie B Alteration and abnormal expression of the c-myc oncogene in human multiple myeloma. Blood 71:30, 1988 7. Neri A, Murphy JP, Cro L, Ferrero D, Tarella C, Baldini L, Dalla-Favera R: Ras oncogene mutation in multiple myeloma. J Exp Med 170:1715, 1989 8. Paquette RL, Berenson J, Lichtenstein A, McCormick F, Koeffler HP: Oncogenes in multiple myeloma: Point mutations of N-ras. Oncogene 5: 1659, 1990 9. Tanaka K, Takechi M, Asaoku H, Dohy H, Kamada N: A high frequency of N-RAS oncogene mutations in multiple myeloma. Int J Hematol 56: I 19, 1992 IO. Barbacid M: Ras genes. Annu Rev Biochem 56:779, 1987 1 I. Jiang W, Kahn SM, Guillem JG, Lu SH, Weinstein I B Rapid detection of ras oncogenes in human tumors: Applications to colon, esophageal, and gastric cancer. Oncogene 4:923, 1989 12. Bos J L Ras oncogenes in human cancer: A review. Cancer Res 49:4682, 1989 13. Toksoz D, Farr CJ, Marshall CJ: Ras genes and acute leukemia. Br J Haematol 71:l, 1989 14. Ahuja HG, Foti A, Bar-Eli M, Cline MJ: The pattern of mutational involvement of ras genes in human hematologic malignancies determined by DNA amplification and direct sequencing. Blood 75: 1684, 1990 15. Bos JL, Verlaan-De Vries M, van der Eb J, Janssen JWG, Delwel R, Lowenberg B, Colly LP: Mutations in N-RAS predominate in acute myeloid leukemia. Blood 69:1237, 1987 16. Neri A, Knowles DM, Greco A, McCormick F, Dalla-Favera R: Analysis of ras oncogene mutations in human lymphoid malignancies. Proc Natl Acad Sci USA 85:9268, 1988 17. Maniatis T, Fntsch EF, Sambrook J: Molecular Cloning: A Laboratory Manual. Cold Spring Harbor, NY, Cold Spring Harbor Laboratory, 1989 18. Suzuki Y, Orita M, Shiraishi M, Hayashi K, Sekiya T: Detection of ras gene mutations in human lung cancers by single strand 2713 conformation polymorphism analysis of polymerase chain reaction products. Oncogene 5: 1037, 1990 19. Orita M, Suzuki Y, Sekiya T, Hayashi K Rapid and sensitive detection of point mutations and DNA polymorphism using the polymerase chain reaction. Genomics 5374, 1989 20. Hayashi K PCR-SSCP: A simple and sensitive method for detection of mutations in the genomic DNA. PCR Methods Applications 1:34, 1991 2 1. Dune BGM, Salmon S: A clinical staging system for multiple myeloma. Cancer 362342, 1975 22. Boccadoro M, Marmont F, Tribalto M, Fossati G, Redoglia V, Battaglio S, Massaia M, Gallamini A, Comotti B, Barbui T, Campobasso N, Dammacco F, Cantonetti M, Petrucci MT, Mandelli F, Resegotti L, Pileri A: Early responder myeloma: Kinetic studies identify a patients subgroup characterized by very poor prognosis. J Clin Oncol 7: I 1, 1989 23. Dune BGM, Stock-Novack D, Salmon SE, Finley P, Beckord J, Crowley J, Coltman CA: Prognostic value of pretreatment serum beta-2 microglobulin in myeloma: A Southwest Oncology Group Study. Blood 75:823, 1990 24. Bataille R, Boccadoro M, Klein B, Dune BGM, Pileri A: Creactive protein and 02 microglobulin produce a simple and powerful myeloma staging system. Blood 80733, 1992 25. Seremetis S, Inghirami G, Ferrero D, Newcomb EW, Knowles M, Dotto GP, Dalla-Favera R: Transformation and plasmacytoid differentiation of EBV-infected human B lymphoblasts by ras oncogenes. Science 243:660, 1989 26. Boccadoro M, Van Acker A, Pilen A, Urbain J: ldiotypic lymphocytes in human monoclonal gammophaties. Ann Immunol 47: 677, 1982 27. Epstein J, Barlogie B, Katzmann J, Alexanian R: Phenotypic heterogeneity in aneuploid multiple myeloma indicates pre-B cell involvement. Blood 71:861, 1988 28. Bergui L, Schena M, Gaidano G, Riva M, Caligaris-Cappio F: Interleukin 3 and interleukin 6 synergistically promote the proliferation and differentiation of malignant plasma cell precursors in multiple myeloma. J Exp Med 170:613, 1989 29. Epstein J, Xiao H, He XY: Markers of multiple hematopoieticcell lineages in multiple myeloma. N End J Med 322:664, 1990 30. Corradini P, Boccadoro M, Pileri A: Molecular evidence for B lymphocyte involvement in multiple myeloma. Blood 78:505a, 1991 (abstr, suppl 1) 3 1. Kumar R, Sukumar S, Barbacid M: Activation of ras oncogenes preceding the onset of neoplasia. Science 248: 1 101, 1990 32. Fearon ER, Vogelstein B: A genetic model for colorectal tumorigenesis. Cell 61:759, 1990 33. Van Kamp H, De Pijper C, Verlaan-de Vnes M, Bos JL, Leeksma CHW, Kerkhofs H, Willemze R, Fibbe WE, Landegent JE: Longitudinal analysis of point mutations of the N-ras proto-oncogene in patients with myelodysplasia using archived blood smears. Blood 79:1266, 1992 From www.bloodjournal.org by guest on February 6, 2015. For personal use only. 1993 81: 2708-2713 Mutational activation of N- and K-ras oncogenes in plasma cell dyscrasias P Corradini, M Ladetto, C Voena, A Palumbo, G Inghirami, DM Knowles, M Boccadoro and A Pileri Updated information and services can be found at: http://www.bloodjournal.org/content/81/10/2708.full.html Articles on similar topics can be found in the following Blood collections Information about reproducing this article in parts or in its entirety may be found online at: http://www.bloodjournal.org/site/misc/rights.xhtml#repub_requests Information about ordering reprints may be found online at: http://www.bloodjournal.org/site/misc/rights.xhtml#reprints Information about subscriptions and ASH membership may be found online at: http://www.bloodjournal.org/site/subscriptions/index.xhtml Blood (print ISSN 0006-4971, online ISSN 1528-0020), is published weekly by the American Society of Hematology, 2021 L St, NW, Suite 900, Washington DC 20036. Copyright 2011 by The American Society of Hematology; all rights reserved.
© Copyright 2026