The Unique Red Cell Heterogeneity of SC Disease: Crystal
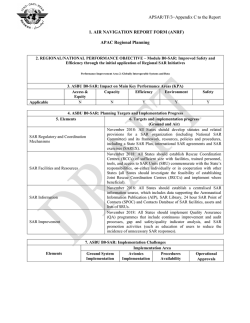
From www.bloodjournal.org by guest on February 6, 2015. For personal use only. The Unique Red Cell Heterogeneity of SC Disease: Crystal Formation, Dense Reticulocytes, and Unusual Morphology By Christine Lawrence, Mary E. Fabry, and Ronald L. Nagel Knowledge concerning SS (homozygous for the psgene) red blood cell (RBC) heterogeneity has been useful for understanding the pathophysiology of sickle cell anemia. No equivalent information exists for RBCs of the compound heterozygotefor the psand pc genes (SC) RBCs. These RBCs are known to be denser than most cells in normal blood and even most cellsin SS blood (Fabryet al,JClinlnvesf70:1284, 1981). We have analyzed the characteristics of SC RBC heterogeneity and find that: (1) SC cells exhibit unusual morphologic features, particularly the tendency for membrane “folding“ (multifolded, unifolded, and triangular shapes are all common); (2) SC RBCs containing crystals and some containing round hemoglobin (Hb) aggregates (billiard-ball cells) are detectable in circulating SC blood; (3) in contrast to normal reticulocytes, which are found mainly in a lowdensity RBC fraction, SC reticulocytes are found in the densest SC RBC fraction; and (4) both deoxygenation and replacement of extracellular CI- by NO,- (both inhibitors of K:CI cotransport)led to moderate depopulationof the dense fraction and a dramatic shift of the reticulocytes to lower density fractions. We conclude that the RBC heterogeneityof SC disease is very different from that of SS disease. The major contributions of properties introduced by HbC are ”folded” RBCs, intracellular crystal formation in circulating SC cells, and apparently a very active K:CI cotransporter that leads to unusually dense reticulocytes. 0 1991 by The American Society of Hematology. S SC disease, based on the assumption that HbC crystallization does not occur in SC cells, at least “in vivo.” Hence, the syndrome has been thought to be dominated by the tendency of the SC cells to sickle. However, evidence reported here shows that a subset of circulating SC cells do have intracellular crystals. This phenomenon can be observed particularly in SC patients with a full complement of a genes and these cells are found predominantly in the densest fraction of RBCs. In addition, we find that SC reticulocytes, independent of a-thalassemia status, are found predominantly among the densest RBCs in SC blood, in contrast to the low density of reticulocytes in AA and SS blood. High-density reticulocytes seem then to be a feature characteristic of the cells containing p’, because CC reticulocytes are also dense.5 Finally, SC RBCs have a tendency to acquire a “folded” appearance, similar to shape changes previously observed in CC disease.’ C DISEASE IS A chronic hemolytic disorder punctuated by acute painful crises and diverse chronic organ damage, secondary to the presence of both hemoglobin (Hb) S and HbC. CC disease is a mild chronic hemolytic anemia in which red blood cells (RBCs) contain only HbC (homozygous for the p” gene). Some of the factors affecting the phenotype of patients with SC disease have been identified during the last 10 years. CC and SC cells have a higher mean corpuscular Hb concentration (MCHC), and hence are denser than normal RBCs, and many of the pathophysiologic features of SC disease can be corrected when these cells are restored to a normal MCHC, a feature with potential therapeutic implications.’,’The high MCHC of SC cells resolves the paradox that SC cells are more prone to sickling than AS cells, despite HbC enhancing the polymerization of HbS “in vitro” only slightly? The increase in MCHC contributed by the p“ phenotype explains many effects attributable to increased polymer formation,* with possible minor contributions from the interactions between HbS and HbC? Some of the observations leading to these conclusions were confirmed by Bunn et a1: who also pointed out that the higher percent of psin SC (about 50% HbS) than in AS (40% HbS) also contributes to increased sickling in SC cells. Little attention has been paid to the potential influence of HbC or HbC crystal formation in the pathophysiology of From the Division of Hematology, Department of Medicine, Albert Einstein College of MedicinelMontefiore Medical Center, Bronx Municipal Hospital Center, Bronx, NY Submitted January 14, 1991; accepted June 6, 1991. Supported by National Institutes of Health (NIH) Center Grant No. HL38655 and NIHProgram Grant No. HL21016. Presented in part as an abstract in Clin Res 3%6024, 1989. Address reprint requests to Christine Lawrence, MD, Professor of Medicine, Division of Hematology, Albert Einstein College of Medicine, 1300Mom‘sParkAve, Ullmann 921, Bronx, NY 10461. The publication costs of this article were defrayed in part by page charge payment. This article must therefore be hereby marked “advertisement” in accordance with I8 U.S.C. section 1734 solely to indicate this fact. @ 1991 by The American Society of Hematology. 0006-4971/91/7808-0011$3.0010 2104 MATERIALS AND METHODS Patient material and clinical laboratory studies. Patients were examined in the Hematology Clinic of the Bronx Municipal Hospital Center, as well as in the Heredity Clinic (Dr H.H. Billett, Director) of the Bronx ComprehensiveSickle Cell Center. Diagnosis was based on two electrophoreses (cellulose acetate, borate buffer, pH 8.6, and agar, citrate buffer, pH 6.4) and a solubility test. Hematologic indices were determined with a Technicon H1 (Technicon, Tarrytown, NY) or a Coulter counter S+IV (Coulter, Hialeah, FL). Reticulocyte determinations were performed by a single observer who counted a minimum of 1,000 cells. Type 1 reticulocytes had abundant intracellular particles that tended to aggregate in one sector of the cell as a pseudo-nucleus; type 2 reticulocytes had abundant stainable particles (typically 15 or more) that were dispersed; type 3 had between 5 and 15; and type 4 had 5 or less particles. Type 1 and 2 are referred to as stress reticulocytes. To classify a cell as containing a crystal, the intracellular body has to be very dense, have sharp, straight edges, and have partially or completely depleted the cytosolic content (Hb in solution) of the cell; this last feature was most apparent when a thin rim of RBC membrane was observed encircling the crystal inclusion(s). In “billiard-ball cells” the dense intracellular body was rounded, without sharp edges, and eccentrically located; this left a portion of the RBC in which the cytosol seemed devoid of Hb and the membrane appears empty. Blood, Vo178,No8(0ctober 15),1991:pp2104-2112 From www.bloodjournal.org by guest on February 6, 2015. For personal use only. 2105 UNIQUE RBC HETEROGENEITY IN SC DISEASE RBC densify fictionation. The percent of dense cells was determined from Percoll-Stractan continuous density gradients as previously described." In these experiments we used Larex, a purified form of Stractan, manufactured by Consulting Associates (Tacoma, WA). All cell density separations were performed at 37°C except where noted. Separations performed at 4°C required an extended period of centrifugation (2 hours) to attain the same density profile. The SC4 fraction (MCHC > 42 g/dL, density > 1.103 g/mL) is the densest of four fractions (SCl to SC4)." Gradients formulated with nitrate as the anion were made with Larex subjected to an additional Amberlite MB-3 (Sigma, St Louis, MO) extraction step as previously described' to remove residual Cl-. The divisions were made at densities that are similar to, but higher than those made for SS cells (Fig I), hence a different nomenclature (SCl to SC4) is used. The densities in grams per deciliter used to define SC fractions were: SCI, less than 1.081; SC2, between 1.081 and 1.087; SC3, between 1.087 to 1.097; SC4, greater than 1.097. The percent of irreversibly sickled cells (ISCs) was determined by a single observer who counted 1,OOO RBCs. HbF determination. The percent of HbF was measured by alkaline denaturation." DNA analysis. DNA was prepared from the subjects' white blood cells (WBCs) by previously described techniques? Haplotype analysis of the P-like globin gene cluster was performed in one group of patients with the following restriction endonucleases: Hindlll,Hincll, Hinfl, and Hpa 1. In another group, the haplotypes were determined by polymerase chain reaction (PCR) amplification of the appropriate sequences that enables the detection of polymorphic sites by simple digestion with either Hindlll, Hincll, or Hinfl5' to the P gene site. The PCR detection of the site Hpa I 3' to f3 chain has proven to be unreliable, so this site has only been defined by Southern blotting. Digestion of the PCR-amplified segments yielded easily identifiable fragments detected by ethidium bromide.'" Some DNA was processed by both methods with identical results. The a-globin gene haplotypes were determined as previously reported? Glucose-6-phosphate dehydrogenase (Gd-PD) determination. Gd-PD was measured using a Sigma kit (345-UV) for kinetic determination of enzyme activity at 340 nm. Complete lysis was ensured by freezing in liquid nitrogen and thawing in water three times. Samples were spun in a microfuge, to remove particulate matter, before recording UV absorption: kinetics were measured at 30°C and (3-6-PD activity was recorded as units per gram of Hb. One unit is the amount of G-6-PD activity that will convert 1 kmol of substrate per minute. Fig 1. Percoll-Stractancontinuous density gradientseparation of normal cells (far left) and of the 10 SC patients discussed. The five patients on the left have a-thalassemia ( - a / m )and average fewer cells in the bottom of the gradient (densest class of cell, SC4). The patients' density gradients are displayed in the same order as Table 1. Density class SC4d. presented in Table 1, consists of the sum of the two densest divisions (marked 4d). whereas SC4 consists of the sum of the three and one-half densest divisions. REF A Scanning electron microscop. Cells were washed in phosphatebuffered isotonic saline, pH 7.4, and fixed in 10% buffered formaldehyde or, on some occasions. 2% glutaraldehyde. Fixed cells were allowed to adhere to polylysine-coatedglass coverslips, rinsed briefly in distilled H,O, followed by dehydration in a graded ethanol series. Specimens were dried in CO, in a Tousimis 790 (Tousimis Research Corp, Lockville, MD) critical point drier, then sputter-coated with goldlpalladium in a Denton Desk-1 sputter coater. Specimenswere observed in a JEOL 25SM or a JEOL 6400 scanning electron microscope at an acceleratingvoltage of 14 kV. Ligand-stateeffect on RBC density. To study the potential effect of ligand on the density distribution of SC RBC and reticulocytes, the following experiment was performed. Cells suspended in plasma were first partially deoxygenated by alternate exposure to N, and vacuum in a serum cap-sealed tube. They were then transferred to an N,-filled glove bag and the suspension was layered on top of 5.9 mL of Percoll-Larexgradient mix, to which 20 kL of a 1 mol/L solution of dithionite in saline had been added. The tubes were stirred and the sample was allowed to equilibrate for 30 minutes at room temperature, after which the tubes were centrifuged as described in the section for density fractionation. Samples for scanningmicroscopywere obtained from the dithionitetreated gradients by removing them with a syringe previously washed in dithionite solution. Before fixing in 10% buffered formaldehyde, the cells were washed in saline containing 20 WLof 1 mol/L dithionite per 10 mL. SC and AA whole blood equilibrated with CO and incubated with the same concentration of dithionite for 30 minutes were used as controls for these experiments. For reticulocyte preparations, the dithionite was washed out with two 1:20 washes with deoxygenated saline, and the cells were resuspended in plasma before incubation with supravital dye. Effect of deoxygenation on intracellularcrystals. There were too few naturally occurring SC crystals to allow reliable determination of changes in the percent of crystal-containingcells after deoxygenation; therefore, 5% NaCl was added to SC whole blood to reach a final osmolarity of 820 mOsm/Kg H?O.After 4 hours, sharp-edged, distinct HbC-like crystals were well formed. These cells were then deoxygenated either by alternate vacuum and N, with hand agitation or in a tonometer with intermittent mixing (Instrumentation Laboratories, Lexington, MA). The percent of oxygen saturation was determined by Cooximeterreadingsof aliquots (Instrumentation Laboratories). In both cases, less than 10%oxygen saturation was reached in about 15 minutes and the cells were then maintained deoxygenated for another 20 minutes. Aliquots were examined at 15-minute intervals and crystals were counted in wet A I II aa/aa aa/-a I I sc I From www.bloodjournal.org by guest on February 6, 2015. For personal use only. 2106 LAWRENCE, FABRY, AND NAGEL preparations and in reticulocyte-stained smears. These experiments were designed to show if crystals in SC RBCs melt when deoxygenated. Effectof isotonic NO,- on SC cell densiy. To estimate the effect of KCI cotransport on the density distribution of SC whole blood and individual elements such as reticulocytes, SC whole blood was incubated in isotonic (280 mOsm) media in which C1- had been replaced with NO,- [the medium contained 10 mmol/L glucose, 0.5 g% bovine serum albumin [BSA], 5 mmol/L PO, buffer at pH 7.4, and 140 mmol/L NaNO, with 4 mmol/L KNO, and Mg(NO,),] for 30 minutes at 38°C. Because K:Cl cotransport is chloride dependent, any role that it might have is negated in the absence of C1-. At the end of 30 minutes the cells were washed with fresh isotonic nitrate media and then reconcentrated. The cells were then separated by density gradient centrifugation by mixing 0.5 mL of packed cells with 5.5 mL of isotonic Percoll-Larex mixture containing NO,- as the anion. The gradient was then fractionated into density classes SC1 to SC4 using the same depth in the tube as was used for chloride-containing gradients to separate the fractions. An aliquot from each fraction was taken for a reticulocyte count and was washed three times in isotonic saline and then resuspended in autologous plasma. The percent of cells in fractions (SC1 to SC4) was determined in two different ways. Grams of Hb in each fraction were measured by diluting the cells in each fraction to a known volume and determining the Hb concentration of an aliquot; alternatively, the density gradients were photographed and read by a densitometer as previously described6with the exception that the depth in the tube was adjusted to conform to the separation used for SC blood. When these two methods were compared, we found a ratio of 1.17 f 0.14 (mean f SD) between grams per deciliter Hb per fraction and the densitometrically determined percent of cells in each fraction. Therefore, we used the densitometrically determined percent of cells in each fraction to calculate the absolute percent of reticulocytes in each fraction. Statistics. The statistics program Statgraphics 4.0 (STSC-PlusWare, Rockville, MD) was used on an IBM-AT (International Business Machine, NY) for plotting and for the two-sample t-test. RESULTS Table 1 summarizes pertinent findings in the 10 patients included in this report. The most striking finding was the presence of large visible intra-erythrocytic crystals in circulating RBCs of all SC patients with a normal complement of a-genes. Crystals in circulating RBCs (taken directly from finger-stick samples) could be seen not only in Wright and supravital stained smears, but also in “wet” preparations in which the finger-stick sample was collected directly into saline with 10% buffered formaldehyde (Fig 2A, B, and C). Blood from three of the five SC patients with a-thalassemia who had the lowest mean corpuscular volumes (MCVs) did not exhibit intra-erythrocytic crystals. Regardless of a-gene status, there were RBCs in all patients that contained a single, eccentrically located, heavily stained globular (round) mass of Hb that we refer to as “billiard-ball cells” (Fig 3). These cells are different from spherocytes in that the globular mass depletes the adjacent Hb and separates from the membrane, which then appears empty. These cells were seen on the blood smears of all SC patients and, when density gradient fractions were examined, they were found predominantly among the denser cells (SC4) (Table 1). In Table 1, we compare the percent billiard-ball cell count of SC4 with that of SC2 (the most abundant density fraction in SC blood). By scanning electron microscopy, SC patients, regardless of a-genes status, have striking, abnormally shaped cells (Fig 4). “Multi-folded cells” were common (Fig 4A), some of them having only a single fold and resembling pita bread (Fig 4B). These are probably the cells that Krauss and Diggs” called “fat cells,” because in the Wright-stained smear they appear as wide bipointed cells and the folding is difficult to appreciate. Cells with triconcave shapes, ie, Table 1. Hematologic and Related Parameters in Ten Patients With SC Genotype Patients Sex p-gene haplotype Hb (g/dL) Hct (%) MCV (fL) RDW WB Retics (YO) SCl* Retics (YO) SC2 Retics (YO) SC3 Retics (YO) SC4 Retics (YO) HbF (Yo) a-gene status Dense cells (%) (SC4)t (SC4d) Densest cells (YO) ISC (%) WE Crystals (%) Billiard-ball cells (YO) (SC2) Billiard-ball cells (%) (SC4) G-6-PD (U/g Hb) CE F BEN/C 10.7 29.9 62 18.0 5.5 0.2 1.3 7.7 23.7 1.7 3a 5.7 2.9 0.6 0 1 10 13.75 PK F BAN/C 11.1 30.0 70 15.6 4.6 3.8 3.0 6.2 6.8 4.4 3a 14.3 1.1 0.5 0 1 5 7.42 ss F BEN/C 10.2 27.8 71 16.6 10.5 4.4 8.8 14.7 10.5 2.2 3a 15.7 2.8 0.2 0 1 10 14.85 RJ M BAN/C 13.5 38.9 76 18.4 7.4 0.6 1.3 8.3 18.1 0.9 3a 18.3 4.1 1.2 0.8 0 4 13.60 YH F SEN/C 10.1 32.9 82 16.0 9.0 2.2 4.9 11.7 14.1 4.8 3a 25.1 4.5 1.2 1.2 1 2 12.96 _. GB F BAN/C 11.7 32.2 75 16.0 7.5 0.8 3.2 15.3 9.2 1.3 4a 14.5 3.4 1.1 0.8 2 9 15.34 NA F BEN/C 11.8 30.6 82 14.1 10.0 5.3 11.2 18.3 11.5 1.8 4a 20.5 2.8 0.5 1.2 0 4 5.04 RT M BEN/C 13.4 39.9 88 18.6 7.1 0.2 3.5 9.5 17.6 0.8 4a 30.5 4.3 1.5 0.1 1 6 3.38 VR F BEN/C 10.6 31.4 90 18.0 8.5 1.9 4.7 13.5 16.7 2.4 4a 17.1 2.3 1.o 0.15 0 10 19.63 SP F BEN/C 11.1 32.9 95 14.2 6.9 1.8 4.4 16.6 23.4 1.3 4a 14.1 4.0 1.E 0.06 0 6 11.50 ~~ Abbreviations: WB, whole blood; BEN, Benin; BAN, Bantu; SEN, Senegal; C, typical HbC associated haplotype. *SCl-SC4, density gradient fractions; underlined numbers are the highest percentage of reticulocytes in each density separation. tBoth percent SC4 and percent SC4d are average valuesfor several determinations. SC4d consists of the two densest divisions as shown in Flg 1. From www.bloodjournal.org by guest on February 6, 2015. For personal use only. UNIQUE RBC HETEROGENEITY IN SC DISEASE 2107 A cells, and was particularly notable for the presence of invaginations (Fig 5 ) ; however, cells in SC3 were also irregular in shape. 3. Crystal-containing cells and billiard-ball cells were found predominantly in SC3 and SC4 in SC patients with the normal complement of a-genes and in two of the five a-thalassemics with the largest MCVs (Fig 6 ) , although any inference must be tentative due to the small number of cases. These crystals were best seen and most easily counted in supravital-stained preparations because most of the crystals remained bright red, ie, unstained, in contrast with the bluish color of the cytosol Hb in the rest of the cells. In contrast, billiard-ball cells were found in all 10 SC patients, regardless of their a-thalassemia status (Fig 3, Table 1). It is worth noting that the ISCs commonly found in the densest fraction in SS blood were uncommon in SC blood samples, even in the SC4 fraction (Table 1). 4. When the separation was conducted at 37T, the highest absolute reticulocyte count (Fig 7) (absolute reticulocytes are the percent reticulocytes tines the percent cells in a fraction) was found in SC3 and SC4, which corresponds to densities greater than 1.0879 g/dL, although the highest percent of stress reticulocytes (as defined in Materials and Methods) was found in fraction SCl (Fig 8). Under the same conditions, CC cells also exhibited increased reticulocyte counts in the densest fraction.' These findings contrast Fig 2. Crystalcantaining RBCs in circulating blood of SC patients. Blood obtained by finger-stick. Note crystals indicatedby arrows. (A) 10% buffered formaldehyde fixed wet preparation;(6)Wright-stained smear; (C) supravital-stainedsmear. Note the cell membrane sunounding the Hb-depleted cytosol in the crystal-containing RBCs (arrows). (Originalmagnification x 1.000.) triangular cells with three dimples, were similar to those seen in acute alcohol intoxication that Bessis'* named "knizocytes" (Fig 4C). The density separation of SC cells (Fig 1) showed several features: 1. Previously reported, most of the RBCS in sc individuals were denser than AA cells, with the majority of cells exhibiting a density intermediate between AA and C c cells.* was their 2*The denser the sc cells, the more shape. Fraction SC4 contained the most abnormally shaped sa Fig 3. Billlard-ball cells in fraction isoiatd from PemollStractan density gradient from patient CE (-dad. (A) Supravital Stain; (B) Wright-stained smear. The dense, eccentrically located Hb aggregateappears to contain most of the Hb in the cell; a piece of the membrane surrounds a portion of the cytosol devoid of Hb. Note that some of these "billiard-balls cells" are reticulocytes. (Original magnification xi,ooo.) From www.bloodjournal.org by guest on February 6, 2015. For personal use only. 2108 Fig 4. Scanning electron microscopy of individual SC cells. Electron micrographs illustrate: (A) mukifolded SC cells (original magnification ~ 6 , 5 0 0 )(B) ; unifolded SC cells resembling pita bread, most likely the same cell described as "fat cell" in Wright-stainedsmears by Krauss and Diggs"; (C) tridimpled SC cell, also called triangular cells and knizocytes by others. (Originalmagnification x 10,000.) strikingly with the usual distribution of reticulocytes in normal blood at 37°C in hemolytic anemias in AA and SS individuals and thalassemics. In most SS patients, 90% of all reticulocytes are found in SSl and SS2 at densities less than 1.091." In all of these cases, reticulocytes are among the lightest cells in the blood. However, if the separation of SC RBCs is conducted at 4"C, the majority of reticulocytes are found in SCl and SC2. 5. There was a ligand-dependent reduction of aggregated forms. We found that deoxygenation, both by hand with LAWRENCE, FABRY, AND NAGEL alternating vacuum and N,, and by tonometer, resulted in the disappearance of more than 80% of the crystals at the end of 30 minutes, and 95% to 100% of the crystals at the end of 45 minutes. 6. There was a ligand-dependent redistribution of RBCs and reticulocytes. In contrast to the effects seen in SS individuals," the density distribution of SC RBCs on deoxygenated density gradients showed a small reduction of cells in the densest fractions (SC3 and SC4). When cells were separated into four fractions and the percent of reticulocytes in each fraction was determined, we found that reticulocytes had migrated from the densest fractions (SC3 and SC4) to the less dense fractions (SCl and SC2) (Fig 9). 7. The replacement of chloride with nitrate had an effect on the distribution of RBCs and reticulocytes. Incubation of SC whole blood in isotonic nitrate medium effected only a small shift in density distribution, with some cells moving from the two densest fractions, SC3 and SC4, into the two lighter fractions, SCl and SC2. However, a much more striking shift in the density distribution of reticulocytes occurred. Dramatic effects were seen on the absolute reticulocyte distribution shifted from a maximum in SC3 and SC4 to a maximum in SC2 in the five patients studied by this approach (Fig IO). 8. G-6-PD determination in the oxygenated SC fractions (room temperature) showed that the activity was similar in all of the density fractions (data not shown). This result is in contrast to AA and SS blood, in which the enzyme activity decreases pari-passu with the increasing density of the fraction, presumably due to the presence of older cells in higher density fractions. These results in SC blood must be interpreted in conjunction with the abnormal density distribution of reticulocytes and the progressively more abnormal shapes observed on scanning electron microscopy (EM). The low G-6-PD activity of the presumably older cells found in SC3 and SC4 (based on their abnormal shapes) is compensated for by the increase in the number of reticulocytes in those denser fractions, resulting in a flat distribution of G-6-PD at all cell densities. Finally, p-gene cluster haplotypes were determined in all patients as a matter of record. Because of the small size of the sample, it is impossible to draw any conclusions from the data. DISCUSSION The data presented here show that circulating RBCs of patients with SC disease do contain crystals. The presence of circulating crystals in SC disease needs to be compared with this tendency in CC and AC genotypes. While all CC individuals form tetragonal CC crystals "in vitro" after dehydration or exposure to hypertonic medium," circulating HbC crystals are observed predominantly in splenectomized CC individuals. SC patients have a greatly reduced splenic function by the time they reach adulthood, although they retain a palpable spleen longer than SS individ~als.'~ In AC subjects, crystals are not observed either "in vivo" or "in vitro"." The formation of morphologically identifiable crystals From www.bloodjournal.org by guest on February 6, 2015. For personal use only. 2109 UNIQUE RBC HETEROGENEITYIN SC DISEASE SC DENSITY FRACTIONATION (3K mag) sc 1 sc 2 Fig 5. Scanning electron microscopy of the four density fractions found in SC blood. Note that as the cells become more dense, they became progressively more abnormal. These cells have unusually deep invaginations that are consistent with dehydration. sc 3 sc 4 appears to be only the tip of the iceberg in terms of Hb aggregation (which is different than HbS polymerization)in SC cells. RBCs with “marginated” Hb, but not sharp crystal-like edges, were commonly observed in Wrightstained smears, “wet” preparations, and supravital-stained reticulocyte smears in these patients. These “marginated,” globular dense bodies incorporated most of the RBC Hb (billiard-ball cells) and were observed in the densest gradient fraction of all SC patients (Fig 3, Table 1). Striking morphologic differences, in addition to the crystal-containing cells, are another feature of the blood of SC patients. Scanning electron microscopy shows unusual shapes of SC cells in the different density fractions. Fraction SCl exhibits flattened RBCs and occasional “folded cells.” These characteristics are more prominent in SC2 and SC3. In this latter fraction, triple-folded cells are quite common. Of note is that these “folded” cells are reminiscent of RBC abnormalities found in HbC homozygotes.’ Finally, in SC4, grossly pitted cells, bizarre folded cells, and cells that appear to have intracellular “crystals” are apparent. The presence of true crystals is confirmed by “wet” preparations and supravital-stained smears under light microscopy (Figs 2 and 6). These crystals rapidly disappear under fully deoxygenated conditions, which is similar to the IF d Fig6. Crystalcontaining cells Insupravital-stained preparation. B Crystals Isolated from SC4 fraction and stained with new methylene blue, which stains the cytosol Hb blue but is excluded from the red crystals. Crystals are indicated by arrows. From www.bloodjournal.org by guest on February 6, 2015. For personal use only. 2110 LAWRENCE, FABRY, AND NAGEL .." A n T sc 1 sc3 sc2 I m 5.0 ~ sc 1 sc4 Fig 7. Absolute reticulocytes in the four SC density fractions. The absolute value was obtained by multiplying the percent of reticulocytes by the percent of cells found in that density fraction. The points are the average values for the 10 patients studied plus or minus the standard error. behavior of crystals formed in vivo in CC individual^.'^ This finding suggests that crystals are formed from the oxygenated form of Hb. Another unique feature of SC disease is the presence of dense reticulocytes. When the density separation is performed at 37T, the highest percent of reticulocytes is found in the SC4 fraction, while the highest absolute number is found in fractions SC3 and SC4. However, if the separation is performed at 4"C, SC reticulocytes are found in the top two fractions. Low temperature inhibits KCl cotransport" and many other RBC processes. The high density of SC reticulocytes observed at the physiologic temperature of 37°C more accurately reflects the in vivo density distribution. At 37"C, 90% of SC reticulocytes are found at densities in excess of 1.087 g/dL. In contrast, 90% of SS reticulocytes are found at densities less than 1.091g/dL. Stress reticulocytes, the youngest forms, are present in the highest percent in SC1. The finding of most of the SC reticulocytes in dense fractions is surprising, because in AA and SS individuals, reticulocytes of all ages are predominantly low-density cells at 37°C. One explanation for this A sc2 sc3 sc4 Fig 9. Absolute reticulocytes in SC patients after deoxygenation and separation on a deoxygenated density gradient. (0.W, A) Cells an average value of five patients from three individual patients; (0) studied on oxygenated chloride Percoll-Stractan gradients. result is that reticulocytes in SC disease exit the marrow as low-density cells and become dense within 24 hours, sinking to the denser fractions. The G-6-PD data show that either SC cells do not exhibit the characteristic reduction of enzyme level usually associated with aged high-density RBCs or that the high-density cells are a mixture of old and young cells. Why are SC reticulocytes so dense? Brugnara et al'*.'' were the first to detect a volume-stimulated K+ efflux in CC and SS cells. Canessa et almI2'were the first to establish that this transport system was C1-dependent and stimulated by N-ethyl maleimide (NEM) in CC and SS cells. These findings showed that the volume-stimulated K+ efflux reported by Brugnara et a1'8.1ywas, in fact, the KCl transport system previously discovered by Ellory and Dunham" in sheep RBCs. Hall and E l l ~ r y ?Canessa ~ et al,7324325 and Brugnara et a126327further showed independently that this transporter was predominantly present in young RBCs (including HbA reticulocytes), explaining its elevated activity in SS blood. These previously reported experiments do not settle the origin of the increased density of CC cells nor can they, by themselves, explain the increased density of SC reticulo- 90 3 v) w E3 3+ x 70 0 0 3 60 .-0 A+ a, 50 40 !z W U v) a: m 80 30 20 10 0 CK j ; ;= W A+ -30 m .I, a sc1 2 SC2 SC3 A ~ A aAA SC4 Y a Whole Blood Fig 8. Stress reticulocytes as percent of all reticulocytes in the four SC density-defined fractions (SC1-4) and in whole blood. ( 0 )Patients with four a-genes; (A)patients with one a-gene deletion (-a/aa). sc 1 sc2 sc3 sc4 Fig 10. Absolute reticulocytes in five SC patients after incubation in isotonic nitrate and separation on a nitrate containing PercollStractan gradient. (0)Average values of five experiments in nitrate average values for five experiments performed under the media; (0) same conditions in chloride-containing gradients. Error bars represent standard error. From www.bloodjournal.org by guest on February 6, 2015. For personal use only. 2111 UNIQUE RBC HETEROGENEITY IN SC DISEASE cytes. Nevertheless, the data in Fig 10 provide a partial explanation for the phenomena. The density distribution of SC reticulocytes, but not mature cells, shifts when C1- is removed from the media and replaced by NO,-, the percent of dense cells is reduced, and the reticulocytes move to less dense fractions. Because KCI cotransport is abolished under these circumstances, we conclude that SC reticulocytes are endowed with a highly active K C l cotransport system (even at isotonic conditions) that decreases RBC volume when the K’ and C1- efflux are not compensated with Na’ influx or Na’/H’ exchange. K C l cotransport and Na’/H’ antiport activity in CC cells have been measured by Fabry et al’ and will be reported in full elsewhere, including similar data for SC cells. This finding should not be confused with the early observation of Bertles and Milnera (recently confirmed by Bookchin et al)29 that SS dense cells mostly originate directly from the lightest density fraction. In the case of SS, the densest cell fraction does not contain a significant number of reticulocytes, although the cells are younger than less dense fractions. The unusual finding in SC blood is that most mature reticulocytes are observed in the densest fraction. What are the implications of these findings vis-a-vis the pathophysiology of SC disease? We need to understand why SC patients exhibit circulating RBCs containing crystals. There are three factors to consider, which are not mutually exclusive: (1) the spleen fails to eliminate crystal or aggregate containing RBCs due to infarction and/or functional asplenia (secondary to blockade of reticuloendothelial cells); (2) HbS accelerates the crystallization of HbC in vitro,” and it is reasonable to infer that this phenomena might occur also “in vivo”; and (3) although the percentage of HbC is only about 50% in SC patients, this Hb is at a higher intra-erythrocytic concentration than in HbC trait RBCs (which also contain 50% HbC). This increased density (MCHC) in SC RBCs is the result of a more active KCI cotransport system in the young RBCs. Why are crystal-containing SC cells particularly prominent in the densest fraction? There are two possible explanations: (1) the presence of crystals increases the density of these cells (the concentration of Hb crystals is about 68 g/dL) and/or (2) the SC cells that are, for whatever reason, destined to become densest are also likely to produce crystals as a byproduct of the progressive increase in MCHC. This phenomenon is, of course, reminiscent of CC disease,’ in which crystals are found in the highest density fraction. Does the presence of SC cells containing crystals and aggregated Hb contribute to the vaso-occlusiveevents in SC disease? The answer is most probably no. Based on the data presented here, and knowledge acquired in the study of CC di~ease,”.~’ some predictions can be made as to the pathophysiologic role of SC RBCs containing Hb aggregates and crystals in vaso-occlusion. As in CC, we have shown that SC crystals melt on deoxygenation, presumably because their crystal structure is based on Hb in the oxygenated conformation, which then changes when oxygen is removed.’’ Hence, the previous analysis developed for CC disease is also applicable to SC disease. After initial vaso-occlusion, low pH and progressive deoxygenation follow, leading to melting of the crystals and increased deformability. In contrast, SS cells become even more rigid under these conditions. In addition, the lower MCV of SC cells affords partial protection from obstruction?’ These characteristics of SC cells might contribute to the lower incidence of painful crises in SC disease when compared with sickle cell disease. In summary, the findings reported here are the following: (1) in addition to the already reported higher than normal MCHC of SC cells,’ the percent of the very dense cells seems to depend in part on the a-thalassemia status, although this fact needs to be confirmed in a larger sample; (2) crystal-containing cells circulate and are observed in the densest fractions; (3) deoxygenation melts intracellular crystals and decreases the MCHC of some of the very dense SC cells (SC3 and SC4), suggesting that other forms of Hb aggregation, besides the morphologicallyrecognizable HbClike tetragonal crystal, occur in these cells and are liganddependent; (4) the majority of SC reticulocytes are of high density, although they might not have entered the circulation in that state. Deoxygenation or removing C1- from the extracellular media dramatically shifts these reticulocytes to lower densities. A highly active K C l co-transport in SC reticulocytes is probably the basis for this phenomenon; and (5) multi-, tri-, or unifolded RBCs are a morphologic feature of SC disease, similar to those of CC disease.’ We conclude that RBC heterogeneity in SC disease is under a different pathophysiologic control than in SS disease, due to the effects of the presence of HbC, including HbC-driven crystal formation in some of the dense SC cells, high-density reticulocytes, and a tendency to form “folded” RBCs. ACKNOWLEDGMENT We are deeply indebted to Sandra Suzuka and Rose Grossman for their excellent technical assistance. In addition, we acknowledge the contribution of Dr Soili Erlingson for p and a cluster haplotype determinations in these patients. We thank the Analytical Ultrastructural Center at the Albert Einstein College of Medicine and Jane Fant and Lynn Dean for their excellent help with the scanning electron microscopy. REFERENCES 1. Fabry ME, Kaul D, Raventos C, Baez S, Rieder R, Nagel R L polymer solubilities of deoxyhemoglobins S + C and S + A Some aspects of the pathophysiology of homozygous hemoglobin mixtures. Blood 673387,1986 CC red cells. J Clin Invest 671284, 1981 4. Bunn HF, Noguchi (JT, Hofrichter J, SchechterGP, Schechter 2. Fabry ME, Kaul DK, Raventos-Suarez C, Chang H, Nagel AN, Eaton W A Molecular and cellular pathogenesis of hemogloRL: SC red cells have an abnormally high intracellular hemoglobin bin SC disease. Proc Natl Acad Sci USA 79:7527,1982 concentration: Pathophysiological consequences. J Clin Invest 5. Fabry ME, Canessa M, Romero J, Lawrence C, Nagel R L 70:1315,1982 The unique density distribution of reticulocytes and ion transport 3. Bookchin RM, Balazs T: Ionic strength dependence of the properties in HbC red cells. Blood 74:983a, 1989 (abstr, suppl 1) From www.bloodjournal.org by guest on February 6, 2015. For personal use only. 2112 6. Fabry ME, Mears JG, Patel P, Schaefer-Rego K, Carmichael D, Martinez G, Nagel R L Dense cells in sickle cell anemia: The effects of gene interaction. Blood 64:1042,1984 7. Canessa M, Fabry ME, Blumenfeld N, Nagel R L A volumestimulated, CI- dependent K+ efflux is highly expressed in young human red cells containing normal hemoglobin or HbS. J Membr Biol97:97, 1987 8. Pembrey ME, McWade P, Weatherall J: Reliable routine estimation of small amounts of foetal haemoglobin by alkali denaturation. J Clin Pathol25:738,1971 9. Nagel RL, Rao SK, Dunda-Belkhodja 0, Connolly MM, Fabry ME, Georges A, Krishnamoorthy R, Labie D: The hematological characteristics of sickle cell anemia bearing the Bantu haplotype: The relationship between G~ and HbF level. Blood 69:1026, 1987 10. Sutton M, Bouhassira EE, Nagel R L Polymerase chain reaction amplification applied to the determination of p-gene cluster haplotypes. Am J Hematol3266,1989 11. Krauss AP, D i g s LW: In vitro crystallization of hemoglobin occurring in citrated blood from patients with hemoglobin C. J Lab Clin Med 47:700,1956 12. Bessis M: Red cell shapes: An illustrated classification and its rationale, in Bessis M, Weed RI, Leblond PF (eds): Red Cell Shape. New York, NY,Springer-Verlag, 1973 13. Kaul DK, Fabry ME, Windisch P, Baez S, Nagel R L Red cells in sickle cell anemia are heterogeneous in their rheological and hemodynamic characteristics. J Clin Invest 72:22,1983 14. Fabry ME, Nagel R L The effects of deoxygenation on red cell density: Significance for the pathophysiology of sickle cell anemia. Blood 601370,1982 15. Hirsch RE, Raventos-Suarez C, Olson JA, Nagel R L Ligand state of intraerythrocytic circulating HbC crystals in homozygote CC patients. Blood 66:775,1985 16. Serjeant GR: Sickle Cell Disease. New York, NY, Oxford, 1985 17. Canessa M: Personal communication, July 1990 18. Brugnara C, Kopin AS, Bunn HF, Tosteson DC: Regulation of cation content and cell volume in patients with homozygous hemoglobin C disease. J Clin Invest 75:1608,1985 19. Brugnara C, Bunn HF, Tosteson D C Regulation of erythrocyte cation and water content in sickle cell anemia. Science 232:388,1986 LAWRENCE, FABRY, AND NAGEL 20. Canessa M, Spalvins A, Nagel R L Volume-dependent and NEM stimulated K+:CI- transport is elevated in SS, SC and CC human red cells. Red Cell Club, Yale University, Nov, 1985. Biophys 549580,1986 (abstr) 21. Canessa M, Spalvins A, Nagel R L Volume-dependent and NEM-stimulated K+:CI- transport is elevated in oxygenated SS, SC and CC human red cells. FEBS Lett 200197,1986 22. Ellory JC, Dunham PB: Volume-dependent passive potassium transport in LK sheep red cells, in Lassen UV, Ussing HH, Wieth JO (eds): Membrane Transport in Erythrocytes. Alfred Benzon Symposium 14. Copenhagen, Denmark, Munksgaard, 1980, p 409 23. Hall AC, Ellory JC: Evidence for the presence of volumesensitive KC1 transport in 'young' human red cells. Biochim Biophys Acta 858:317,1986 24. Canessa M, Fabry ME, Blumenfeld N, Spalvins A, Nagel R L A volume-dependent K+:CI- transporter is highly expressed in young human red cells with AA and SS hemoglobin: Physiological and pathophysiological implications. J Gen Physiol 88:14, 1986 (abstr) 25. Canessa M, Fabry ME, Spalvins A, Blumenfeld N, Nagel R L Activation of a KC1 transporter by cell swelling in Hb SS red cells, in Nagel RL (ed): Progress in Clinical and Biological Research: Pathophysiological Aspects of Sickle Cell Vasoocclusion (~01240).New York, NY,Liss, 1987, p 201 26. Brugnara C, Tosteson D C Cell volume, K' transport and cell density in human erythrocytes. J Gen Physiol88:14a, 1986 27. Brugnara C, Tosteson DC: Cell volume, K' transport and cell density. Am J Physiol21:C269,1987 28. Bertles JF, Milner P F A Irreversibly sickled erythrocytes: A consequence of the heterogeneous distribution of hemoglobin types in sickle cell anemia. J Clin Invest 47:1731,1968 29. Bookchin RM, Ortiz OE, Lew V L Evidence for a direct reticulocyte origin of dense cells in sickle cell anemia. J Clin Invest 87:113, 1991 30. Kaul DK, Baez S, Nagel R L Flow properties of oxygenated HbS and HbC erythrocytes in the isolated microvasculature of the rat. A contribution to the hemorheology of hemoglobinopathies. Clin Hemorheol1:73,1981 From www.bloodjournal.org by guest on February 6, 2015. For personal use only. 1991 78: 2104-2112 The unique red cell heterogeneity of SC disease: crystal formation, dense reticulocytes, and unusual morphology C Lawrence, ME Fabry and RL Nagel Updated information and services can be found at: http://www.bloodjournal.org/content/78/8/2104.full.html Articles on similar topics can be found in the following Blood collections Information about reproducing this article in parts or in its entirety may be found online at: http://www.bloodjournal.org/site/misc/rights.xhtml#repub_requests Information about ordering reprints may be found online at: http://www.bloodjournal.org/site/misc/rights.xhtml#reprints Information about subscriptions and ASH membership may be found online at: http://www.bloodjournal.org/site/subscriptions/index.xhtml Blood (print ISSN 0006-4971, online ISSN 1528-0020), is published weekly by the American Society of Hematology, 2021 L St, NW, Suite 900, Washington DC 20036. Copyright 2011 by The American Society of Hematology; all rights reserved.
© Copyright 2026