Origin of Human Mast Cells: Development From
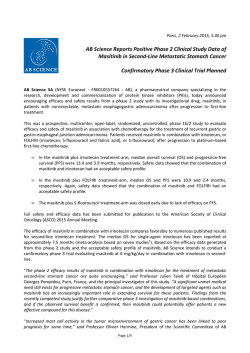
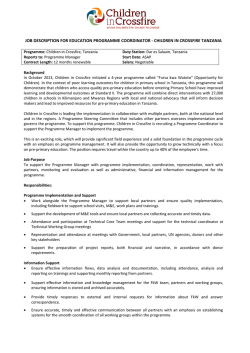
Origin of Human Mast Cells: Development From Transplanted Hematopoietic Stem Cells After Allogeneic Bone Marrow Transplantation By M. Fodinger, G. Fritsch, K. Winkler, W. Emminger, G. Mitterbauer, H. Gadner, P. Valent, and C. Mannhalter Although mast cells are hematopoietic cells, little is known about the origin of their precursors in vivo. In this study, the origin(donor Y recipient genotype) ofhuman mastcells (MCs) was analyzed in a patient who underwentallogeneic bone marrow transplantation (BMT). The patient presented with secondary acute myeloid leukemia (French-AmericanBritish classification, M21 arising from refractory anemia with excess of blast cells and bone marrow (BM) mastocytosis. Transplantation was performed in chemotherapyinduced complete remission. On days 88, 126, 198, and 494 after BMT, mast cells were enriched t o homogeneity from bone marrow mononuclear cells (BM MNCs) by cell sorting for CD117'/CD34- cells. Purified mast cell populations were CD117(c-kit)+ (>95%),CD34(<l%), CD3- (<l%), CD14(<l%), and virtuallyfree of contaminating cells as assessed by Giemsa staining. The genotype of MCs was analyzed after amplification by polymerase chain reaction (PCR) of a variable number tandem repeat (VNTR) region within intron 40 of the vonWillebrand factor(vWF) gene.Unexpectedly, on days 88 and 126 after BMT, sorted MCs displayed recipient genotype as shown by vWF.VNTR-PCR. However, on days 198 and 494, PCR analysis showed a switch t o donor genotype in isolated mast cells. Peripheral blood (PS) and BM MNC as well as highly enriched (sorted) CD3+ T cells (PB, BM), CD4+ helper T cells (PB), CD8' T cells (PB), CD19' B cells (PB), CD14+ monocytes (PB, BM), and CD34' precursor cells (BM) showed donor genotype throughout the observation period. Together, these results provide evidence that human MCs developed in vivo fromtransplanted hematopoietic stem cells. Engraftment and in vivo differentiation of MCs from early hematopoietic progenitor cells may be a prolonged process. 0 1994 by The American Society of Hematology. M transplantation (BMT) in complete remission (CR). For discrimination between donor and recipient genotype of MCs we used amplification by polymerase chain reaction (PCR) of a highly variable region (variable number tandem repeat, VNTR) within intron 40 of the von Willebrand factor(vWF) gene. AST CELLS (MCs) represent a distinct cell lineage within the hematopoietic cell ~ y s t e m . "These ~ cells have characteristic secretory granules and produce a number ofvasoactive andimmunomodulatingsubstances suchas histamine,heparin, ortumor necrosis factor Mast cells reside in various organs including lung, skin, and thegastroheintestinal However, although MCs belong to the matopoietic cell system, the number of human MCs in normal bone marrow (BM) usually is very low. The origin of MCs from hematopoietic progenitor cells isagenerallyaccepted hyp~thesis.'.''"~Differentiationof humanMCscanbe inducedinvitro from c-kit', CD34' colony-forming cell^.'^^'^ However, whether human MCs are replenished from BM-derived or circulating stemcells throughout life remains unknown at present. Alternatively, MCs may develop fromlocal progenitor cell pools in various tissues. To study in vivo originof human MCs from BMprecursor cells, we analyzed the MC genotype (donor v recipient) in a patient with acute myeloid leukemia (AML) (after myelodysplastic syndrome [MDS]) who underwent allogeneic BM From the Clinical Institute of Medical and Chemical Lab Medicine, Department of Molecular Biology: and the I. Medical Department, Division of Hematology and Hemostaseology, Universiv of Vienna, and St Anna Childrens ' Hospital, Vienna, Austria. Submitted March 15, 1994; accepted June 30, 1994. Supported by Fonds zur Forderung der Wissenschaftlichen Forschung in Osterreich and Grant No. P-9359. Address reprint requests to Christine Mannhalter, PhD, Clinical Institute of Medical and Chemical Lab Medicine, Department of Molecular Biology, The University of Vienna, Wahringer Giirtel 1820, A-1090 Vienna, Austria. The publication costsof this article were defrayedin part by page chargepayment. This article must therefore be hereby marked "advertisement" in accordance with 18 U.S.C. section 1734 solely to indicate this fact. 0 1994 by The American Society of Hematology. 0006-4971/94/8409-0016$3.00/0 2954 MATERIALS AND METHODS Patient's description. In December 1991, a IO-year-old girl presented with anemia and thrombocytopenia. The hemoglobin concentration was 5.7 g/dL; the red blood cell count, 1.67 TiL; the white blood cell count, 8.4 G/L; and the platelet count, 20 GiL. BM examination showed myelodysplasia with 16% blast cells and BM mastocytosis (Fig 1). The diagnosis of a MDS (French-American-British [FAB] subgroup: refractory anemia with an excess of blast cells [RAEB]) was established. After transition to AML [FAB: M2, 32% blast cells, karyotype: t(8; l)(q22,q21),de1(5)(q13,q23)] the patient was treated with chemotherapy (AML-BFM 83 protocol)Ib and CR was achieved. However, BM mastocytosis persisted. In September 1992, the patient was still in CR and received allogeneic BMT (1.1 X IOx BM mononuclear cells [MNCsIkg body weight) from her HLA-identical sister. The conditioning regimen consisted of 12 mg/ kg busulfan, 40 mgkg etoposide, and 120 m a g cyclophosphamide. Methotrexate and cyclosporin-A were administered as graft-versushost disease (GVHD) prophylaxis. Because of late engraftment and acute GVHD, grade I1 (day 26 after BMT), the patient received prednisolon and anti-interleukin-2 (anti-IL-2; 0.15 to 0.3 mg/kg/d), high-dose lgs and recombinant human IL-3. On day 121, complete hematopoietic recovery was noted and successful engraftment of all cell lineages (except MCs) was evidenced by vWF.VNTR-PCR. During the whole observation period, mastocytosis persisted. Five hundred days after BMT, all cell lineages displayed donor genotype and the patient was still in CR. Monoclonal antibodies (MoAbs). The following MoAbs were used to analyze and purify MNCsubpopulations. The phycoerythrinor fluorescein isothiocyanate-conjugated MoAbs UCHTl (CD3), MT310 (CD4).DK25(CD8). TUK2 (CD14), and HD37 (CD19) were purchased from Dakopatts (Glostrup, Denmark) and MoAb 8G12 (CD34) was purchased from Becton Dickinson (Sunnyvale, CA). The anti-c-kit MoAb YB5.B8 (CD1 17)" was kindly provided by Leonie Ashman (University of Adelaide, Australia). Flow-cytometric analysisand cell sorting. Peripheral blood (PB) Blood, Vol 84. No 9 (November l ) , 1994: pp 2954-2959 ORIGIN OF HUMANMAST CELLS 2955 Fig l. BM MCs on day 88 after BMT Giemsa staining. and BM MNCs were separatedby density centrifugation (Nycoprep; Nycomed, Oslo, Norway). MNCs were prepared on days 78 (PB), 88 (BM),126(BM), 133 (PB), 198(BM),and 494 (BM) after BMT and incubated with the appropriately diluted MoAbs. Flowcytometric analysis and cell sorting were performed on a FACStar Plus(BectonDickinson,MountainView,CA) as previously described.” MNC wereenriched for CD3+T cells, CD4+T cells, CD8’ T cells, CD19’ B cells, CD34+ precursor cells, and CD117+ MCs. In case of sorting for MCs, double staining with MoAbs YBS.B8 ( 0 1 1 7 , c-kit) and 8G12 (CD34) was used to enrich for CD117’/ CD34- cells (exclusion of c-kit+ precursor cell subsets). The purity of each sort was assessed by reanalysis and usually ranged between 96% and 99.5%. The presence of MCs in the c-kit+ cell fractions was confirmed by Giemsa staining of cytospin preparations as well as by measurement of histamine in cell lysates. Histaminewas measured by a radioimmunoassay (Immunotech, Marseille, France) as described.’~‘~ PCR analysis of a VNTR region within the vWF gene in highly enriched leukocyte subsets. The vWF gene contains a polymorphic region of ATCT repeats (VNTR) within intron 40. This region was shown to vary in length between different individuals.” Analysis of the vWF gene has been used for carrier detection and prenatal diagnosis in vWF disease”.” and more recently for the investigation of engrafted hematopoietic cells after allogeneic BM transplantation.” In this study, the vWF.VNTR-PCR was used to analyze the genotype (donor v recipient) of individual cell lineages in a patient after allogeneic BMT. The PCR technique was applied on highly enriched CD1 17+/CD34- BM MCs (days 88, 126, 198, and 494 after BMT), CD34+ BM precursor cells (days 72 and 494). CD3’ BM T cells (days 126 and 198), CD14’ BM cells (day 126). isolated BM MNCs (day 494), isolated BM polymorphonuclear cells (PMNCs) (days 198 and 494). CD3+ PB T cells (day 78), CD4’ PB T cells (day 133), CD8+ PB T cells (day 133), CD4+/CD8+ PB T cells (day 133), CD19+ PB B cells (day 78), isolated PB MNCs (day 133), isolated PB PMNCs (day 133) as well as on citrated whole blood (days S9 and 64). After sorting, cell fractions were washed once in phosphate-buffered saline, resuspended to a final concentration of 500 cells per pL and frozen at -20°C. Cellular DNA (PB, MNCs, PMNCs, and sorted cell fractions) was obtained by thawing and boiling for 10 minutes, followed by centrifugation at 12,OOOg (for 10minutes). The supernatants were collected and stored at -20°C. The PCR was performed as described by Peake et al.”The PCR amplification products were analyzed by electrophoresis on vertical 8% polyacrylamide (PAA) gels in 1 X TBE buffer (90 mmoliL TRIS, 90 mmoVL boric acid, 1.25 mmol/L EDTA) and stained with ethidium bromide. The sensitivity of the vWF.VNTR-PCR was determined by dilution experiments using DNA samples from two healthy individuals whose VNTR polymorphism could be distinguished by PCR. Isolated PBMNCsof one inividual weremixedwith l%, 2%, S%, lo%, 20%, 30%,40%, SO%, 60%, 70%, 80%, 90%,95%. 98%, and 99% MNCs from the other individual. Each aliquotof IO’ cells was as boiledandtheSupernatantswereusedforPCRamplification described above. The PAA gel electrophoresisof the PCR products showed amplification fragments of both genotypes when at least 10% MNCs of one and 90% MNCs of the other individual were present. Below 10%. a reliable detection of the smaller MNC population was not possible. RESULTS Isolation and purity of leukocyte populations. The purity of the FACS-sorted cell fractions was analyzed by morphol- ogy, flowcytometry, andbymeasuring cellularhistamine levels. Reanalysis of sorted (c-kit+/CD34-) MCs with YB5.B8 MoAb revealed a purity of >95% (Fig 2). h addition, the isolated MCs were more than 95% pure as assessed by Giemsa staining. A significant contamination of purified MCswith CD3+ T cells (<l%), CD34’precursor cells (< 1 %) or CD14+ monocytes (<1%) could be excluded by flow-cytometric examination. Selective enrichment of MCs was also analyzedbymeasurement of cellularhistamine. 2956 FODINGER ET AL 10:F1401038 I ~ B R1 CD34 1 FLl-H\FLi-Hei&t ---> 10rF1401040 10:F1401041 c I r\4 D C R2 The calculated amounts of cellular histamine in the pure MC populations ranged between 0.6 and 25 pg per cell, whereas in other cell fractions (CD3' T cells, CD19+ B cells, CD14+ monocytes, and CD34+ precursor cells) the histamine levels were below the detection limit. Approximately 1 to 2 X lo4 BM MCs were recovered from MNC specimens (percentage of MCs in primary MNC samples: 0.1% to 0.3%). The viability of the cells was more than 70% as assessed by trypan blue exclusion. In each MC preparation, 5.000 cells were used for PCR analysis and 5,000 cells for cytospin preparation. Remaining cells were used for control experiments. The punty of the CD34+ BM precursor cells was 94% to 98%; of CD3+ T cells, 98% to 99%; of CD4+ T cells, 99%; of CD8+ T cells, 98%; of CD19' B cells, 98%; of CD14' PB monocytes, 95% to 98%. Analysis of vWF.VhTR on whole blood cells before BMT. 2957 ORIGIN OF HUMAN MAST CELLS A DISCUSSION l 2 3 4 5 6 7 8 9 1 0 90 b B Fig 3. Comparison of BM MCs genotype with various cell fractions as assessed by PAA gel electrophoresis of PCR amplification products. (A) Recipient genotype of BM MCs on day 88 after BMT is shown. PCR was performed with donor's PB (lane 2). recipient's PB before BMT (lane 3). recipient's PB on day 59 after BMT (lane 4). CD3' T cells (day 78, lane 5). CD19' B cells (day 78, lane 6), CD14' monocytes (day 126, lane 7 ) . CD34' progenitor cells (day 72, lane 8). and CD117+/c-kit' MCs (day 88, lane 9). Markers (lanes 1, 10): Msp Idigested plasmid pBR322 (Clontech, Palo Alto, CA). (B) Donor genotype of MCs on day 198 after BMT is shown: donor's PB (lane 2). recipient's P6 before BMT (lane 3), recipient's PB after BM (day 198, lane 41, BM MNC (day 198, lane 5). BM PMNC (day 198, lane 6). and BM MCs (day 198,lane7). Markers (lanes 1,8): MspI-digested plasmid pBR322. In a first set of experiments, we amplified DNA extracted fromthe recipient's andthe donor's wholebloodbefore BMT. Gel electrophoresis of the PCR products showed two different banding patterns in the two individuals (Fig 3) representing the donor's and recipient's genotype. At1clIwi.v of VWF.VNTR on highly cwrichd RM MCs. To determine the genotype and origin ofBMMCs and other leukocyte subsets on various days after BMT, fractionated and unfractionated PB and BM cells of thepatient were analyzed by vWF.VNTRPCR.Highly enriched BM MCs were analyzed on days 88, 126. 198. and 494 (Table I ) . On days 88 and 126, MCs displayed recipient genotype in PCR analyses (Fig 3A). However, a consecutive switch in the genotype was observed. and on days 198and 494, MCs exhibited donor genotype (Fig 3B). At1crIwi.v of vWF. VNTR it1 P R crncl BM leukocyte suhsets. In contrast withpurifiedMCs,all other leukocyte subsets showed donor origin in vWF.VNTR PCR experiments during theobservation period. On days S9 and64, analysis of the patient's whole blood displayed donor genotype, suggesting successful engraftment. On days 78 and 133. PB MNC and PMNC as well a s purified (sorted)T cells, B cells. and monocytes were analyzed. VNTR-PCR showed donor origin of all circulating leukocyte subsets tested (data not shown). BM cells and subfractions were analyzed on days 72, 88, 126,198,and 494 after BMT. PCR analysis ofDNA extracted from pure BM precursor cells (CD34'k-kit' cells) on days 72 and 494 showed donor genotype. BM-derived (CD14') monocytes and (CD3 + ) T cells were analyzed on days 126 and 198 and displayed donor genotype. PCR data onBM cells are summarized in Table I . Although it iswell established thatMCsbelongto the hematopoietic cell system,'.I3little is knownabout origin and differentiation pathways of cells that become committed to and differentiate into mature MCs. Studies using clonal cell assays and MC growth factor (MGF) (c-kit ligand) have shown origin of human MCs from multipotent colony-forming precursor cells in vitro.".I5 However, confirmation for the situation in vivo has not been provided so far. In the present study, origin of human MCs from transplanted stem cells in vivo was investigated by vWF.VNTR-PCR. MCs were purified from BMbyuse of anti-c-kit MoAb YBS.B8 and analyzed on various days after BMT. Unexpectedly, on days 88 and 126 after BMT, PCR analysis showed recipient origin of MCs. However, on days 198 and 494 after BMT, a switch to donor genotype was evidenced. Like all other hematopoietic cells, MCs develop from immature, uncommitted hematopoietic progenitor cells. In the case of MCs, it is unknown whether the BM remains the constant source of precursor cells throughout life or whether these cells develop from a local pool of precursor cells in extramedullary tissues. Our data support the concept that MCs are constantly replenished from BM precursor cells, although one has to take into account that in contrast with the situation in normal tissue, MCs were obtained and analyzed shortly after BMT (a highly abnormal situation). Moreover, these MCs could onlybe analyzed in BM specimens, but not in other organs or tissues, and although the BMof the donor did not contain MCs, the donor MCs developed in a patient who had persistent BM mastocytosis. Nevertheless, our data provide the first evidence that BM stem cells give risetohumanMCs in vivo.However, further studies are required to elucidate whether this canbe translated to all MC systems in humans. It is noteworthy in this regard, that in MC-deficient WIW' mice, transplanted hematopoietic precursor cells (obtained from normal littermates) gave rise to MCs in various extramedullary organs.'3.23 In contrast with other hematopoietic cells, MCsneed a longer time to develop from their precursor cells and (as mature cells) exhibit prolonged survival. Development and differentiation of human MCs in vitro (with c-kit ligand as Table 1. Genotype of Sorted BMMNC Fractions as Assessed by vWF.VNTR-PCR Days After BMT 72 88 126 198 494 CD34'l CD117' Precursors CD14' CD117'1 CD34 MC Donor - - Recipient Donor Recipient Donor Donor - CD3' Lymphocytes Granulocytes Monocytes - - - Donor Donor Donor Donor - - IPMNCI - BM MNC fractions were obtained by cell sorting with MoAbs. The purity ofthe isolated cells ranged between 97% and 99.5%. The genotype(donor v recipient) of the MNC fractions was analyzed by vWF.VNTR-PCR as described in Materials and Methods. 2958 FODINGER ET AL growthfactor)takesabout 4 to 10 ~ e e k s . ’ ~ * In ’ this ~ , ~ ~ , ~ ~ 10. Gordon RG,Burd PR, Galli SJ: Mast cells as a source of multifunctional cytokines. Immunol Today 11:458, 1990 study, the genotype ofMCs had not switched from recipient I 1. Gordon JR, Galli SJ: Mast cells as a source of both preformed todonortypebeforeday 180 after BMT, whereas donor and immunologically inducable TNF-alphdcachectin. Nature origin of othercelltypeswasidentified earlier (day 50). 346:274, 1990 These observations suggest that in vivo differentiation of 12. Kmhenbaum AS, Goff JP, Kessler SJ, Mican JM, Zsebo M. MCs from their precursor cells is a prolonged process as Metcalfe DD: Effect of L-3 and stem cell factor on the appearence compared withgranulocyte, monocyte, or lymphocyte differof human basophils and mast cells from CD34’ pluripotent progenientiation. Alternatively, the prolonged presence of recipient tor cells. J Immunol 148:772, 1992 MCs could have inhibited rapid growth of donor MCs (nega13. Kitamura Y, Yokoyama M, Matsuda H, Ohno T: Spleen coltive inhibition). ony-forming cell as common precursor for tissue mast cells and granulocytes. Nature 291:159, 1981 A number of studies have suggested an association be14. Agis H, Willheim M, Sperr WR, Wilfing A, Kromer E, tween BM mastocytosis andmyelodysplastic or myeloprolifKabrna E, Spanbiichl E, Strobl H, Geissler K, Spittler A, Boltzerativesyndromes.26-3’In our patient, the initial diagnosis Nitulescu G, Majdic 0, Lechner K, Valent P: Monocytes do not was RAEB associated with BM mastocytosis. Interestingly, make mast cells when cultered in the presence of SCF. J Immunol BM mastocytosis persisted throughout the observation pe151:4221, 1993 riod, even when donor stem cells were the apparent source 15. Kirshenbaum AS, Kessler SW, Goff JP, Metcalfe DD: Demof MCs. Possibly, MC proliferationin BM tissuewas a onstration of the origin of human mast cells from CD34’bone marreactive process. The hypothesis of a reactive MC process row progenitor cells. J Immunol 146:1410, 1991 would be in line with the mature morphology of MCs in BM 16. Sartori PC, Taylor MH, Stevens MC, Darbyshire PJ, Mann specimens and with the observation that the MC genotype JR: Treatment of childhood acute myeloid leukaemia using the B F ” 83 protocol. Med Pediatr Oncol 2123, 1993 switched from recipient to donor. 17. Mayrhofer G, Gadd SJ, Spargo LDJ, Ashman LK: Specificity To confirm the hypothesis of a reactive process and to of a mouse monoclonal antibody raised against acute myeloid cells excludethe recurrence of clonal disease of donor origin for mast cells in human mucosal and connective tissues. Immunol after BMT, which has been described for various types of Cell Biol 65:241, 1987 leukemias,32s33 genetic studiesare currently under way. 18. Fritsch G, Buchinger P, Printz D, Fink FM, Mann G, Peters For most hematopoietic cell lineages donor origin after C, Wagner T, Adler A, Gadner H: Rapid discrimination of early BMT has been d e s ~ r i b e d .Origin ~ ~ , ~ of ~ MCs from early preCD34+ myeloid progenitors using CD45-RA analysis. Blood cursor cells has long been a matter of intensive discussions. 81:2301, 1993 Our data provide the first evidence that human MCs derive 19. Valent P, Spanblochl E, Sperr W, Sillaber C, Agis H, Strobl in vivo from the earliest (transplantable) hematopoietic proH, Zsebo KM, Geissler K, Bettelheim P, Lechner K: Induction of differentiation of human mast cells from bone marrow andperipheral genitor cells. The development of human MCs in vivo from blood mononuclear cells by recombinant human stem cell factor their precursor cells seems to be a prolonged process. (SCF)/kit ligand (KL) in long term culture. Blood 80:2237, 1992 20. Peake IR, Bowen D, Bignell P, Lidell MB, Sadler JE, Standen ACKNOWLEDGMENT G, Bloom AL: Family studies and prenatal diagnosis in severe von We thank P. Buchinger, D. Printz, H. Semper, B. Keck, 0. Haas, Willebrands disease by polymerase chain reaction amplification of M. Veitl, and H.C. Bankl for excellent technical assistance. a variable number of tandem repeat region of the von Willebrand factor gene. Blood 76:555, 1990 REFERENCES 21. Mannhalter C, Kyrle PA, Brenner B, Lechner K: Rapid neonatal diagnosis of type IIB von Willebrand disease using the poly1. Galli SJ: New concepts about the mast cells. N Engl J Med 328:257, 1993 merase chain reaction. Blood 77:2539, 1991 22. Gaiger A, Mannhalter C, Hinterberger W, Haas 0, Marosi C, 2. Schwartz LB, Huff TF: Mast cells, in Crystal RG, West JB Kier P, Eichinger S, Funovic M, Lechner K: Detection of en(eds): The Lung. New York, NY, Raven, 1991, pp 601-16 graftment and mixed chimerism following bone marrow transplanta3. Valent P, Ashman LK, Hinterberger W, Eckersbexger F, Majtion using PCR amplification of a highly variable region-variable dic 0, Lechner K, Bettelheim P: Mast cell typing: Demonstration number of tandem repeats (VNTR) in the von Willebrand gene. Ann of a distinct hematopoietic cell type and evidence for immunophenoHematol 63:227, 1991 typic relationship to mononuclear phagocytes. Blood 73:1778, 1989 23. Qiu F, Ray P, Brown K, Barker PE, Jhanwar S, Ruddle FH, 4. Valent P, Bettelheim P Cell surface structures on human basoBesmer P: Primary structure of c-kit: Relationship with the CSF-l/ phils and mast cells: Biochemical and functional characterization. PDGF receptor kinase family. EMBO J 7:1003, 1988 Adv Immunol 52:333, 1992 24. Mitsui H, Furitsu T, Dvorak AM, bani AMA, Schwartz LB, 5. Galli SJ: Biology of disease. New insights into “The riddle of Inagaki N, Takei M, Ishizaka K, Zsebo KM, Gillis S , Ishizaka T: the mast cell”: Microenviromental regulation of mast cell developDevelopment of human mast cells from umbilical cord blood cells ment and phenotypic hterogeneity. Lab Invest 62:5, 1990 by recombinant human and murine stem cell factor c-kit ligand. Proc 6. Valent P, Sillaber C, Bettelheim P: The growth and differentiaNatl Acad Sci USA 90:735, 1993 tion of mast cells. Prog Growth Factor Res 3:27, 1991 25. Irani AM, Nilsson G, Miettinen U, Craig S S , Ashman LK, 7. Denburg JA: Basophil and mast cell lineages in vitro and in Ishizaka T, Zsebo KM, Schwartz LB: Recombinant human stem cell vivo. Blood 792346, 1992 factor stimulates differentiation of human mast cells from dispersed 8. Johnston SL, Holgate ST: Cellular and chemical mediatorsfetal liver cells. Blood 80:3009, 1992 Their roles in allergic diseases. Cum Opin Immunol 2:513, 1990 26. Horny HP, Ruck M, Wehrmann M, Kaiserling E: Blood find9. Serafin WE, Austen KF: Mediators of immediate hypersensiings in generalized mastocytosis: Evidence of frequent simultaneous tivity reactions. N Engl J Med 317:30, 1987 ORIGIN OF HUMAN MAST CELLS occurrence of myeloproliferative disorders. Br J Haematol 76:186, 1990 27. Lewis JP, Welborn JL, Meyers FJ, LevyNB, Roschak T: Mast cell disease followed by leukemia with clonal evolution. Leuk Res 11:769,1987 , RG: Sig28. Travis WD, Li CY, Yam LT, Bergstralh €3Swee nificance of systemic mast cell disease with associated hematologic disorders. Cancer 62:965, 1988 T, Kandels S, Radaszkiewicz T, UllrichA, 29. vonRuden Wagner EF: Development of a lethal mast cell disease in mice reconstituted with bone marrow cells expressing the v-erbB oncogene. Blood 79:3145, 1992 30. Webb TA, Li CY, Yam LT: Systemic mast cell disease: A clinical and hematopathologic study of 26 cases. Cancer 49:927, 1982 2959 31. Prokicimer M, Polliack A: Increased bone marrow mast cells in preleukemic syndromes, acute leukemia, and lymphoproliferative disorders. Am J Clin Pathol 75:34, 1981 32. Boyd CN, Ramberg RC, Thomas ED: The incidence of recurrence of leukemia in donor cells after allogeneic bone marrow transplantation. Leuk Res 62333, 1982 33. Smith JL, Heerema NA, Provisor A: Leukaemic transformation of engrafted bone marrow cells. Br J Haematol 60:415, 1985 34. Ginsburg D, Antin JH, Smith BR, Orkin SH, Rappeport JM: Origin of cell populations after bone marrow transplantation. Analysis using DNA sequence polymorphisms. J Clin Invest 75596, 1985 35. Ault KA, Antin JH, Ginsburg D, Orkin SH, Rappeport JM, Keohan ML, Martin P, Smith BR: Phenotype of recovering lymphoid cell populations after marrow transplantation. J Exp Med 161:1483, 1985
© Copyright 2026