Molecular Basis of the Kell (Kl) Phenotype
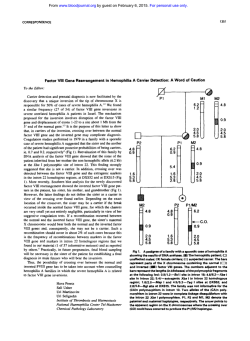
From www.bloodjournal.org by guest on February 6, 2015. For personal use only. RAPID COMMUNICATION Molecular Basis of the Kell ( K l ) Phenotype By Soohee Lee, Xu Wu, Marion Reid, Teresa Zelinski, and Colvin Redman K1 (K, Kell) is a strong immunogen; its antibodies can cause severe reactions if incompatible blood is transfused and may cause hemolytic disease ofthe newborn in sensitized mothers. K1 is a member of the Kell blood group system, which is complex, containing over 20 different antigens. Some of the antigens are organized in allelic pairs of high and low prevalence whereas others are independently expressed. K1, which is present in 9% of the population, is antithetical to the high-prevalence K2 (k) antigen. We have determined the molecular basis of the K1/K2 polymorphism by sequencing the 19 exons of the Kell gene (KEL) of a Kl/Kl person. Polymerase chain reaction was performed on genomic DNA isolated fromperipheral blood and the ampliiied products were either directly sequenced or subclonedand sequenced. Com- parisonsof Kl/Kl and K2/K2 DNA showed a C to T base substitution in exon 6 that predicts a threonine to methionine change at amino acid residue 193. This amino acid substitution occurs at aconsensus N-glycosylation site (Asn. X. Thr) and probably prevents N-glycosylation, leading to a change in phenotype. The C to T substitution creates a Bsm I restriction enzyme site, which was tested in 42 different samples to confirm that this base change identifies the K11 K1 genotype. This test differentiates genotypes, Kl/Kl, K2/ K 2 , and the K l / U heterozygote and should prove useful in the prenatal diagnosis of K1-related hemolytic disease ofthe newborn. 0 1995 by The American Society of Hematology. T samples. Among blood groups stimulated by alloimmunization, K1 (K) isprobably second onlyto Rh(D) in the Rh system as an immunogen. Molecular cloning established that Kell blood group antigens are carried on a 93-kD type I1 glycoprotein." Kell protein has a short, 46 amino acid, N-terminal domainin the cytoplasm and a large C-terminal portion, of 665 amino acids, on theexternal surface of the RBC. All of the carbohydrates are N-linked" and are probably located in 5 sites at asparagines 93, 115, 191, 345, and 627. Early biochemical studies suggested thatKell antigens reside on a protein whose conformation is largely dependent on disulfide bonds.'' Kell protein has 16 cysteine residues, 1 in the transmembrane region and 15 in the external portion.'o Reduction of RBCs by sulfhydryl reagents results in loss of Kell antigens and exposure of some neo-epitopes."," The molecular basis of the different Kell phenotypes has not been determined. Expression of Kell protein in transfected cells using a wild-type cDNA resulted in the detection of the high-prevalence antigens K2, K7, and K14 but not of the low-prevalence antigens K1 or K3.I3 This finding indicates that several antigens may be carried on a single protein and that low-prevalence antigens probably reside on variant proteins. Having studied the structure of the Kell gene and identified the 19 exons that encode Kell protein,I4 we have now determined the molecular basis of the KUK2 polymorphism by sequencing the exons of Kl/K1 DNA and comparing them to K2/K2 sequences. A base substitution in exon 6 of the KUK1 genotype predicts an amino acid change. This base substitution creates a restriction enzyme site that was tested in more than 40 different samples to confirm that the base substitution identifies the KllKl genotype. HE KELL BLOOD GROUP system is important in transfusion medicine because the antibodies can cause severe reactions to transfusion of incompatible blood and hemolytic disease in newborn infants. The Kell system is complex andmorethan 20 different Kell-related antigens have been identified. Kell antigens appear to be encoded in five sets of antithetical paired alleles expressing high- and low-prevalence antigens. Thus, K1 (K) and K2 (k) are products of alleles, as are K3 (Kp"), K4 (Kpb), and K21 (Kp'); K6 (Js") and K7 (Jsb); K17 and K l I ; andK24 and K14. However, a number of high-prevalence antigens, such as K12, K13,K18, and K22, are independently expressed. These relationships and their place in the Kell system have been established through the years by serologic analyses of informative families.'.' A recently developed immunologic test, monoclonal antibody-specific immobilization of erythrocyte antigens (MAIEA), which usesmonoclonal antibodies to different Kell antigens, indicates that different antigens occur in spatially distinct regions of the glycoprotein. Thus, Kl/K2 and K6/K7are close together, whereas K3/K4 epitope is in a different location and K18 is in yet another protein domaim6 Inheritance is autosomal and codominant and KEL has been mapped to chromosome 7q33.'~' An antibody to K1, named Kell after its propositus, reacts with approximately 9% of randomredblood cell (RBC) From the Lindsley F. Kimball Research Institute of the New York Blood Center, New York, NY;andtheRh Laboratory, Department of Pediatrics, University of Manitoba, Winnipeg,Manitoba, Canada. Submitted October 17, 1994; accepted November 16, 1994. Supported in part by National Institutes of Health Grant No. HL35841 and the Starr Foundation (to C.R.), and by MRC Grant No. MA3391 and the Children's Hospital Research Foundation (to T.Z.). Address reprint requests to Colvin Redman, PhD, The New York Blood Center, 310 E 67 St, New York, NY 10021. The publication costs of this article were defrayed in part by page charge payment. This article must therefore be hereby marked "advertisement" in accordance with 18 U.S.C. section 1734 solely to indicate this fact. 0 1445 by The American Society of Hematology. 0006-4971/95/8504-0033$3.00/0 912 MATERIALS AND METHODS DNA preparation. DNAwas prepared from peripheral blood obtained from 42 persons whose Kell phenotypes have been determined serologically. DNA was prepared either from 1 to 5 mL of whole blood collected with anticoagulants or, when RBCs were removed by centrifugation at 1,OOOg for IO minutes, from the resulting buffy coat. In both cases, the procedure described by John et a1" to prepare DNA was used. Seven of the DNA samples were Blood, Vol 85,No 4 (February 15). 1995: pp 912-916 From www.bloodjournal.org by guest on February 6, 2015. For personal use only. KELL ( K I ) PHENOTYPE 913 obtained from Canadian Hutterites and serologic studies of these families indicated that they were homozygous for either K1 or K2. In these samples DNA was isolated as described.'6 Approval for these studies was obtained from the Institutional Review Board of the NewYork Blood Center and the HumanEthics Committee of the University of Manitoba. Persons were informed that samples were obtained for research purposes and that their privacy would be protected. Polymerase chain reaction(PCR). The following denaturation, annealing, and polymerization steps were performed in an automated thermocycler (Minicycler; MJ Research Inc. Watertown, MA): an initial cycle of 94°C for 3 minutes, 62°C for 1 minute, and 72°C for 30 seconds; in cycles 2 through 30, the conditions were 94°C for 30 seconds, 62°C for 30 seconds, and 72°C for 30 seconds; in the last cycle, the polymerization step at 72°C was extended to 10 minutes. The final concentrations of reagents were 50 mmoVL KCI, IO mmoVL Tris-HC1 (pH 9.0), 3 mmoVL MgCI2, 350 nmol/L of each primer, 200 pmoVL of each dNTP, 0.1% Triton-X100, 100 to 200 ng genomic DNA, and 2.5 U of taq polymerase in a final volume of 100 pL. The "hot start" method using Ampliwax from Perkin Elmer (Branchburg, NJ) was used. The amplified PCRproducts were separated by electrophoresis on 0.8% agarose gels and detected by ethidium bromide staining. DNA sequencing. The PCR products, separated by electrophoresis on low 2.8% melting agarose, were eluted, ligated to pT7Blue (R) plasmid vector, and transformed in DH5aF' strain Escherichia coli. Plasmid DNA was prepared in a small scale by the alkali lysis method andpurified with a Quick Spin (Sephadex G50) column. Standard molecular biology procedures were used." DNA sequencing was performed by an automated system (Model 373A, Version 1.2.0; Applied Biosystems, Foster City, CA). Restriction enzyme digestion. Bsrn I was added directly tothe final PCR reaction mixture. The PCR mixture (10 pL) was optimized for Bsrn I digestion by adding 2 pL of 35 mmol/L MgCI,, 1 pL of 10 mmom mercaptoethanol or 10 mmoVL D m , 1 pL of 1OX Bsm I buffer, 4 pL of water, and 2 pL of 5 U/mL Bsrn I. Incubations were performed for 90 minutes at 65°C. The DNA in the reaction mixture was analyzed by electrophoresis in 0.8% agarose. Otherreagents. Taq DNA polymerase and dNTPs were purchased from Promega (Madison, WI). X-Gal was from Appligene Inc (Pleasanton, CA). The DNA I-kb ladder standards, DHSaF' strain E coli competent cells, and low melting agarose were from Bethesda Research Laboratories (Gaithesburg, MD). T4 DNA ligase and Bsrn I were from New England Biolabs (Beverly, MA).pT7 blue (R) plasmid vector was from Novagen (Madison, WI) and Quick Spin Column (G-50 Sephadex) for DNA purification was from Boehringer Mannheim (Indianapolis, IN). RESULTS Comparison of K1 and K2 DNA sequences. Nine pairs of forward and reverse primers were used to amplify the 19 KEL exons. The sequences of the primers and the target exons are shown in Table 1. Genomic DNA from a homozygous K1 person was used as template DNA. In all cases, single products ranging in sizes from 0.48 to 1.5 kb were obtained (Fig 1). All of the PCR products were sequenced and compared with that of K2 The sequence of K1 DNA encoded identical amino acids to those of K2 DNA, except for a single-base change in a PCR product that spans exons 5 and 6. In this PCR product, which was 740 bp in length, there was a single cytosine (C) to thymine (T) substitution, predicting a threonine to methionine change at a consensus N-glycosylation site (Asn. X. Thr).This difference between K1 and K2 occurs in exon 6 (Fig 2). Because this was the only difference between K1 and K2 encoding changes in amino acids, it suggested that the threonine to methionine change would prevent N-glycosylation at asparagine 191 in proteins expressing K1, thus identifying the K1/ K2 polymorphism. Confirmation of KUK2 polymorphism by Bsm I analysis. The C to T substitution creates a new restriction enzyme site with specificity for Bsm I. To confirm that this base change identifies the K1 genotype, this region was analyzed in 42 Table 1. Primers Used in PCR of KEL Exons PCR 1 2 3 4 5 6 7 8 9 Primers 5'-CAG TCC TCC GAA TCA GCT CCT AGA-3' 5"CTC l T G GCT CCA GAG AGT TCC CAT-3' 5"GAA GGT GGG GAC CAA AGT GAG GAA-3' 5'-ACA GGG TTT GGA GCA GTC ATG GTC-3' 5 " l T AGT CCT CAC TCC CAT GCT TCC-3' 5"TAT CAC ACA GGT GTC CTC TCT TCC-3' 5"ATA l T C CCC ACC TCC CCA CAC CTG-3' 5'-ATC TAC GGT GCT CAG GCTCTC CTC-3' 5"GGA AGC ATG GGA GTG AGG ACT AAA-3' 5"TGG CAT CCA TGG TAC CTC ATG GAA-3' 5"GAG GCT TTT 11 GAA ACC TGA-3' CCA GGA 5"lTC CCC AGC CAC CTG CCA TCT CAT-3' AAG TTT CAGTCC GGTAAG CTG-3' 14, 13, 5"CCC 5"GGG C l T A l TTGA CCC CCA GAA TCT-3' 5"CCT AAT CCC ATG TGG CCT GCC TGT-3' 17, 16, 15, 5"CAG TGA GGA CAT CTG CAG AAG AGG-3' GGA 5"TCC TGT CCC TCC CCC 19*l T C AAT-3' 5"GGG CGG AAG CCA AGT GCC AGC TTT T-3' Approximate Size of PCR Product (kb) Target Exons 1, 2* 0.48 2*, 3, 4 1.o 5, 6 0.74 7. 8. 9 0.8 10 1.2 1.3 12, 14*, 15 1.4 18 1.5 0.33 The first primer is the forward sequence and the second is the antisense primer. The 2 G bases at the 5' end of antisense primer of PCR 9 are not in the gene and were added to create an Smal site for another purpose. The PCR products of exons 1 (PCR 1) and 19 (PCR g) contain the entire translated regions. Exon 2 was spanned by overlapping PCR products (PCR f and 2) and exon 14 was covered by PCR7. * PCR products that did not cover the entire exon. From www.bloodjournal.org by guest on February 6, 2015. For personal use only. LEE ET AL 914 KVK2 heterozygotes (lanes 6 and 7) can be easily distinguished from the K1 homozygotes because the 740-bp band of KUK2 is more pronounced than its split products of 540 and 200 bp. 1 2 3 4 5 6 7 8 91011 DISCUSSION 4 1.6 Kb 4 1.OKb 4 0.5 Kb Fig 1. PCR amplification of KEL exons. Genomic K1 DNA was amplified with 9 sets of primers that cover the open reading frames of the KEL exons. The PCR productswere separated by electrophoresis on 0.8% agarose gels and stained with ethidium bromide. The primers used and the spanning regions are described in Table 1. Lanes 1 and 11 are l-kb DNA ladder standards; lanes 2 through 10 contain PCR products of PCR 1, 2,3, 4, 5, 6, 7, 8, and 9, respectively. different persons of known KI/K2 phenotype. Included in these samples were DNA from 7 Hutterites, because family studies indicated their Kell genotypes. All other samples were from unrelated persons. The 740-bp PCR product that spans exons 5 and 6 (PCR 3, Table 1) was treated with Bsm 1. A KI/KI genotype should yield two fragments, of 540 and 200 bp; the K2/K2 genotype will yield the uncut 740bp PCR product and KI/K2 heterozygotes should yield 3 fragments of 740, 540, and 200 bp. Of the 42 DNA samples tested, 12 were either K I or K2 homozygotes, 6 were KI/K2 heterozygotes, and 24 were KI , K2 phenotypes but contained low-prevalence or rare Kell phenotypes. These phenotypes includedK3,K6,KIO, KO (null), a K14/K24 heterozygote, and a McLeod phenotype. In 40 of the 42 cases, the Bsm I genotyping agreed with the Kell phenotypes that were determined by serologic analysis of RBCs. In 2 cases, genotyping identified one of the samples as K2/K2 and the other as a KI/K2 heterozygote and these 2 samples were serologically identified as having “weak” K1 phenotypes. None of the other low-prevalence or rare Kell phenotypes listed above had the C to T base substitution in exon 6, indicating that this change is specific for the KI/K2 polymorphism. Examples of selected results are shown in Fig 3. In some cases (lanes 3, 4, and17). the K1 homozygotes, in addition to showing bands at 540 and 200 bp, contained a faint bandat 740 bp caused by incomplete digestion. The Approximately 9% of the population has the K1 RBC phenotype and antibodies to K1 are developed in about 5% of persons receiving a single unit of incompatible blood.IK Hemolytic disease of the newborn (HDN) is usually associated with maternal alloimmunization to Rh(D), but K1 incompatibilities can also cause severe HDN.’9-24Determination of the molecular basis of the KVK2 polymorphisms will allow genotyping from DNA samples and should prove useful in prenatal diagnosis. The most prevalent Kell phenotype is K:-1,2,-3,4,-6, 7,9,11,12,14,18,19,22. We have, in a previous study, defined the 19 exons of the KEL gene of a person with common Kell phenotype, but the molecular basis for the K1 genotype was notknown.I4 Polymorphic differences are caused by differences in amino acid sequence that may be caused by point mutations, gene rearrangements, or alternative splicing. To determine the molecular basis of KI/K2 polymorphism, we designed a series of primers that would amplify the 19 exons of KEL and compared the DNA sequences of Kl/Kl and K2/K2 DNA. The only base change that would encode a different amino acid was found in exon 6 and changed a threonine to a methionine at a consensus N-glycosylation motif (Asn. X. Thr “* Met). This change would prevent Nlinked glycosylation at this site. Based on the amino acid sequence of Kell protein of common phenotype, there are 6 possible N-glycosylation sites at asparagine residues 93, 1 15, 191, 345, 627, and 724. However, the asparagine at position 724 is probably not glycosylated because it ispart of a sequence Asn. Pro. Ser and the presence of proline between asparagine and serinehheonine inhibits N-glycosylation.2s Changing threonine to methionine at position 193 would prevent glycosylation at asparagine 191. Thus, K1 protein would be composed of 4 instead of 5 carbohydrate moieties. Assuming an average molecular size of an N-linked oligosaccharide to be about 2.5 kD, the K1 protein should be 90.5 kD as compared with the 93-kD proteinthat carries the common Kell phenotypes.” This difference in size is difficult to detect by sodium dodecyl sulfate-polyacrylamide gel electrophoresis because glycoproteins tend to migrate as diffuse K2 185 K1 - TrpThrser TQQ ACTTCC Leu Asn Phe A m APO TM Leu Arg LOU LeuYetser TTA M C TTT M C ’X4 ACQ CTQ AOA CTTCTQ ATG AGT TQQ ACTTCC Trp Thr Ser TTA M C 19s l m M C ‘X4 AT0 CTQ AOA CTTCTQ ATG AQT Leu Asn Phe ASn APO #at Leu Arp Leu LeuYetSer Fig 2. C t o T substitution in exon 6 encodes a threonine to methionine change. PCR 3 (Fig 1 and Table 1) that spans exons 5 and 6 had a singlebase difference when compared with K2 DNA. The base sequences of a portion of exon 6 and the amino acids that they encode are shown. The sequence of K2 DNA is on the top and K1 DNA on the bottom. The C to T substitution is marked in bold letters and is highlighted with an arrow. An N-linked glycosylation motif in K2 and the disrupted motif in K1 are underscored. From www.bloodjournal.org by guest on February 6, 2015. For personal use only. KELL ( K t ) PHENOTYPE 915 1 2 3 4 5 6 7 8 9 10 11121314151617181920 4740 bp 4 540 bp 4200 bp Fig 3. Bsm I analysis of K1 and K2 genotypes and other Kell-related samples. PCR 3 (740 bp1 was prepared from DNA obtained from various Kell phenotypes. The samples were treated with Bsm I and separated by electrophoresis on 0.8% agarose gels. Lanes 1 and 20 contain l-kb ladder DNA standards. Lane 2 is untreated PCR3 from K1 homozygotes. Lanes 3 through 19 are treated with Bsm 1. Lanes 3 and 4 are K1 homozygotes; lane 5 is K2 homozygote; lanes 6 and 7 are Kl/K2 heterozygotes; lane 8 is a common K:-12 phenotype; lane 9, KO; lane 10, K1.2; lane 11, K:-12,3,-4; lane 12, K:-1,2,6,-7; lane 13, McLeod; lane 14, K:-1.2.10; lane 15, K:-l2,14,24; lane 16, K:12; lane 17, K:l,-2; and lanes 18 and 19, K-1.2. All K2 samples gave uncut 740-bp products and K l l K l yielded 540- and 200-bp fragments. Kl/K2 heterozygotes had 3 bands, the uncut 740-bp and the smaller 540-bp and 200-bp products. bands. Nevertheless, analysis by Western immunoblots, using rabbit antibody to a synthetic peptide derived from the cytoplasmic domain of Kell protein,I3 indicated that K1 protein migrates slightly ahead of the Kell protein that carries common Kell phenotypes (data not shown). Lack of a carbohydrate side chain may expose different parts of the protein leading to immunogenicity. This is another example of loss of glycosylation in an RBC surface protein leading to a change in blood group phenotype. The Webb glycophorin C variant also lacks an N - g l ~ c a n . ~ ~ , ~ ’ The point mutation from C to T in exon 6 creates a new restriction enzyme site, 5’-GAATGCT-3’, that can be cut by Bsm I. This restriction enzyme digestion allows the differentiation of KI/KI and K2/K2 homozygotes and of KUK2 heterozygotes and should be useful as a diagnostic genotype procedure. A possible drawback is that, in very rare cases, RBCs do not express any Kell antigens. In this phenotype, known as Ko(null), the RBCs appear not to have any Kell protein on the RBC membrane. Yet, preliminary experiments in our laboratory indicate that 2 KO persons contain Kell mRNA in peripheral blood and thatthe sequence of the mRNA from the initiation ATG codon to the poly A tail is identical to mRNA obtained from persons with common Kell phenotype. This finding indicates that the base sequences in the 19 exons of K2 and of some KO persons are identical. Therefore, PCR amplification of exon 6 and genotyping by treatment with Bsm I would indicate a K2 genotype in KO persons. Serologic analysis easily detects the KO homozygote, but the KO heterozygotes would be serologically identitied as K2 or K1 and Bsm I analysis would also not discriminate. Presumably the same would occur in theKmod phenotypes in which expression of all Kell-related antigens are weakened. The PCRmethod described could easily be applied to DNA samples obtained from amniotic fetal cells and should prove useful in determining the K1 and K2 genotypes of the fetus. This test can potentially identify those pregnancies at risk for hemolytic disease of the newborn. REFERENCES 1. MarshWL:Bloodgroups ofhumanred cells, in PetzLD, Swisher SN (eds): ClinicalPractice ofBlood Transfusion. New York, NY, Churchill-Livingstone, 1981, p 79 2.MarshWL,RedmanCM:Recent developments in theKell blood group system. Transfus MedRev 1:4, 1987 3. MarshWL,RedmanCM: The Kellbloodgroupsystem: A review. Transfusion 30:158, 1990 4. Redman CM, Marsh WL: The Kell antigens and McLeod red cells, in Agre PC, CartronJP (eds): Protein Blood Group AntigensOf The Human Red Cell: Structure, Function And Clinical Significance. Baltimore, MD, Johns Hopkins, 1992, p 53 5. RedmanCM,Marsh W L The Kell blood group systemand the McLeod phenotype. Semin Hematol 30:209, 1993 6. Petty AC, Daniels CL, Tippett P Application of the MAIEA assay IO the Kell blood group system. Vox Sang 66:216, 1994 7. Zelinski T, Coghlan G, Myal Y, Shiu RPC, Phillips S, White L, Lewis M: Genetic linkage between the Kell blood group system and prolactin-inducible protein loci: Provisional assignmentof KEL to chromosome 7. Ann Hum Gene1 55: 137, 1991 8. Murphy MT. Momson N. Miles JS, Fraser RH, Spurr NK, Boyd E: Regional chromosomal assignment of the Kell blood group locus (KEL) to chromosome 7q33-q35 by fluorescence in situ hybridization: Evidence for the polypeptide nature of antigenic variations. HumGenet 91585, 1993 From www.bloodjournal.org by guest on February 6, 2015. For personal use only. LEE ET AL 916 9. Lee S, Zambas E, Marsh WL, Redman CM: The human Kell blood group mapsto chromosome 7q33 andits expression is restricted to erythroid cells. Blood 81:2804, 1993 IO.Lee S, Zambas ED, Marsh WL, Redman CM: Molecular cloning andprimary structure ofKellblood group proteins. Proc NatlAcad Sci USA 88:6353, 1991 I I. Redman CM, Lee S, Ten Bokkel Huinink D, Rabin BI, Johnson CL, Oyen R, Marsh WL: Comparison of human and chimpanzee Kell blood group system. Transfusion 239:486, 1989 12.BranchD, Muensch H, Sy Siok Hian A,Petz D: Disulfide bonds are a requirement of Kell and Cartwright (Yt") blood group antigen integrity. Br J Haematol 54:573, 1983 13. Russo D, Lee S, Reid M, Redman C: Topology of the Kell blood group protein and the expression of multiple antigens by transfected cells. Blood 84:3518, 1994 14. Lee S, Zambas E, Redman C: Organization of the gene encoding the human Kell blood group protein. Blood 85:1364, 1995 1S. John SWM, Weitzner G , Rozen R, Scriver CR: A rapid procedure for extracting genomic DNA from leukocytes. Nucleic Acids Res 19:408,1991 16. Zelinski T: The use of DNA restriction fragment length polymorphisms in conjunction with blood group serology. Transfusion 31:762, 1991 17. Maniatis T, Fritsch EF, Sambrook J: Molecular Cloning: A Laboratory Manual. Cold Spring Harbor, NY, Cold Spring Harbor Laboratory, 1982 18. Giblett ER: A critique of the theoretical hazard o f inter vs intra-racial transfusion. Transfusion 1:233, 196I 19. Mayne KM, Bowell PJ, Pratt CA: The significance o f antiKell sensitization in pregnancy. Clin Lab Haematol 12:379, 1990 20. Duguid JKM, Bromilow IM: Haemolytic disease of the newborn due to anti-K. Vox Sang S8:69, 1990 21. Moncharmont P, Juron-Dupraz F, Doillon M, Vignal M, Debeaux V: A case of hemolytic disease of the newborn infant due to anti-K (Cellano). Acta Haematol 85:4S, 1991 22. Constantine G, Fitzgibbon N, Weave JB: Anti-Kell in pregnancy. Br J Obstet Gynaecol 98:943, 1991 23. Leggat HM, Gibson JM, Barron SL, Reid MM: Anti-Kell i n pregnancy. Br J Obstet Gynaecol 98:162, 1991 24. Bowman JM, Pollock JM, Manning FA, Harman CK, Menticoglou S: Maternal Kell blood group alloimmunization. Obstet Gynecol 79:239, 1992 25. Bause E: Structural requirements of N-glycosylation proteins. Biochem J 209:33 I , 1983 26. Telen MJ, Le Van Kim C, Guizzo ML, Cartron JP, Colin Y: Erythrocyte Webb-type glycophorin C variant lacks N-glycosylation due to an asparagine to serine substitution. Am J Hematol 37:s I , 1991 27. Chang S, Reid M, Conboy J, Kan Y. Mohandds N: Molecular characterization of erythrocyte glycophorin C variants. Blood 77544, I99 I From www.bloodjournal.org by guest on February 6, 2015. For personal use only. 1995 85: 912-916 Molecular basis of the Kell (K1) phenotype S Lee, X Wu, M Reid, T Zelinski and C Redman Updated information and services can be found at: http://www.bloodjournal.org/content/85/4/912.full.html Articles on similar topics can be found in the following Blood collections Information about reproducing this article in parts or in its entirety may be found online at: http://www.bloodjournal.org/site/misc/rights.xhtml#repub_requests Information about ordering reprints may be found online at: http://www.bloodjournal.org/site/misc/rights.xhtml#reprints Information about subscriptions and ASH membership may be found online at: http://www.bloodjournal.org/site/subscriptions/index.xhtml Blood (print ISSN 0006-4971, online ISSN 1528-0020), is published weekly by the American Society of Hematology, 2021 L St, NW, Suite 900, Washington DC 20036. Copyright 2011 by The American Society of Hematology; all rights reserved.
© Copyright 2026