Overproduction of Proinflammatory Cytokines Imbalanced by
Overproduction of Proinflammatory Cytokines Imbalanced by Their
Antagonists in POEMS Syndrome
By Romain K. Gherardi, Laurent BBlec, Martin Soubrier, Denis Malapert, Mathieu Zuber, Jean-Paul Viard,
Liliane Intrator, Jean-Denis Degos, and FranGois-JerBme Authier
The polyneuropathy, organomegaly, endocrinopathy,
M protein, skin changes (POEMS)syndrome is a rare multisystem
with osteosdedisorder of obscure pathogenesis associated
rotic myeloma. Circulating levels of proinflammatory cytokines (tumor necrosisfactor-a TTNF-rul interleukin-1/3[IL-1/31,
IL-2, IL-6, and interferon y [IFNyl), anti-inflammatory cytokines (transforming growth factor p1[TGF/3,], IL-4, IL-10, and
IL-131, the cytokine carrier protein a2macroglobulin. IL-l receptor antagonist (IL-lra), soluble TNF receptors (sTNFr) p55
and p75, and soluble 11-6 receptor (slL-6r)were determined
in 15 patients with POEMS syndrome and 15 with multiple
myeloma. Patientswith POEMS syndrome had higher serum
levels of IL-1/3, TNF-a, and 11-6 and lower serum levels of
TGFpl than did patients with multiple myeloma. Serumlev-
els of IL-2, IL-4, IL-10, IL-13, IFNy, cu2macroglobulin, and slL6r were similar in both groups. IL-lra and sTNFrs were increased in POEMS syndrome, but out of proportion to the
increase of IL-l/3 and TNF-a. Serial evaluations in 1 patient
showed that proinflammatory cytokine serum levels paralleled disease activity assessed by platelet count and neurologic involvement. Our results suggest that the manifestations of POEMS syndrome might be regardedas the result
of a marked
activation of the proinflammatory cytokine network (IL-1/3, 11-6,and TNF-a) associated
with a weak or even
decreased (TGF/31)antagonistic reaction insufficent to counteract the noxious effects of cytokines.
0 7 9 9 6 by The American Societyof Hematology.
T
werealsofoundto
be elevated79:3 patients had chnicaUy
elevated serum levels of tumor necrosis factor-a W-a),9
a
findingreminiscentoftheincreased
TNF-a serum levels observed in patients with acute inflammatory demyelinating neuropathies,l0." and 5 had elevated serum levels of b l p , likely
related to a sustained activationof macrophages within tissues.'
L 2 and interferon y (IFNy) that stimulate human monocytes/
macrophages12 were not evaluated. The antagonistic mechanisms
that modulate release and biologic activity of proinflammatory
cytokines in vivo were also not evaluated. These mechanisms
include (1) inhibition of human monocyte production ofTNFa,
IL-l@,and L 6 by natural regulators such as
and L-13"; (2) variation of serum levels of carrier proteins such
as a2-macrog10bulin16;(3) binding of circulating cytokines by
soluble forms of their cell surface receptors (eg, soluble TNF-a
receptors [sTNFr] appear in sem in reaction to TNF-a release,
bindthemolecule,andinhibit
TNF-a activitybypreventing
its binding to cellular re~eptors)'~"~;
However, soluble cytokine
receptors may act as agonists rather than antagonists of the relevant cytokineDZ; (4) competitive binding to cellular receptors
of cytokine stmctural analogs devoid of biologic activity (this is
the case of the L-1 receptor antagonist
a member of
the IL-1 family that binds competitively to &l receptors but
does not induce signal transduction)16; and (5) release of functionallyantagonisticcytokinessuch
as transforming growth
factor-p (TGF-p) that antagonizes the effects of TNFa, L-1,
L-2, and IFNy and behavesas a potent anti-inflammatory cyto-
HE POEMS SYNDROME is a rare multisystem disorder usually associated with osteosclerotic myeloma
and characterized by the combination of polyneuropathy(chr0nic inflammatory demyelinating neuropathy),
organomegaly, endocrinopathy, M protein (mainly IgG or IgA with
a A light chain), skin changes (hyperpigmentation, skin thickening, and hypertrichosis), and various other clinical and
pathologic signs such as cachexia, fever, edema, finger clubbing, telangectasias, thrombocytosis, and multicentric Castleman's di~ease."~
Unlike polyneuropathies associated with
IgM gammopathies, an autoimmune mechanism directed toward peripheral nerve components has not been shown in
POEMS ~yndrome.~
It has been suggested that pleiotropic proinflammatory cytokines, which act in synergy on the immune, nervous, and endocrine systems, could play a pathogenetic role in POEMS syndrome. Increased serum levels of interleukin-6 (L-6) have been
occasionally r e p o d in patients with POEMS syndrome?-7 but
whether the finding was relevant to
POEMS syndrome itself
or to an associated Castleman's disease was debated! In
two
preliminary reports from our group, other circulating cytokines
From the Groupe d'Etude et de
Recherche sur le Nerfet le Muscle,
G E M E N , Faculte' de Me'decine de Cre'teil-Paris XIIS Paris; the
Servict d'lmmunologie Biologique, Hbpital Henri Mondor, Cre'teil;
the Service de Rhumatologie, Hbpital Monpied, Clennont-Ferrand;
the Service de Neurologie, Hbpital Saint Anne, Paris; and the Service d'lmmunologie Clinique, Hbpital Necker, Paris, France.
Submitted April 24, 1995; accepted September 28, 1995.
Supported by grants toR. K . G. from the De'le'gation a la Recherche Clinique AP/HP and Agence Nationale de Recherche sur le
Sida.
Address reprint requests to Romain K. Gherardi, MD, De'partement de Pathologie, Hbpital Henri Mondor, F-94010 Cre'teil Cedex,
France.
The publication costsof this article were defrayedin part by page
chargepayment. This article must therefore be hereby marked
"advertisement" in accordance with 18 U.S.C. section 1734 solely to
indicate this fact.
0 1996 by The American Society of Hematology.
0006-4971/96/8704-0026$3.00/0
1450
wlra],
kne.23.24
The present study was performed (l) to substantiate the
finding of increased serum levels of proinflammatory cytokines in a series of 15 patients with POEMS syndrome; (2)
to compare the balance between proinflammatory cytokines
and their antagonists in POEMS syndrome and multiple myeloma (MM); and (3) to correlate dysregulation of the cytokine network in POEMS syndrome with disease markers.
PATIENTS AND METHODS
Patients
Fifteen patients with POEMS syndrome were included. Clinical
and pathologic findings in patients 1 through 57.9 and patient 9*'
Blood, Vol 87, No 4 (February 15). 1996: pp 1458-1465
CYTOKINES AND CYTOKINE ANTAGONISTS
SYNDROME
IN POEMS
were previously published. When the multiple clinical manifestations
of the syndrome were classified into the six categories shown in
Table 1, 13 of the 15 patients were represented under all six categories and 2 under five.
All patients had sensorimotor polyneuropathy and elevated cerebrospinal fluid (CSF) protein levels. Nerve conduction velocities
were in the range of demyelinating disorders in 14 patients and
normal in 1. Organomegaly included hepatomegaly (13 patients),
splenomegaly (10 patients), and lymphadenopathy (1 1 patients). All
patients had at least one biological endocrine abnormality. Monoclonal protein consisted ofIgAX (10 patients), IgGX (3 patients),
andboth IgAX and IgGK (1 patient). Serum levels ofthe A light
chain-bearing monoclonal protein ranged from undetectable (patient
1, who only had free X light chain in blood and urine) to 7 g/L(patient
15). Radiologic bone abnormalities were present in 14 patients and
were multiple in 13. Myeloma was documented histologically in 8
patients. Fourteen patients had at least one typical skin change.
Weight loss was noted in 14 patients and was marked in 10. Other
manifestations of the disease included peripheral edema, anasarca,
hypoalbuminemia, chronic diarrhea, behavioral changes, depression
and other psychiatric disturbances, glomerular nephropathy, severe
diffuse noninflammatory arteriopathy, hypertriglyceridemia, and
thrombocytosis. Castleman’s disease-like lesions were detected by
lymph node biopsy in 6 patients. The follow-up of patients ranged
from 1 to 15 years, and 8 patients died within 1 to 9 years after the
first symptoms.
Serum measurements of patients with POEMS syndrome were
compared with those obtained in 15 patients with MM without neuropathy in whom the serum monoclonal protein level ranged from
10 to 40 g/L.
In an attempt to correlate serum cytokine levels and disease markers at the individual level, serial evaluations were performed in
patient 15. Subsequent to one cure of cytotoxic chemotherapy and
pelvic bone tumor irradiation, circulating cytokine levels hadreturned to normal limits. No treatment was administered during the
following 70 days while blood sampling was performed every 10
days to assess platelet count, monoclonal IgAA, and cytokine levels.
The neurologic status was evaluated clinically, using the neuropathy
disability score (NDS),26and by the study of nerve conduction velocities.
1459
and 5 pg/mL for IL-10. Healthy controls have L - 4 and IL-l0 serum
levels less than these threshold values. Domestic ELISA for IL-13
was kindly performed byA. Minty (Sanofi, LaMge, France) in 3
patients with POEMS syndrome and 2 patients with MM. Threshold
of detection with this test is 200 pg/mL. TGF-P1 was measured by
the Predicta ELISA test (Genzyme). The normal range of TGF-81
is 24 to 104 ng/mL (mean, 70 ng/mL).
Measurements of a2-macroglobulin. Serum a2-macroglobulin
(normal range, 1.2 to 3.2 m&) was determined by ELISA (Immunodiagnostik, Bensheim, Germany).
Measurements of IL-Ira and soluble cytokine receptors (sTNFrs
and slL-6rj. Serum L - l r a and sIL-6r were determined using the
ELISAs Quantikine (R&D Systems, Minneapolis, MN). Using these
assays, the upper limit of IL-lra serum levels in healthy subjects is
250 pg/mL and that of sIL-6r is 46 ng/mL. Serum sTNFr (p55) and
sTNFr (p75) levels were determined by the Cobas-Core enzymelinked immunobiologic assay (Roche Diagnostic Systems, Basel,
Switzerland). Using this assay, the upper limits of sTNFr (p55) and
sTNFr (p75) serum levels in healthy donors never exceeded 1,700
pg/mL and 5,500 pg/mL, respectively. To estimate whether the elevations of cytokine antagonist levels were proportional to thatof
their relevant cytokine in POEMS syndrome and MM, we calculated
the following ratio:
R=
[Mean Antagonist Level in POEMS Syndrome]
[Mean Cytokine Level in POEMS Syndrome]
X
[Mean Cytokine Level in MM]
[Mean Antagonist Level in MM]
Statistical Analysis
Concentrations were expressed as the mean -C standard error (SE).
Statistical analysis was performed using the Mann and Whitney U
test for comparison of average serum concentrations of cytokine
and cytokine antagonists, the Fisher’s exact test for comparison of
prevalences of elevated values, and the Spearman’s test for correlation between cytokines and cytokine antagonist serum levels. A P
value less than .05 was considered significant.
RESULTS
Serum Measurements
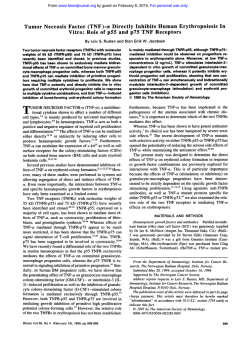
Proinjammatory Cytokines (TNF-a, IL-10, IL-2,IL-6, and
IFNy; Fig l )
Serum sampling. Determinations of serum cytokines levels were
performed prospectively, except in patients 4 and 5.Peripheral blood
was taken in dry tubes at 8 AM,the storage of the whole blood was
performed at room temperature, the serum was separated within 1
hour, and the sera were kept frozen at -70°C until analyzed. Blood
samples were obtained in the absence of fever, shock, and overt
infection.
Measurements of proinjammatory cytokines (TNF-a, IL-IP, IL2, IL-6, and IFNy). Commercially available kits for enzyme-linked
immunosorbent assays (ELISA) were used to detect total TNF-a,
ie, TNF-a bound and unbound to sTNFrs, L I P , IL-6 (Immunotech,
Marseille, France), IL-2, and IFNy (Genzyme, Cambridge, MA).
Using these tests, the TNF-a serum levels upper limit is 15 pg/mL
in healthy subjects, for IL-I@ is 5 pg/mL, for IL-2 is 100 pg/mL,
for IL-6 is 10 pg/mL, and for IFNy is 100 pg/mL. Biologic activity
of TNF-a was kindly assessed on D-actinomycin-treated L929 cells
by S. Chouaib (Institut Gustave Roussy, Villejuif, France) in 5 patients with POEMS syndrome and 5 with MM.
Measurements of suppressor cytokines (IL-4, IL-IO, IL-13, and
TGF-PI). IL-4 and IL-IO were measured by commercial ELISA
(Genzyme). The sensitivity of ELISA tests was 15 pdmL for IL-4
In the POEMS syndromegroup,serum IL-lP was increased (>5 pg/mL) in 14’patients,TNF-a ( > l 5 pg/mL) in
10, and IL-6 ( > l 0 pg/mL) in 10. In the MM group, serum
E - 1 0 was increased in 1 patient, TNF-a in 4, and IL-6 in
1.
The average serum concentrations of IL-10, TNF-a, and
IL-6 were greater in patients with POEMS syndrome than
in control patients with multiple myeloma (Fig 1). The mean
concentration of IL-10 was 161 ? 73 pg/mL in patients with
POEMS syndrome and 3 5 3 pg/mL in MM (P < .0001;
95% confidence interval [CI], 5 to 317 and 0 to 9, respectively). The mean TNF-a concentration was 102 2 36 pg/
mL in POEMS syndrome and 10 ? 5 pg/mL in MM ( P <
,005; 95% CI, 25 to 179and 0 to 20, respectively). The
meanIL-6 concentration was 40 ? 9 pg/mLin POEMS
syndrome and 4 5 3 pg/mL MM ( P < .OOOl; 95% CI, 20
to 60 and 0 to 11, respectively).
Serum concentrations of IL-2 and IFNy were similar in
POEMS syndrome and MM. The mean IL-2 concentration
1460
GHERARDI ET AL
Y
a
+
I
t
i
I l + + + l +
l
+ +
+ + +
+ +
I
I
+
P .L!
I
I
I
l
+
l
+ + l
l
+
+
l
+ + +
I
I
l
l
I
/
+ + l
I
I
1
1
+
+ +
+ + +
l
l
l
+
l
+ +
+ + l
l
l
+ m , + + +
+
+++
+-
l
l
+
l
1
l
+
l
(C. +(C.*.#..
+ +
+
I
+
+
l
+ +
+ + +
l
(C.-.-.-.
+ +
+ + +
++
+++
I + + l + l l
++
+
+ + 1 + + + 1
l
+
+(C.+
+ P , +
I
+
+
l
l
l
+
l
+
l
+
l
l
l
+ + + + + +
l l + + + + +
+ +
l l + + + l +
l
+
+
I
l
I
I
l
+
l
l
I
+
.L!
+
-.(C.
t
l
+ + m .
I
/
Q
+ + + + + + l
I
l
U .U
l
+
+
+
+
I
l
l
l
l
l
l
l
I
!
I
U .L!
.=S+
l
+
+
+
l
l
l
l
I
+ + + + l
I
I
l
l
l
I
I
l
l
l
l
I
+
+
+
+
+
l
I
l
!
.L! +
:g
Q
l
+
+
l
l
+
+
+
+
l
l
l
l
l
l
l
+
l
+
-
+
+
+
+ + + + + l
l
+
l
!
l
l
l
l
i + . +
+ + + + & . l + .
+
l
+
+ +
+
l
:
+
I
l
l + + + + +
+
+
+
l
l
+
l
l
I
+(C.
+
l
l
t
l
l
+
+
l
+
I
'
,
"
+
l
+I;;
I N
l
+(C.-;:
I
I
+:
l
l
l -
l
l
I
I
+
1 0 )
l
l
+?
l
+
,
l
+
I;;
1
N
%
l - . w
+ + m
+ + + + + + +
+++e
+
+++y
l
+
l
+
I
+ + + + + l 1
l
+++(D
1461
CYTOKINES AND CYTOKINE ANTAGONISTS IN POEMS SYNDROME
dm1
T
200
100
LIIl
TNF,
IL-6
IL-2'
IFNy
p < 0.mOl
p < 0.005
p' 0.mt
NS
NS
lLlra
p 0.03
Fig 1. Serum proinflammatory cytokine levels (mean f SE) in
patients with POEMS syndrome (n = 15) and MM (n = 15). Serum
levels of IL-2 are expressed as 10" x pglmL (*l.
was elevated in both groups (488 t 135 pg/mL in POEMS
syndrome and 385 ? 125 pg/mL in MM; NS). The mean
IFNy concentration wasnormal in both groups (79 t 38
pg/mL in POEMS syndrome and 40 t 14 pg/mL in MM;
NS).
Suppressor Cytokines (IL-4, IL-IO, IL-13, and TGF-01;
Fig 2 )
IL-4 and IL-l0 were not detected in the serum of patients
with POEMS syndrome and MM. In the 3 POEMS and 2
MM patients evaluated, IL-13 serum levels greater than 200
pg/mL were not observed. Serum levels of TGF-P1 were
within normal limits (24 to 104 ng/mL) in 9 of 14 patients
with POEMS syndrome and 14 of 14 patients with MM.
The mean concentration of serum TGF-P1 was significantly
lower in POEMS syndrome than in MM (43 5 9 pg/mL in
POEMS syndrome and 79 2 l 1 pg/mL in MM; P < .04).
a2-Macroglobulin (Fig 2 )
Mean serum a2-macroglobulin levels were in the normal
range (1.2 to 3.2 m&) in both groups (1.20 t 0.07 mg/L
in POEMS syndrome and 1.37 t 0.1 1 mg/L in MM: NS).
sTNFr(pss)*
p < 0.01
sTNFr(p79*
p = 0.01
slL-6r.
NS
Fig 3. Serum levels of IL-lra andsoluble cytokine receptors (mean
f SE) in patients withPOEMS syndrome (n = 14) and MM (n = 14).
Serum levels of sTNFr (p55) and sTNFr (p751 are expressed as lo-*
x pglmL ("1. Serum levels of slL-6r are expressed as lo3 x pglmL
(**L
IL-Ira and Soluble Cytokine Receptors (sTNFrs and slL6r: Fig 3 )
In the POEMS syndrome group, serum IL-Ira was increased in 3 patients, sTNFr ( p 5 3 in 13, sTNFr ( p 7 3 in 10,
and sIL-6r in 7. In the MM group, IL-Ira was increased in
1 patient, sTNFr ( p 5 3 in 13, sTNFr ( p 7 3 in 4, and sILdr
in 7.
The average serum concentrations of IL-lra, sTNFr (p55),
and sTNFr (p75), but not of sIL-6r, were greater in POEMS
syndrome than in MM (Fig 2). The mean concentration of
IL-lra was 193 t 58 pg/mL in patients with POEMS syndrome and I19 ? 69.2 pg/mL in MM (P < .03; 95% CI,
67 to 320 and 0 to 267, respectively). The mean sTNFr
( p 5 3 concentration was 6,900 2 1,100 in pg/mL in POEMS
syndrome and 3,300 ? 500 in MM ( P < .01; 95% CI, 4,100
to 8,700 and 1,900 to 4,100, respectively). The mean sTNFr
( p 7 3 concentration was 8,300 t 1,100 pg/mL in POEMS
syndrome and 4,600 t 700 pg/mL in MM ( P < .01; 9596
CI, 5,500 to 10,500 and 2,800 to 5,800, respectively). The
mean sIL-6r concentration was 51 2 4 ng/mL in POEMS
syndrome and 48 2 4 ng/mL in MM (NS).
L
Balance Between P roinjlammatory Cytokines and Their
Antagonists
TGF-Rt
ILO
p<OM
NS
ILIO
NS
atm
NS
Fig 2. (Left) serum suppressor cytokine levels (mean & SE) in
patients with POEMS syndrome (n = 14) and MM (n = 14). (Right)
serum u2macroglobulin (m2-M) levels (mean f SE) in patients with
POEMS syndrome (n = 12) and MM (n = 14).
Increase of IL-Ira levels was less frequent than increase
of IL-10 levels in POEMS syndrome ( P < .005). This was
not the case in MM, in which a single patient had elevation
of both IL-lra and L-1P serum levels (NS). Mean levels of
IL-lra werenot
proportional to mean IL-1P levels in
POEMS syndrome and MM (R = 1 :3). Serum IL-lra concentrations correlatedpositivelywith
those of IL-lp in
POEMS syndrome ( r = +.74; P < .005).
Increase of sTNFr ( p 5 3 levels was more frequent than
increase of TNF-a levels in both POEMS syndrome ( P <
.05) and MM ( P < .001). No difference was foundfor sTNFr
( p 7 3 (NS). Mean levels of sTNFrs were not proportional to
1462
GHERAADI ET AL
mean TNF-a levels in POEMS syndrome andMM [R =
1:4.9 for sTNFr (p55); R = 15.6 for sTNFr (p75)]. Consistently, the detected TNF-a was biologically active in patients
with POEMS syndrome, as shown by the killing of L929
cells, whereas no biologic activity of TNF-a was detected
in patients with MM. In POEMS syndrome, no significant
correlations could be established between sTNFr (p%) or
sTNFr ( p 7 3 levels and TNF-a levels. In MM, sTNFr (p75)
levels correlated positively with TNF-a levels ( r = +.75; P
< .002), whereas sTNFr ( p 5 3 levels did not.
Increase of sIL-6r levels was more frequent than increase
of IL-6 levels inMM (7/14 v 1/15, P < .02), butnotin
POEMS syndrome (7/14 v 10/15, NS).
PiW-
120
100
80
60
40
20
Clinical Correlations
Cross-sectional correlations between point evaluations of
serum cytokines levels and clinical or biologic manifestations of the disease collected over a long period of time
could not be established.
At the individual level (patient 15), increase of proinflammatory cytokines and decrease of TGF-P1 detected in
blood from day 1 to day 70 were observed at the time of
worsening of the neuropathy (assessed by the neuropathy
disability score and nerve conduction velocities) and increase
of the platelet count above normal values (Fig 4). Serial
evaluations (n = 7) showed positive correlation between
serum IL-6 levels and platelet count ( r = +.9; P < .003).
Patient 1 I had nodetectable circulating IL-lp, TNF-a,IL6, IL-lra, and sTNFr (p75) levels, but he did have markedly
elevated levels of sTNFr (p55) (10,200 pg/mL). He had been
treated using long-term cytoxic and steroid therapy and was
considered to be in complete remission. This patient had the
longest survival time of the series (>15 years).
day 1
day 70
35 -
- 120
- 100
-
- 80
-60
25 -.- 4 0
t
*O
DISCUSSION
In the present study, 14 of 15 patients with POEMS syndrome had increased IL-lp, 10 had increased TNF-a, and
10 had increased IL-6 serum levels. Serum concentrations
of IL-lp, TNF-a, and L-6, but not IL-2 and IFNy, were
higher in POEMS syndrome than in MM without neuropathy. These results substantiate our previous finding^'.^ and
confirm that an increased release of proinflammatory cytokines occurs in patients with POEMS syndrome. These cytokines are functionally related as IL-1 and TNF-a stimulate
one another, andboth IL-I and TNF-a stimulate IL-6.”
Our findings, therefore, strongly suggest an activation of the
proinflammatory cytokine network. The primary site and the
cause of activation of cytokine production are undetermined.
Production of IL-lp in POEMS syndrome has been evidenced in lymph node interfollicular areas in 2 patients7
The lymph nodes were devoid of monotypic B-cell infiltration, and it waslikely that nodal production of IL-1 reflected
a systemic activation of the monocyte/macrophage system.
In the same way, the finding of normal levels of IFNy and
IL-2 levels similar to controls in the present study suggests
that activation of macrophages rather than T cells is the
primary process in POEMS syndrome. However, activation
Fig 4. Serum cytokine levels (top) and disease markers (bottom)
in patient 15.
of cytokine production appears to be linked in some fashion
to a unique property of the plasma cell clone, or its secretory
products, because complete recovery of POEMS syndrome
occurs in patients with a solitary plasmocytoma after surgery
and local irradiation.**One can speculate that the monoclonal
gammopathy or its X light chain triggers the monocytdmacrophage system to produce proinflammatory cytokines. Alternatively, the tumor itself may produce cytokines, as increased production of IL-6, IL- 1,and TNF-a by bone
marrow cells from patients with myeloma has been occasionally shown in vitro.29
A balance between production of cytokines and their antagonists, ie, either functionally antagonistic cytokines or
specific cytokine antagonists, is important in determining
host responses. Among suppressor cytokines, TGF-P1 was
significantly lower in serum of patients with POEMS syndrome than in patients with MM. Knockout mice experiments have shown that suppressed TGF-P production is as-
CYTOKINES AND CYTOKINE ANTAGONISTS IN POEMS SYNDROME
1463
in POEMS syndrome.However,lowconcentrationsofIL-1
sociated with severe systemic inflammation." It is
paradoxically stimulate bone formation in vitro55ILand
l upregestablished that TGF-@l antagonizes the effects of proinulates surface receptor of TGF-@?O andit is possible that osteoflammatory cytokines and acts as a monocyte/macrophage
sclerosis in POEMS syndrome results from local cytokine-indeactivating factor by decreasing hydrogen peroxide and niduced dysregulation of the complex metabolism of bone.
trous oxide production as well as L - 6 and TNFa producIn conclusion, our results suggest that the manifestations
t i ~ n . ' It
~ is currently believed that the biologic effects inof POEMS syndrome might be regarded as the result of a
duced by a given concentration of IL-1 are inhibited by 10
marked activation of the proinflammatory cytokine network
to 100 times more IL-lra.30 In our series, only 3 patients
associated with aweak, or even decreased, antagonistic reacwith POEMS syndrome had increased L - l r a levels, which
tion insufficent to buffer the noxious effects of cytokines.
contrasted with the almost constant increase of circulating
IL-l@ in this group. The mean concentration of LIra was
ACKNOWLEDGMENT
of the same order as the mean concentration of IL-10. Thus,
it is likely that L - l r a production in POEMS syndrome was
We acknowledge Roche Diagnostic Systems (France) for their
insufficent to buffer the effects of increased IL-lP produchelp in determination of circulating soluble TNF receptors.
tion. Increased sTNFrs levels suggestive of an activation of
the TNF-a system14 were observed in both POEMS synREFERENCES
drome and MM. However, concentrations of sTNFr ( p 5 9
1. Bardwick PA, Zwaifler NJ, Gill GN, Newman D, Greenway
and (p75) relative to the homologous concentrations of TNFGD: Plasma cell dyscrasia with polyneuropathy, organomegaly, ena were about fivefold less important in POEMS syndrome
docrinopathy, M-protein and skin changes: The POEMS syndrome.
Medicine 59:311, 1980
than in MM, suggesting that increase of sTNFreceptors was
2. Nakanishi T, Sobue I, Toyokura Y, Nishitani H, Kuroiwa Y,
weak with regard to that of TNF-a. Biologic activity of
Satoyoshi
E, Tsubaki T, Igata A, Ozaki Y: The Crow-Fukase synTNF-a was consistently shown in vitro with sera of patients
drome: A study of 102 cases in Japan. Neurology 34:712, 1984
with POEMS syndrome but not with MM. The sIL-6r in3. Miralles GD, O'Fallon JR, Talley NJ: Plasma cell dyscrasia
crease was similar in POEMS syndrome and MM (7/14 pawith polyneuropathy. The spectrum of POEMS syndrome. N Engl
tients in each group). The feature was associated witha
J Med 327:1919, 1992
frequent increase of IL-6 in POEMS syndrome (10 patients)
4. Gherardi R, Zuber M, Viard JP: Les neuropathies dysglobubut not in MM (1 patient).
lintmiques. Rev Neurol (Paris) 144:391, 1988
The strong activation of the proinhnmatory cytokine net5. Fukatsu A, Ito Y, Yuzawa Y, Yoshida F, Kat0 M, Miyakawa
work in POEMS syndrome and the imbalance between produc- K, Matsuo S: A case of POEMS syndrome showing elevated serum
interleukin 6 and abnormal expression of interleukin 6 in the kidney.
tions of cytokines and their antagonists suppofl the view that
Nephron 62:47, 1992
cytokines may be implicated in the expressionof the disease. A
6. Mandler RN, Kerrigan DP, Smart J, Kuis W, Villiger P, Lotz
correlationwasfoundattheindividuallevelbetweenproinM:
Castleman's disease in POEMS syndrome with elevated interleuflammatory cytokine serum levels and disease activity assessed
kin-6. Cancer 69:2697, 1992
by platelet count and both clinical and electrophysiologic severity
7. Gherardi RK, Belec L, Fromont G, Divine M, Malapert D,
of the neuropathy. In fact, it is not possible
to ascribe onesymp
Gaulard P, Degos J-D: Elevated levels of IL-lp and IL-6 in serum,
tom to a single cytokinebecause TNF-a,IL-lP, and, to a lesser and increased production of IL-lp mRNA inlymph nodes of patients
extent, I L 6 have widely overlapping biologic activities and act
with POEMS syndrome. Blood 83:2587, 1994
synergistically." However, in light of human and experimental
8. Emile C, Danon F, Fermand JP, Clauvel JP: Castleman disease
studies, chronically elevated TNF-a levels correlate well with
in POEMS syndrome with elevated interleukin-6. Cancer 71:874,
1993 (letter)
inflammatorydemyelinatingneumpathy,l0.l' oqpnomegaly af9. Gherardi RK, Chouaib S, Malapert D, Belec L, Intrator L,
fecting liver and spleen?' endocrine dysfunctions of POEMS
the
Degos JD: Early weight loss and high serum levels of tumor necrosis
syndrome, including hypotestosteronemia and reactional release
of gonadotrophins?'hypoc0rtisolism,33~" h y p o t h ~ i d i ~ m , ~ ' factor-a
~ ~ ~ in patients with POEMS syndrome. AnnNeurol 35501,
and hw~proiacthemiq~'
skin changes, such as h~rtrichosis3* 1994
10. Sharief MK, McLean B, Thomson EJ: Elevated serum levels
and finger ~lubbing:~and other clinical manifestations such as
of
tumor necrosis factor-a in Guillain-Barre syndrome. Ann Neurol
&,w40,41
Inhibition of key adipogenic enzymes with weight
333591, 1991
~ O S S , ~ ~hypertriglyceridemia,"
"'
and
High
&l@levels
11. CrBange A, BBlec L, Clair B, Raphael JC, Gherardi RK:
can produce cachexia with an~rexia,'~ sympathic activation of
Differential kinetics of circulating tumor necrosis factor (TNF)-alpha
brown adipose tissue,4 and skin pigmentation through the activa- and soluble TNF receptors (sTNFrs) in patients with Guillain-Barr6
syndrome (GBs). Neurology 45:A415, 1995 (suppl 4)
tion of the proopiomelanocortin gene." Overproduction ofIL-IP
may also accountfor multiple endocrine abnormalities, including 12. Varesio L, Espinoza-Delgado I, Gusella L, Cox GW, Melillo
G, Musso T, Bosco MC: Role of cytokines in the activation of
glucose intolerance," behavioral andpsychiahc dist~rbances,4~~~*
monocytes,
in Aggarwal BB, PuriRK (eds): Human Cytokines:
and accelerated atherosclerosis."9 HighIG6levels correlate well
Their Role in Disease and Therapy. Cambridge, MA, Blackwell
withplasmacellproliferationandgammopathy,"thromboScience, 1995, p 55
cytosis;'
Castleman's
hemangjomas,"
and
microan13. te Velde AA, Huijbens RJF, Heije K, de Vries JE, Figdor
giopathic glomedopathy? In contrast, L-10 and TNF-a are
CG: Interleukin 4 (IL-4) inhibits secretion of IL-10, tumor necrosis
potent osteoclast activating factors and TGF-0 stimulates bone
factor-a and IL-6 by human monocytes. Blood 76: 1392, 1990
f~rmation~'
which do not fit well with osteosclerosis observed
14. de Malefyt RW, Abrams J, Bennett B, Figdor CG, de Vries
'
1464
JE: Interleukin-l0 (IL-10) inhibits cytokine synthesis by human
monocytes: An autoregulatory role of IL-10 produced by monocytes.
J Exp Med 1741209, 1991
15. Minty A, Chalon P, Derocq JM, Dumont X, Guillemot JC,
Kaghad M, Labit C, Leplatois P, Lauzun P, Miloux B, Minty C,
Casellas P, Loison G, Lupker J, Shire D, Ferrara P, Caput D: Interleukin-13 is a new human lymphokine regulating inflammatory
and immune responses. Nature 362:248, 1988
16. Legres LG, Pochon F, Barray M, Heinrich PC, Delain E:
Human alpha 2-macroglobulin as a cytokine-binding plasma protein.
A study with rh-interleukin lbeta and rh-interleukin 6. Ann NY
Acad Sci 737:439, 1994
17. Seckinger P, Isaaz S, Dayer J-M: A human inhibitor of tumor
necrosis factor-a. J Exp Med 167:1511, 1988
18. Engelmann H, Novick D, Wallach D: Two tumor necrosis
factor-binding proteins purified from human urine. Evidence for immunological cross-reactivity with cell surface tumor necrosis factor
receptors. J Biol Chem 265:1531, 1990
19. Lantz M, Malik S, Slevin ML, Olsson I: Infusion of tumor
necrosis factor (TNF) causes an increase in circulating TNF-binding
protein in humans. Cytokine 2:402, 1990
20. Aderka D, Engelmann H, Maor Y, Brakbusch C, Wallach D:
Stabilization of the bioactivity of tumour necrosis factor by its soluble receptors. J Exp Med 175:323, 1992
21. Burger D, Chicheportiche R, Giri JG, Dayer JM: The inhibitory activity of human interleukin-l receptor antagonist is enhanced
by type I1 interleukin-l soluble receptor and hindered by type I
interleukine 1 soluble receptor. J Clin Invest 96:38, 1995
22. Salvati AL, Lahm A, Paonessa G , Ciliberto G, Toniatti C:
Interleukin-6 (IL-6) antagonism by soluble IL-6 receptor alpha mutated in the predicted gpl30-binding surface. J Biol Chem
270:12242, 1995
23. Roberts AB, Sporn MB: Physiological actions and clinical
applications of transforming growth factor-P (TGF-P). Growth Factors 8:1, 1993
24. Kulkami AB, Karlsson S: Transforming growth factor$
knockout mice. Am J Pathol 143:3, 1993
25. Viard JP, Lesavre P, Boitard C, Noel LH, Roth A, Said G ,
Bach JF: POEMS syndrome presenting as systemic sclerosis: Clinical and pathological study of a case with microangiopathic glomerular lesions. Am J Med 84:524, 1988
26. Dyck PJ, Low PA, Windebank AJ, Jaradeh SS, Gosselin S,
Bourque P, Smith BE, Kratz KM, Kames JL, Evans BA, Pineda
AA, O'Brien P, Kyle RA: Plasma exchange in polyneuropathy associated with monoclonal gammopathy of undetermined significance.
N Engl J Med 325:1482, 1991
27. Akira S, Hirano T, Taga T, Kishimoto T: Biology of multifunctional cytokines: IL6 and related molecules (ILl and TNF).
FASEB J 4:2860, 1990
28. Gherardi RK, Amiel H, Martin-Mondiere C, Viard JP, Salama
J, Delaporte P: Solitary plasmocytoma of the skull revealed by a
mononeuritis multiplex associated with immune complex vasculitis.
Arthritis Rheum 32:1470, 1989
29. Lichtenstein A, Berenson J, Norman D, Chang MP, Carile
A: Production of cytokines by bone marrow cells obtained from
patients with multiple myeloma. Blood 74:1266, 1989
30. Dinarello CA: Anti-cytokine strategies. Eur Cytokine Netw
3:7, 1992
31. Patton JS, Peters PM, McCabe J, Crase D, Hansen S, Chen
AB, Liggitt D: Development of partial tolerance to the gastrointestinal effects of high doses of recombinant tumor necrosis factor-a in
rodents. J Clin Invest 80:1587, 1987
32. Mealy K, Robinson B, Millette CF. Majzoub J, Wilmore DW:
GHERARDIETAL
The testicular effects of tumor necrosis factor. Ann Surg 211:470,
1990
33. Jaattela M, Ilsvemiiki V, Voutilainen R, Stenman U-H, Saksela E: Tumor necrosis factor as a potent inhibitor of adrenocorticotropin-induced cortisol production and steroidogenic P450 enzyme
gene expression in cultured human fetal adrenal glands. Endocrinology128:623, 1991
34. Reincke M, Heppner C, Petzke F, Allolio B, Arlt W, Mbulamberi D, Siekmann, Vollmer D, Winkelmann W, Chrousos GP:
Impairment of adrenocortical function associated with increased
plasma tumor necrosis factor-alpha and interleukind concentrations
in African trypanosiomasis. Neuroimmunomodulation l:l4, 1994
35. Pang W,Hershman JM, Mire11 CJ, Pekary AE: Impairment
of hypothalamic-pituitary-thyroidfunction in rats treated with human
recombinant tumor necrosis factor-a (cachectin). Endocrinology
125:76, 1989
36. Van der Poll T, Romijn JA, Wiersinga WM, Sauerwein HP:
Tumor necrosis factor: A putative mediator of the sick euthyroid
syndrome in man. J Clin Endocrinol Metab 71:1567, 1990
37. Koike K, Masumoto N. Kasahara K, Yamaguchi M, Tasaka
K, Hirota K, Miyake A, Tanizawa 0:Tumor necrosis factor-a stimulates prolactin release from anterior pituitary cells: A possible
involvement of intracellular calcium mobilization. Endocrinology
128:2785, 1991
38. Tracey KJ, Morgello S, Koplin B, Fahey TJ, Fox J, Aledo
A, Manogue KR, Cerami A: Metabolic effects of cachectidtumor
necrosis factor are modified by the site of production. Cachectid
tumor necrosis factor-secreting tumor in skeletal muscle induces
chronic cachexia, while implantation in brain induces predominantely acute anorexia. J Clin Invest 86:2014, 1990
39. Braegger CP, Comgan CJ, MacDonald 'IT: Finger clubbing
and tumour necrosis factor a . Lancet 336:759, 1990
40. Brett J, Gerlach H, Nawroth P, Steinberg S, Godman G, Stem
D: Tumor necrosis factorkachectin increases permeability of endothelial cells monolayers by a mechanism involving regulatory G
proteins. J Exp Med 169:1977, 1989
41. Darling G , Fraker DL, Jensen JC, Gorschboth CM, Norton
JA: Cachectic effects of recombinant human tumor necrosis factor
in rats. Cancer Res 504008, 1990
42. Feingold KR, Adi S, Staprans I, Moser AH, Neese R, Verdier
JA, Doeller W, Grunfeld C: Diet affects the mechanisms by which
TNF stimulates hepatic triglyceride production. Am J Physiol
259:E177, 1990
43. Plata-Salaman CR, Oomura Y, Kai Y: Tumor necrosis factor
and interleukin-l-beta: Suppression of food intake by direct action
in the central nervous system. Brain Res 449:106, 1988
44. Dascombe MJ, Rothwell NJ, Sagay BO, Stock MJ: Pyrogenic
and thermogenic effects of interleukin-l beta in the rat. Am J Physiol
256:E7, 1989
45. Brown SL, Smith LR, Blalock JE: Interleukin-l and interleukin-2 enhance proopiomelanocortin gene expression in pituitary
cells. J Immunol 139:3181, 1987
46. Bendtzen K, Mandrup-Poulsen T, Nerup J, Nielsen JH, Dinarello CA, Svenson M: Cytotoxicity of human p17 interleukin-l for
pancreatic islets of Langherans. Science 232:1545, 1986
47. Maes M, Bosmans E, Meltzer HY, Scharpi S, Suy E: Interleukin-l@ A putative mediator of HPA axis hyperactivity in major
depression? Am J Psychiatry 150:1189, 1993
48. Otterness IG, Golden H W , Seymour PA, Eskra JD, Daumy
GO: Role of prostaglandins in behavioral changes induced by murine
interleukin 1 alpha in the rat. Cytokine 3:333, 1991
49. Clinton SK, Libby P: Cytokines and growth factors in atherogenesis. Arch Pathol Lab Med 116:1292, 1992
50. Kishimoto T: The biology of interleukin-6. Blood 74:1, 1989
CYTOKINES AND CYTOKINE ANTAGONISTS IN POEMSSYNDROME
51. Ishibashi T, Kimura H, Shikama Y, Uchida T, Kariyone S ,
Hirano T, Kishimoto T, Takatsuki F, Akiyama A: Interleukin-6 is
a potent thrombopoietic factor in vivo in mice. Blood 74: 1241, 1989
52. Yoshizaki K, Matsuda T, Nishimoto N, Kuritani T, Taeho L,
Aozasa K, Nakahata T, Kawai H, Tagoh H, Komori T, Kishimoto
S , Hirano T, Kishimoto T: Pathogenic significance of interleukin-6
(IL-6/BSF-2) in Castleman’s disease. Blood 74:1360, 1989
53. Leger-Ravet MB, Peuchmaur M, Devergne 0, Audouin J,
1465
Raphael M, Van Damme J, Galanaud P, Diebold J, Emilie D: Interleukin-6 gene expression in Castleman’s disease. Blood 78:2923,
1991
54. Motro B, Itin A, Sachs L, Keshet E: Pattern of interleukin-6
expression in vivo suggests a role for this cytokine in angiogenesis.
Proc Natl Acad Sci USA 87:3092, 1990
55. Watrous DA, Andrews BS: The metabolism and immunology
of bone. Semin Arthritis Rheum 19:45, 1989
© Copyright 2026