Rapid Eye Movement-Related Disordered Breathing*
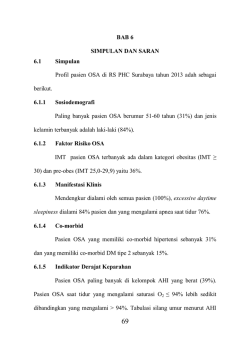
Rapid Eye Movement-Related Disordered Breathing* Clinical and Polysomnographic Features Jose´ Haba-Rubio, MD; Jean-Paul Janssens, MD; Thierry Rochat, MD, PhD; and Emilia Sforza, MD, PhD Objective: The existence of a rapid eye movement (REM)-specific sleep-disordered breathing (SDB) has been suggested based on the finding of an association between sleepiness and respiratory disturbances confined primarily to REM sleep. The aim of the study was to define the frequency and the clinical and polysomnographic features of REM SDB in a large clinical population. Methods: Anthropometric, clinical, and polysomnographic characteristics of 415 patients undergoing polysomnography for SDB were examined. For all patients the apnea-hypopnea index (AHI) during total sleep time, the AHI during REM (AHI-REM), and the AHI during non-REM sleep (AHI-NREM) were calculated. REM SDB was defined as an AHI-REM/AHI-NREM ratio >2. Patients were stratified according to the severity of disease in mild, moderate, and severe cases. Daytime sleepiness was assessed subjectively by the Epworth sleepiness scale (ESS), and objectively, in a subgroup of 228 patients, by the maintenance wakefulness test (MWT). Results: Of the initial sample, 36.4% of cases (n ⴝ 151) fulfilled the REM SDB criteria. No significant differences in subjective complaints, medical history, and drug intake were present between REM and non-REM SDB patients, and no significant differences were found in ESS scores and mean sleep latency of the MWT between groups. A high occurrence of REM SDB was found in mild (73.1%) and moderate cases (47.2%). While in the entire group and in non-REM SDB patients a strong male prevalence was found, the incidence of REM SDB was similar in men and women. Conclusion: Our results show that neither clinical history nor daytime sleepiness differentiate patients with REM SDB from non-REM SDB patients. The disorder is more common in mild and moderate cases; there is an equal incidence in women and men. These findings may suggest that REM-related SDB is a part of the spectrum of SDB. (CHEST 2005; 128:3350 –3357) Key words: polysomnography; rapid eye movement sleep; sleep-disordered breathing; sleepiness Abbreviations: AHI ⫽ apnea-hypopnea index; AHI-NREM ⫽ apnea-hypopnea index during non-rapid eye movement; AHI-REM ⫽ apnea-hypopnea index during rapid eye movement; AHI-TST ⫽ apnea-hypopnea index during total sleep time; BMI ⫽ body mass index; ESS ⫽ Epworth sleepiness scale; MWT ⫽ maintenance wakefulness test; NREM ⫽ non-rapid eye movement; ODI ⫽ oxygen desaturation index; REM ⫽ rapid eye movement; Sao2 ⫽ arterial oxygen saturation; SDB ⫽ sleep-disordered breathing; SFI ⫽ sleep fragmentation index; TST ⫽ total sleep time apid eye movement (REM)-related sleep-disorR dered breathing (SDB) has been introduced by sleep researchers to refer to a specific SDB characterized by daytime sleepiness and respiratory distur*From the Sleep Laboratory, Department of Psychiatry (Drs. Haba-Rubio and Sforza), and Pneumonology Division (Drs. Janssens and Rochat), University Hospital, Geneva, Switzerland. Manuscript received January 12, 2005; revision accepted May 27, 2005. Reproduction of this article is prohibited without written permission from the American College of Chest Physicians (www.chestjournal. org/misc/reprints.shtml). Correspondence to: Emilia Sforza, MD, PhD, Laboratoire de Sommeil, Service de Psychiatrie Adulte, Hoˆpitaux Universitaires de Gene`ve, 2 Chemin du Petit Bel Air, 1225 Cheˆne Bourg, Gene`ve, Switzerland; e-mail: [email protected] 3350 Downloaded From: http://journal.publications.chestnet.org/ on 02/06/2015 bances confined to REM sleep in patients with a global respiratory disturbance index ⬍ 10.1 To the first hypothesis of a state-specific sleep disorder expression of sleep fragmentation limited to REM sleep,1 data have not confirmed a major impact of REM respiratory events on diurnal impairment,2,3 with REM-related SDB reflecting more a sleep disorder related to gender4 and severity of the disease2 than a specific sleep disorder inducing sleepiness. In the light of these contradictory results, the aim of the present study was to evaluate the frequency and the clinical and polysomnographic aspects of patients presenting with REM-related SDB. A second aim was to assess whether specific Clinical Investigations daytime complaints, clinical aspects, and polysomnographic features differentiate these patients from those having respiratory disturbances in all sleep stages. Materials and Methods Subjects From a computerized database of all patients undergoing polysomnography for suspected SDB at the Geneva University Hospital sleep laboratory between October 2000 and February 2004, 492 patients were identified. Patients were excluded for the following: (1) apnea-hypopnea index (AHI) ⬍ 5/h of total sleep time (TST) (n ⫽ 59); (2) previous treatment for SDB by continuous positive airway pressure therapy, surgery, and/or oral device (n ⫽ 1); (3) REM sleep ⬍ 15% of TST during nocturnal recording (n ⫽ 54), or if complete clinical data were unavailable (n ⫽ 23). Of the initial sample, 415 patients fulfilled the inclusion criteria (mean age, 54.1 ⫾ 12.1 years [mean ⫾ SD]; 73% men); mean body mass index (BMI) was 31.3 ⫾ 6.3 kg/m2. Globally, the patient had moderate-to-severe SDB (AHI, 34.1 ⫾ 25.5/h; range, 5.1 to 126.4/h). Patients were informed that some of the collected data would be used for research purposes, and they gave written informed consent. mean minimal Sao2, and the oxygen desaturation index (ODI). Apnea/hypopnea events were classified as central, obstructive, or mixed according to the absence or presence of breathing efforts. The AHI was defined as the number of apneas and hypopneas per hour of TST. According to standard recommendations,8 cases were stratified as mild (AHI during TST [AHI-TST] between 5/h and 15/h, n ⫽ 119), moderate (AHI-TST ⬎15/h to ⬍ 30/h, n ⫽ 108), and severe (AHI-TST ⬎30, n ⫽ 188). In order to define the presence of respiratory disorders predominantly confined to REM sleep, the AHI was also calculated during REM sleep (AHI-REM) and during non-REM sleep (AHI-NREM), and patients were classified as having REM SDB if the AHIREM/AHI-NREM ratio was ⬎ 2, and non-REM SDB if the AHI-REM/AHI-NREM ratio was ⱕ 2, according to a previous report.4 Sleepiness Assessment Subjective daytime sleepiness was assessed in all patients by the administration of the Epworth sleepiness scale (ESS).9 In patients willing to perform an objective measure of sleepiness, the maintenance wakefulness test (MWT) was performed according to standard criteria (n ⫽ 228).10 This was done by asking the patients to sit in a quiet, dark room and to try to stay awake for five sessions scheduled at 9 am, 11 am, 1 pm, 3 pm, and 5 pm. All tests were terminated 15 min after sleep onset or after 40 min without sleep, and a mean sleep latency was calculated by averaging the latencies to sleep for the five naps. Clinical Evaluation All patients underwent a detailed clinical interview with an experienced sleep specialist concerning the primary complaint motivating the consultation (ie, snoring, reported apneas, and sleepiness) and medical history, with special focus on cardiac and cerebrovascular disease, hypertension, obstructive or restrictive lung disease, metabolic disorders and psychiatric diseases. Actual drug intake including antihypertensives, antiarrythmics, hypolipemiants, hypoglicemiants, antidepressants, benzodiazepines, hypnotics, and neuroleptics was also considered. A semistructured clinical interview for assessing symptoms possibly related with a SDB (morning headache, fatigue, daytime sleepiness, witnessed apneas, snoring, cognitive difficulties, nycturia, disturbed sleep) was performed. Nocturnal Sleep Studies Polysomnography included seven EEGs, right and left electrooculograms, and one electromyogram of chin muscle for conventional sleep staging. Respiratory airflow was monitored with a nasal cannula connected to a pressure transducer (Protech2; Minneapolis, MN), thoracic and abdominal respiratory movements with piezoelectric strain gauges, and tracheal sound by microphone. Arterial oxygen saturation (Sao2) was continuously measured with a finger oximeter. Sleep was scored using the criteria of Rechtschaffen and Kales5 for epochs of 20 s by a scorer experienced in the use of standard guidelines. As indexes of sleep fragmentation, we considered the number of awakenings and the number of stage shifts combined to calculate a sleep fragmentation index (SFI) per hour of TST.6,7 Respiratory events were scored using standard criteria.8 Apneas were defined as the absence of airflow on the nasal cannula lasting ⬎ 10 s. Hypopneas were defined as a ⱖ 50% reduction in airflow from the baseline value lasting at least 10 s, or a clear amplitude airflow reduction lasting ⱖ 10 s and associated with either an oxygen desaturation of ⬎ 3% or an arousal. As indexes of nocturnal hypoxemia, we considered the minimal Sao2, the www.chestjournal.org Downloaded From: http://journal.publications.chestnet.org/ on 02/06/2015 Statistical Analysis Polygraphic and clinical findings in REM-related and non-REM– related SDB were compared using respectively the Mann-Whitney U test and the 2 test. Statistical significance was determined as p ⬍ 0.01 after Bonferroni correction. All statistical analysis were performed with statistical software (SPSS for Windows, version 10.0; SPSS; Chicago, IL). Results are reported as mean ⫾ SD. Results Parient Characteristics In the group of patients as a whole, 46.5% were referred for snoring, 30.3% for witnessed apneas, and 17.3% for daytime sleepiness. Detailed clinical interviews revealed a high percentage of patients presenting with habitual and loud snoring (88.9%), fatigue (66.3%), excessive daytime sleepiness (52.7%), nycturia (55.2%), and witnessed apneas (50.6%). A high proportion of patients had a history of cardiovascular (55.8%), metabolic (47.4%), or psychiatric illness (32.4%); 24.5% and 17.8% were receiving antihypertensive or antidepressant drugs, respectively (Table 1). As a whole, the patients had a mean ESS score of 9.4 ⫾ 4.9 (Table 2). In the subsample of 228 patients who underwent the MWT, mean sleep latency was 21.8 ⫾ 12.1 min. In order to ascertain if these patients were different from those without an objective sleepiness assessment, we compared both groups. Patients who performed the MWT CHEST / 128 / 5 / NOVEMBER, 2005 3351 Table 1—Anthropometric and Clinical Data of the Total SDB Patients, REM SDB Patients, and Non-REM SDB Patients* Variables Total (n ⫽ 415) REM SDB (n ⫽ 151) Non-REM SDB (n ⫽ 264) Patients Female gender Age, yr BMI, kg/m2 Neck circumference, cm Primary complaint Snoring Witnessed apnea Sleepiness Medical history Cardiovascular Psychiatric Lung disease Metabolic Neurologic Medications Antihypertensive Antidepressant Benzodiazepine-hypnotic 100 27 54.1 (12.1) 31.3 (6.3) 40.7 (5.7) 36.4 46.4 53 (11.6) 32.2 (6.8) 39.5 (6.6) 63.6 16.5† 55 (12.2) 30.8 (5.9) 41.4 (5)† 46.5 30.3 17.3 52.3 20.5 19.2 43 36.2† 15.4 55.8 32.4 6.8 47.4 3.6 54.2 39 6.5 46.3 4.6 57.9 29 6.3 49 2.8 24.5 17.8 20.6 26.4 17.8 27.7 24 17.5 16.4 *Data are presented as % or mean (SD). †p ⬍ 0.001, REM SDB vs non-REM SDB. were of similar age, BMI, and gender distribution, but they had a more severe SDB with higher AHI-TST (AHI, 40.2 ⫾ 26.1/h vs 29.2 ⫾ 24.9/h; p ⬍ 0.001), and complained more frequently of day- time sleepiness (p ⬍ 0.001), fatigue (p ⬍ 0.001), witnessed apneas (p ⬍ 0.01), snoring (p ⬍ 0.001), and perspiration (p ⬍ 0.01) when compared with patients without MWT evaluation. Table 2—Polysomnographic Data of the Total SDB Patients, REM SDB Patients, and Non-REM SDB Patients* Variables Total (n ⫽ 415) REM SDB (n ⫽ 151) Non-REM SDB (n ⫽ 264) TST, min Wake after sleep onset, min Stage 1, min Stage 2, min Stage 3–4, min Stage REM, min Sleep latency, min Sleep efficiency, % SFI, No./h Sleep time in dorsal position, min Sleep time in lateral position, min Periodic leg movement index, No./h AHI, No./h REM AHI, No./h Non-REM AHI, No./h Apnea duration, s Hypopnea duration, s Wake Sao2, % Mean minimal Sao2, % Minimal Sao2, % ODI, No./h MWT, min ESS score 415.3 (70.2) 98.5 (57.4) 74.5 (31.9) 221 (58.4) 51.8 (40.1) 67.9 (28.8) 10.4 (14.1) 78.1 (10.9) 139.8 (77.2) 183.5 (128.4) 230.8 (130.3) 11.6 (16.2) 34.1 (25.5) 37.9 (23.4) 30.3 (25.1) 18.1 (5.9) 15 (2.6) 93.1 (4.9) 88.4 (3.9) 77.8 (8.6) 21.9 (20.3) 21.8 (12.1)‡ 9.4 (4.9) 421.3 (70) 91 (53.4) 61.5 (22.1) 218 (53.1) 66.3 (40) 75.4 (29.1) 10.3 (12.8) 79.3 (10.8) 104.4 (38.3) 186 (131.6) 229.7 (134.9) 9 (12.7) 15.7 (9.2) 40.2 (20.9) 9.6 (7.9) 16.3 (5.7) 14.3 (2.2) 93.1 (7.7) 89.3 (3.2) 79.9 (6.8) 9.7 (7.7) 23.7 (10.7) 9.3 (4.7) 413.1 (69.4) 101.4 (58.7) 81.4 (34)† 223.1 (60.2) 44.5 (38.2)† 64 (27.4)† 10.6 (15.1) 77.5 (10.8) 158.1 (84.6)† 181.3 (126.8) 230.5 (128.3) 13.2 (17.6) 43.3 (25.9) 37.2 (24.5) 40.7 (24.3)† 19.1 (5.8)† 15.4 (2.8)† 93.1 (1.9) 87.9 (4.2)† 76.7 (9)† 27.9 (21.8)† 21.3 (12.5) 9.3 (5) *Data are presented as mean (SD). †p ⬍ 0.001, REM SDB vs non-REM SDB. ‡Total patients, n ⫽ 228; REM SDB patients, n ⫽ 67; non-REM SDB patients, n ⫽ 169. 3352 Downloaded From: http://journal.publications.chestnet.org/ on 02/06/2015 Clinical Investigations REM SDB vs non-REM SDB Table 1 shows the anthropometric and clinical characteristics of the patient groups. One hundred fifty-one patients (36.4%) presented with REM SDB; the remaining 279 patients (63.6%) were considered as having a SDB nondependent on sleep stage (ie, non-REM SDB), the AHI-REM/AHINREM ratios being 7.2 ⫾ 7.7 and 1.3 ⫾ 3.6, respectively (p ⬍ 0.001). REM SDB patients were slightly younger, had higher BMI, and had lower neck circumference; however, differences reaching statistical significance only for neck circumference (p ⬍ 0.001). While in the non-REM SDB group a clear male prevalence was present (83.5%), in the REM SDB group, 46.4% of cases were women and 53.6% were men. Compared to REM SDB, non-REM SDB patients were referred more frequently for witnessed breathing pauses during sleep (p ⬍ 0.001). No differences were found between groups as to snoring and daytime sleepiness as chief complaints. Detailed clinical interview did not reveal significant differences between groups as to incidence of morning headache, daytime sleepiness, cognitive difficulties, abnormal motor activity during sleep, nycturia, habitual snoring, or excessive nocturnal sweating. No significant differences were present in medical history for cardiovascular, neurologic, psychiatric, and metabolic disease between non-REM and REM SDB, and no difference was found for habitual drug intake. Table 2 shows the polysomnographic findings in REM SDB and non-REM SDB patients. The two groups differed significantly in all parameters of sleep continuity and sleep fragmentation, with nonREM SDB patients having lower amounts of slow wave sleep and REM sleep. Since body position could influence the occurrence of respiratory events, we calculated for the two groups the sleep time spent in back and lateral positions, with no significant difference found between groups (p ⫽ 0.7 and p ⫽ 0.95, respectively). Analysis of respiratory disturbances in the two groups revealed that non-REM patients had higher AHI-TST, more severe nocturnal hypoxemia indexes, and longer apneas and hypopneas. Despite differences in SDB severity, no difference in the EES score (p ⫽ 0.8) or in the mean sleep latency at the MWT (p ⫽ 0.1) was present between groups. As shown in Tables 1 and 2, there were no significant differences in the percentage of those receiving different types of medication in REM SDB and in non-REM SDB patients, and the amount of REM sleep was not different between groups. To see whether a possible effect of medication could explain our results, we analyzed data from patients without www.chestjournal.org Downloaded From: http://journal.publications.chestnet.org/ on 02/06/2015 treatment. Of the total group, 229 patients (55.1%) were completely free of medication, 76 patients (50.3%) in the REM SDB group, and 153 patients (57.3%) in the non-REM SDB group. Two hundred ninety-nine patients did not receive any psychotropic drug that could influence sleep parameters. Ninetynine patients presented with REM SDB, and 200 patients presented with non-REM SDB. Moreover, analysis of polysomnographic findings between patients with REM and non-REM SDB free of medication or without psychotropic drugs did not reveal significant differences. In particular, there were no differences in subjective sleepiness (p ⫽ 0.9) or objective sleepiness (p ⫽ 0.3) between REM SDB patients and non-REM SDB patients free of medication. REM SDB Characteristics in Groups of Varying Severity In order to assess whether the occurrence of REM SDB was related to the severity of disease, the incidence of REM SDB was assessed in the three groups of patients stratified on the basis of the AHI-TST (Table 3). A high incidence of REM SDB was found in mild cases (73.1%), with lower incidence in moderate cases (47.2%) and especially in severe cases (6.9%) [Fig 1]. No significant differences in age, BMI, and neck circumference were seen between REM and non-REM SDB among the different severity groups, except for the BMI that was greater in REM SDB in mild cases (p ⬍ 0.001) and moderate cases (p ⬍ 0.005). Considering the effect of gender, again the incidence of REM SDB was greater in women, representing, respectively, 48.3% and the 51% of the population in mild and moderate REM SDB cases. This gender difference was not found in severe cases, the male/female ratio being ⬎ 4:1 both in REM and non-REM SDB (Table 3, Fig 2). As far as clinical findings are concerned, no differences in initial complaints (snoring, witnessed apneas, sleepiness) and medical history for cardiovascular, lung, metabolic, neurologic or lung diseases, or drug intake (antihypertensives, antidepressants, benzodiazepines) were noted between REM SDB and non-REM SDB patients in the different groups stratified on the basis of disease severity. The detailed clinical interview also failed to identify any specific complaint usually associated with SDB, related to one or other group. No significant differences were found in frequency of morning headache, daytime tiredness or sleepiness, memory or concentration complaints, motor activity during sleep, witnessed apneas, nycturia, snoring, or nocturnal sweating. In all severity groups, neither the ESS nor the CHEST / 128 / 5 / NOVEMBER, 2005 3353 Table 3—Clinical, Anthropometric, and Polygraphic Findings of REM SDB and Non-REM SDB According to Severity of Disease* AHI 5 to 15/h AHI 15 to 30/h AHI ⬎ 30/h Variables REM SDB (n ⫽ 87) Non-REM SDB (n ⫽ 32) REM SDB (n ⫽ 51) Non-REM SDB (n ⫽ 57) REM SDB (n ⫽ 13) Non-REM SDB (n ⫽ 175) Patients Female gender Age, yr BMI, kg/m2 Neck circumference, cm TST, min Wake after sleep onset, min Stage 1, min Stage 2, min Stage 3–4, min Stage REM, min Sleep latency, min Sleep efficiency, % SFI, No./h Periodic leg movement index, No./h Apnea duration, s Hypopnea duration, s AHI, No./h REM AHI, No./h Non-REM AHI, No./h Wake Sao2, % Mean minimal Sao2, % Minimal Sao2, % ODI, No./h MWT, min ESS score 73.1 48.3 51.6 (12) 32.3 (6.9) 39.5 (5.6) 423.7 (66.2) 89.6 (53.2) 59 (22.6) 215.6 (51.7) 69 (43.1) 79.9 (28.4) 11 (14.9) 79.8 (10.5) 96.1 (33.3) 8.8 (13.8) 15.3 (6.3) 14.1 (2.4) 9.2 (2.9) 27.8 (12.5) 4.8 (2.7) 92.6 (10.2) 89.5 (3.4) 81.2 (6.4) 6.6 (4.7) 24.3 (9.8) 9.6 (4.5) 26.9 9.3† 50.6 (12.4) 26.8 (3.7)† 40.1 (2.6) 426.9 (62.3) 72.3 (55.3) 68.2 (24.6) 217.4 (58.1) 63.6 (29.9) 77.5 (28.1) 8.3 (9.5) 82.7 (9.3) 114.5 (38.5) 9.4 (13.4) 15.5 (4.5) 13.9 (1.5) 10.3 (2.8) 7 (5.3)† 10 (3.1)† 94 (1.4) 90.9 (1.9) 84.6 (3.2)‡ 6.2 (5.8) 24.8 (9.7) 9.4 (4.1) 47.2 51 53.8 (10.4) 32.3 (7.2) 39.8 (6.6) 424.2 (70) 89.1 (49) 63.6 (21.1) 224.5 (54.8) 64.3 (33.5) 71.6 (28.6) 9.1 (9.4) 79.3 (10.2) 111.3 (41.2) 9 (11) 17.1 (4.5) 14.6 (1.8) 14.5 (5) 53.3 (15.7) 13.2 (5.5) 93.7 (1.3) 89.1 (2.9) 78.9 (7.1) 11.7 (7.4) 22.1 (10.4) 9.3 (5.1) 52.8 14† 52.2 (11.1) 29.1 (3.9)‡ 40.4 (2.9) 408.7 (67.7) 94.2 (50.9) 65.2 (27.3) 213.8 (63.6) 58.3 (27.7) 71.5 (25.4) 7.9 (8.6) 78.3 (10) 118.9 (40.6) 10.9 (15.7) 16.3 (4.1) 14.9 (2.4) 22.1 (4) 17.1 (12.5)† 22.2 (6.8)† 93.4 (1.4) 89.5 (2.4) 82.2 (4.7)‡ 12.4 (8.1) 22.7 (9.7) 9.2 (4.8) 6.9 15.4 59 (11.2) 31.4 (4.9) 38.5 (11.8) 394 (92.2) 108 (70.4) 70.1 (21.6) 207.9 (57.2) 56.2 (43) 59.7 (30.2) 10 (8.7) 76.2 (15.4) 133.1 (41.1) 10.6 (11.9) 19 (4.9) 14.3 (2.1) 36.5 (6) 71.5 (20.6) 28 (3.7) 93.5 (1.6) 88.3 (1.9) 75.6 (5.7) 23.5 (7.9) 28.2 (13.8) 8.1 (4.8) 92.1 17.7 56.3 (12.4) 32.1 (6.3) 42 (5.8) 410 (72.5) 111.1 (60.5) 89.9 (35.1) 226.5 (61) 35.1 (39.3) 58.4 (27.1) 11.7 (17) 76 (11.2) 181.8 (94.9) 14.5 (18.9) 20.6 (5.9) 15.8 (3) 58.2 (21)† 48.4 (21)† 54.6 (19.4)† 92.9 (2.1) 86.7 (4.6) 73.3 (9.4) 38.4 (20.8)§ 20.2 (13.4) 9.4 (5.2) *Data are presented as % or mean (SD). †p ⬍ 0.001, REM SDB vs non-REM SDB inside different severity groups. ‡p ⬍ 0.005, REM SDB vs non-REM SDB inside different severity groups. §p ⬍ 0.001, REM SDB vs non-REM SDB inside different severity groups. mean sleep latency on the MWT differed between REM and non-REM SDB patients. Table 3 reports the polysomnographic findings for REM SDB and non-REM SDB patients according to severity of disease. No significant differences in all analyzed sleep variables were found between groups, including amount of REM sleep. No significant differences in the AHI-TST and indexes of nocturnal hypoxemia were present between REM SDB and non-REM SDB in mild and moderate cases except for the minimal Sao2 value, which was lower in REM SDB (p ⬍ 0.005). In severe cases, the AHI-TST (p ⬍ 0.001) and the ODI (p ⬍ 0.01) were greater in non-REM SDB patients. As expected, AHI-REM was higher in REM SDB than in non-REM SDB patients in the three severity groups (p ⬍ 0.001). Discussion The aim of the current study was to determine whether clinical and polysomnographic variables dif3354 Downloaded From: http://journal.publications.chestnet.org/ on 02/06/2015 ferentiate REM SDB patients in a relatively large group with different degrees of SDB severity. The major results of the study are as follows: (1) neither clinical history nor daytime sleepiness differentiates patients with and without respiratory disturbances confined to REM sleep; (2) REM SDB is a sleep disorder more common in mild and moderate cases, no sleep stage effect having been found in severe cases; and (3) the prevalence of REM SDB is relatively the same in women and men, in contrast to the strong male predominance generally described in SDB.11,12 These results suggest that REM SDB is more a sleep-related breathing disorder linked to gender and to the severity of the disease, rather than a specific breathing disorder inducing sleepiness. The first finding of our study was that despite the fact that REM and non-REM sleep are functionally distinct sleep states, no differences in clinical presentation and sleepiness were found in our patients. Subjective and objective daytime sleepiness were consistently similar between REM and non-REM SDB patients, and complaints of sleepiness did not Clinical Investigations Figure 1. Percentage of patients with REM SDB and non-REM SDB in the three groups of patients stratified according to disease severity. A high incidence of REM SDB is found in mild and moderate cases. differentiate REM SDB. These results are partially in contrast with the first description of the disorder,1 in which the AHI during REM predicted the objective and subjective sleepiness of the patients, at least in patients with mild SDB. This could be explained by some differences in criteria applied to define REM SDB and in the assessment of sleepiness. Firstly, we considered patients with a wide range of SDB severity, while Kass et al1 examined only patients with clinically suspected SDB having AHITST ⬍ 10/h. In order to see if a population sample could explain the above differences, we extracted from our group patients with AHI-TST ⬍10/h, and we applied the criteria of Kass and coworkers1 to compare REM-SDB, ie, patients with AHI-REM ⱖ 15/h to non-REM SDB patients, ie, those with AHI-REM ⬍ 15/h. Sixty-six patients in our sample had AHI-TST ⬍10/h, 53 cases defined as REM SDB and 13 cases defined as non-REM SDB according to criteria of Kass and coworkers.1 Comparison between these subgroups confirmed the greater prevalence of women in the REM SDB group (50.9%), without, however, any differences for anthropometric, clinical, and polygraphic findings. Moreover, patients with AHI-REM ⱖ 15/h were not more sleepy than patients with AHI-REM ⬍ 15/h, with no significant difference found for sleep latency at the MWT (p ⫽ 0.16), ESS score (p ⫽ 0.4), or the complaints of sleepiness (p ⫽ 0.6) or fatigue (p ⫽ 0.55). Thus we can conclude that the range of severity and the sample population alone could not explain the differences in the results. Second, while Kass et al1 used the multiple sleep latency test, objective sleepiness was assessed by means of the MWT in our sample. Although the use of a different method to assess sleepiness could affect results, we believe that this is unlikely to be a factor contributing to different results. In fact, in line with our results, two extensive studies2,3 considering the influence of sleep stage on daytime sleepiness using the multiple sleep latency test have shown that sleep fragmentation limited to REM sleep has no specific impact on diurnal sleepiness. This is also confirmed by experimental data using acoustically induced clustered sleep fragmentation, which reproduces in some ways the sleep alterations found in REM SDB.13 In line with our results, the authors13 did not find any difference in daytime sleepiness, mood, and cognitive functions, suggesting that REM SDB should not be considered a specific sleep-state breathing disorder inducing greater sleepiness. The second interesting finding is that REM SDB appears to occur more frequently in mild-to-moderate cases with an equal incidence in men and in Figure 2. Percentage of male and female patients with REM SDB (left panel) and non-REM SDB (right panel) stratified according to disease severity. The male/female ratio is constant in non-REM SDB among the different severity groups. In REM SDB, the male/female ratio is approximately 1:1 in mild and moderate cases. www.chestjournal.org Downloaded From: http://journal.publications.chestnet.org/ on 02/06/2015 CHEST / 128 / 5 / NOVEMBER, 2005 3355 women, as opposed to a higher prevalence of male subjects with non-REM SDB. This finding replicates the study of O’Connor et al,4 showing a high prevalence of REM SDB in women and in mild-tomoderate cases. The lack of a greater daytime sleepiness in REM SDB and the equal prevalence in women and in men and in mild-to-moderate cases opens discussion as to whether REM SDB really is a distinct clinical entity or whether it reflects the natural progression of the disease. Since neither clinical history, polysomnographic data, nor indexes of daytime sleepiness differentiate REM SDB from non-REM SDB in a sample larger than that firstly described,1 we believe that the existence of the disease as a specific entity could be discarded. We therefore suggest that occurrence of REMrelated SDB may be suspected more frequently in women and in patients in whom clinical and polygraphic findings suggest a mild-to-moderate severity. An attractive hypothesis is that REM SDB may represent the clinical spectrum of the disease, beginning with intermittent apneas predominantly during REM sleep, in stages 0 and 1 of the hypothesis of Lugaresi et al,14 and affecting all sleep stages when the disease progresses. This could also explain why, in untreated patients prospectively examined,15–17 the deterioration of the disease is significantly greater in mild-to-moderate cases and in men compared to women.17 There are several limitations to our study that should be keep in mind. First, this is a retrospective study, with all the biases related to such clinical recruitment and referral patterns. However, we think that we can consider our population as clinically representative of the disease, all patients referred for suspected SBD during a specific period being studied. Second, our clinical assessment was based on the medical interview, focusing on subjective complaints such as fatigue and sleepiness, and on nocturnal symptoms. Therefore, we cannot exclude that subtle changes in other diurnal consequences such as cognitive functions could have gone undetected by clinical interview, more specific tests being necessary to allow a better identification of the clinical impact of predominant respiratory events in REM. Third, the criteria we used to define REM SDB (AHI-REM/AHI-NREM ratio ⬎ 2) is somewhat arbitrary. However, in the absence of formally established criteria, we applied strictly the criteria previously proposed.4 The use of other cutoff values reduced considerably the size of the REM SDB groups (particularly in the most severe group) without changing the main conclusions of the present study. Fourth, we know that sleep position can influence occurrence of respiratory events, with back position frequently inducing appearance or worsen3356 Downloaded From: http://journal.publications.chestnet.org/ on 02/06/2015 ing of respiratory events. Although we did not calculate for non-REM and REM sleep the time spent in each position, we found no significant difference between groups concerning the sleep time spent in both positions, suggesting that sleep position alone did not affect our results. Finally, we did not have an objective assessment of sleepiness in all patients, and patients undergoing the MWT complained more frequently of sleepiness and differed in terms of severity of the disease. Nevertheless, a significant number of patients in the different groups underwent the MWT, allowing us a sufficient comparison between REM SDB and non-REM SDB. In conclusion, after analyzing the clinical and polysomnographic features of a large group of patients with SDB, we found that REM SDB is frequent in mild-to-moderate cases and its prevalence is similar in women and in men. The occurrence of respiratory disturbances in REM sleep does not seem to affect initial complaints, medical history, and daytime sleepiness, and therefore could not be considered a specific form of SDB. Whether the occurrence of REM SDB reflects only the over-time progression of the disease needs to be confirmed in prospective studies. ACKNOWLEDGMENT: The authors are grateful to B. Adjivon, E. Claudel, D. Grasset, and A. Lalji for technical assistance. References 1 Kass JE, Akers SM, Bartter TC, et al. Rapid-eye-movementspecific sleep-disordered breathing: a possible cause of excessive daytime sleepiness. Am J Respir Crit Care Med 1996; 154:167–169 2 Chervin RD, Aldrich MS. The relation between multiple sleep latency test findings and the frequency of apneic events in REM and non-REM sleep. Chest 1998; 113:980 –984 3 Punjabi NM, Bandeen-Roche K, Marx JJ, et al. The association between daytime sleepiness and sleep-disordered breathing in NREM and REM sleep. Sleep 2002; 25:307–314 4 O’Connor C, Thornley KS, Hanly PJ. Gender differences in the polysomnographic features of obstructive sleep apnea. Am J Respir Crit Care Med 2000; 161:1465–1472 5 Rechtschaffen A, Kales A. A manual of standardized terminology, technique and scoring system for sleep stages of human sleep. Los Angeles, CA: Los Angeles Brain Information Service, Brain Information Institute, UCLA, 1968 6 Morrell MJ, Finn L, Kim H, et al. Sleep fragmentation, awake blood pressure, and sleep-disordered breathing in a population-based study. Am J Respir Crit Care Med 2000; 162: 2091–2096 7 Haba-Rubio J, Ibanez V, Sforza E. An alternative measure of sleep fragmentation in clinical practice: the sleep fragmentation index. Sleep Med 2004; 5:577–581 8 ASDA. Sleep-related breathing disorders in adults: recommendations for syndrome definition and measurement techniques in clinical research. Sleep 1999; 22:667– 689 9 Johns MW. A new method for measuring daytime sleepiness: the Epworth Sleepiness Scale. Sleep 1991; 14:540 –545 10 Doghramji K, Mitler MM, Sangal RB, et al. A normative study of the maintenance of wakefulness test (MWT). ElecClinical Investigations tronceph. Clin Neurophysiol 1997; 103:554 –562 11 Block AJ, Boysen PG, Wynne JW, et al. Sleep apnea, hypopnea and oxygen desaturation in normal subjects: a strong male predominance. N Engl J Med 1979; 300:513–517 12 Young T, Palta M, Dempsey J, et al. The occurrence of sleep-disordered breathing among middle-aged adults. N Engl J Med 1993; 328:1230 –1235 13 Martin SE, Brander PE, Deary IJ, et al. The effect of clustered versus regular sleep fragmentation on daytime function. J Sleep Res 1999; 8:305–311 14 Lugaresi E, Mondini S, Zucconi M, et al. Staging of heavy www.chestjournal.org Downloaded From: http://journal.publications.chestnet.org/ on 02/06/2015 snorers’ disease: a proposal. Bull Eur Physiopathol Respir 1983; 19:590 –594 15 Svanborg E, Larson H. Development of nocturnal respiratory disturbance in untreated patients with obstructive sleep apnea syndrome. Chest 1993; 104:340 –343 16 Sforza E, Addati G, Cirignotta F, et al. Natural evolution of sleep apnoea syndrome: a five year longitudinal study. Eur Respir J 1994; 7:1765–1770 17 Pendlebury ST, Pepin JL, Veale D, et al. Natural evolution of moderate sleep apnoea syndrome: significant progression over a mean of 17 months. Thorax 1997; 52:872– 878 CHEST / 128 / 5 / NOVEMBER, 2005 3357
© Copyright 2026