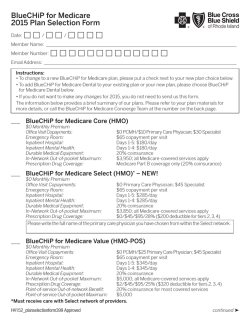
2015 Health Plans - Independence Blue Cross
2015 Health Plans 2-50 Employees Platinum Gold Silver Bronze Table of contents Blue Solutions for small business employers �������������������������������������������� 1 Your 2015 Blue Solutions plan guide ������������������������������������������������������� 2 What’s new and important for 2015�������������������������������������������������������� 3 Flexible health plan options to meet your needs ���������������������������������������� 4 Learn about affordable and innovative plan options���������������������������������� 5 More ways your employees can save on health care costs�������������������������� 8 Prescription drug coverage���������������������������������������������������������������������� 9 Vision coverage������������������������������������������������������������������������������������ 11 Pediatric dental coverage ��������������������������������������������������������������������� 12 Making health insurance easier for you and your employees �������������������� 13 2015 Benefits at a Glance......................................................................15 Platinum���������������������������������������������������������������������������������������������� 16 Gold���������������������������������������������������������������������������������������������������� 20 Silver��������������������������������������������������������������������������������������������������� 26 Bronze������������������������������������������������������������������������������������������������� 32 Important plan details ������������������������������������������������������������������������� 35 Underwriting information �������������������������������������������������������������������� 36 Blue Solutions for small business employers ® Your employees are your most valuable asset, and providing health insurance is one of the most important things you can do for them and their families. With Blue Solutions, you can choose from a suite of products specially designed for small businesses. And because no two businesses are alike, we give you a wide range of options to choose from so you can find the health plans that meet your needs at the price that’s right for your business. Everything you need to get started is here. With this brochure, you’ll be able to: • Find out what’s new and important for 2015 • Learn about our most innovative and affordable health plans • Understand • Discover how our health plans work the details of our health plans • Read important information about our health plans and underwriting process 1 Your 2015 Blue Solutions plan guide As your partner in health care, Independence Blue Cross (IBC) is committed to providing innovative solutions that enhance the health and wellness of you and your employees. Part of that commitment is to help you navigate through health care reform. Comprehensive coverage Regardless of the metallic levels, all products cover essential health benefits like doctor visits, prescription drugs, X-rays, and hospital stays. For 2015, our comprehensive Blue Solutions health plans have been updated to comply with the most recent Affordable Care Act (ACA) requirements. All plans will continue to be arranged by metallic levels of coverage (platinum, gold, silver, and bronze), which makes it easier to find plans that are right for your business and your budget. The chart below shows how the metallic levels compare on coverage and costs. P G S B Platinum Gold Silver Bronze Monthly cost $$$$ $$$ $$ $ Cost of care $ $$ $$$ $$$$ plan to use a lot of health care services want to save on monthly premiums while keeping out-of-pocket costs low need to balance monthly premium with out-ofpocket costs don’t plan to need a lot of health care services Good option if you … 2 What’s new and important for 2015 • Deductible limitations have been removed. This means that deductible amounts on certain plans have changed. See specific plan details which begin on page 15. • Out-of-pocket maximum limits have been updated. In-network out-ofpocket maximums have been raised to $6,600/$13,200 on certain non HSA-qualified plans. For HSA-qualified plans, in-network out-of-pocket maximums have been raised to $6,450/$12,900. Once this limit is reached, all covered benefits are covered in-network 100 percent by the health plan. All coinsurance, copays, and deductibles for essential health benefits accrue to the plan’s overall out-of-pocket maximum. See specific plan details which begin on page 15. • New low-cost health plan available. If you’re looking to continue offering your employees a plan with comprehensive benefits that fits within your budget, take a look at our new HMO Bronze Basic plan. The plan is ACA-compliant and offers full access to our Keystone HMO network at an affordable price. Note: This health plan does not include coverage for routine adult vision exams or eyewear. • Access to low-cost retail generic prescription drugs. For most plans, $7 is the most your employees will pay for generic prescription drugs. For select health plans, your employees must meet their deductible first before the copay applies. For Keystone HMO Proactive plans, the copay for generic drugs is $4 for preferred generics and $15 for all other generic drugs. No cost sharing is required at participating retail and mail order pharmacies for certain designated preventive drugs, prescription and over the counter (with a doctor’s prescription). For more information about our comprehensive prescription drug plans, see page 9. • More dollars to spend at Visionworks.1 Your employees get even more dollars to spend when they purchase frames at a Visionworks store. See page 11 for more details. • HRA plans with $0 employer contribution no longer offered. We will continue to offer plans that can be paired with HRAs. However, we will no longer offer the following plans that do not include an employer contribution amount – PPO Gold HRA, PPO Silver HRA, PPO Bronze Premier HRA, and PPO Bronze HRA. If you offered your employees one of these plans in 2014, we will assist you in selecting a comparable plan for 2015. 1. An affiliate of Independence Blue Cross has a financial interest in Visionworks. 3 Flexible health plan options to meet your needs PPO, Direct POS, and HMO plans There are three main types of plans you can choose from – PPO, Direct POS, and HMO. Each product type is offered across metallic levels at various price points, so your choice is all about how much flexibility you want to give your employees when they receive covered services. • Personal Choice® PPO plans provide the ultimate in flexibility. Your employees get in-network coverage across the country when using participating BlueCard® PPO providers and coverage out-of-network. Plus, your employees won’t need referrals to visit specialists. • Keystone Direct POS provides both in and out-of-network coverage, but your employees select a primary care physician (PCP) and only need referrals for certain services, which helps keep costs down. • Keystone HMO plans require employees to select a PCP to coordinate all of their care with network providers. Take a look at how the plans compare. KEYSTONE HMO KEYSTONE DIRECT POS PERSONAL CHOICE Access to network of more than 60,000 physicians and specialists X X X Selection of a PCP required X X No referrals needed to visit in-network specialists X2 In-network benefits coast-tocoast through BlueCard PPO X X Away from Home Care® program for employees who temporarily reside outside the service area X X Emergency and urgent care access across the country and around the world through BlueCard PPO and BlueCard Worldwide X X X 2. D irect POS employees need a referral from their PCP for spinal manipulations, routine X-rays, and physical/occupational therapy. For lab work, employees should use the facility recommended by their PCP for the lowest out-of-pocket costs. 4 Learn about affordable and innovative plan options While our bronze plans work well for employees who want a more affordable “just in case” plan, we also have a number of cost-saving options across all metallic levels so your employees can choose the amount of coverage they need. You can select from plans that include health spending accounts, like a Health Savings Account (HSA) or a Health Reimbursement Account (HRA), or try Keystone HMO Proactive – our plans with a tiered network. Lower your costs and take advantage of tax savings with HSA and HRA plans Blue Solutions HSA and HRA plans give you flexible options when you’re looking to lower health care costs and offer your employees top-quality health coverage. They help you: • Save on premium. High-deductible health plans offer access to our Personal Choice PPO network at a lower premium. • Save on taxes. There are potential tax advantages for you and employees because contributions to an HSA or HRA are not treated as taxable income if used for qualified medical expenses. • Encourage employees to become savvy health care consumers. Employees play a greater role in managing their health care purchases and using covered services appropriately. Managing your spending accounts has never been easier For employers • Integrated, streamlined enrollment process • Easy access to account information including online reporting • Convenient funding options • No monthly account fee • No pre-funding for HRA For employees • Direct-pay-to-provider • Automated reimbursements • Pay claims quickly • Pharmacy-only debit cards for covered members The BlueSaver℠ HSA through Bank of America™ Our BlueSaver HSA offers employees all of the advantages of an HSA through Bank of America, and independent company, along with claim and payment integration to make account management easy. The interest-bearing account includes a wide variety of investment options once the balance reaches $500 to help maximize savings year after year. And, there is no monthly account fee for as long as employees remain enrolled in a qualified IBC plan. 5 Comparing Blue Solutions HSA and HRA plans HSA HRA What is it? A bank account which is paired with a qualified high deductible health plan, to help employees save money to pay for future qualified medical expenses on a tax-free basis. An employer-funded medical reimbursement account used to pay current qualified medical expenses and save for future qualified medical expenses. How is it funded? Employee and/or employer Employer only What are the employer contribution amounts? Please refer to Benefits at a Glance section beginning on page 15 for plan details. Please refer to Benefits at a Glance section beginning on page 15 for plan details. How much can employees contribute to the account? The total annual contributions from all sources cannot exceed IRS guidelines.3 For 2015, the maximum contribution is $3,350 for self only, $6,650 for family. There is also an optional “catch-up” contribution of $1,000 for individuals 55 or older. N/A Who owns the account? Employee Employer. Any balances left at the end of the plan year or when an employee leaves the company remain with the employer. Do funds carry over? Yes, funds and any interest or investment earnings roll over to use for qualified medical expenses in subsequent years. No What are the tax implications?4 Contributions are generally excluded from an employee’s gross income. Interest and earnings from investments are tax-free. Future withdrawals are tax-free provided that they are for qualified medical expenses. Taxes and penalties apply for non-qualified reimbursements. Employer contributions are tax deductible to the employer and generally excluded from an employee’s gross income. What type of deductible does the plan have? Aggregate deductible: For family coverage, the entire family annual deductible must be met before copayments or coinsurance is applied for any individual family member. Embedded deductible: Each covered family member only needs to satisfy his or her individual deductible, not the entire family deductible, prior to receiving plan benefits. 3. Details available at www.irs.gov. 4. IBC does not provide legal or tax advice. You should consult with your own legal and/or tax advisor regarding the tax advantages of an HRA or HSA. 6 Tiered network plans – Keystone HMO Proactive Keystone HMO Gold and Silver Proactive, our tiered network plans, offer your employees full access to the Keystone network at a lower premium. As with any HMO plan, the member will select a PCP who will refer them to specialists. Your employees can save even more money by choosing certain health care providers when they seek care. Online Provider Finder Your employees can find out which tier their doctor is in by using the online Provider Finder. ibx.com/providerfinder How Keystone HMO Proactive works All Keystone HMO providers are grouped into one of three tiers based on cost and, in many cases, quality measures. The three tiers are: Tier 1 – Preferred, Tier 2 – Enhanced, and Tier 3 – Standard. All doctors and hospitals in the Keystone HMO network are accessible in the Proactive plans. When your employees choose providers in Tier 1 – Preferred or Tier 2 – Enhanced, they will save on out-of-pocket costs each time they receive care for certain services. While all of the doctors and hospitals in our Keystone HMO network must meet high quality standards, some are able to offer the same services at a lower cost. The good news is that more than 50 percent of doctors and hospitals in the Keystone HMO provider network are in Tier 1 – Preferred, so your employees will have plenty of choices. Employees pay the same cost for select services Even though your employees can save money on certain health services by choosing Tier 1 – Preferred or Tier 2 – Enhanced providers, there are some health services that cost the same across all tiers, such as: • Preventive care • Emergency room • Emergency ambulance • Urgent care • Outpatient labs • Prescription drugs • Pediatric dental and vision • Mental health • Physical and occupational therapy • Outpatient lab and pathology • Routine radiology • Spinal manipulations Remember: All doctors and hospitals in the Keystone HMO network are accessible in the Proactive plans. Save on quality care The cost of covered services varies across tiers. Your employees will have access to quality care at a lower cost when they choose a provider in Tier 1 - Preferred or Tier 2 – Enhanced. Is Keystone HMO Proactive right for your business and your employees? Before you decide to purchase one of the Proactive plans, you may want to consider a few key questions. 1. D o your employees live within our five-county service area or the contiguous counties? These plans are only available to employees who reside in our service area. 2. Are most of the Tier 1 – Preferred or Tier 2 – Enhanced hospitals conveniently located near your employees? Visit www.ibx.com/proactivehospitals to see a list of hospitals and their tiers. 3. Are your employees willing to change doctors if it will save them money? If you answered yes to these questions, Keystone HMO Proactive may be right for you and your employees. To see the Keystone HMO Proactive plan details, please refer to the Benefits at a Glance section beginning on page 15. 7 More ways your employees can save on health care costs Many of our health plans encourage employees to make more cost-effective choices when spending their health care dollars. Your employees can save on out-of-pocket costs when they visit certain providers for select services. $0 outpatient laboratory services at freestanding labs When your employees need blood work or other covered laboratory services, they will be covered in full as long as they use a freestanding lab in our network. If they choose to use a hospital-based lab, they will pay the costsharing designated in their Benefits at a Glance. To find an in-network freestanding lab, visit ibx.com/providerfinder. Note: This feature applies to PPO Platinum Premier, PPO Platinum, PPO Gold Premier, PPO Gold, and PPO Silver. $0 preventive colonoscopies from Preventive Plus designated providers Colorectal cancer is highly treatable when it’s detected early, which is why we cover preventive colonoscopies at $0 cost-sharing when your employees use one of our Preventive Plus designated providers. Our Preventive Plus providers are chosen based on cost and quality measures so that it’s easy for your employees to get high-quality care. In addition to $0 cost-sharing, Preventive Plus offers more convenience for employees, with sameday preliminary screening results and nearby screening centers. To find a Preventive Plus provider, visit ibx.com/providerfinder. Lower cost-sharing for outpatient surgery For certain plans, your employees will pay less by visiting in-network ambulatory surgical centers (ASC) when they require an outpatient surgical procedure. But as with any important health care matter, decisions should not be based on cost alone. Your employees should work with their health care providers to determine the best setting for the care they need. To see specific plan details, please reference Benefits at a Glance beginning on page 15. Both in-network ASCs and hospitals can be found by visiting ibx.com/providerfinder. 8 Prescription drug coverage Promoting better health Your Blue Solutions medical benefits include IBC Prescription Drug coverage.5 Your employees’ prescription drug benefit program provides many advantages to help your employees have access to covered prescription drugs prescribed by their doctor at an affordable cost. All Blue Solutions plans are designed to incent your employees to use the most cost-effective medications available. Convenient mail order pharmacy If your employee’s doctor has prescribed a medication that they’ll need to take regularly over a long period of time, the mail-order service is an excellent way to get a long-lasting supply and reduce out-of-pocket costs. Mail order is convenient and safe to use. If your employee chooses mail order, their doctor can prescribe a supply that will last up to 90 days. Employees can get three times as many doses of their maintenance medication at one time through mail order. Specialty Pharmacy Program Rx Online services Your employees can log on to ibxpress.com and click Manage My Prescription Drugs to take advantage of convenient features, such as: • Network pharmacy search • Formulary search • Claims information • Mail-order refill requests The Specialty Pharmacy Program is a convenient delivery system for specialty medications. Since specialty drugs require special handling, administration, and monitoring, these complex and costly medications may not be readily available at local pharmacies. With the Specialty Pharmacy Program, your employees’ medications will be delivered directly to their homes or to their doctors. In addition, your employees will have 24/7 access to clinical staff who will answer questions about specialty medications. Mandatory Generic Mandatory generic is featured in all Silver and Bronze Blue Solutions plans and our Keystone HMO Proactive plans as a way of providing coverage to your employees at a lower cost. Generic drugs are as effective as brand drugs and can save your employees money. If your employees choose to purchase a brand drug that is available in a generic form, they will be responsible for paying the dispensing pharmacy the difference between the negotiated discount price for the generic drug and the brand drug plus the appropriate cost-sharing for the brand drug. 5. Pharmacy benefits are administered by Futurescripts, a Catamaran company, an independent company providing pharmacy benefit management services. 9 Pharmacy Networks Participating pharmacies The FutureScripts® network includes more than 68,000 retail pharmacies. When traveling, your employees will find that most of the pharmacies in all 50 states accept their ID card and can fill their prescription for the same cost-sharing they pay at home, as long as they use a participating pharmacy. There is no need for employees to select just one pharmacy for their prescription needs. To locate a participating pharmacy, visit ibx.com and select Find a Pharmacy. FutureScripts Preferred Pharmacy Network Use of the preferred pharmacy network is required for all Silver and Bronze Blue Solutions plans and our Keystone HMO Proactive plans in order to provide coverage at a lower cost. This network is a subset of the national retail pharmacy network and includes over 50,000 pharmacies, including most major chains and local pharmacies, except Walgreens and Rite Aid stores. Non-participating pharmacies Out-of-network benefits apply to prescriptions filled at non-participating pharmacies. The employee must pay the full retail price for their prescription, then file a paper claim for partial reimbursement. 10 Vision coverage IBC Vision Care: The clear solution to your vision care needs6 When your employees visit their vision provider, they are getting more than just their eyes checked. Eye exams can help detect more serious medical conditions like diabetes, hypertension, or heart disease. Vision benefits could help reduce your company’s overall health care spending and increase employee productivity. To help your employees maximize their coverage, we provide enhanced adult vision benefits in most of our Blue Solutions plans. Now your employees can get an even richer benefit when visiting a Visionworks location, with a $150 frame allowance, while at other participating providers the frame allowance is $100. Visionworks and other providers provide a $100 contact lens allowance, as well as an annual routine eye exam at no cost. Conveniently located providers and value-added services The network includes more than 40,000 ophthalmologists, optometrists, and regional and national retailers, including Visionworks optical retail centers. Visionworks retail centers are conveniently located across the Philadelphia five-county area and surrounding states. With adult vision coverage, your employees can take advantage of: • No frame limitations. They have the freedom to use their frame allowance at any network location toward any frame on the market today. • Fully covered designer brands. They can select any frame from the Exclusive Frame Collection of over 200 of the latest, stylish, contemporary frames covered in full, or with a minimal copay. • One-year warranty. Every frame or lens purchased at a participating provider is backed by an unconditional one-year breakage warranty for repair or replacement. Your employees get even more through value-added services such as: • Contact lenses replacement. LENS123® will ship replacement contact lenses or solution anywhere the same day and employees are guaranteed low prices. • Vision correction discounts. Laser Vision Correction gives employees up to 25 percent off the participating provider’s usual and customary fees, or 5 percent off any participating provider’s advertised specials on laser vision corrections services. Pediatric Vision benefits Pediatric vision, an essential health benefit, is covered for your employees’ dependents up to age 19. These benefits include yearly eye care visits and a pair of eyeglasses every calendar year. These benefits can be used at Visionworks, which has one of the largest selections of eyeglasses especially designed for children. 6. IBC Vision Care is administered by Davis Vision, an independent company. 11 Pediatric dental coverage Pediatric Dental 7 is considered an essential health benefit. When you buy a Blue Solutions plan8 from IBC, it will include pediatric dental coverage for enrolled dependents up to age 19. Coverage includes preventive and diagnostic treatment that can help reduce the frequency and cost of expensive procedures. Pediatric Dental PPO included with PPO plans If you offer your employees a PPO plan — including plans with an HRA or HSA — those plans also include IBC Personal Choice pediatric dental coverage. The plan fully covers in-network dental exams and cleanings every six months to help maintain a child’s oral health. Your employees can choose a dental provider from the nationwide Concordia Advantage network. Dental options for adults Pediatric DHMO included with HMO and DPOS plans Visit www.ibx.com/sgdental to learn about your options for providing comprehensive dental coverage for adults. If you offer your employees an HMO or DPOS plan, those plans also include Keystone Health Plan East (KHPE) pediatric dental coverage. To obtain services, your employees will need to select a Primary Dental Office (PDO) from the KHPE DHMO network. PDO referral is required for specialist services. Diagnostic and preventive services, like exams and cleanings, are fully covered once every six months. More information on Pediatric Dental Benefits Pediatric dental benefits are in-network only and also include basic and major services, and medically necessary orthodontia. All coinsurance, deductibles, and copayments used for pediatric dental services will contribute toward the employee’s medical out-of-pocket expense. Network dentists can be found using the online dental directory at www.ibx.com. You can find descriptions of covered Pediatric Dental services and how much your employees have to pay for them by visiting www.ibx.com/sgdental. 7. Benefits administered by United Concordia, an independent company. 8. P lans offered through the small business health options program (SHOP) do not include pediatric dental coverage. 12 Making health insurance easier for you and your employees ibxpress.com for employers Running a small business means that you have a lot of responsibilities to juggle, so we make managing your health benefits as easy as possible. Whether you’re looking for account information or online billing, you get 24/7 access through ibxpress.com. Account Management features: • Add or delete an employee • Change • View employee or dependent information coverage history • Download • View forms your daily work log and transaction history eBilling and epayment features: • View current and prior invoices • Review • Get billing and payment history monthly billing reminders • Receive and pay invoices online ibxpress.com and IBX smartphone app for your employees Your employees can also access ibxpress.com, which is loaded with wellness tools and information to help your employees stay healthy. Whether they want to research symptoms, complete a health assessment, engage in an online lifestyle improvement program, or record and track important health information, ibxpress.com can help. Employees can use ibxpress.com to review their benefits, find a doctor or hospital, and check the status of claims. It’s free, secure, and convenient. IBX app makes it easy for employees to manage their health on the go Even if they aren’t near a computer, your employees can still access their benefits. They can download the free IBX app for their iPhone or Android to help them make the most of their health plan. The IBX app gives your employees easy access to their health care coverage 24/7, so they can: • View benefits and claim information • View temporary ID card information • View open referrals • View their Personal Health Record • Find a doctor • Estimate • Call Log in with the same username and password used for ibxpress.com the price of a drug customer service 13 Helping your employees make the most of their coverage We’re making it easier for your employees to get started using the online and mobile tools and resources that are available to help them maximize their benefits and save time. Your employees will receive an insert with their member ID card that directs them to visit www.ibx.com/start, where they can register or log in to ibxpress. A short video helps them learn about tools and resources at ibxpress to manage their benefits, estimate care costs, track spending, and make informed decisions about their health. The website also walks them through some of the most important ways they can start to make the most of their coverage, including how to find in-network doctors, learn what their plan covers, get covered services and use prescription drug benefits, and receive free, customized messages about their benefits on their smartphone. To deliver the most rewarding and positive member experience, we will regularly engage your employees through timely, relevant communications to help them understand their benefits and how to use them effectively. 14 2015 Benefits at a Glance Platinum health plans PPO Platinum Premier2 Benefits per contract year1 You pay in-network You pay out-of-network7 Deductible, individual/family $0 $2,000/$4,000 Coinsurance 0% 50% Out-of-pocket maximum, individual/family includes: $1,500/$3,000 coinsurance and copays $5,000/$10,000 coinsurance and ded Preventive care for adults and children $0 50% no ded Preventive colonoscopy for colorectal cancer screening - Preventive Plus providers $0 N/A Preventive colonoscopy for colorectal cancer screening - All other providers $750 50% no ded Primary care office visit/retail clinic $10 50% after ded Specialist office visit $20 50% after ded Urgent care $70 50% after ded Spinal manipulations (20 visits per year)9 $20 50% after ded $20 50% after ded Inpatient hospital services (includes maternity) $0 50% after ded Inpatient professional services (includes maternity) $0 50% after ded Emergency room (not waived if admitted) $100 $100 no ded Routine radiology/diagnostic $20 50% after ded MRI/MRA, CT/CTA scan, PET scan $175 50% after ded Biotech/specialty injectables $50 50% after ded Durable medical equipment/prosthetics 30% 50% after ded Mental health, serious mental illness & substance abuse - outpatient $20 50% after ded Mental health, serious mental illness & substance abuse - inpatient $0 50% after ded Ambulatory surgical facility $0 50% after ded Hospital-based $0 50% after ded Freestanding $0 50% after ded Hospital-based 50% 50% after ded Rx deductible (individual/family) $0 $0 Retail generic $7 Member pays 70% of retail Retail brand $40 Member pays 70% of retail Retail non-formulary brand $70 Member pays 70% of retail Pediatric routine eye exam25, 26 $0 Not covered Pediatric glasses $0 Not covered Adult routine eye exam26 $0 Not covered Allowance up to $150 for frames or $100 for contact lenses at Visionworks stores Not covered $50 Not covered $0 no ded Not covered 50% after ded Not covered Preventive services8 Physician services Physical/occupational therapy (30 visits per year) 9 Hospital/other medical services Outpatient surgery Outpatient lab/pathology Prescription drugs16, 17, 18, 19, 20 Additional benefits Vision24 25, 27 Adult eyewear (glasses or contacts) 28 Dental29 Pediatric dental deductible (per individual)30 Pediatric exams and cleanings 30, 31 Pediatric basic, major and orthodontia services 30, 32, 33 16 PPO Platinum2 DPOS Platinum Premier2 DPOS Platinum2 You pay in-network You pay out-of-network7 You pay in-network You pay out-of-network5 You pay in-network You pay out-of-network5 $0 $2,000/$4,000 $0 $2,000/$4,000 $0 $2,000/$4,000 0% 50% 0% 50% 0% 50% $2,000/$4,000 coinsurance and copays $5,000/$10,000 coinsurance and ded $2,000/$4,000 coinsurance and copays $5,000/$10,000 coinsurance and ded $3,000/$6,000 coinsurance and copays $5,000/$10,000 coinsurance and ded $0 50% no ded $0 50% no ded $0 50% no ded $0 N/A $0 N/A $0 N/A $750 50% no ded $750 50% no ded $750 50% no ded $15 50% after ded $10 50% after ded $15 50% after ded $30 50% after ded $20 50% after ded $30 50% after ded $70 50% after ded $70 50% after ded $70 50% after ded $30 50% after ded $2010 50% after ded $3010 50% after ded $30 50% after ded $20 50% after ded $30 50% after ded $100 per day11 50% after ded $0 50% after ded $100 per day11 50% after ded $0 50% after ded $0 50% after ded $0 50% after ded $100 $100 no ded $100 $100 no ded $100 $100 no ded $30 50% after ded $20 50% after ded $30 50% after ded $175 50% after ded $40 50% after ded $60 50% after ded $75 50% after ded $50 50% after ded $75 50% after ded 30% 50% after ded 50% 50% after ded 50% 50% after ded 50% after ded $20 50% after ded $30 $100 per day 50% after ded $0 50% after ded $100 per day 50% after ded $25 50% after ded $0 50% after ded $25 50% after ded $125 50% after ded $0 50% after ded $125 50% after ded $0 50% after ded $0 50% after ded $0 50% after ded 50% 50% after ded $0 50% after ded $0 50% after ded $0 $0 $0 $0 $0 $0 $7 Member pays 70% of retail $7 Member pays 70% of retail $7 Member pays 70% of retail $45 Member pays 70% of retail $40 Member pays 70% of retail $45 Member pays 70% of retail $75 Member pays 70% of retail $70 Member pays 70% of retail $75 Member pays 70% of retail $0 Not covered $0 Not covered $0 Not covered $0 Not covered $0 Not covered $0 Not covered $0 Not covered $0 Not covered $0 Not covered Allowance up to $150 for frames or $100 for contact lenses at Visionworks stores Not covered Allowance up to $150 for frames or $100 for contact lenses at Visionworks stores Not covered Allowance up to $150 for frames or $100 for contact lenses at Visionworks stores Not covered $50 Not covered $0 Not covered $0 Not covered $0 no ded Not covered $0 Not covered $0 Not covered 50% after ded Not covered Copay varies Not covered Copay varies Not covered $30 11 10 12 10 10 50% after ded 11 All footnotes listed on page 35 ded = Deductible 17 Platinum health plans (cont.) HMO Platinum Premier3 HMO Platinum3 Benefits per contract year1 You pay in-network6 You pay in-network6 Deductible, individual/family $0 $0 Coinsurance 0% 0% Out-of-pocket maximum, individual/family includes: $2,000/$4,000 coinsurance and copays $3,000/$6,000 coinsurance and copays Preventive care for adults and children $0 $0 Preventive colonoscopy for colorectal cancer screening - Preventive Plus providers $0 $0 Preventive colonoscopy for colorectal cancer screening - All other providers $750 $750 Primary care office visit/retail clinic $10 $15 Specialist office visit $20 $30 Urgent care $70 $70 Spinal manipulations (20 visits per year)9 $20 $30 $20 $30 Inpatient hospital services (includes maternity) $0 $100 per day11 Inpatient professional services (includes maternity) $0 $0 Emergency room (not waived if admitted) $100 $100 Routine radiology/diagnostic $20 $30 MRI/MRA, CT/CTA scan, PET scan $40 $60 Biotech/specialty injectables $50 $75 Durable medical equipment/prosthetics 50% 50% Mental health, serious mental illness & substance abuse - outpatient $20 $30 Mental health, serious mental illness & substance abuse - inpatient $0 $100 per day11 Ambulatory surgical facility $0 $25 Hospital-based $0 $125 Freestanding $0 $0 Hospital-based $0 $0 Rx deductible (individual/family) $0 $0 Retail generic $7 $7 Retail brand $40 $45 Retail non-formulary brand $70 $75 Pediatric routine eye exam25, 26 $0 $0 Pediatric glasses25, 27 $0 $0 $0 $0 Allowance up to $150 for frames or $100 for contact lenses at Visionworks stores Allowance up to $150 for frames or $100 for contact lenses at Visionworks stores Pediatric dental deductible (per individual)30 $0 $0 Pediatric exams and cleanings $0 $0 Pediatric basic, major and orthodontia services30, 32, 33 Copay varies Copay varies Preventive services8 Physician services Physical/occupational therapy (30 visits per year) 9 Hospital/other medical services Outpatient surgery Outpatient lab/pathology Prescription drugs16, 17, 18, 19, 20 Additional benefits Vision24 Adult routine eye exam 26 Adult eyewear (glasses or contacts) 28 Dental29 30, 31 18 PPO Platinum HSA 50 PPO Platinum HRA 50 Employer Contribution - $750 individual/$1,500 family4 You pay in-network Employer Contribution - $750 individual/$1,500 family4 You pay out-of-network7 You pay in-network You pay out-of-network7 $1,500/$3,000 $10,000/$20,000 $1,500/$3,000 $10,000/$20,000 0% 50% 0% 50% $6,450/$12,900 coinsurance, copays, and ded $20,000/$40,000 coinsurance and ded $6,450/$12,900 coinsurance, copays, and ded $20,000/$40,000 coinsurance and ded $0 no ded 50% no ded $0 no ded 50% no ded $0 no ded N/A $0 no ded N/A $750 no ded 50% no ded $750 no ded 50% no ded $0 after ded 50% after ded $0 after ded 50% after ded $0 after ded 50% after ded $0 after ded 50% after ded $0 after ded 50% after ded $0 after ded 50% after ded $0 after ded 50% after ded $0 after ded 50% after ded $0 after ded 50% after ded $0 after ded 50% after ded $0 after ded 50% after ded $0 after ded 50% after ded $0 after ded 50% after ded $0 after ded 50% after ded $0 after ded $0 after in-network ded $0 after ded $0 after in-network ded $0 after ded 50% after ded $0 after ded 50% after ded $0 after ded 50% after ded $0 after ded 50% after ded $0 after ded 50% after ded $0 after ded 50% after ded $0 after ded 50% after ded $0 after ded 50% after ded $0 after ded 50% after ded $0 after ded 50% after ded $0 after ded 50% after ded $0 after ded 50% after ded $0 after ded 50% after ded $0 after ded 50% after ded $0 after ded 50% after ded $0 after ded 50% after ded $0 after ded 50% after ded $0 after ded 50% after ded $0 after ded 50% after ded $0 after ded 50% after ded Integrated Integrated Integrated Integrated $7 after ded 50% after ded $7 after ded 50% after ded $40 after ded 50% after ded $40 after ded 50% after ded $60 after ded 50% after ded $60 after ded 50% after ded $0 after ded Not covered $0 after ded Not covered $0 after ded Not covered $0 after ded Not covered $0 after ded Not covered $0 after ded Not covered Allowance up to $150 for frames or $100 for contact lenses at Visionworks stores after ded Not covered Allowance up to $150 for frames or $100 for contact lenses at Visionworks stores after ded Not covered Integrated Not covered Integrated Not covered $0 no ded Not covered $0 no ded Not covered $0 after ded Not covered $0 after ded Not covered All footnotes listed on page 35 ded = Deductible 19 Gold health plans PPO Gold Premier2 Benefits per contract year1 You pay in-network You pay out-of-network7 Deductible, individual/family $0 $6,000/$12,000 Coinsurance 0% 50% Out-of-pocket maximum, individual/family includes: $5,000/$10,000 coinsurance and copays $18,000/$36,000 coinsurance and ded Preventive care for adults and children 0% 50% no ded Preventive colonoscopy for colorectal cancer screening - Preventive Plus providers $0 N/A Preventive colonoscopy for colorectal cancer screening - All other providers $750 50% no ded Primary care office visit/retail clinic $35 50% after ded Specialist office visit $70 50% after ded Urgent care $105 50% after ded Spinal manipulations (20 visits per year) $70 50% after ded Physical/occupational therapy (30 visits per year)9 $70 50% after ded Inpatient hospital services (includes maternity) $600 per day11 50% after ded Inpatient professional services (includes maternity) $0 50% after ded Emergency room (not waived if admitted) $150 $150 no ded Routine radiology/diagnostic $70 50% after ded MRI/MRA, CT/CTA scan, PET scan $175 50% after ded Biotech/specialty injectables $125 50% after ded Durable medical equipment/prosthetics 50% 50% after ded Mental health, serious mental illness & substance abuse - outpatient $70 50% after ded Mental health, serious mental illness & substance abuse - inpatient $600 per day11 50% after ded Ambulatory surgical facility $300 50% after ded Hospital-based $700 50% after ded $0 50% after ded 50% 50% after ded Rx deductible (individual/family) $0 $0 Retail generic $7 Member pays 70% of retail Retail brand $50 Member pays 70% of retail Retail non-formulary brand $75 Member pays 70% of retail Pediatric routine eye exam25, 26 $0 Not covered Pediatric glasses $0 Not covered Adult routine eye exam $0 Not covered Adult eyewear (glasses or contacts)28 Allowance up to $150 for frames or $100 for contact lenses at Visionworks stores Not covered $50 Not covered $0 no ded Not covered 50% after ded Not covered Preventive services8 Physician services 9 Hospital/other medical services Outpatient surgery Outpatient lab/pathology Freestanding Hospital-based Prescription drugs 16, 17, 18, 19, 20 Additional benefits Vision24 25, 27 26 Dental29 Pediatric dental deductible (per individual)30 Pediatric exams and cleanings 30, 31 Pediatric basic, major and orthodontia services 30, 32, 33 20 PPO Gold2 DPOS Gold Premier2 You pay in-network You pay out-of-network7 You pay in-network You pay out-of-network5 $1,000/$2,000 $7,500/$15,000 $0 $5,000/$10,000 10% 50% 0% 50% $5,000/$10,000 coinsurance and copays $25,000/$50,000 coinsurance and ded $6,600/$13,200 coinsurance and copays $15,000/$30,000 coinsurance and ded $0 no ded 50% no ded $0 50% no ded $0 no ded N/A $0 N/A $750 no ded 50% no ded $750 50% no ded $25 no ded 50% after ded $30 50% after ded $50 no ded 50% after ded $60 50% after ded 10% after ded 50% after ded $87 50% after ded $50 no ded $50 no ded 50% after ded $60 10 50% after ded 50% after ded $6010 50% after ded 10% after ded 50% after ded $500 per day11 50% after ded 10% after ded 50% after ded $0 50% after ded 10% after ded 10% after in-network ded $300 $300 no ded 10% after ded 50% after ded $6010 50% after ded 10% after ded 50% after ded $250 50% after ded $100 no ded 50% after ded $125 50% after ded 50% after ded 50% after ded 50% 50% after ded $50 no ded 50% after ded $60 50% after ded 10% after ded 50% after ded $500 per day11 50% after ded 10% after ded 50% after ded $300 50% after ded 10% after ded 50% after ded $500 50% after ded $0 no ded 50% after ded $0 50% after ded 50% after ded 50% after ded $0 50% after ded $0 $0 $0 $0 $7 Member pays 70% of retail $7 Member pays 70% of retail $50 Member pays 70% of retail $50 Member pays 70% of retail $75 Member pays 70% of retail $75 Member pays 70% of retail $0 no ded Not covered $0 Not covered $0 no ded Not covered $0 Not covered $0 no ded Not covered $0 Not covered Allowance up to $150 for frames or $100 for contact lenses at Visionworks stores Not covered Allowance up to $150 for frames or $100 for contact lenses at Visionworks stores Not covered $50 Not covered $0 Not covered $0 no ded Not covered $0 Not covered 50% after ded Not covered Copay varies Not covered All footnotes listed on page 35 ded = Deductible 21 Gold health plans (cont.) DPOS Gold2 Benefits per contract year1 You pay in-network You pay out-of-network5 Deductible, individual/family $1,000/$2,000 $7,500/$15,000 Coinsurance 10% 50% $6,600/$13,200 coinsurance, copays, and ded $25,000/$50,000 coinsurance and ded Preventive care for adults and children $0 no ded 50% no ded Preventive colonoscopy for colorectal cancer screening - Preventive Plus providers $0 no ded N/A Preventive colonoscopy for colorectal cancer screening - All other providers $750 no ded 50% no ded Primary care office visit/retail clinic13 $25 no ded 50% after ded Specialist office visit $50 no ded 50% after ded Urgent care 10% after ded 50% after ded Spinal manipulations (20 visits per year)9 $50 no ded10 50% after ded $50 no ded 50% after ded Inpatient hospital services (includes maternity) 10% after ded 50% after ded Inpatient professional services (includes maternity) 10% after ded 50% after ded Emergency room (not waived if admitted)14 10% after ded 10% after in-network ded Routine radiology/diagnostic $40 no ded 50% after ded MRI/MRA, CT/CTA scan, PET scan $80 no ded 50% after ded Biotech/specialty injectables $100 no ded 50% after ded Durable medical equipment/prosthetics 50% after ded 50% after ded Mental health, serious mental illness & substance abuse - outpatient $50 no ded 50% after ded Mental health, serious mental illness & substance abuse - inpatient 10% after ded 50% after ded Ambulatory surgical facility 10% after ded 50% after ded Hospital-based 10% after ded 50% after ded Freestanding $0 no ded 50% after ded Hospital-based $0 no ded 50% after ded Rx deductible (individual/family) $0 $0 Retail generic $7 Member pays 70% of retail Retail brand $50 Member pays 70% of retail Retail non-formulary brand $75 Member pays 70% of retail Pediatric routine eye exam25, 26 $0 no ded Not covered Pediatric glasses25, 27 $0 no ded Not covered $0 no ded Not covered Allowance up to $150 for frames or $100 for contact lenses at Visionworks stores Not covered Pediatric dental deductible (per individual)30 $0 Not covered Pediatric exams and cleanings30, 31 $0 Not covered Copay varies Not covered Out-of-pocket maximum, individual/family includes: 12 Preventive services8 Physician services Physical/occupational therapy (30 visits per year) 9 10 Hospital/other medical services 10 Outpatient surgery Outpatient lab/pathology Prescription drugs16, 17, 18, 19, 20 Additional benefits Vision24 Adult routine eye exam 26 Adult eyewear (glasses or contacts) 28 Dental29 Pediatric basic, major and orthodontia services 30, 32, 33 22 HMO Gold Premier3 HMO Gold2 Keystone HMO Gold Proactive2 You pay in-network6 You pay in-network6 You pay in-network6 Tier 1 - Preferred You pay in-network6 Tier 2 - Enhanced You pay in-network6 Tier 3 - Standard $0 $1,000/$2,000 $0 $0 $0 0% 10% 0%; unless otherwise noted 20%; unless otherwise noted 30%; unless otherwise noted $6,600/$13,200 coinsurance and copays $6,600/$13,200 coinsurance, copays, and ded $6,600/$13,200 coinsurance and copays $6,600/$13,200 coinsurance and copays $6,600/$13,200 coinsurance and copays $0 $0 no ded $0 $0 $0 $0 $0 no ded $0 $0 $0 $750 $750 no ded $750 $750 $750 $30 $25 no ded $15 $30 $45 $60 $50 no ded $40 $60 $80 $87 10% after ded $100 $100 $100 $60 $50 no ded $50 $50 $50 $60 $50 no ded $60 $60 $60 $500 per day11 10% after ded $350 per day11 $700 per day11 $1,100 per day11 $0 10% after ded 0% 20% 30% $300 10% after ded $400 $400 $400 $60 $40 no ded $60 $60 $60 $250 $80 no ded $120 $120 $120 $125 $100 no ded 50% 50% 50% 50% 50% after ded 50% 50% 50% $60 $50 no ded $40 $40 $500 per day 10% after ded $350 per day $350 per day $350 per day11 $300 10% after ded $150 $550 $1,000 $500 10% after ded $150 $550 $1,000 $0 $0 no ded $0 $0 $0 $0 $0 no ded $0 $0 $0 $0 $0 $021 $021 $021 $7 $7 $15 $15 $1521, 23 $50 $50 50% up to $200 max per prescription21, 22 50% up to $200 max per prescription21, 22 50% up to $200 max per prescription21, 22 $75 $75 50% up to $300 max per prescription21, 22 50% up to $300 max per prescription21, 22 50% up to $300 max per prescription21, 22 $0 $0 no ded $0 $0 $0 $0 $0 no ded $0 $0 $0 $0 $0 no ded $0 $0 $0 Allowance up to $150 for frames or $100 for contact lenses at Visionworks stores Allowance up to $150 for frames or $100 for contact lenses at Visionworks stores Allowance up to $150 for frames or $100 for contact lenses at Visionworks stores Allowance up to $150 for frames or $100 for contact lenses at Visionworks stores Allowance up to $150 for frames or $100 for contact lenses at Visionworks stores $0 $0 $0 $0 $0 $0 $0 $0 $0 $0 Copay varies Copay varies Copay varies Copay varies Copay varies 11 11 21, 23 $40 11 21, 23 All footnotes listed on page 35 ded = Deductible 23 Gold health plans (cont.) PPO GOLD HSA 254 PPO Gold HSA4 Employer Contribution $500 individual/$1,000 family Benefits per contract year1 You pay in-network You pay out-of-network7 You pay in-network You pay 0ut-of -network7 Deductible, individual/family $1,500/$3,000 $10,000/$20,000 $2,000/$4,000 $10,000/$20,000 Coinsurance 0% 50% 0% 50% Out-of-pocket maximum, individual/family includes: $6,450/$12,900 coinsurance, copays, and ded $20,000/$40,000 coinsurance and ded $6,450/$12,900 coinsurance, copays, and ded $20,000/$40,000 coinsurance and ded Preventive care for adults and children $0 no ded 50% no ded $0 no ded 50% no ded Preventive colonoscopy for colorectal cancer screening - Preventive Plus providers $0 no ded N/A $0 no ded N/A Preventive colonoscopy for colorectal cancer screening - All other providers $750 no ded 50% no ded $750 no ded 50% no ded Primary care office visit/retail clinic $0 after ded 50% after ded $0 after ded 50% after ded Specialist office visit $0 after ded 50% after ded $0 after ded 50% after ded Urgent care $0 after ded 50% after ded $0 after ded 50% after ded Spinal manipulations (20 visits per year) $0 after ded 50% after ded $0 after ded 50% after ded Physical/occupational therapy (30 visits per year)9 $0 after ded 50% after ded $0 after ded 50% after ded Inpatient hospital services (includes maternity) $0 after ded 50% after ded $0 after ded 50% after ded Inpatient professional services (includes maternity) $0 after ded 50% after ded $0 after ded 50% after ded Emergency room (not waived if admitted) $0 after ded $0 after in-network ded $0 after ded $0 after in-network ded Routine radiology/diagnostic $0 after ded 50% after ded $0 after ded 50% after ded MRI/MRA, CT/CTA scan, PET scan $0 after ded 50% after ded $0 after ded 50% after ded Biotech/specialty injectables $0 after ded 50% after ded $0 after ded 50% after ded Durable medical equipment/prosthetics $0 after ded 50% after ded $0 after ded 50% after ded Mental health, serious mental illness & substance abuse - outpatient $0 after ded 50% after ded $0 after ded 50% after ded Mental health, serious mental illness & substance abuse - inpatient $0 after ded 50% after ded $0 after ded 50% after ded Ambulatory surgical facility $0 after ded 50% after ded $0 after ded 50% after ded Hospital-based $0 after ded 50% after ded $0 after ded 50% after ded Freestanding $0 after ded 50% after ded $0 after ded 50% after ded Hospital-based $0 after ded 50% after ded $0 after ded 50% after ded Rx deductible (individual/family) Integrated Integrated Integrated Integrated Retail generic $7 after ded 50% after ded $7 after ded 50% after ded Retail brand $40 after ded 50% after ded $40 after ded 50% after ded Retail non-formulary brand $60 after ded 50% after ded $60 after ded 50% after ded Pediatric routine eye exam25, 26 $0 after ded Not covered $0 after ded Not covered Pediatric glasses25, 27 $0 after ded Not covered $0 after ded Not covered $0 after ded Not covered $0 after ded Not covered Allowance up to $150 for frames or $100 for contact lenses at Visionworks stores after ded Not covered Allowance up to $150 for frames or $100 for contact lenses at Visionworks stores after ded Not covered Integrated Not covered Integrated Not covered $0 no ded Not covered $0 no ded Not covered $0 after ded Not covered $0 after ded Not covered Preventive services8 Physician services 9 Hospital/other medical services Outpatient surgery Outpatient lab/pathology Prescription drugs16, 17, 18, 19, 20 Additional benefits Vision24 Adult routine eye exam 26 Adult eyewear (glasses or contacts) 28 Dental29 Pediatric dental deductible (per individual)30 Pediatric exams and cleanings30, 31 Pediatric basic, major and orthodontia services 30, 32, 33 24 PPO Gold HRA 252 PPO Gold HSA 504 PPO Gold HRA 502 Employer Contribution $500 individual/$1,000 family Employer Contribution $1,000 individual/$2,000 family Employer Contribution $1,000 individual/$2,000 family You pay in-network You pay out-of-network7 You pay in-network You pay out-of-network7 You pay in-network You pay out-of-network7 $2,000/$4,000 $10,000/$20,000 $2,000/$4,000 $10,000/$20,000 $2,000/$4,000 $10,000/$20,000 30% 50% 0% 50% 30% 50% $6,450/$12,900 coinsurance, copays, and ded $20,000/$40,000 coinsurance and ded $6,450/$12,900 coinsurance, copays, and ded $20,000/$40,000 coinsurance and ded $6,450/$12,900 coinsurance, copays, and ded $20,000/$40,000 coinsurance and ded $0 no ded 50% no ded $0 no ded 50% no ded $0 no ded 50% no ded $0 no ded N/A $0 no ded N/A $0 no ded N/A $750 no ded 50% no ded $750 no ded 50% no ded $750 no ded 50% no ded 30% after ded 50% after ded $0 after ded 50% after ded 30% after ded 50% after ded 30% after ded 50% after ded $0 after ded 50% after ded 30% after ded 50% after ded 30% after ded 50% after ded $0 after ded 50% after ded 30% after ded 50% after ded 30% after ded 50% after ded $0 after ded 50% after ded 30% after ded 50% after ded 30% after ded 50% after ded $0 after ded 50% after ded 30% after ded 50% after ded 30% after ded 50% after ded $0 after ded 50% after ded 30% after ded 50% after ded 30% after ded 50% after ded $0 after ded 50% after ded 30% after ded 50% after ded 30% after ded 30% after in-network ded $0 after ded $0 after in-network ded 30% after ded 30% after in-network ded 30% after ded 50% after ded $0 after ded 50% after ded 30% after ded 50% after ded 30% after ded 50% after ded $0 after ded 50% after ded 30% after ded 50% after ded 30% after ded 50% after ded $0 after ded 50% after ded 30% after ded 50% after ded 30% after ded 50% after ded $0 after ded 50% after ded 30% after ded 50% after ded 30% after ded 50% after ded $0 after ded 50% after ded 30% after ded 50% after ded 30% after ded 50% after ded $0 after ded 50% after ded 30% after ded 50% after ded 30% after ded 50% after ded $0 after ded 50% after ded 30% after ded 50% after ded 30% after ded 50% after ded $0 after ded 50% after ded 30% after ded 50% after ded 30% after ded 50% after ded $0 after ded 50% after ded 30% after ded 50% after ded 30% after ded 50% after ded $0 after ded 50% after ded 30% after ded 50% after ded Integrated Integrated Integrated Integrated Integrated Integrated $7 after ded 50% after ded $7 after ded 50% after ded $7 after ded 50% after ded $40 after ded 50% after ded $40 after ded 50% after ded $40 after ded 50% after ded $60 after ded 50% after ded $60 after ded 50% after ded $60 after ded 50% after ded $0 after ded Not covered $0 after ded Not covered $0 after ded Not covered $0 after ded Not covered $0 after ded Not covered $0 after ded Not covered $0 after ded Not covered $0 after ded Not covered $0 after ded Not covered Not covered Allowance up to $150 for frames or $100 for contact lenses at Visionworks stores after ded Not covered Allowance up to $150 for frames or $100 for contact lenses at Visionworks stores after ded Not covered Integrated Not covered Integrated Not covered Integrated Not covered $0 no ded Not covered $0 no ded Not covered $0 no ded Not covered 30% after ded Not covered $0 after ded Not covered 30% after ded Not covered Allowance up to $150 for frames or $100 for contact lenses at Visionworks stores after ded All footnotes listed on page 35 ded = Deductible 25 Silver health plans PPO Silver2 Benefits per contract year1 You pay in-network You pay out-of-network7 Deductible, individual/family $2,500/$5,000 $7,500/$15,000 Coinsurance 20% 50% Out-of-pocket maximum, individual/family includes: $6,000/$12,000 coinsurance, copays, and ded $25,000/$50,000 coinsurance and ded Preventive care for adults and children $0 no ded 50% no ded Preventive colonoscopy for colorectal cancer screening - Preventive Plus providers $0 no ded N/A Preventive colonoscopy for colorectal cancer screening - All other providers $750 no ded 50% no ded Primary care office visit/retail clinic $30 no ded 50% after ded Specialist office visit $60 no ded 50% after ded Urgent care 20% after ded 50% after ded Spinal manipulations (20 visits per year) $60 no ded 50% after ded Physical/occupational therapy (30 visits per year)9 $60 no ded 50% after ded Inpatient hospital services (includes maternity) 20% after ded 50% after ded Inpatient professional services (includes maternity) 20% after ded 50% after ded Emergency room (not waived if admitted) 20% after ded 20% after in-network ded Routine radiology/diagnostic 20% after ded 50% after ded MRI/MRA, CT/CTA scan, PET scan 20% after ded 50% after ded Biotech/specialty injectables $100 no ded 50% after ded Durable medical equipment/prosthetics 50% after ded 50% after ded Mental health, serious mental illness & substance abuse - outpatient $60 no ded 50% after ded Mental health, serious mental illness & substance abuse - inpatient 20% after ded 50% after ded Ambulatory surgical facility 20% after ded 50% after ded Hospital-based 20% after ded 50% after ded $0 no ded 50% after ded 50% after ded 50% after ded Rx deductible (individual/family) $0 $0 Retail generic $7 Preventive services8 Physician services 9 Hospital/other medical services Outpatient surgery Outpatient lab/pathology Freestanding Hospital-based Prescription drugs 16, 17, 18, 19, 20, 21 Member pays 70% of retail Retail brand 50% up to $125 max per prescription 22 Member pays 70% of retail22 Retail non-formulary brand 50% up to $250 max per prescription22 Member pays 70% of retail22 Pediatric routine eye exam25, 26 $0 no ded Not covered Pediatric glasses $0 no ded Not covered $0 no ded Not covered Allowance up to $150 for frames or $100 for contact lenses at Visionworks stores Not covered Pediatric dental deductible (per individual)30 $50 Not covered Pediatric exams and cleanings30, 31 $0 no ded Not covered 50% after ded Not covered Additional benefits Vision24 25, 27 Adult routine eye exam 26 Adult eyewear (glasses or contacts) 28 Dental29 Pediatric basic, major and orthodontia services 30, 32, 33 26 DPOS Silver Premier2 DPOS Silver2 You pay in-network You pay out-of-network5 You pay in-network You pay out-of-network5 $2,000/$4,000 $7,500/$15,000 $2,500/$5,000 $7,500/$15,000 30% 50% 40% 50% $6,600/$13,200 coinsurance, copays, and ded $25,000/$50,000 coinsurance and ded $6,600/$13,200 coinsurance, copays, and ded $25,000/$50,000 coinsurance and ded $0 no ded 50% no ded $0 no ded 50% no ded $0 no ded N/A $0 no ded N/A $750 no ded 50% no ded $750 no ded 50% no ded $25 no ded 50% after ded $30 no ded 50% after ded $50 no ded 50% after ded $60 no ded 50% after ded 30% after ded 50% after ded 40% after ded 50% after ded 10 $50 no ded 50% after ded 10 $60 no ded 50% after ded $50 no ded10 50% after ded $60 no ded10 50% after ded 30% after ded 50% after ded 40% after ded 50% after ded 30% after ded 50% after ded 40% after ded 50% after ded 30% after ded 30% after in-network ded 40% after ded 40% after in-network ded $50 no ded10 50% after ded $60 no ded10 50% after ded $100 no ded 50% after ded $120 no ded 50% after ded $100 no ded 50% after ded $100 no ded 50% after ded 50% after ded 50% after ded 50% after ded 50% after ded $50 no ded 50% after ded $60 no ded 50% after ded 30% after ded 50% after ded 40% after ded 50% after ded 30% after ded 50% after ded 40% after ded 50% after ded 30% after ded 50% after ded 40% after ded 50% after ded $0 no ded 50% after ded $0 no ded 50% after ded $0 no ded 50% after ded $0 no ded 50% after ded $0 $0 $0 $0 $7 Member pays 70% of retail $7 Member pays 70% of retail 50% up to $125 max per prescription Member pays 70% of retail 50% up to $250 max per prescription22 Member pays 70% of retail22 50% up to $250 max per prescription22 Member pays 70% of retail22 $0 no ded Not covered $0 no ded Not covered $0 no ded Not covered $0 no ded Not covered $0 no ded Not covered $0 no ded Not covered Allowance up to $150 for frames or $100 for contact lenses at Visionworks stores Not covered Allowance up to $150 for frames or $100 for contact lenses at Visionworks stores Not covered $0 Not covered $0 Not covered $0 Not covered $0 Not covered Copay varies Not covered Copay varies Not covered 22 22 50% up to $125 max per prescription 22 Member pays 70% of retail22 All footnotes listed on page 35 ded = Deductible 27 Silver health plans (cont.) HMO Silver Premier2 HMO Silver 2 Benefits per contract year1 You pay in-network6 You pay in-network6 Deductible, individual/family15 $2,000/$4,000 $2,500/$5,000 Coinsurance 30% 40% $6,600/$13,200 coinsurance, copays, and ded $6,600/$13,200 coinsurance, copays, and ded Preventive care for adults and children $0 no ded $0 no ded Preventive colonoscopy for colorectal cancer screening - Preventive Plus providers $0 no ded $0 no ded Preventive colonoscopy for colorectal cancer screening - All other providers $750 no ded $750 no ded Primary care office visit/retail clinic13 $25 no ded $30 no ded Specialist office visit $50 no ded $60 no ded 30% after ded 40% after ded Spinal manipulations (20 visits per year) $50 no ded $60 no ded Physical/occupational therapy (30 visits per year)9 $50 no ded $60 no ded Inpatient hospital services (includes maternity) 30% after ded 40% after ded Inpatient professional services (includes maternity) 30% after ded 40% after ded Emergency room (not waived if admitted)14 30% after ded 40% after ded Routine radiology/diagnostic $50 no ded $60 no ded MRI/MRA, CT/CTA scan, PET scan $100 no ded $120 no ded Biotech/specialty injectables $100 no ded $100 no ded Durable medical equipment/prosthetics 50% after ded 50% after ded Mental health, serious mental illness & substance abuse - outpatient $50 no ded $60 no ded Mental health, serious mental illness & substance abuse - inpatient 30% after ded 40% after ded Ambulatory surgical facility 30% after ded 40% after ded Hospital-based 30% after ded 40% after ded Freestanding $0 no ded $0 no ded Hospital-based $0 no ded $0 no ded Rx deductible (individual/family) $0 $0 Retail generic $7 Out-of-pocket maximum, individual/family includes: 12 Preventive services8 Physician services Urgent care 9 Hospital/other medical services Outpatient surgery Outpatient lab/pathology Prescription drugs16, 17, 18, 19, 20, 21 $7 Retail brand 50% up to $125 max per prescription 22 50% up to $125 max per prescription22 Retail non-formulary brand 50% up to $250 max per prescription22 50% up to $250 max per prescription22 Pediatric routine eye exam25, 26 $0 no ded $0 no ded Pediatric glasses $0 no ded $0 no ded Adult routine eye exam26 $0 no ded $0 no ded Allowance up to $150 for frames or $100 for contact lenses at Visionworks stores Allowance up to $150 for frames or $100 for contact lenses at Visionworks stores Pediatric dental deductible (per individual)30 $0 $0 Pediatric exams and cleanings $0 $0 Pediatric basic, major and orthodontia services30, 32, 33 Copay varies Copay varies Additional benefits Vision24 25, 27 Adult eyewear (glasses or contacts) 28 Dental29 30, 31 28 Keystone HMO Silver Proactive2 You pay in-network6 Tier 1 - Preferred You pay in-network6 Tier 2 - Enhanced You pay in-network6 Tier 3 - Standard $0 $4,500/$9,000 $4,500/$9,000 0%; unless otherwise noted 5%; unless otherwise noted 10%; unless otherwise noted $6,600/$13,200 coinsurance and copays $6,600/$13,200 coinsurance, copays, and ded $6,600/$13,200 coinsurance, copays, and ded $0 $0 no ded $0 no ded $0 $0 no ded $0 no ded $750 $750 no ded $750 no ded $25 $40 no ded $50 no ded $50 $70 no ded $100 no ded $100 $100 no ded $100 no ded $50 $50 no ded $50 no ded $60 $60 no ded $60 no ded $500 per day11 Subject to ded and $900 per day11 Subject to ded and $1,300 per day11 0% 5% after ded 10% after ded $550 $550 no ded $550 no ded $60 $60 no ded $60 no ded $250 $250 no ded $250 no ded 50% 50% no ded 50% no ded 50% 50% no ded 50% no ded $50 $50 no ded $50 no ded $500 per day $500 per day no ded $500 per day11 no ded $250 Subject to ded and $750 copay Subject to ded and $1,250 copay $250 Subject to ded and $750 copay Subject to ded and $1,250 copay $0 $0 no ded $0 no ded $0 $0 no ded $0 no ded $022 $022 $022 11 11 $1522,23 50% up to $400 max per prescription $1522,23 50% up to $400 max per prescription $1522,22 22 50% up to $400 max per prescription22 50% up to $500 max per prescription22 50% up to $500 max per prescription22 50% up to $500 max per prescription22 $0 $0 no ded $0 no ded $0 $0 no ded $0 no ded $0 $0 no ded $0 no ded Allowance up to $150 for frames or $100 for contact lenses at Visionworks stores Allowance up to $150 for frames or $100 for contact lenses at Visionworks stores Allowance up to $150 for frames or $100 for contact lenses at Visionworks stores $0 $0 $0 $0 $0 $0 Copay varies Copay varies Copay varies 22 All footnotes listed on page 35 ded = Deductible 29 Silver health plans (cont.) Benefits per contract year1 PPO Silver HSA4 You pay in-network You pay out-of-network7 Deductible, individual/family $2,200/$4,400 $10,000/$20,000 Coinsurance 10% 50% Out-of-pocket maximum, individual/family includes: $6,450/$12,900 coinsurance, copays, and ded $20,000/$40,000 coinsurance and ded Preventive care for adults and children $0 no ded 50% no ded Preventive colonoscopy for colorectal cancer screening - Preventive Plus providers $0 no ded N/A Preventive colonoscopy for colorectal cancer screening - All other providers $750 no ded 50% no ded Primary care office visit/retail clinic 10% after ded 50% after ded Specialist office visit 10% after ded 50% after ded Urgent care 10% after ded 50% after ded 10% after ded 50% after ded 10% after ded 50% after ded Inpatient hospital services (includes maternity) 10% after ded 50% after ded Inpatient professional services (includes maternity) 10% after ded 50% after ded Emergency room (not waived if admitted) 10% after ded 10% after in-network ded Routine radiology/diagnostic 10% after ded 50% after ded MRI/MRA, CT/CTA scan, PET scan 10% after ded 50% after ded Biotech/specialty injectables 10% after ded 50% after ded Durable medical equipment/prosthetics 10% after ded 50% after ded Mental health, serious mental illness & substance abuse - outpatient 10% after ded 50% after ded Mental health, serious mental illness & substance abuse - inpatient 10% after ded 50% after ded Ambulatory surgical facility 10% after ded 50% after ded Hospital-based 10% after ded 50% after ded Freestanding 10% after ded 50% after ded Hospital-based 10% after ded 50% after ded Rx deductible (individual/family) Integrated Integrated Retail generic $7 after ded 50% after ded Retail brand $40 after ded22 50% after ded22 Retail non-formulary brand $60 after ded 50% after ded22 Preventive services8 Physician services Spinal manipulations (20 visits per year) 9 Physical/occupational therapy (30 visits per year) 9 Hospital/other medical services Outpatient surgery Outpatient lab/pathology Prescription drugs16, 17, 18, 19, 20, 21 22 Additional benefits Vision24 Pediatric routine eye exam25, 26 $0 after ded Not covered Pediatric glasses25, 27 $0 after ded Not covered Adult routine eye exam $0 after ded Not covered Adult eyewear (glasses or contacts)28 Allowance up to $150 for frames or $100 for contact lenses at Visionworks stores after ded Not covered Pediatric dental deductible (per individual)30 Integrated Not covered Pediatric exams and cleanings $0 no ded Not covered Pediatric basic, major and orthodontia services30, 32, 33 10% after ded Not covered 26 Dental29 30, 31 30 PPO Silver HSA 254 PPO Silver HRA 252 Employer Contribution - $550 individual/$1,100 family Employer Contribution - $550 individual/$1,100 family You pay in-network You pay out-of-network7 You pay in-network You pay out-of-network7 $2,200/$4,400 $10,000/$20,000 $2,200/$4,400 $10,000/$20,000 50% 50% 50% 50% $6,450/$12,900 coinsurance, copays, and ded $20,000/$40,000 coinsurance and ded $6,450/$12,900 coinsurance, copays, and ded $20,000/$40,000 coinsurance and ded $0 no ded 50% no ded $0 no ded 50% no ded $0 no ded N/A $0 no ded N/A $750 no ded 50% no ded $750 no ded 50% no ded 50% after ded 50% after ded 50% after ded 50% after ded 50% after ded 50% after ded 50% after ded 50% after ded 50% after ded 50% after ded 50% after ded 50% after ded 50% after ded 50% after ded 50% after ded 50% after ded 50% after ded 50% after ded 50% after ded 50% after ded 50% after ded 50% after ded 50% after ded 50% after ded 50% after ded 50% after ded 50% after ded 50% after ded 50% after ded 50% after in-network ded 50% after ded 50% after in-network ded 50% after ded 50% after ded 50% after ded 50% after ded 50% after ded 50% after ded 50% after ded 50% after ded 50% after ded 50% after ded 50% after ded 50% after ded 50% after ded 50% after ded 50% after ded 50% after ded 50% after ded 50% after ded 50% after ded 50% after ded 50% after ded 50% after ded 50% after ded 50% after ded 50% after ded 50% after ded 50% after ded 50% after ded 50% after ded 50% after ded 50% after ded 50% after ded 50% after ded 50% after ded 50% after ded 50% after ded 50% after ded 50% after ded 50% after ded 50% after ded Integrated Integrated Integrated Integrated $7 after ded 50% after ded $7 after ded 50% after ded $40 after ded22 50% after ded22 $40 after ded22 50% after ded22 $60 after ded 50% after ded $60 after ded 50% after ded22 $0 after ded Not covered $0 after ded Not covered $0 after ded Not covered $0 after ded Not covered $0 after ded Not covered $0 after ded Not covered Allowance up to $150 for frames or $100 for contact lenses at Visionworks stores after ded Not covered Allowance up to $150 for frames or $100 for contact lenses at Visionworks stores after ded Not covered Integrated Not covered Integrated Not covered $0 no ded Not covered $0 no ded Not covered 50% after ded Not covered 50% after ded Not covered 22 22 22 All footnotes listed on page 35 ded = Deductible 31 Bronze health plans DPOS Bronze2 Benefits per contract year1 You pay in-network You pay out-of-network5 Deductible, individual/family $6,000/$12,000 $10,000/$20,000 Coinsurance 0% 50% Out-of-pocket maximum, individual/family includes: $6,600/$13,200 coinsurance, copays, and ded $40,000/$80,000 coinsurance and ded Preventive care for adults and children $0 no ded 50% no ded Preventive colonoscopy for colorectal cancer screening - Preventive Plus providers $0 no ded N/A Preventive colonoscopy for colorectal cancer screening - All other providers $750 no ded 50% no ded Primary care office visit/retail clinic $40 no ded 50% after ded Specialist office visit $80 no ded 50% after ded Urgent care $0 after ded 50% after ded Spinal manipulations (20 visits per year)9 $80 no ded10 50% after ded 10 $80 no ded 50% after ded Inpatient hospital services (includes maternity) $0 after ded 50% after ded Inpatient professional services (includes maternity) $0 after ded 50% after ded Emergency room (not waived if admitted) $0 after ded $0 after in-network ded Routine radiology/diagnostic 10 $60 no ded 50% after ded MRI/MRA, CT/CTA scan, PET scan $250 no ded 50% after ded Biotech/specialty injectables $100 no ded 50% after ded Durable medical equipment/prosthetics 50% after ded 50% after ded Mental health, serious mental illness & substance abuse - outpatient $80 no ded 50% after ded Mental health, serious mental illness & substance abuse - inpatient $0 after ded 50% after ded Ambulatory surgical facility $0 after ded 50% after ded Hospital-based $0 after ded 50% after ded Freestanding $0 no ded 50% after ded Hospital-based $0 no ded 50% after ded Rx deductible (individual/family) Integrated Integrated Retail generic $7 no ded Member pays 70% of retail no ded Retail brand $50 after ded22 Member pays 70% of retail after ded22 Retail non-formulary brand $75 after ded Member pays 70% of reatil after ded22 Pediatric routine eye exam25, 26 $0 no ded Not covered Pediatric glasses25, 27 $0 no ded Not covered $0 no ded Not covered Allowance up to $150 for frames or $100 for contact lenses at Visionworks stores Not covered Pediatric dental deductible (per individual)30 $0 Not covered Pediatric exams and cleanings30, 31 $0 Not covered Copay varies Not covered Preventive services8 Physician services Physical/occupational therapy (30 visits per year) 9 Hospital/other medical services Outpatient surgery Outpatient lab/pathology Prescription drugs16, 17, 18, 19, 20, 21 22 Additional benefits Vision24 Adult routine eye exam 26 Adult eyewear (glasses or contacts) 28 Dental29 Pediatric basic, major and orthodontia services 30, 32, 33 32 HMO Bronze2 HMO Bronze Basic2 PPO Bronze HSA4 You pay in-network6 You pay in-network6 You pay in-network You pay out-of-network7 $6,000/$12,000 $6,300/$12,600 $5,500/$11,000 $10,000/$20,000 0% 0% 0% 50% $6,600/$13,200 coinsurance, copays, and ded $6,600/$13,200 coinsurance, copays, and ded $6,450/$12,900 coinsurance, copays, and ded $20,000/$40,000 coinsurance and ded $0 no ded $0 no ded $0 no ded 50% no ded $0 no ded $0 no ded $0 no ded N/A $750 no ded $750 no ded $750 no ded 50% no ded $40 no ded $50 no ded $0 after ded 50% after ded $80 no ded $0 after ded $0 after ded 50% after ded $0 after ded $0 after ded $0 after ded 50% after ded $80 no ded $0 after ded $0 after ded 50% after ded $80 no ded $50 no ded $0 after ded 50% after ded $0 after ded $0 after ded $0 after ded 50% after ded $0 after ded $0 after ded $0 after ded 50% after ded $0 after ded $0 after ded $0 after ded $0 after in-network ded $60 no ded $60 no ded $0 after ded 50% after ded $250 no ded $250 no ded $0 after ded 50% after ded $100 no ded $100 no ded $0 after ded 50% after ded 50% after ded 50% after ded $0 after ded 50% after ded $80 no ded $0 after ded $0 after ded 50% after ded $0 after ded $0 after ded $0 after ded 50% after ded $0 after ded $0 after ded $0 after ded 50% after ded $0 after ded $0 after ded $0 after ded 50% after ded $0 no ded $0 no ded $0 after ded 50% after ded $0 no ded $0 no ded $0 after ded 50% after ded Integrated Integrated Integrated Integrated $7 no ded $7 after ded $7 after ded 50% after ded $50 after ded22 $30 after ded22 $40 after ded22 50% after ded22 $75 after ded $50 after ded $60 after ded 50% after ded22 $0 no ded $0 no ded $0 after ded Not covered $0 no ded $0 no ded $0 after ded Not covered $0 no ded Not covered $0 after ded Not covered Allowance up to $150 for frames or $100 for contact lenses at Visionworks stores Not covered Allowance up to $150 for frames or $100 for contact lenses at Visionworks stores after ded Not covered $0 $0 Integrated Not covered $0 $0 $0 no ded Not covered Copay varies Copay varies 50% after ded Not covered 22 22 22 All footnotes listed on page 35 ded = Deductible 33 Bronze health plans (cont.) PPO Bronze Premier HSA4 Benefits per contract year1 You pay in-network You pay out-of-network7 Deductible, individual/family $4,000/$8,000 $10,000/$20,000 Coinsurance 50% 50% Out-of-pocket maximum, individual/family includes: $6,450/$12,900 coinsurance, copays, and ded $20,000/$40,000 coinsurance and ded Preventive care for adults and children $0 no ded 50% no ded Preventive colonoscopy for colorectal cancer screening - Preventive Plus providers $0 no ded N/A Preventive colonoscopy for colorectal cancer screening - All other providers $750 no ded 50% no ded Primary care office visit/retail clinic 50% after ded 50% after ded Specialist office visit 50% after ded 50% after ded Urgent care 50% after ded 50% after ded 50% after ded 50% after ded 50% after ded 50% after ded Inpatient hospital services (includes maternity) 50% after ded 50% after ded Inpatient professional services (includes maternity) 50% after ded 50% after ded Emergency room (not waived if admitted) 50% after ded 50% after in-network ded Routine radiology/diagnostic 50% after ded 50% after ded MRI/MRA, CT/CTA scan, PET scan 50% after ded 50% after ded Biotech/specialty injectables 50% after ded 50% after ded Durable medical equipment/prosthetics 50% after ded 50% after ded Mental health, serious mental illness & substance abuse - outpatient 50% after ded 50% after ded Mental health, serious mental illness & substance abuse - inpatient 50% after ded 50% after ded Ambulatory surgical facility 50% after ded 50% after ded Hospital-based 50% after ded 50% after ded Freestanding 50% after ded 50% after ded Hospital-based 50% after ded 50% after ded Rx deductible (individual/family) Integrated Integrated Retail generic $7 after ded 50% after ded Retail brand $40 after ded22 50% after ded22 Retail non-formulary brand $60 after ded 50% after ded22 Pediatric routine eye exam25, 26 $0 after ded Not covered Pediatric glasses25, 27 $0 after ded Not covered Adult routine eye exam $0 after ded Not covered Adult eyewear (glasses or contacts)28 Allowance up to $150 for frames or $100 for contact lenses at Visionworks stores after ded Not covered Pediatric dental deductible (per individual)30 Integrated Not covered Pediatric exams and cleanings $0 no ded Not covered Pediatric basic, major and orthodontia services30, 32, 33 50% after ded Not covered Preventive services8 Physician services Spinal manipulations (20 visits per year) 9 Physical/occupational therapy (30 visits per year) 9 Hospital/other medical services Outpatient surgery Outpatient lab/pathology Prescription drugs16, 17, 18, 19, 20, 21 22 Additional benefits Vision24 26 Dental29 30, 31 34 All footnotes listed on page 35 ded = Deductible Important plan details Medical 1. Certain plan benefits may be enhanced to comply with health care reform law/regulations. Eligible dependent children are covered to age 26. 2. Family deductible and out-of-pocket maximum apply when an individual and one or more dependents are enrolled. Once an individual meets the individual deductible amount, claims for that individual will apply. Once the family deductible is met, claims for all individuals will pay. Single deductible and out-of pocket maximum apply only when an individual is enrolled without dependents. 3. Family out-of-pocket maximum applies when an individual and one or more dependents are enrolled. Once an individual meets the individual out-of-pocket maximum, benefits for that individual are covered in full. Once the family out-of-pocket maximum is met, benefits for all family members are covered in full. Single out-of pocket maximum applies only when an individual is enrolled without dependents. 4. Family deductible and out-of-pocket maximum apply when an individual and one or more dependents are enrolled. The full family deductible must be met by family members before claims are eligible to pay. Once the family out-of pocket maximum is met, benefits for all family members are covered in full. If an individual is enrolled without dependents, the single deductible and out-of-pocket maximum apply. 5. To receive maximum benefits, services must be provided by a Keystone Health Plan East participating provider. This is a highlight of benefits available. The benefits and exclusion for in-network and out-of-network care are not the same. All benefits are provided in accordance with the HMO group contract and out-of-network benefit booklet/certificate. 6. There are no out-of-network services available except for emergency services. 7. Non-Participating Preferred Providers may bill you for differences between the Plan allowance, which is the amount paid by IBC, and the actual charge of the provider. This amount may be significant. Claims payments for Non-Preferred Professional Providers (physicians) are based on the lesser of the Medicare Professional Allowable Payment or the actual charge of the provider. For covered services that are not recognized or reimbursed by Medicare, payment is based on the lesser of the IBC applicable proprietary fee schedule or the actual charge of the provider. For covered services not recognized or reimbursed by Medicare or IBC’s fee schedule, the payment is based on 50 percent of the actual charge of the provider. It is important to note that all percentages for out-of-network services are percentage of the Plan allowance, not the actual charge of the provider. 8. Age and frequency schedules may apply. For routine colonoscopy for colorectal cancer screening, your cost share may vary depending on where you receive service. 9. For PPO plans, visit limits are combined in-and out-of-network. 10. Referral required from primary care physician. 11. Amount shown reflects the copayment per day. There is a maximum of five copayments per admission. 12. For Keystone HMO Proactive plans, the out-of-pocket maximum for Tiers 1, 2, and 3 are combined. 13. For Keystone HMO Proactive plans, all in-network retail clinics are assigned to Tier 1, with the exception of Walgreens Healthcare Clinic, which is assigned Tier 3. 14. For Keystone HMO Proactive plans, if admitted to an in-network hospital from the emergency room, the out-of-pocket costs for inpatient hospital will apply based on the tier of the in-network hospital. If admitted to an out-of-network hospital following an emergency room admission, the Tier 3 in-network level of benefits will apply. Non-Participating Providers for Emergency Services will be covered at the Tier 3 level of benefits. 15. For Keystone HMO Silver Proactive plan, deductible is combined for Tiers 2 and 3. Prescription Drugs 16. Prescription drug benefits are administered by FutureScripts, a Catamaran company, an independent company providing pharmacy benefit management services. 17. No cost-sharing is required at participating retail and mail order pharmacies for certain designated preventive drugs, prescription and over-the-counter (with a doctor’s prescription). 18. Out-of-Network benefits apply to prescriptions filled at non-participating pharmacies and the member must pay the full retail price for their prescription then file a paper claim for reimbursement. The member should refer to their benefit booklet to determine the out-of-network coverage for their plan. 19. Mail Order coverage is available for all Prescription Drug Plans. The FutureScripts Mail Order service is a convenient and cost-effective way to order up to a 90-day supply of maintenance or long-term medication for delivery to a home, office, or location of choice. 20. All covered self-administered specialty medications except insulin will be provided through the convenient FutureScripts Specialty Pharmacy Program for the appropriate retail cost sharing. Benefits are available for up to a 30-day supply. If the doctor wants the member to start the drug immediately, an initial 30-day supply may be obtained at a participating retail pharmacy. However, all subsequent fills must be purchased through the Specialty Pharmacy Program. 21. Select plans utilize the FutureScripts Preferred Pharmacy Network – a subset of the national retail pharmacy network. It includes over 50,000 pharmacies, including most major chains and local pharmacies except Walgreens and Rite Aid. 22. When a prescription drug is not available in a generic form, benefits will be provided for the brand drug and the member will be responsible for the cost sharing for a brand drug. When a prescription drug is available in a generic form, benefits will be provided for that drug at the generic drug level only. If the member chooses to purchase a brand drug, the member will be responsible for paying the dispensing pharmacy the difference between the negotiated discount price for the generic drug and the brand drug plus the appropriate cost sharing for a brand drug. 23. Certain designated generic drugs available at participating retail and mail order pharmacies for a reduced member cost sharing ($4 Retail/$8 Mail Order), after any applicable deductible. Additional Benefits 24. IBC Vision Care is administered by Davis Vision, an independent company. 25. Pediatric vision benefits expire at the end of the month in which the child turns 19. 26. One eye exam per calendar year period. 27. Pediatric spectacle lenses covered at no extra cost include: single vision, lined bifocal, lined trifocal, or lenticular lenses. For frames to be covered in full, choose from Davis Vision’s Pediatric Frame Selection (available at most independent participating providers and at Visionworks retail centers, a national optical chain). 28. For all other Davis Vision providers, there is a $100 allowance for frames or contact lenses, after any applicable deductible to high deductible health plans. 29. Independence Blue Cross dental plans are administered by United Concordia, an independent company. 30. Pediatric dental benefits are covered until the end of the contract year in which the child turns 19. 31. One exam and one cleaning every six months per contract year. 32. Only medically necessary orthodontia is covered. There is a 12-month waiting period for all orthodontia. 33. You can find descriptions of covered Pediatric Dental services and specific member cost share by visiting ibx.com/sgdental. The Member has the right to receive health care services without discrimination based on race, ethnicity, age, mental or physical disability, genetic information, color, religion, gender, sexual orientation, national origin, or source of payment. 35 Underwriting information Maximum Product offerings1 • Small groups (2-50) are allowed up to three packaged plans which include medical, prescription drug, vision (adult and pediatric) and pediatric dental benefits. • If a group is offering a PPO plan for out of area enrollment, the PPO benefit level must be equivalent to the benefit plans offered to the in-area employees. Group offerings may not exceed three plans, including a plan for out-of-area PPO coverage. Participation requirements2 • Groups of 2-50 must have 70 percent participation, which includes all product lines. IBC and affiliates must be sole carrier. • IBC will count waivers in the eligibility calculations. • Credit is given for those eligible subscribers who opt out because they have coverage through a spouse, as an eligible dependent to 26, or are enrolled in Medicare or Medicaid. Only these types of opt-outs, or waivers, are excluded from the calculation to determine if a group meets the participation requirement. • Retiree-only groups will not be accepted. For groups covering retirees, 100 percent participation will be required for retired employees. The group must consist of a minimum of 70 percent active employees. Employer contribution requirement2 • For contributory plan offerings, you must contribute a minimum of 25 percent of the calculated gross monthly premium. Off-anniversary benefit change • Upgrades and downgrades will only be allowed on anniversary. High deductible health plan funding limitation • Per the ACA regulations, employers should not fund more or less than the federally mandated standards for funding employee deductibles. • The high deductible plan design selected will specify the funding requirement; please refer to each plan design for specific funding requirements. Submission guidelines • All offerings are subject to final underwriting review and acceptance. Additional guidelines and policies may apply. This document is for informational purposes only and is not intended to be all inclusive. 1. P lease visit ibx.com/bc for maximum product offerings and underwriting guidelines specific to Blue Solutions Choice. 2. As permitted by the state and federal laws and regulations. 36 What’s not covered? The information in this brochure represents only a partial listing of benefits and exclusions of the plans. Benefits and exclusions may be further defined by medical policy. The managed care plan may not cover all of your health care expenses. Read your contract/member handbook/benefit booklet carefully to determine which health care services are covered. If you need more information please call 1-800-275-2583. • Services not medically necessary • Services or supplies that are experimental or investigative, except routine costs associated with qualifying clinical trials • Hearing aids, hearing examinations/tests for the prescription/fitting of hearing aids, and cochlear electromagnetic hearing devices • Assisted fertilization techniques, such as in vitro fertilization, GIFT, and ZIFT • Reversal of voluntary sterilization • Expenses related to organ donation for nonemployee recipients • Music therapy, equestrian therapy, and hippotherapy • Treatment of sexual dysfunction not related to organic disease except for sexual dysfunction relating to an injury • Routine foot care, unless medically necessary or associated with the treatment of diabetes • Foot orthotics, except for orthotics and podiatric appliances required for the prevention of complications associated with diabetes • Cranial prosthesis, including wigs intended to replace hair loss • Alternative therapies/complementary medicine such as acupuncture • Routine physical exams for nonpreventive purposes, such as insurance or employment applications, college, or premarital examinations • Immunizations for travel or employment • Services or supplies payable under workers’ compensation, motor vehicle insurance, or other legislation of similar purpose • Cosmetic services/supplies • Bariatric or obesity surgery • Outpatient private duty nursing Benefits that require preapproval Additional approval from IBC may be required before your employees may receive certain tests, procedures, and medications. When your employees need services that require preapproval, their primary care physician or provider contacts the Care Management and Coordination (CMC) team and submits information to support the request for services. The CMC team, made up of physicians and nurses, evaluates the proposed plan of care for payment of benefits. The CMC team will notify your employee’s physician/provider if the services are approved for coverage. If the CMC team does not have sufficient information or the information evaluated does not support coverage, your employee and his or her physician/provider are notified in writing of the decision. Employees or a provider acting on their behalf may appeal the decision. At any time during the evaluation process or the appeal, the provider or your employee may submit additional information to support the request. For a list of services that require preapproval, visit www.ibx.com/preapproval. 37 Blue Solutions Independence Blue Cross offers products directly, through its subsidiaries Keystone Health Plan East and QCC Insurance Company, and with Highmark Blue Shield. Independent Licensees of the Blue Cross and Blue Shield Association 17357 2014-1537 7/14
© Copyright 2026